Abstract
Abdominal aortic aneurysm (AAA) disease is characterized by an asymptomatic, permanent, focal dilatation of the abdominal aorta progressing towards rupture, which confers significant mortality. Patient management and surgical decisions rely on aortic diameter measurements via abdominal ultrasound surveillance. However, AAA rupture can occur at small diameters or may never occur at large diameters, implying that anatomical size is not necessarily a sufficient indicator. Molecular imaging may help identify high-risk patients through AAA evaluation independent of aneurysm size, and there is the question of the potential role of positron emission tomography (PET) and emerging role of novel radiotracers for AAA. Therefore, this review summarizes PET studies conducted in the last 10 years and discusses the usefulness of PET radiotracers for AAA risk stratification. The most frequently reported radiotracer was [18F]fluorodeoxyglucose, indicating inflammatory activity and reflecting the biomechanical properties of AAA. Emerging radiotracers include [18F]-labeled sodium fluoride, a calcification marker, [64Cu]DOTA-ECL1i, an indicator of chemokine receptor type 2 expression, and [18F]fluorothymidine, a marker of cell proliferation. For novel radiotracers, preliminary trials in patients are warranted before their widespread clinical implementation. AAA rupture risk is challenging to evaluate; therefore, clinicians may benefit from PET-based risk assessment to guide patient management and surgical decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Abdominal aortic aneurysm (AAA) disease is characterized by localized, irreversible dilatation of the abdominal aorta from a normal diameter of approximately 10–20 mm to an aneurysmal diameter of 30 mm or greater. AAA is asymptomatic, yet simultaneously progressive towards rupture and profound internal bleeding, resulting in a high mortality rate in the range of 59–83% for patients with ruptured AAA who cannot access a hospital promptly and do not undergo surgery.1,2,3 From 2005 to 2012, 39,740 aneurysm-associated deaths occurred in England alone.4 Various environmental and genetic risk factors contribute to the development and progression of AAA; the predominant risk factors of AAA include advanced age, male sex, smoking, and elevated blood pressure.1,5,6 Emerging evidence also suggests that diabetes may play a protective role in patients who are susceptible to developing AAA; however, this correlation requires further investigation.7,8
Scope of the clinical problem
Early-stage AAA does not manifest with any apparent signs or symptoms; therefore, it is usually diagnosed incidentally during unrelated medical check-ups or through screening programs, which have been formally launched in several countries including the UK, the US, and Sweden.9,10,11,12 The National Health Service AAA Screening Programme was fully implemented in 2013 in England to offer routine ultrasound scanning (USS)-based screening for all men 65 years of age and older. This program was established based on the results of the UK Multicentre Aneurysm Screening Study, which demonstrated a nearly 50% reduction in AAA-related mortality risk after 13 years in men invited for screening compared with that in men who did not undergo screening (0.66% vs 1.12%). This reduction was also found to be associated with an incremental cost-effectiveness ratio of £7,600 per quality-adjusted life years gained at 10 years.13,14 With a maximum reported sensitivity of 95% and specificity of nearly 100%, USS is predominantly used in the clinic to screen for AAA because of its ease of operability, low costs, low post-imaging workload and instantaneous results, and widespread availability.3 It is important to note here that although there is extensive ongoing research to establish more reliable and informative risk markers of AAA, the only indicator that is used consistently in the clinic is aortic size, which is derived from serial USS, or occasionally, computed tomography (CT). This is the simplest and most convenient parameter to extract using USS, but may not always accurately reflect prognosis, as small AAA has been reported to rupture, while large AAA has been reported as remaining intact.15 Therefore, the inability to accurately predict the prognosis of patients with AAA and stratify patients according to AAA risk remains a significant unmet clinical challenge.
In this context, molecular imaging may have a significant role in assessing AAA evolution. Positron emission tomography (PET) imaging offers a means to quantitatively measure molecular mechanisms related to AAA even at early stages as an adjunctive tool to USS-based screening and surveillance. PET is an attractive functional modality to reveal the underlying molecular changes that occur before the more apparent anatomical changes associated with AAA progression. The use of PET with a suitable radiotracer may then successfully help personalize a surveillance regimen or define a more precise intervention threshold to prevent aortic complications. Furthermore, it may contribute to the discovery of an appropriate pharmacological treatment for AAA, as currently, the only viable treatment option available is surgical intervention, the indication for which is based solely on the aortic size, as measured using USS. Establishing a pharmacological treatment that could reduce or even reverse AAA progression is a strategic aim of AAA-related research, but this necessitates a stratification imaging biomarker that could (a) help select patients who would benefit from such treatment, (b) predict AAA growth and rupture and refine watchful waiting regimens, (c) determine patient-specific intervention thresholds, or (d) be applied in all the aforementioned applications. Therefore, this review summarizes preclinical and clinical PET studies published in the last 10 years and discusses the usefulness of PET for AAA risk stratification.
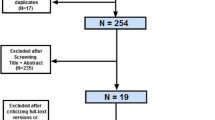
Preclinical studies
Much of our pathological understanding of AAA in patients is based on aortic tissue acquired during surgery (i.e., late-stage disease); hence, theories derived from these samples may not accurately represent the mechanisms of early-stage disease, when a novel pharmacological therapy may be administered. Preclinical studies of AAA are the first step in achieving a more complete picture of early-stage AAA pathophysiology, which may help establish stratification biomarkers that may be translated to the clinic. Table 1 presents the details of all preclinical PET studies of AAA published between 2010 and 2020.
Preclinical studies are conducted with the aim of better matching animal models to the equivalent stage of human AAA. Calcification, proliferation, angiogenesis, and inflammation are some key processes that contribute to the AAA pathogenesis16; elucidating how these mechanisms are inter-connected at various stages of AAA progression can guide the development of more longitudinally representative preclinical models. For example, English et al. demonstrated that the uptake of [64Cu]DOTA-ECL1i shows little variation between days 7 and 14 post-aneurysm induction in the porcine pancreatic elastase-induced AAA murine model, reflecting non-fluctuating levels of vascular wall inflammation during this period.17 Another [64Cu]-based radiotracer, [64Cu]NOTA-TRC105-Fab, has been shown to exhibit high uptake in the calcium-induced murine model, indicating increased angiogenic activity; however, its high residual blood pool activity even 24 hours post-injection remains a key limitation.18 Using the angiotensin II-induced AAA murine model, Gandhi et al. showed that there is increased [18F]fluorothymidine ([18F]FLT) uptake on day 14 post-aneurysm induction, but this uptake is significantly reduced on day 28.19 These findings have important implications in supporting the idea of early-stage cellular remodeling that may drive disease progression, a notion that has been introduced and deliberated by several groups.20,21,22 In the future, knowledge gained from these studies may facilitate early-stage risk stratification; however, further preclinical and clinical investigations are warranted to reinforce this theory.23 Li et al. demonstrated that the uptake of [18F]-labeled sodium fluoride ([18F]NaF), reflecting microcalcification, is increased between days 14 and 28 in the angiotensin II-induced AAA murine model preceding notable aortic expansion.24 In the same model, Nahrendorf et al. showed that the uptake of [18F]-cross-linked iron oxide ([18F]CLIO) in AAA is associated with the risk of AAA growth and rupture.25 However, a key drawback to the use of nanoparticle-based radiotracers such as [18F]CLIO is their extended circulation period, necessitating delayed imaging to avoid capturing the blood pool activity that may mask AAA uptake. Radiotracers consisting of smaller nanoparticles with a shorter clearance time may evade this issue. These are just a few examples of studies that have attempted to investigate the time course of biological events in AAA, which can help develop more informative preclinical models of AAA that are easily translatable to the clinic.
Nevertheless, the translation of preclinical PET research to the clinic is not free of hurdles. There is an overwhelming cost of introducing new radiotracers in the clinic, along with long-standing regulations that may prevent or delay the implementation of radiotracers not readily used for other applications such as cancer diagnostics. Few centres have easy access to a cyclotron for radiotracer production, thereby largely limiting centers to using radiotracers with sufficiently workable half-lives such as radiotracers labeled predominantly with [18F]; instead, alternatives that do not require a cyclotron for production such as [68Ga]-labeled radiotracers may be employed.26 Moreover, the translational success of preclinical findings may then be influenced by several factors, such as differences in toxicology and pharmacokinetics27; gaining a better understanding of these factors will ultimately benefit the clinical translation of important preclinically validated biomarkers.
Clinical studies
Over the last several decades, the incidence of AAA rupture has decreased. This is largely attributed to the implementation of AAA screening programs and novel therapeutic interventions, such as endovascular aortic repair (EVAR). That being said, the low rupture rate of small aneurysms and risks associated with surgery do not sufficiently rationalize the routine repair of small AAA.28 Clinical guidelines on the use of EVAR have been amended often, owing to its reduced long-term durability and moderate long-term survival benefits.29 Therefore, by non-invasively detecting established biological targets, such as inflammation with [18F]fluorodeoxyglucose ([18F]FDG) PET, clinicians may be able to identify patients with a high risk of clinical events and those who may benefit the most from elective repair. Generally, PET radiotracers approved for non-AAA applications have facilitated clinical studies of AAA. Table 2 presents the details of all clinical PET studies of AAA conducted between 2010 and 2020, revealing as expected that the predominant radiotracer in use is [18F]FDG.
Controversy of [18F]FDG
[18F]FDG is the most common radiotracer utilized for PET imaging. As presented in Table 1 and Table 2, there has been an extensive focus on markers of inflammatory activity, evidenced by the overwhelming predominance of [18F]FDG PET studies: 5 of 11 preclinical and 24 of 28 clinical studies. With its widespread availability and well-established safety profile, [18F]FDG is a typically universal starting point for clinical PET research. The intracellular distribution of [18F]FDG is associated with the degree of metabolic activity and inflammation in regions of uptake.30 [18F]FDG uptake on PET has been demonstrated to correlate with macrophage density in plaques, cardiovascular risk factors, the Framingham risk score, and various inflammatory and glycolysis-related biomarkers, such as glucose transporters 1 and 3 and total lesion glycolysis.31,32,33 Yet, a patient receiving anti-inflammatory drugs has been reported to develop AAA that rapidly expanded and ruptured34; this case suggests that inflammation may be fallible as a single indicator of patient prognosis and may need to be supplemented with other biomarkers. A downside to the advantage of [18F]FDG highlighting all regions of active glucose metabolism is that, as a result, it is difficult to differentiate disease-specific activity. Moreover, the uptake of [18F]FDG can be influenced by conditions of disease microenvironments, such as hypoxia or increased myocardial muscle activity, or the efficiency with which the microcirculation distributes the radiotracer.35,36,37
Both preclinical and clinical studies of gold-standard [18F]FDG PET to assess glucose metabolism and inflammation in AAA have yielded varying results of both increased and variable [18F]FDG uptake.38,39,40,41 Some studies have shown that [18F]FDG PET may be useful to predict AAA expansion and/or progression,42,43 while other studies have contradicted this.38,44 For example, Tsuruda et al. showed that increased aortic uptake of [18F]FDG in patients is associated with active aortic wall inflammation, which may contribute to AAA progression and rupture, while patients showing [18F]FDG uptake in AAA revealed no correlation with aortic expansion 12 months later in a study by Kotze et al.38,45 Moreover, Nchimi et al. and Huang et al. demonstrated that [18F]FDG uptake correlates positively with wall stress and strength in AAA, whereas Barwick et al. found no significant difference in aortic uptake of [18F]FDG between patients with infra-renal AAA and patients without AAA.40,43,44
In a study of [18F]FDG PET and contrast-enhanced magnetic resonance imaging (MRI), Kuzniar et al. demonstrated that the hotspots of [18F]FDG uptake and late gadolinium enhancement rarely coincide in AAA, although both are associated with aneurysm growth, raising interesting questions about the distribution of cellular activity in AAA.46 Collectively, these findings contribute to a complicated story of glucose metabolism in AAA. This scenario is further confounded by the lack of consistency in the type of AAA presentation studied, such as asymptomatic, symptomatic, end-stage, and/or early-stage AAA. Meanwhile, [18F]FDG PET may have a promising role in identifying patients who may be at risk of experiencing endoleaks after undergoing EVAR.47,48,49 Validation of these prior studies would benefit from larger prospective studies investigating patients with a consistent type of AAA presentation. Further data corresponding to kinetic modeling and corrections for blood flow and volume would also be informative, lending to more comprehensive analysis and validation. Therefore, supplementing the information yielded by [18F]FDG with information from other radiotracers may facilitate a more detailed understanding of the molecular workings of AAA.
Emerging radiotracers
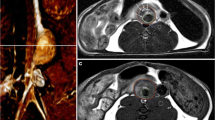
AAA comprises an intricate environment of various biological pathways; therefore, other PET radiotracers are also promising in the context of AAA. The sodium fluoride imaging of AAA (SoFIA3) trial has shown that uptake of [18F]NaF, which reflects regions of calcification, in patients with end-stage asymptomatic AAA predicts AAA progression and rupture, providing proof-of-concept data for the feasibility of a non-[18F]FDG PET radiotracer for AAA stratification. The findings of the trial suggest that [18F]NaF PET/CT is an effective tool to identify AAA disease activity in patients, based on the localization of the radiotracer in regions of microcalcification, which in turn, is a susceptibility marker of aneurysm expansion and rupture early after AAA formation.50
A key point arising from this study is that aneurysm size is not necessarily a predictor of rupture; AAA growth may be non-linear and influenced by biomechanical processes that may not necessarily exhibit an obvious detectable pattern. The SoFIA3 trial demonstrated that [18F]NaF uptake is a positive predictor of aneurysm growth and clinical outcomes, which are independent but supplementary to classic clinical parameters such as aneurysm diameter.50 The findings of this trial must be considered in light of the confounding issue of spill-in contamination from the nearby bone into the aneurysm; thus, background correction techniques are likely necessary to provide more robust quantitative assessments of AAA using [18F]NaF.51 Alternative radiotracers that may prove to be useful include markers of other characteristics of AAA development, such as angiogenesis, using integrin- or endoglin-targeted agents.18,52,53 Markers of cell proliferation and chemokine receptors such as [18F]FLT and [64Cu]DOTA-ECL1i are promising, and preliminary trials in patients are warranted to determine if these approaches may translate to the clinic.17,19,23 [18F]fluoromethylcholine, which is commonly implemented in prostate cancer staging, may also be beneficial to incidentally detect AAA in patients with prostate cancer.54 With these radiotracer applications, PET remains an attractive modality to advance our understanding of AAA pathophysiology, while novel molecular tracer agents are introduced, and hybrid multimodality systems are improved. As PET is readily accessible and already being used in the clinic, continued research using PET has practical applications that are feasible for clinical translation.
Outlook of PET for AAA assessment
AAA remains a significant cause of mortality due to aortic rupture. USS reveals anatomical changes in AAA size and shape; however, there remain gaps in our knowledge of the molecular changes that precede physical manifestation of AAA and in our ability to visualize these pathological mechanisms at the molecular level. Despite the large number of AAA studies conducted, our knowledge of AAA pathobiology is incomplete, and there remains a lack of concrete data to translate preclinical findings to clinical practice. The contributions of inflammatory activity, biomechanical disturbances, calcification, angiogenesis, and cell proliferation to aortic growth and aneurysm progression remain only partially understood; these may be clarified with the application of PET imaging utilizing specific biologically targeted radiotracers. A better understanding of these functional changes in early-stage AAA may help stratify patients based on rupture risk early in the disease course and guide appropriate treatment selection. In this context, the multifactorial pathophysiology of AAA in humans represents a growing area in cardiovascular research, largely because clinical studies of AAA are predominantly limited to using late-stage aortic tissue obtained during surgery, owing to the asymptomatic presentation of early-stage AAA and lack of intervention (and easy access to tissue) at this stage. Although several risk factors and potential contributors to the disease process have been identified, such as sex, age, comorbidities, and smoking, these are not yet sufficiently predictive when applied to individual patients as reliable and accurate assessment methods for these factors are not yet readily available. Thus, as management decisions are made based solely on aortic size, many patients are needlessly subjected to the risks of aortic repair, even in cases wherein an aneurysm might not have ruptured if left untreated.
As we move forward, a shift away from the size of an aneurysm as the sole indicator of AAA repair is perhaps required. The feasibility of alternative markers of AAA progression that may be more reliable must be investigated as adjuncts to traditional USS-based size information, including circulating biomarkers, four-dimensional or dynamic contrast-enhanced MRI findings such as vascular flow patterns, CT-based calcium scores, and haemodynamic parameters.55,56,57,58,59,60 Although anatomical imaging is mainly used in both preclinical and clinical imaging of AAA, molecular imaging is gaining increasing importance, and several new studies are anticipated in forthcoming years. Anatomical and molecular imaging techniques are not necessarily competitive; rather, they can be complementary in their usefulness for AAA management. Thus, PET offers a non-invasive means to detect and evaluate components of potentially contributing pathways in patients to better understand AAA development beyond morphological features. Ultimately, the most successful imaging tracer will reveal key aspects of AAA formation in humans, be used for patient risk stratification, and help assess treatment efficacy in novel clinical trials.61 Introducing a novel imaging tracer to the clinic is a lengthy and costly process, akin to drug research and development. Ultimately, novel radiotracers that may also be implemented in multiple diseases are more likely to undergo rapid and efficient clinical translation. Considering the rupture rate of small AAA, a large sample of patients would be required to demonstrate a novel agent’s value in assessing rupture risk for AAA smaller than 55 mm in diameter. Meanwhile, the presence of comorbidities such as heart and vascular diseases greatly affects a patient’s outcomes of surgical repair.62 Hence, a transitional step may be to first investigate patients with AAA larger than 55 mm in diameter, as they consequently carry a risk of complications, to identify who may benefit from repair in the presence of comorbidities.
PET technology and methodology
The ability of PET to yield precise, longitudinal quantitative data makes it a strong contender for clinical translation in the context of AAA risk stratification. Improvements in spatial resolution and the application of partial volume correction and background activity adjustments may improve the accuracy and precision of PET analysis methods in the future.63 One setback of PET is the potential inter-analytical variability depending on how the aortic region of interest (ROI) is defined. Standardizing ROI definitions and analytical methods is imperative to overcoming this challenge, and a significant advantage of PET is that data can be reviewed and corrected post-acquisition for temporal and spatial resolution, something that USS that does not yet offer. The ability to perform kinetic modeling of PET data, which would elucidate radiotracer biodistribution in the blood circulation, further makes PET an attractive and useful technology for AAA assessment. The small size of arteries and vessel walls necessitates the coupling of PET with anatomical modalities to distinguish radiotracer uptake in the aorta from that in surrounding regions. Standalone PET is typically combined with CT to add a layer of anatomical information while compensating for the limited spatial resolution of PET. With their widespread availability and low associated costs, hybrid PET/CT systems continue to advance towards becoming a valuable prognostic and risk stratification tool; meanwhile, the combination of MRI and PET has also emerged, with the superior advantage of combining molecular imaging with substantial soft tissue contrast than that achieved using CT. With these new imaging systems, PET and MRI data are acquired simultaneously in a single scan, and the images are promptly co-registered, effectively reducing misalignment errors. More studies will confirm whether PET and MRI parameters are correlated or reveal different types of information.46,64 Nonetheless, technical developments in PET and hybrid PET systems will continually help our understanding of the pathophysiological factors contributing to AAA evolution.
Conclusions
Despite substantial advances in AAA screening and management over the years, AAA remains clinically significant. Management of patients with AAA is currently based on morphological characteristics derived from USS-based surveillance, including aortic size and growth rate. USS provides reliable anatomical data in this regard. However, the classical anatomy-centered approach to AAA imaging is insufficient to comprehensively assess rupture risk and factors that may result in complications associated with repair. Emerging radiotracers with PET can provide complementary functional information at the molecular level. [18F]FDG PET studies have yielded equivocal results, urging the introduction of more relevant radiotracers. Importantly, the strength of PET lies in its ability to elucidate the molecular evolution of AAA, which can inform the need for surgical intervention or response to pharmacological therapy. Despite the low number of preclinical studies, these are important for pilot evaluations of novel agents and improved characterization of existing radiotracers prior to their clinical translation. Finally, for clinical translation, the standardization of analysis methods and improvements in hybrid technology are warranted. Therefore, in patients with AAA, the road ahead for PET imaging is promising to facilitate assessments of functional aortic characteristics that may help distinguish patients with rupture-prone AAA requiring surgery from patients with low-risk AAA for whom a watchful waiting approach may be sufficient.
Abbreviations
- AAA:
-
Abdominal aortic aneurysm
- CT:
-
Computed tomography
- EVAR:
-
Endovascular aortic repair
- [18F]FDG:
-
[18F]fluorodeoxyglucose
- [18F]FLT:
-
[18F]fluorothymidine
- [18F]NaF:
-
[18F]-labeled sodium fluoride
- MRI:
-
Magnetic resonance imaging
- PET:
-
Positron emission tomography
- SoFIA3 :
-
Sodium fluoride imaging of AAA
- USS:
-
Ultrasound scanning
References
Blanchard JF, Armenian HK, Friesen PP. Risk factors for abdominal aortic aneurysm: Results of a case-control study. Am J Epidemiol. 2000;151:575–83.
National Institute for Health and Clinical Excellence. Abdominal aortic aneurysm: diagnosis and management. 2020. Available from: https://www.nice.org.uk/guidance/ng156.
Kumar Y, Hooda K, Li S, Goyal P, Gupta N, Adeb M. Abdominal aortic aneurysm: Pictorial review of common appearances and complications. Ann Transl Med. 2017;5:256.
Karthikesalingam A, Vidal-Diez A, Holt PJ, Loftus IM, Schermerhorn ML, Soden PA, et al. Thresholds for abdominal aortic aneurysm repair in England and the United States. N Engl J Med. 2016;375:2051–9.
Thompson RW, Geraghty PJ, Lee JK. Abdominal aortic aneurysms: Basic mechanisms and clinical implications. Curr Probl Surg. 2002;39:110–230.
Sakalihasan N, Michel JB, Katsargyris A, Kuivaniemi H, Defraigne JO, Nchimi A, et al. Abdominal aortic aneurysms. Nat Rev Dis Primers. 2018;4:34.
Patel K, Zafar MA, Ziganshin BA, Elefteriades JA. Diabetes mellitus: Is it protective against aneurysm? A narrative review. Cardiology. 2018;141:107–22.
Raffort J, Lareyre F, Clément M, Hassen-Khodja R, Chinetti G, Mallat Z. Diabetes and aortic aneurysm: Current state of the art. Cardiovasc Res. 2018;114:1702–13.
Davis M, Harris M, Earnshaw JJ. Implementation of the National Health Service abdominal aortic aneurysm screening program in England. J Vasc Surg. 2013;57:1440–5.
Guirguis-Blake JM, Beil TL, Senger CA, Whitlock EP. Ultrasonography screening for abdominal aortic aneurysms: A systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2014;160:321–9.
Johansson M, Hansson A, Brodersen J. Estimating overdiagnosis in screening for abdominal aortic aneurysm: Could a change in smoking habits and lowered aortic diameter tip the balance of screening towards harm? Br Med J. 2015;350:
Zarrouk M, Lundqvist A, Holst J, Troëng T, Gottsäter A. Cost-effectiveness of screening for abdominal aortic aneurysm in combination with medical intervention in patients with small aneurysms. Eur J Vasc Endovasc Surg. 2016;51:766–73.
Ashton HA, Buxton MJ, Day NE, Kim LG, Marteau TM, Scott RA, et al. The Multicentre Aneurysm Screening Study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: A randomised controlled trial. Lancet. 2002;360:1531–9.
Thompson SG, Ashton HA, Gao L, Buxton MJ, Scott RAP, Group obotMASS. Final follow-up of the Multicentre Aneurysm Screening Study (MASS) randomized trial of abdominal aortic aneurysm screening. Br J Surg. 2012;99:1649–56.
McGloughlin TM, Doyle BJ. New approaches to abdominal aortic aneurysm rupture risk assessment: Engineering insights with clinical gain. Arterioscler Thromb Vasc Biol. 2010;30:1687–94.
Kuivaniemi H, Ryer EJ, Elmore JR, Tromp G. Understanding the pathogenesis of abdominal aortic aneurysms. Expert Rev Cardiovasc Ther. 2015;13:975–87.
English SJ, Sastriques SE, Detering L, Sultan D, Luehmann H, Arif B, et al. CCR2 positron emission tomography for the assessment of abdominal aortic aneurysm inflammation and rupture prediction. Circ Cardiovasc Imaging. 2020;13:
Shi S, Orbay H, Yang Y, Graves SA, Nayak TR, Hong H, et al. PET imaging of abdominal aortic aneurysm with 64Cu-labeled anti-CD105 antibody Fab fragment. J Nucl Med. 2015;56:927–32.
Gandhi R, Cawthorne C, Craggs LJL, Wright JD, Domarkas J, He P, et al. Cell proliferation detected using [(18)F]FLT PET/CT as an early marker of abdominal aortic aneurysm. J Nucl Cardiol 2019; Online ahead of print.
Ailawadi G, Moehle CW, Pei H, Walton SP, Yang Z, Kron IL, et al. Smooth muscle phenotypic modulation is an early event in aortic aneurysms. J Thorac Cardiovasc Surg. 2009;138:1392–9.
Riches K, Angelini TG, Mudhar GS, Kaye J, Clark E, Bailey MA, et al. Exploring smooth muscle phenotype and function in a bioreactor model of abdominal aortic aneurysm. J Transl Med. 2013;11:208.
Riches K, Clark E, Helliwell RJ, Angelini TG, Hemmings KE, Bailey MA, et al. Progressive development of aberrant smooth muscle cell phenotype in abdominal aortic aneurysm disease. J Vasc Res. 2018;55:35–46.
Syed MBJ, Fletcher AJ, and Dweck MR. Imaging cellular activity and proliferation in the aortic wall. J Nucl Cardiol 2019; Online ahead of print.
Li Z, Zhao Z, Cai Z, Sun Y, Li L, Yao F, et al. Runx2 (runt-related transcription factor 2)-mediated microcalcification is a novel pathological characteristic and potential mediator of abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol. 2020;40:1352–69.
Nahrendorf M, Keliher E, Marinelli B, Leuschner F, Robbins CS, Gerszten RE, et al. Detection of macrophages in aortic aneurysms by nanoparticle positron emission tomography-computed tomography. Arterioscler Thromb Vasc Biol. 2011;31:750–7.
Dash A, Chakravarty R. Radionuclide generators: The prospect of availing PET radiotracers to meet current clinical needs and future research demands. Am J Nucl Med Mol Imaging. 2019;9:30–66.
Leenaars CHC, Kouwenaar C, Stafleu FR, Bleich A, Ritskes-Hoitinga M, De Vries RBM, et al. Animal to human translation: A systematic scoping review of reported concordance rates. J Transl Med. 2019;17:223.
Filardo G, Powell JT, Martinez MA, and Ballard DJ. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane DB Syst Rev 2015;Cd001835.
Patel R, Sweeting MJ, Powell JT, Greenhalgh RM. Endovascular versus open repair of abdominal aortic aneurysm in 15-years’ follow-up of the UK endovascular aneurysm repair trial 1 (EVAR trial 1): A randomised controlled trial. Lancet. 2016;388:2366–74.
Tarkin JM, Dweck MR, Evans NR, Takx RA, Brown AJ, Tawakol A, et al. Imaging atherosclerosis. Circ Res. 2016;118:750–69.
Zhao S, Kuge Y, Tsukamoto E, Mochizuki T, Kato T, Hikosaka K, et al. Fluorodeoxyglucose uptake and glucose transporter expression in experimental inflammatory lesions and malignant tumours: Effects of insulin and glucose loading. Nucl Med Commun. 2002;23:545–50.
Tarkin JM, Joshi FR, Rudd JHF. PET imaging of inflammation in atherosclerosis. Nat Rev Cardiol. 2014;11:443.
Suzuki H, Tamaki T, Nishio M, Nakata Y, Hanai N, Nishikawa D, et al. Total lesion glycolysis on FDG-PET/CT before salvage surgery predicts survival in laryngeal or pharyngeal cancer. Oncotarget. 2018;9:19115–22.
Lindeman JH, Rabelink TJ, van Bockel JH. Immunosuppression and the abdominal aortic aneurysm: Doctor Jekyll or Mister Hyde? Circulation. 2011;124:e463–5.
Wykrzykowska J, Lehman S, Williams G, Parker JA, Palmer MR, Varkey S, et al. Imaging of inflamed and vulnerable plaque in coronary arteries with 18F-FDG PET/CT in patients with suppression of myocardial uptake using a low-carbohydrate, high-fat preparation. J Nucl Med. 2009;50:563–8.
Folco EJ, Sheikine Y, Rocha VZ, Christen T, Shvartz E, Sukhova GK, et al. Hypoxia but not inflammation augments glucose uptake in human macrophages: Implications for imaging atherosclerosis with 18Fluorine-labeled 2-deoxy-D-glucose positron emission tomography. J Am Coll Cardiol. 2011;58:603–14.
Taqueti VR, Di Carli MF, Jerosch-Herold M, Sukhova GK, Murthy VL, Folco EJ, et al. Increased microvascularization and vessel permeability associate with active inflammation in human atheromata. Circ Cardiovasc Imaging. 2014;7:920–9.
Kotze CW, Groves AM, Menezes LJ, Harvey R, Endozo R, Kayani IA, et al. What is the relationship between (1)(8)F-FDG aortic aneurysm uptake on PET/CT and future growth rate? Eur J Nucl Med Mol Imaging. 2011;38:1493–9.
English SJ, Piert MR, Diaz JA, Gordon D, Ghosh A, D’Alecy LG, et al. Increased (18)F-FDG uptake is predictive of rupture in a novel rat abdominal aortic aneurysm rupture model. Ann Surg. 2015;261:395–404.
Huang Y, Teng Z, Elkhawad M, Tarkin JM, Joshi N, Boyle JR, et al. High structural stress and presence of intraluminal thrombus predict abdominal aortic aneurysm 18F-FDG uptake: Insights from biomechanics. Circ Cardiovasc Imaging. 2016;9:
Nie M-X, Zhang X-H, Yan Y-F, Zhao Q-M. Relationship between inflammation and progression of an abdominal aortic aneurysm in a rabbit model based on 18F-FDG PET/CT imaging. Vascular. 2018;26:571–80.
Courtois A, Nusgens BV, Hustinx R, Namur G, Gomez P, Somja J, et al. 18F-FDG uptake assessed by PET/CT in abdominal aortic aneurysms is associated with cellular and molecular alterations prefacing wall deterioration and rupture. J Nucl Med. 2013;54:1740–7.
Nchimi A, Cheramy-Bien JP, Gasser TC, Namur G, Gomez P, Seidel L, et al. Multifactorial relationship between 18F-fluoro-deoxy-glucose positron emission tomography signaling and biomechanical properties in unruptured aortic aneurysms. Circ Cardiovasc Imaging. 2014;7:82–91.
Barwick TD, Lyons OT, Mikhaeel NG, Waltham M, O’Doherty MJ. 18F-FDG PET-CT uptake is a feature of both normal diameter and aneurysmal aortic wall and is not related to aneurysm size. Eur J Nucl Med Mol Imaging. 2014;41:2310–8.
Tsuruda T, Nagamachi S, Nishimura M, Nakamura K, Kitamura K. Multiple 18F-fluorodeoxyglucose positron emission tomography scans showing progression of abdominal aortic aneurysm: A case report. Medicine (Baltimore). 2016;95:
Kuzniar M, Tegler G, Wanhainen A, Ahlstrom H, Mani K, Hansen T. Feasibility of assessing inflammation in asymptomatic abdominal aortic aneurysms with integrated 18F-fluorodeoxyglucose positron emission tomography/magnetic resonance imaging. Eur J Vasc Endovasc Surg. 2020;59:464–71.
Courtois A, Makrygiannis G, El Hachemi M, Hultgren R, Allaire E, Namur G, et al. Positron emission tomography/computed tomography predicts and detects complications after endovascular repair of abdominal aortic aneurysms. J Endovasc Ther. 2019;26:520–8.
Paraskevas KI, Tzovaras AA, Stathopoulos V, Gentimi F, Mikhailidis DP. Increased fluorodeoxyglucose uptake following endovascular abdominal aortic aneurysm repair: A predictor of endoleak? Open Cardiovasc Med J. 2010;4:117–9.
Marie PY, Plissonnier D, Bravetti S, Coscas R, Rouer M, Haulon S, et al. Low baseline and subsequent higher aortic abdominal aneurysm FDG uptake are associated with poor sac shrinkage post endovascular repair. Eur J Nucl Med Mol Imaging. 2018;45:549–57.
Forsythe RO, Dweck MR, McBride OMB, Vesey AT, Semple SI, Shah ASV, et al. (18)F-sodium fluoride uptake in abdominal aortic aneurysms: The SoFIA(3) study. J Am Coll Cardiol. 2018;71:513–23.
Akerele MI, Karakatsanis NA, Forsythe RO, Dweck MR, Syed M, Aykroyd RG, et al. Iterative reconstruction incorporating background correction improves quantification of [18F]-NaF PET/CT images of patients with abdominal aortic aneurysm. J Nucl Cardiol 2019;Online ahead of print.
Kitagawa T, Kosuge H, Chang E, James ML, Yamamoto T, Shen B, et al. Integrin-targeted molecular imaging of experimental abdominal aortic aneurysms by (18)F-labeled Arg-Gly-Asp positron-emission tomography. Circ Cardiovasc Imaging. 2013;6:950–6.
Tegler G, Estrada S, Hall H, Wanhainen A, Bjorck M, Sorensen J, et al. Autoradiography screening of potential positron emission tomography tracers for asymptomatic abdominal aortic aneurysms. Ups J Med Sci. 2014;119:229–35.
Ferda J, Baxa J, Ferdova E, Kucera R, Topolcan O, Molacek J. Abdominal aortic aneurysm in prostate cancer patients: the “road map” from incidental detection to advanced predictive, preventive, and personalized approach utilizing common follow-up for both pathologies. EPMA J. 2019;10:415–23.
Joshi NV, Elkhawad M, Forsythe RO, McBride OMB, Rajani NK, Tarkin JM, et al. Greater aortic inflammation and calcification in abdominal aortic aneurysmal disease than atherosclerosis: A prospective matched cohort study. Open Heart. 2020;7:
Folsom AR, Yao L, Alonso A, Lutsey PL, Missov E, Lederle FA, et al. Circulating biomarkers and abdominal aortic aneurysm incidence: The Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2015;132:578–85.
Salman HE, Ramazanli B, Yavuz MM, and Yalcin HC. Biomechanical investigation of disturbed hemodynamics-induced tissue degeneration in abdominal aortic aneurysms using computational and experimental techniques. Frontiers in Bioengineering and Biotechnology 2019;7:Online ahead of print.
Adams LC, Brangsch J, Reimann C, Kaufmann JO, Nowak K, Buchholz R, et al. Noninvasive imaging of vascular permeability to predict the risk of rupture in abdominal aortic aneurysms using an albumin-binding probe. Sci Rep. 2020;10:3231.
Deeg MA, Meijer CA, Chan LS, Shen L, Lindeman JH. Prognostic and predictive biomarkers of abdominal aortic aneurysm growth rate. Curr Med Res Opin. 2016;32:509–17.
Acosta S, Gottsäter A, Engström G, Melander O, Zarrouk M, Nilsson PM, et al. Circulating midregional proadrenomedullin and risk of incident abdominal aortic aneurysm: A prospective longitudinal cohort study. Angiology. 2018;69:333–8.
Aguiar P, Fernández-Ferreiro A, Galli F, Tsoumpas C. Imaging biomarkers in translational small animal models. Contrast Media Mol Imaging. 2019;2019:9469041.
Müller V, Miszczuk M, Althoff CE, Stroux A, Greiner A, Kuivaniemi H, et al. Comorbidities associated with large abdominal aortic aneurysms. Aorta. 2019;7:108–14.
Tsoumpas C, Visvikis D, Loudos G. Innovations in small-animal PET/MR imaging instrumentation. PET Clinics. 2016;11:105–18.
Molacek J, Baxa J, Opatrny V, Treska V, Hollan I, Ferda J. Benefits of hybrid methods (PET/CT, PET MRI) in the diagnosis of abdominal aortic pathology. Rozhl Chir. 2019;98:450–6.
English SJ, Diaz JA, Shao X, Gordon D, Bevard M, Su G, et al. Utility of (18) F-FDG and (11)C-PBR28 microPET for the assessment of rat aortic aneurysm inflammation. EJNMMI Res. 2014;4:20.
Nchimi A, Courtois A, El Hachemi M, Touat Z, Drion P, Withofs N, et al. Multimodality imaging assessment of the deleterious role of the intraluminal thrombus on the growth of abdominal aortic aneurysm in a rat model. Eur Radiol. 2016;26:2378–86.
Sarda-Mantel L, Alsac JM, Boisgard R, Hervatin F, Montravers F, Tavitian B, et al. Comparison of 18F-fluoro-deoxy-glucose, 18F-fluoro-methyl-choline, and 18F-DPA714 for positron-emission tomography imaging of leukocyte accumulation in the aortic wall of experimental abdominal aneurysms. J Vasc Surg. 2012;56:765–73.
Courtois A, Nusgens B, Garbacki N, Hustinx R, Gomez P, Defraigne JO, et al. Circulating microRNAs signature correlates with positive [(18)F]fluorodeoxyglucose-positron emission tomography in patients with abdominal aortic aneurysm. J Vasc Surg. 2018;67(585–95):
Kotze CW, Rudd JH, Ganeshan B, Menezes LJ, Brookes J, Agu O, et al. CT signal heterogeneity of abdominal aortic aneurysm as a possible predictive biomarker for expansion. Atherosclerosis. 2014;233:510–7.
Lee H, Paeng JC, Kim KH, Cheon GJ, Lee DS, Chung J-K, et al. Correlation of FDG PET/CT findings with long-term growth and clinical course of abdominal aortic aneurysm. Nucl Med Mol Imaging. 2018;52:46–52.
Maier A, Essler M, Gee MW, Eckstein HH, Wall WA, Reeps C. Correlation of biomechanics to tissue reaction in aortic aneurysms assessed by finite elements and [18F]-fluorodeoxyglucose-PET/CT. Int J Numer Method Biomed Eng. 2012;28:456–71.
Marini C, Morbelli S, Armonino R, Spinella G, Riondato M, Massollo M, et al. Direct relationship between cell density and FDG uptake in asymptomatic aortic aneurysm close to surgical threshold: An in vivo and in vitro study. Eur J Nucl Med Mol Imaging. 2012;39:91–101.
McBride OMB, Joshi NV, Robson JMJ, MacGillivray TJ, Gray CD, Fletcher AM, et al. Positron emission tomography and magnetic resonance imaging of cellular inflammation in patients with abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2016;51:518–26.
Morbelli S, Ghigliotti G, Spinella G, Marini C, Bossert I, Cimmino M, et al. Systemic vascular inflammation in abdominal aortic aneurysm patients: A contrast-enhanced PET/CT study. Q J Nucl Med Mol Imaging. 2014;58:299–309.
Morel O, Mandry D, Micard E, Kauffmann C, Lamiral Z, Verger A, et al. Evidence of cyclic changes in the metabolism of abdominal aortic aneurysms during growth phases: (1)(8)F-FDG PET sequential observational study. J Nucl Med. 2015;56:1030–5.
Murakami M, Morikage N, Samura M, Yamashita O, Suehiro K, Hamano K. Fluorine-18-fluorodeoxyglucose positron emission tomography–computed tomography for diagnosis of infected aortic aneurysms. Ann Vasc Surg. 2014;28:575–8.
Palombo D, Morbelli S, Spinella G, Pane B, Marini C, Rousas N, et al. A positron emission tomography/computed tomography (PET/CT) evaluation of asymptomatic abdominal aortic aneurysms: another point of view. Ann Vasc Surg. 2012;26:491–9.
Reeps C, Bundschuh RA, Pellisek J, Herz M, van Marwick S, Schwaiger M, et al. Quantitative assessment of glucose metabolism in the vessel wall of abdominal aortic aneurysms: Correlation with histology and role of partial volume correction. Int J Cardiovasc Imaging. 2013;29:505–12.
Tegler G, Ericson K, Sorensen J, Bjorck M, Wanhainen A. Inflammation in the walls of asymptomatic abdominal aortic aneurysms is not associated with increased metabolic activity detectable by 18-fluorodeoxglucose positron-emission tomography. J Vasc Surg. 2012;56:802–7.
Tegler G, Sorensen J, Ericson K, Bjorck M, Wanhainen A. 4D-PET/CT with [(11)C]-PK11195 and [(11)C]-(D)-deprenyl does not identify the chronic inflammation in asymptomatic abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2013;45:351–6.
Xu XY, Borghi A, Nchimi A, Leung J, Gomez P, Cheng Z, et al. High levels of 18F-FDG uptake in aortic aneurysm wall are associated with high wall stress. Eur J Vasc Endovasc Surg. 2010;39:295–301.
Funding
Gandhi R is funded by the Engineering and Physical Sciences Research Council. Bailey M and Bell M are funded by the British Heart Foundation. Tsoumpas C is funded by the Royal Society and the Engineering and Physical Sciences Research Council. This work was partially funded by the Academy of Medical Sciences (Clinical Lecturer Starter Grant to MB).
Disclosures
Gandhi R declares that she has no conflict of interest. Bell M declares that he has no conflict of interest. Bailey M declares that he has no conflict of interest. Tsoumpas C declares that he has no conflict of interest.
Author Contributions
RG wrote the manuscript and obtained funding; MB edited the manuscript and obtained funding; MB edited the manuscript, obtained funding, and provided intellectual input, overall responsibility for the study; and CT edited the manuscript and provided intellectual input, overall responsibility for the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
The authors have also provided an audio summary of the article, which is available to download as ESM, or to listen to via the JNC/ASNC Podcast.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gandhi, R., Bell, M., Bailey, M. et al. Prospect of positron emission tomography for abdominal aortic aneurysm risk stratification. J. Nucl. Cardiol. 28, 2272–2282 (2021). https://doi.org/10.1007/s12350-021-02616-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-021-02616-8