Abstract
Introduction
Duchenne muscular dystrophy (DMD) is characterized by rapid functional decline. Current available treatment options aim to delay disease progression or stabilize physical function. To aid in healthcare providers’ understanding of the symptoms of disease that impact patients’ experience, this study explored children’s physical functioning, activities of daily living (ADLs), and health-related quality of life (HRQoL) after receiving eteplirsen, a weekly infusion indicated for individuals with DMD with exon 51 skip-amenable mutations.
Methods
Fifteen caregivers of male individuals with DMD participated in a 60-min, semi-structured interview. Open-ended questioning explored changes in the children’s condition or maintenance in abilities since eteplirsen initiation.
Results
Children with DMD (age 7–15 years [mean 10.9]; steroid treatment at interview, n = 8; time since eteplirsen initiation 3–24 months [mean 14.9]) were described by caregivers as ambulatory (n = 9) and non-ambulatory (n = 6). Caregivers of ambulatory children reported improvements or maintenance of walking ability (n = 7/9), running (n = 6/9), and using stairs (n = 4/9). Continued decline in using stairs was reported by two caregivers. In upper-limb functioning, improvements or maintenances in fine-motor movements were reported by nearly half of all caregivers (n = 7/15), with one caregiver noting a continued decline. Subsequent improvements or maintenances in ADLs were described. Improvements or maintenances in fatigue (n = 9/15), muscle weakness (n = 7/15), and pain (n = 6/15) were reported, although some caregivers described a continued decline (n = 3/15 fatigue, n = 1/15 muscle weakness, n = 2/15 pain). Importantly, most caregivers who reported maintenances in ability perceived this as a positive outcome (n = 6/9).
Conclusion
This exploratory study indicated that most caregivers perceived improvements or maintenances in aspects of their child’s physical functioning, ADLs, and HRQoL since eteplirsen initiation, which they perceived to be a positive outcome.
Plain Language Summary
Duchenne muscular dystrophy (DMD) is a rare disease characterized by progressive muscle weakness. Early on, this weakness presents as difficulty walking, but eventually children lose the ability to walk, develop spinal curvature, and experience problems with the heart and lung muscles. People with DMD are missing a key protein in their bodies called dystrophin. Eteplirsen is a weekly, intravenous treatment approved to treat people with a specific DMD genetic misspelling. The goal of the treatment is to slow down the disease and delay the time to losing ability to walk or needing help breathing. Fifteen caregivers of children living with DMD participated in a 60-min telephone interview. Caregivers were asked questions about the child’s DMD symptoms and how those symptoms impact the child’s daily life. Caregivers discussed their child’s experience while receiving eteplirsen treatment and changes since the start of treatment. Caregivers described their child’s muscle weakness and how this has affected their movements (e.g., using stairs, running or walking). Since starting eteplirsen treatment, all caregivers reported some improvement or maintenance in parts of their child’s physical functioning, activities of daily living (e.g., sports/leisure, getting dressed and self-care), and symptoms (e.g., muscle weakness, pain and fatigue), even though some decline was also reported (e.g., physical functioning, getting dressed, self-care, muscle weakness, pain and fatigue). The results provide insights into physical functioning and quality of life of children with DMD who are receiving eteplirsen. However, more research is needed to fully understand the impact of eteplirsen on these experiences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Patients with Duchenne muscular dystrophy (DMD) suffer progressive and irreversible muscle damage which has a substantial impact on physical functioning, daily and social activities, emotional well-being, and caregiver burden. |
Novel therapies such as gene therapy and exon skipping that address the disease-causing mutations in the gene that codes for dystrophin have only relatively recently become available and there are limited qualitative insights of their impact on patients’ experience of disease. |
This study sought to further explore caregiver perceptions of DMD, identify the key symptoms of disease that impact the patients’ experience, and understand the changes that children treated with eteplirsen experience, as described by their caregivers. |
What was learned from the study? |
Since eteplirsen initiation, most caregivers perceived improvements or maintenances in aspects of their child’s physical functioning, activities of daily living, and of health-related quality of life to be a positive outcome. |
This study provides a comprehensive picture of caregivers’ experience living with ambulatory and non-ambulatory children with DMD with exon 51 skip-amenable mutations before and after treatment with eteplirsen. |
Introduction
Duchenne muscular dystrophy (DMD) is a rare, debilitating neuromuscular disease characterized by a lack of functional dystrophin protein production in the body, causing muscle deterioration [1]. Without treatment, progressive and irreversible muscle damage leads to loss of ambulation, usually by the age of 10–11 years, followed by muscle weakness in the arms and trunk, respiratory impairment (requiring ventilatory support), and cardiac dysfunction leading to death in the mid to late twenties [2,3,4].
Qualitative studies have shown that children with DMD experience muscle weakness, fatigue, and pain and have highlighted the substantial impact of declining motor function on physical functioning, daily and social activities, emotional well-being, and caregiver burden or perceived burden on others [5,6,7,8,9]. In previous studies, caregivers have described that overall care for a child with nonsense mutations on the DMD gene (nmDMD) impacts their physical and emotional well-being [8]. When considering treatment goals for debilitating neuromuscular diseases, delaying disease progression and stabilizing physical functions is essential. Maintenance or stabilization of current ability has been shown to be an important outcome for children with DMD, especially from the perspective of caregivers of ambulatory children [6, 7].
Current dystrophin restoration therapies approved by the US Food and Drug Administration (FDA) include phosphorodiamidate morpholino oligomers (PMOs [eteplirsen, golodirsen, viltolarsen, casimersen]) [10,11,12,13] and a gene transfer therapy (delandistrogene moxeparvovec) [14]. A dissociative steroidal anti-inflammatory drug (vamorolone) and a histone deacetylase (HDAC) inhibitor (givinostat) have also received FDA approval [15, 16]. These few approved pharmacological treatments only became available relatively recently, and consequently there are limited qualitative insights into individuals’ experience of these treatments. Previous studies have explored the patient and caregiver experience of the relationship between symptoms, impacts, and challenges in individuals with DMD [8, 9]; however, treatment perceptions and expectations may continue to change over time as the treatment landscape evolves.
Eteplirsen is indicated for individuals with DMD with exon 51 skip-amenable mutations, which account for approximately 13% of all those diagnosed with DMD [10, 17]. Eteplirsen is administered intravenously at weekly intervals. In phase 2 interventional studies, eteplirsen was shown to increase dystrophin expression in individuals with DMD, contribute to maintenance of ambulatory ability, and, when compared with natural history data, demonstrate a slower deterioration in pulmonary function [18,19,20,21]. A larger phase 3, multicenter, open-label study (PROMOVI) corroborated these findings and showed that eteplirsen had a positive treatment effect and a favorable safety profile and slowed disease progression when compared with natural history data [22], including a notable attenuation of decline on the 6-min walk test over 96 weeks and percent predicted forced vital capacity annual decline. Among additional longitudinal studies and post hoc analyses comparing data from eteplirsen-treated patients enrolled in clinical trials with natural history data, eteplirsen was associated with significantly longer median time to/age at loss of ambulation and significantly attenuated rates of pulmonary decline [23,24,25,26]. Median age at loss of ambulation for eteplirsen-treated patients from a phase 4 study (EVOLVE) was also consistent with these results [27]. Additional data suggest eteplirsen may prolong survival and reduce rates of multiple healthcare resource utilization measures, including need for pulmonary management and assisted ventilation [28, 29].
This qualitative interview study sought to (a) further explore caregiver perceptions of DMD and identify the key symptoms of disease that impact the patients’ experience (e.g., physical functioning, activities of daily living (ADL), and other aspects of health-related quality of life [HRQoL]) and (b) document the changes that children treated with eteplirsen experience, as described by their caregivers. Informing of caregivers’ experiences will likely help healthcare providers to better understand the symptoms of disease that impact patients’ experience during treatment. As a result of age, disease status, and the potential intellectual disability and neurobehavioral comorbidities associated with DMD, it is not reasonable or appropriate to expect children with DMD to self-report on changes in their physical functioning and ADLs; therefore, caregiver interviews were utilized to provide insights that may have otherwise been difficult to obtain.
Methods
Study Design and Participants
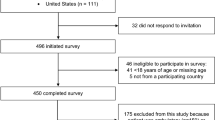
This study involved the conduct of qualitative, concept elicitation interviews with caregivers of children with DMD who had received eteplirsen treatment. All caregivers and their children resided in the USA. The study was reviewed and approved by New England Independent Review Board (NEIRB [now part of WCG-IRB] number 20203393) and was performed in line with the principles of the Declaration of Helsinki. A convenience sample of participants were recruited through SareptAssist, a patient support program founded by Sarepta Therapeutics, Inc., for individuals in the USA seeking treatment or currently being treated with eteplirsen (or other Sarepta treatments). An initial total of 54 eligible patients were identified. The study was described to eligible participants by members of the SareptAssist team; if interested, participants were then provided with an informed consent form. The consent form stated that any published findings would not allow for identification of the caregiver; all verbatim quotes include only the patients’ age and ambulatory status.
Efforts were made to recruit a diverse and representative sample of patients with DMD with different levels of ambulation; however, demographic sampling quotas (e.g., race/ethnicity, age, caregiver gender) were not possible to implement within the convenience sample. Caregivers were informed that their participation (or choice to not participate) in the study would in no way affect their child’s treatment, support, or engagement with the SareptAssist program.
Caregivers were eligible to participate if they were ≥ 18 years old and the primary caregiver of a male aged ≥ 7 years with a confirmed diagnosis of DMD amenable to exon 51 skipping. Caregivers had to agree that they had the linguistic, cognitive, and physical capability to participate in an interview and had to be willing and able to provide written informed consent to participate. Their child must have started taking eteplirsen 3–24 months prior to recruitment and have been receiving treatment at the time of the interview; this timeframe was selected to allow caregivers to adequately recall their child’s experience pre-treatment. Diagnosis and treatment were confirmed by the SareptAssist team via their existing records of eteplirsen treatment history or evidenced by an eteplirsen prescription or signed doctor’s note. Ambulatory status at eteplirsen treatment initiation was confirmed by SareptAssist; however, ambulatory stage at screening/interview relied on caregiver interpretation. Caregivers were provided with the following brief, plain-language descriptions of the ambulatory stages as part of a demographic screener: early ambulatory (can walk and rise independently); late ambulatory (can walk but has lost the ability to rise); early non-ambulatory (loss of ability to walk but is not on ventilation); late non-ambulatory (loss of ability to walk and is on ventilation). Although the study took a convenience sampling approach, ambulatory status at screening/interview was collected and used to stratify children during analysis to compare any notable differences in the experience of DMD.
Interview Process and Content
Interviews were 60-min long and conducted by the Clarivate research team via audio-conferencing using a semi-structured interview guide comprising open-ended, concept elicitation questions. The interview guide was informed by published qualitative literature, including conceptual models in DMD [30, 31], and utilized concept elicitation techniques [30,31,32]. Notably, questions relating to non-ambulatory impacts were not presented to caregivers of ambulatory children to avoid upset.
To aid concept elicitation, participants were shown or asked to visualize a timeline of a 6-month period before eteplirsen initiation, and then from eteplirsen initiation to the time of the interview, with the discussion structured into the following sections:
-
Symptoms and impacts before taking eteplirsen: Questions such as “can you describe how DMD impacted your child in the 6 months before they started taking eteplirsen?” were used to elicit spontaneous reports of the patient experience before eteplirsen treatment.
-
Patient experience during eteplirsen treatment: Questions were used to explore the patient experience of DMD after receiving eteplirsen treatment and the impact of treatment on symptoms, physical function, ADLs, and aspects of their child’s HRQoL. Specific probes were asked depending on whether the primary caregiver reported that there was some improvement, no change/maintenance, or a continued decline in their child’s DMD symptoms. There was not a formal definition of the term “improvement.” The improvement code was applied in any instances where a caregiver reported that a symptom or impact of DMD had improved.
Analysis
Anonymized transcripts were analyzed with coding techniques/structure based in the principles of semantic, directed content analysis, using Atlas.ti software (Version 7). Each transcript was analyzed by a researcher following a stepwise process of (1) immersion in the study, (2) coding, (3) iterative review of codes, (4) defining and refining concepts, and (5) reporting.
Data relating to the symptoms and impacts experienced before eteplirsen treatment were summarized in a thematic map, which was reviewed and corroborated by DMD experts. Data relating to patient experience with eteplirsen were assessed and reported in terms of concept frequency (i.e., the number of caregivers who described each change). Verbatim comments illustrate the themes, but any identifiable data have been removed.
Results
Sample Characteristics
Fifteen primary caregivers of children with DMD participated in the study (Table 1). Thirteen interviews were conducted in US English and two in US Spanish.
Child clinical and demographic characteristics are shown in Table 2. All children were male (mean age 10.9 years; range 7–15 years) and had received eteplirsen for an average of 14.9 months (range 3–24 months; Fig. 1). Some used a wheelchair all the time (n = 5/15; 33.3%) or sometimes (n = 3/15; 20%). One child (n = 1/15; 6.7%) required assisted ventilation at night. Around half (ambulatory, n = 3; non-ambulatory, n = 5) were receiving steroid treatment (prednisone and/or deflazacort) at the time of their interview.
Relationship between time on eteplirsen treatment (months) and patient age at treatment initiation (years). *The age at treatment initiation starts at 5 years old. Although children with DMD were only eligible for the interview study if aged ≥ 7 years, they may have been receiving eteplirsen for 3–24 months prior
At treatment initiation, eight children (n = 8/15; 53.3%) were early ambulatory. Most of them were still early ambulatory at screening/interview (n = 6/8; 75%); however, one child had progressed to late ambulatory (time since eteplirsen initiation 12 months) and one child had progressed to early non-ambulatory (time since eteplirsen initiation 24 months). Of the three children who were late ambulatory at treatment initiation, one child had progressed to early non-ambulatory (time since eteplirsen initiation 12 months). The four children who were early non-ambulatory at treatment initiation remained at this ambulation stage at screening/interview. It should be noted that ambulatory status at screening/interview was based entirely on caregiver observations and reported according to fixed definitions on the demographic screener, and therefore may have been subject to reporting errors. Changes in ambulatory status from treatment initiation to interview screening are shown in Fig. 2.
Changes in ambulatory status from treatment initiation to interview screening. †Data confirmed by SareptAssist clinical records; At interview screening, caregivers were provided with the following brief, plain-language descriptions of the ambulatory stages as part of a demographic screener: early ambulatory (can walk and rise independently); late ambulatory (can walk but has lost the ability to rise); early non-ambulatory (loss of ability to walk but is not on ventilation); late non-ambulatory (loss of ability to walk and is on ventilation)
Symptoms and Impacts Before Taking Eteplirsen
For the first portion of the interview, participants were asked to consider their child’s life with DMD 6 months prior to eteplirsen initiation to gain insights into the symptoms and impact of DMD on patient experience. The analysis focused on identifying key symptoms and thematic areas of impact from DMD; the thematic map is shown in Fig. 3. Quotes supporting the concepts identified are presented in Supplementary Material 1.
As interviews were semi-structured, not all questions were asked to all participants, and therefore counts may not always equate to the total sample size.
Physical functioning
Caregivers of children who were ambulatory at the time of interview (n = 9/15) reported impacts to their child’s physical functioning of the lower limbs, including using stairs (n = 8/9), difficulty running (n = 7/9) and walking (n = 6/9).
“He obviously couldn’t run like a normal kid […] he could kind of run, […], but it was definitely not a normal run, and he couldn’t run for very long.” (Caregiver of an ambulatory 13-year-old)
“Stairs were an issue, he had to […] pull himself up. He would go one at a time. He would step up with his right leg and push himself up and do that with every single step.” (Caregiver of an ambulatory 7-year-old)
Caregivers of children who were non-ambulatory at the time of their interview (n = 6/15) described limitations in upper limb functioning, including reaching above the head (n = 4/6) and hand grip (n = 2/6).
“He can’t lift his arms high […] it’s too difficult to reach his head.” (Caregiver of a non-ambulatory 13-year-old)
“He can grip some stuff, but he wouldn’t be able to, like, take a lid off of […] a cup or […] a jar.” (Caregiver of a non-ambulatory 13-year-old)
Physical functioning was also reported to be impacted by DMD in other physical impacts, including difficulty with movements requiring core strength, e.g., getting up from the floor/seated, bending down, and balancing.
“He just was not able to get up, and that was the biggest sign, and that’s why we took him to the doctor in the first place, because he was doing what you call Gower sign, which is the beginning […] of muscular dystrophy.” (Caregiver of an ambulatory 7-year-old)
Activities of Daily Living (ADLs)
Impacts to ADLs were reported in ambulatory and non-ambulatory children, including sports/leisure/play activities involving the upper and lower limbs (n = 13/15 and n = 8/15 respectively), getting dressed (n = 12/15), and washing/bathing (n = 11/15).
“He couldn’t really do any of the things that his friends do, […], or that his dad does […] he mostly just did schoolwork and video games, he didn’t really do, like, outdoor activities that he wanted to […] like sporting events, school events, um, hunting, farming, bike riding.” (Caregiver of an ambulatory 13-year-old)
“Shoes is the biggest thing that he can’t do. But, like, putting on a shirt, pants, um, he can’t have anything with, like, buckles […] He can’t, he can’t button pants.” (Caregiver of an ambulatory 11-year-old)
Activities related to school (e.g., difficulty writing, difficulty participating in physical education, and difficulty interacting with children in class) and home (e.g., difficulty toileting, difficulty using utensils, and difficulty tidying) were also affected.
“Writing, he had a big difficulty with. He’s doing better now, but […], he had a, err, big difficulty with trying to figure out what hand he uses to write.” (Caregiver of an ambulatory 8-year-old)
“If I told him to […] make his bed […] it took him forever to put his sheet on, and then I didn’t understand why it was so hard for him to put his sheet on his bed.” (Caregiver of a non-ambulatory 11-year-old)
Signs and Symptoms of DMD
Pain (n = 14/15) and fatigue (n = 12/15) were frequently described as impacting children, which further limited physical functioning and ADLs.
“He, […], [experiences] a lot of back pain, I was told because of the way […] that he walked because of his muscle weakness was, like, grating the bone in his back, so that’s why his back would hurt.” (Caregiver of a non-ambulatory 11-year-old)
Other Aspects of HRQoL
Other impacts on HRQoL included impaired emotional well-being and cognitive-behavioral functioning. Caregivers described difficulties with concentrating (n = 7/15), reading (n = 6/15), learning information (n = 3/15), and speech (n = 2/15).
“He had some difficulty with speech and reading, […], which obviously I can’t say was DMD or not […] it seemed like it was.” (Caregiver of an ambulatory 13-year-old)
Additionally, caregivers reported that their child generally felt upset (n = 9/15), angry (n = 6/15), and/or frustrated (n = 5/15) about DMD and its impact on their life.
“I feel like he would get frustrated a lot, […], not being able to keep up with his friends […] not being able to do the things that he used to be able to do.” (Caregiver of an ambulatory 7-year-old)
Caregivers perceived that impaired emotional well-being and cognitive-behavioral functioning further affected their child’s ADLs:
“He is very impulsive, and struggles to sit still and concentrate and focus […] and so he would often be very distracted.” (Caregiver of an ambulatory 7-year-old)
Patient Experience During Eteplirsen Treatment
The next portion of the interview focused on children’s experience with eteplirsen treatment. A summary of the findings is provided in Table 3.
Caregivers were advised to consider aspects of their child’s physical functioning, ADLs, and/or HRQoL that may have improved, stayed the same, or declined from treatment initiation to the time of the interview (Fig. 4).
In total, seven caregivers reported at least one aspect of their child’s condition that had continued to decline (n = 5/7 received steroids at screening; time on eteplirsen 12–24 months). Importantly, caregivers were not asked to attribute the changes to any factor (e.g., treatment, DMD progression, external factors) as the reports were entirely based on their own observations and subjective opinion. Quotes supporting the concepts identified in the qualitative interviews are presented in Supplementary Material 2.
Physical Functioning
Walking was reported to have improved or been maintained since eteplirsen initiation by most caregivers with ambulatory children (n = 7/9), and, notably, no caregivers of children who were still ambulatory at the time of screening reported a continued decline. Some improvement or maintenance in ability was also reported in running (n = 6/9) and using stairs (n = 4/9) by caregivers of ambulatory children.
“He’s walking a further distance […] we were using the wheelchair when he got tired. Now he’s not using the wheelchair.” (Caregiver of an ambulatory 8-year-old)
“It seems like he just keeps on running faster and faster […] within the first week he started running faster.” (Caregiver of an ambulatory 7-year-old)
When considering upper limb movements, some improvement or maintenance of ability in fine motor movements (n = 7/15, 3 of whom were non-ambulatory at interview) were reported by nearly half of all caregivers; one caregiver (non-ambulatory) reported a continued decline (Fig. 4).
“You know the twist-top soda bottles, he used to not […] do that on his own […] he can’t always, but there has been a couple of times where he has been able to do that on his own and he wasn’t able to before.” (Caregiver of an ambulatory 13-year-old).
Ability of Daily Living (ADLs)
Some improvements or maintenance in ability in relation to ADLs were reported in the total sample (Fig. 5).
“He wasn’t able to, […] lift his legs when he, when he’s sitting down, and now he’s able to do all of that. […] he’s a little stronger now.” (Caregiver of a non-ambulatory, 15-year-old).
Signs and Symptoms of DMD
Caregivers reported some improvement or maintenance in their child’s level of fatigue (n = 9/15), muscle weakness (n = 7/15), and pain (n = 6/15) or continued decline in fatigue (n = 3/15), muscle weakness (n = 1/15), and pain (n = 2/15), as presented in Fig. 5.
“He’s able to, kind of, get through a full school day, and then we’re able to do things, […] after school […] before even the end of the school day, he was, like, done, didn’t want to do anything.” (Caregiver of an ambulatory 13-year-old).
Other Aspects of HRQoL
Some improvement or maintenance of cognitive-behavioral ability and of emotional well-being were reported in the total sample (Fig. 6). While some improvement was perceived in cognitive ability (e.g., concentration, reading ability, and learning ability), emotional wellness such as feeling upset or angry/frustrated by DMD remained unchanged.
“I would say even his ability to concentrate [laughs] has improved.” (Caregiver of an ambulatory 7-year-old)
Overall Experience of Changes During Eteplirsen Treatment
When asked about the timing of improvements or stabilization in their child’s abilities, caregivers stated that they first perceived some improvements between 1 and 12 months following eteplirsen initiation. Notably, improvements in lower limb functioning typically appeared sooner (within 1–3 months) than improvements in upper limb functioning (≥ 3 months).
Most caregivers perceived a maintenance of abilities as a positive outcome (n = 6/9); one caregiver did not (n = 1/9). Two found it hard to comment on whether maintenance was a positive or negative outcome (n = 2/9), as ultimately their child’s ability had not changed.
“Interviewer: And do you consider the fact that his abilities have stayed the same to be a positive outcome?” “Yeah, I–I’d say so […] some kids can’t, can’t walk, but he still can. He’s able to use his hands. He’s, he’s able to get up […] I’d say that that’s a good thing [laughs].” (Caregiver of an ambulatory 14-year-old).
“Well, yeah […] there’s no change, he’s still positive, he still does schoolwork, he still participates in anything the teachers ask him to participate.” (Caregiver of a non-ambulatory, 15-year-old).
Discussion
This study highlighted the considerable burden of DMD on children’s physical functioning, ADLs, and other aspects of HRQoL, as perceived by caregivers. The findings provide a comprehensive picture of caregivers’ experience living with ambulatory and nonambulatory children with DMD with exon 51 skip-amenable mutations. This study adds to the existing body of qualitative literature [5,6,7,8,9] reporting the patient experience in DMD holistically from a caregiver perspective. The symptoms and impacts of DMD reported by caregivers largely corroborated published conceptual models [8, 33] and conceptual frameworks identifying impacted HRQoL concepts in young people with DMD [5].
Most caregivers interviewed reported some improvements or maintenances in their child’s ability since eteplirsen initiation, particularly in terms of physical functioning ability and ADLs. Walking was reported to have improved or been maintained by most caregivers of ambulatory children, while fine motor movements were reported to have improved or been maintained by almost half of the caregivers. Other research has suggested that there is a moderate correlation between participation in physical and/or social activities and functional tests (e.g., 10 m walk/run and time to walk up four stairs), which highlights the benefit of improved or maintained walking ability in individuals with DMD [34]. It is important to note that some caregivers reported continued decline in some aspects of their child’s condition [physical functioning, ADLs, and symptoms (e.g., muscle weakness, pain, and fatigue)]. Additionally, two children in this study appeared to have progressed to early non-ambulatory DMD from the period prior to treatment to the time of their interview. Studies of eteplirsen enrolling individuals at a more advanced disease stage at baseline have similarly seen children lose ambulation while being treated [21]. This highlights the importance of early treatment intervention in preserving muscle function. Most caregivers who were asked, confirmed that a maintenance or stabilization of ability would be a positive outcome, a sentiment shared by caregivers in other qualitative studies evaluating DMD treatment expectations [6, 7]. Some improvements and maintenance of other aspects of HRQoL (e.g., cognitive-behavioral ability and emotional well-being) were reported to a lesser extent by caregivers, which may be due to the subjective nature and difficulty in observing these concepts.
Limitations of this exploratory study include the small number of caregivers of children with DMD in the USA amenable to exon 51 skipping who participated (with no comparison group), albeit the overall sample size and lack of a comparison group is consistent with other qualitative studies in rare disease, and specifically DMD [7, 8, 33]. All participants in this study were recruited via SareptAssist, in order to identify participants who met the eligibility criteria of “taking eteplirsen 3–24 months prior to recruitment and have been receiving treatment at the time of the interview”. Although the sponsor of SareptAssist was not involved in the conduct or analysis of the qualitative interviews, the possibility cannot be ruled out that their involvement in the SareptAssist program may have introduced bias into their responses. Participation in the interview study was not mandatory for any individuals receiving eteplirsen, and caregivers were informed that the interview study was being conducted by another company and that their participation (or decision not to participate) would not affect their child’s treatment or subsequent interactions with SareptAssist.
The concepts identified in this study and summarized in the thematic map were reviewed and confirmed by experts in DMD; however, it is important to note that the results may not be entirely generalizable. Impacts relating to late non-ambulatory DMD could not be fully explored as no caregivers of late non-ambulatory children were recruited. This may explain the limited coverage and descriptions of impacts relating to respiratory functioning (e.g., use of ventilation and the associated impacts) [5]. It is important to continue to explore the patient experience of DMD as treatment perceptions and expectations may continue to change as the treatment landscape evolves.
Furthermore, the study relied on proxy reporting of the lived experience of DMD. Caregivers may be the closest witness of day-to-day changes experienced by patients; however, caregivers are not clinical experts and thus can only qualitatively describe perceived changes in their child’s abilities and potential progression to a more severe health state. It is acknowledged that it is not possible for caregivers to know how their child’s condition may have progressed without treatment, and the findings from this study are not intended as a comparison. Furthermore, in qualitative research, there is no formal threshold or analysis to assess the magnitude of the improvements described by caregivers. Improvement thresholds are typically determined quantitatively, with qualitative insights generated to provide additional context [35]. Additionally, the study was retrospective and relied on caregiver recall. With these considerations, confirmation bias cannot be ruled out [36]. As a result of the age and disease status of the children living with DMD, and because of the frequently associated central nervous system involvement, which includes intellectual disability and neurobehavioral comorbidities, it is not reasonable or appropriate to expect children to self-report on changes in their physical functioning and ADLs; therefore, caregiver interviews helped to provide insights that may have otherwise been difficult to obtain. The accuracy of patient reporting in DMD may be questioned as cognitive challenges may be experienced.
Overall, this study provides preliminary qualitative insights into the potential impact since starting eteplirsen on aspects of physical functioning and HRQoL from the caregiver perspective. Future research should explore this further using longitudinal study designs and clinical outcome assessment (COA) measures to quantify the longitudinal improvements, stabilizations or worsening in children’s functioning and well-being (allowing for potential comparisons with natural history data in DMD). As a result of the self-reporting constraints in this population, future studies using COAs are likely to require observer-reported outcomes, performance tests, and/or clinician-reported outcomes. Another topic for future exploration could be the patient and caregiver experience of eteplirsen administration to understand current convenience/burden of weekly intravenous treatments.
Conclusion
This exploratory study highlighted the patient experience of DMD from a caregiver perspective. The findings indicated that since eteplirsen initiation, most caregivers perceived some improvement or maintenance in some aspects of physical functioning, ADLs, and symptoms (e.g., muscle weakness, pain, and fatigue). This information can benefit healthcare providers by informing them of caregivers’ experiences to better understand the symptoms of disease that impact the patient experience during treatment.
Data Availability
To protect participant confidentiality, the data set for this study cannot be shared.
References
Ryder S, Leadley R, Armstrong N, et al. The burden, epidemiology, costs and treatment for Duchenne muscular dystrophy: an evidence review. Orphanet J Rare Dis. 2017;12:1–21.
Broomfield J, Hill M, Guglieri M, Crowther M, Abrams K. Life expectancy in Duchenne muscular dystrophy: reproduced individual patient data meta-analysis. Neurology. 2021;97:e2304–14.
Bach JR, Martinez D, Saulat B. Duchenne muscular dystrophy: the effect of glucocorticoids on ventilator use and ambulation. Am J Phys Med. 2010;89:620–4.
Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol. 2018;17:251–67.
Powell PA, Carlton J. A comprehensive qualitative framework for health-related quality of life in Duchenne muscular dystrophy. Qual Life Res. 2023;32:1–12.
Brown V, Merikle E, Johnston K, Audhya I, Gooch K, Lowes L. A qualitative study to understand the Duchenne muscular dystrophy experience from the caregiver/patient perspective. Presented at the MDA Clinical & Scientific Conference; March 16–18, 2022; Nashville.
Staunton H, Trennery C, Arbuckle R, et al. Development of a Clinical Global Impression of Change (CGI-C) and a Caregiver Global Impression of Change (CaGI-C) measure for ambulant individuals with Duchenne muscular dystrophy. Health Qual Life Outcomes. 2021;19:1–16.
Williams K, Davidson I, Rance M, Buesch K, Acaster S. A qualitative study on the impact of caring for an ambulatory individual with nonsense mutation Duchenne muscular dystrophy. J Patient Rep Outcomes. 2021;5:1–12.
Williams K, Davidson I, Rance M, Boehnke A, Buesch K, Acaster S. Symptoms and impacts of ambulatory nonsense mutation Duchenne muscular dystrophy: a qualitative study and the development of a patient-centred conceptual model. J Patient Rep Outcomes. 2021;5:75.
EXONDYS 51 (eteplirsen) injection. Last revised January 2022. Cambridge, MA: Sarepta Therapeutics, Inc.
VYONDYS 53 (golodirsen) injection. Last revised June 2024. Cambridge, MA: Sarepta Therapeutics, Inc.
VILTEPSO (viltolarsen) injection. Last revised March 2021. Paramus, NJ: NS Pharma, Inc.
AMONDYS 45 (casimersen) injection. Last revised March 2023. Cambridge, MA: Sarepta Therapeutics, Inc.
ELEVIDYS (delandistrogene moxeparvovec-rokl) suspension. Last revised October 2023. Cambridge, MA: Sarepta Therapeutics, Inc.
AGAMREE (vamorolone) oral suspension. Coral Gables, FL: Catalyst Pharmaceuticals, Inc.
DUVYZAT (givinostat) oral suspension. Revised March 2024. Madrid: Italfarmaco S.A.
Aartsma-Rus A, Fokkema I, Verschuuren J, et al. Theoretic applicability of antisense-mediated exon skipping for Duchenne muscular dystrophy mutations. Hum Mutat. 2009;30:293–9.
Kinane TB, Mayer OH, Duda PW, Lowes LP, Moody SL, Mendell JR. Long-term pulmonary function in Duchenne muscular dystrophy: comparison of eteplirsen-treated patients to natural history. J Neuromuscul Dis. 2018;5:47–58.
Mendell JR, Rodino-Klapac LR, Sahenk Z, et al. Eteplirsen for the treatment of Duchenne muscular dystrophy. Ann Neurol. 2013;74:637–47.
Charleston JS, Schnell FJ, Dworzak J, et al. Eteplirsen treatment for Duchenne muscular dystrophy: exon skipping and dystrophin production. Neurology. 2018;90:e2146–54.
Alfano LN, Charleston JS, Connolly AM, et al. Long-term treatment with eteplirsen in nonambulatory patients with Duchenne muscular dystrophy. Medicine (Baltimore). 2019;98: e15858.
McDonald CM, Shieh PB, Abdel-Hamid HZ, et al. Open-label evaluation of eteplirsen in patients with Duchenne muscular dystrophy amenable to exon 51 skipping: PROMOVI trial. J Neuromuscul Dis. 2021;8:989–1001.
Mendell JR, Goemans N, Lowes LP, et al. Longitudinal effect of eteplirsen versus historical control on ambulation in Duchenne muscular dystrophy. Ann Neurol. 2016;79:257–71.
Mitelman O, Abdel-Hamid HZ, Byrne BJ, et al. A combined prospective and retrospective comparison of long-term functional outcomes suggests delayed loss of ambulation and pulmonary decline with long-term eteplirsen treatment. J Neuromuscul Dis. 2022;9:39–52.
Iff J, Bungey G, Paine A, et al. Delay in Duchenne muscular dystrophy progression with eteplirsen: longer time to loss of ambulation versus standard of care. Neuropediatrics. 2021;52(P5):24.
Iff J, Gerrits C, Zhong Y, et al. Delays in pulmonary decline in eteplirsen-treated patients with Duchenne muscular dystrophy. Muscle Nerve. 2022;66:262–9.
Ricchetti-Masterson K, Santra S, Hornibrook S, et al., editors. Interim analysis of EVOLVE: a long-term observational study evaluating eteplirsen, golodirsen, or casimersen in routine clinical practice. 27th International Hybrid Annual Congress of the World Muscle Society; 2022; Halifax, Nova Scotia, Canada.
Iff J, Zhong Y, Tuttle E, Gupta D, Paul X, Henricson E. Real-world evidence of eteplirsen treatment effects in patients with Duchenne muscular dystrophy in the USA. J Comp Effect Res. 2023;12:e230086.
Iff J, Done N, Tuttle E, et al. Survival among patients receiving eteplirsen for up to 8 years for the treatment of Duchenne muscular dystrophy and contextualization with natural history controls. Muscle Nerve. 2024;70(1):60–70.
Williams K, Buesch K, Piglowska N, et al. PRO119 Symptoms and impacts of nonsense mutation Duchenne muscular dystrophy: a qualitative study and the development of a patient-centred conceptual model. Value Health. 2020;23:S711.
Williams K, Buesch K, Piglowska N, Acaster S. PRO136 Symptoms and impacts of nonsense mutation Duchenne muscular dystrophy at different stages of ambulation. Value Health. 2020;23:S714.
Powell PA, Carlton J, Rowen D, Brazier JE, Chandler F, Godfrey J. PRO130 Project HERCULES: Construction of a new preference-based measure of quality of life for Duchenne muscular dystrophy (DMD). Value Health. 2019;22:S865.
Williams K, Buesch K, Acaster S. Symptoms and impacts of nonsense mutation Duchenne muscular dystrophy at different stages of ambulation. Future Neurol. 2022;16:FNL55.
Bendixen RM, Lott DJ, Senesac C, Mathur S, Vandenborne K. Participation in daily life activities and its relationship to strength and functional measures in boys with Duchenne muscular dystrophy. Disabil Rehabil. 2014;36:1918–23.
Staunton H, Willgoss T, Nelsen L, et al. An overview of using qualitative techniques to explore and define estimates of clinically important change on clinical outcome assessments. J Patient-Report Outcomes. 2019;3:16.
McSweeney B. Fooling ourselves and others: confirmation bias and the trustworthiness of qualitative research–Part 1 (the threats). J Organ Change Manag. 2021;34:1063–75.
Acknowledgements
Medical Writing and Editorial Assistance
Editorial assistance in the preparation of this article was provided by Dr. Paraskevi Briassouli of Eloquent Scientific Services. Support for this assistance was funded by Sarepta Therapeutics, Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
Sarepta Therapeutics Inc. funded this study as well as the journal’s Rapid Service and Open Access fees associated with this publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: Joel Iff, Chloe Carmichael, Stephanie McKee, Helen Kitchen. Methodology: Joel Iff, Chloe Carmichael, Stephanie McKee, Ihor Sehinovych, Carolina Tesi-Rocha, Erik Henricson, Francesco Muntoni, Helen Kitchen. Formal analysis and investigation: Chloe Carmichael, Stephanie McKee, Helen Kitchen. Writing: original draft preparation: Chloe Carmichael, Helen Kitchen. Writing: review and editing: Joel Iff, Chloe Carmichael, Stephanie McKee, Ihor Sehinovych, Carolyn McNeill, Carolina Tesi-Rocha, Erik Henricson, Francesco Muntoni, Helen Kitchen.
Corresponding author
Ethics declarations
Conflict of Interest
Joel Iff, Ihor Sehinovych, and Carolyn McNeill are employees of Sarepta Therapeutics, Inc., and may hold stock/options. Chloe Carmichael, Stephanie McKee, and Helen Kitchen are employees and stockholders of Clarivate, a healthcare research company that provides consultancy to pharmaceutical companies, including Sarepta Therapeutics, Inc. Carolina Tesi-Rocha reports consulting fees (Avexis, Biogen, Sarepta Therapeutics, Inc., Novartis, NS Pharma) and is a site investigator for clinical trials: Avexis, Biogen, Cytokinetics, Genzyme, Pfizer, PTC Therapeutics, Roche, Sarepta Therapeutics, Inc., Scholar Rock, and Janssen. Erik Henricson has received consulting fees from Sarepta Therapeutics, Inc., Santhera Pharmaceuticals, Pfizer, Eprirum Bio, Capricor, Catabasis, Mallinkrodt, Bristol-Myers Squibb, PTC Therapeutics, PepGen, and GSK and has received speaker honoraria from Parent Project Muscular Dystrophy, Muscular Dystrophy Association, and ENMC. Francesco Muntoni has received consultant fees and speaker honoraria from Sarepta Therapeutics, Inc. He is a member of the Pfizer SAB and, relevant for DMD, has received consultancies from Dyne Therapeutics, Roche, and PTC Therapeutics.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. The study was reviewed and approved by New England Independent Review Board (NEIRB [now part of WCG-IRB] number 20203393).
Additional information
Prior Presentation: Data from this study has been presented at the International Society for Pharmacoeconomics and Outcomes Research Annual Meeting (Virtual ISPOR Europe), November 30–December 3, 2021; Academy of Managed Care & Specialty Pharmacy Annual Meeting, March 29–April 1, 2022, Chicago, IL, USA; Neuromuscular Study Group Annual Scientific Meeting, September 30–October 02, 2022, Stressa, Lake Maggiore, Italy.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Iff, J., Carmichael, C., McKee, S. et al. Eteplirsen Treatment for Duchenne Muscular Dystrophy: A Qualitative Patient Experience Study. Adv Ther 41, 3278–3298 (2024). https://doi.org/10.1007/s12325-024-02915-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-024-02915-9