Abstract
Introduction
Studies have reported health-related quality-of-life impacts of Duchenne muscular dystrophy (DMD); however, further research is needed to understand how those with DMD experience their condition and how psychosocial impacts evolve over time in response to disease progression. This qualitative study explores the social and emotional implications of key transitions, challenges and adaptations throughout the disease course from the perspective of patients and family caregivers.
Methods
Semi-structured interviews were conducted with men and boys with DMD, and/or their caregivers, in the USA. Thematic analysis was used to examine patterns in data collected across the interviews.
Results
Nineteen participants were included. Three major themes were identified: (1) barriers to participation are multifaceted; (2) an emotional journey shaped by ‘inevitable progression;' (3) family provides critical tangible and emotional support. This study illustrates that psychosocial impacts of DMD are shaped by knowledge of the condition’s natural history alongside other factors including the extent of social barriers, personal growth and adaptation, and family support.
Conclusions
Findings provide insight into the strength and resilience with which individuals and their families respond to daily challenges and major clinical milestones and highlight the relative importance of loss of upper limb function as a transition in DMD affecting health-related quality-of-life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Duchenne muscular dystrophy (DMD) is a neuromuscular disease primarily impacting males, characterized by progressive muscular degeneration from birth resulting in loss of ambulation (LOA) and upper limb function, pulmonary dysfunction, cardiomyopathy and early mortality |
While previous studies investigating the health-related quality-of-life impact and lived experience in DMD have been conducted, more in-depth qualitative investigations into the emotional and social implications of DMD are needed |
We asked patients and family caregivers what they consider to be the social and emotional implications of key disease transitions and what are the challenges and adaptations necessary throughout the disease course |
What was learned from the study? |
The study findings provide insight into the strength and resilience with which individuals and their families respond to daily challenges and major clinical milestones |
The findings highlight the relative importance of loss of upper limb function as a transition in DMD affecting health-related quality-of-life |
Introduction
Duchenne muscular dystrophy (DMD) is a rare neuromuscular condition caused by mutations in the gene encoding dystrophin, a structural protein of muscle cells [1, 2]. As an X-linked disease, DMD primarily impacts males. Symptom onset typically occurs in early childhood and is characterized by muscle weakness, gait abnormalities and delayed motor milestones [3, 4]. Progressive muscular degeneration in DMD results in loss of ambulation (LOA) and upper limb function, pulmonary dysfunction, cardiomyopathy and early mortality [3,4,5]. For some boys and young men, cognitive and behavioral comorbidities—including autism-spectrum disorder, attention-deficit hyperactivity disorder and obsessive-compulsive disorder—also contribute to their individual clinical courses [6].
The profound clinical impacts of DMD and its progression on affected individuals’ lives and resultant health-related quality-of-life (HRQoL) have been documented in numerous studies [7]. Many measures that are commonly used used to quantify impact, including the PedsQL and EQ-5D, for example, have been critiqued for their inadequacy in capturing the nuanced experiences of those living with DMD [7,8,9]. These critiques help highlight uncertainties as to which physical, social and emotional issues are of greatest concern to those affected and how these issues evolve throughout the DMD life course. Qualitative research—which focuses on the meanings people attach to experiences, the relationship among knowledge, experience and action, and the social factors that shape these processes [10]—can provide context to quantitative estimates of HRQoL and improve understanding of the lived experiences of those with DMD. These methods also provide an opportunity to examine HRQoL more comprehensively and to explore its relationship with disease progression, particularly in rare diseases for which available sample sizes for quantitative research can be small [11].
A recent systematic review identified 11 qualitative studies that investigated the lived experiences of men and boys with DMD that explored subjects of body powerlessness, identity, social challenges, emotional coping and approaching end of life [12]. Despite the existence of rich qualitative data, previous studies often focused on particular life stages—such as learning about one’s diagnosis [13], transitioning into adulthood [14,15,16,17,18] or end-of-life planning [19]—or addressed specific research questions related to issues such as perceptions of masculinity in DMD [14, 17, 20] or participation in research [21]. The authors of the systematic review called for more in-depth qualitative investigations into the emotional and social implications of DMD [12]. Although that review focused on patient perspectives, many HRQoL data in DMD are derived from caregiver reports [7, 22]. This is because the young age or cognitive and behavioral impairments affecting some boys and young men with DMD preclude their self-reporting [23, 24]. Incorporating the accounts of caregivers reporting on behalf of patients is therefore also important to capture experiences throughout all potential stages of health experienced by those with DMD. The present study aimed to contribute to this underexplored area by examining the psychosocial impacts of DMD, including patient and caregiver perspectives on the social and emotional implications of key transitions, challenges and adaptations throughout the disease course.
Methods
Study Design and Participants
Men and boys living with DMD, and/or their caregivers reporting on their behalf, were recruited through a patient recruitment agency (Global Perspectives). Eligible individuals were engaged using a combination of patient databases, physician referrals and social media. This approach was informed by previous studies, which have demonstrated that flexible recruiting strategies using a combination of methods for reaching participants, including online recruitment, are effective for engaging rare disease populations [25, 26].
In addition to a self- or caregiver-reported confirmed diagnosis of DMD, eligibility criteria included living in the US, fluency in English and the ability to provide informed consent. For minors < 7 years of age, caregivers were recruited because of the complex subject matter of the research. Minors 7 years of age or older were deemed able to participate if they provided assent, with the informed consent of a parent or guardian. An effort was made to recruit a sample that included a range of DMD patient ages and clinical stages and both patient and caregiver respondents.
The present study is a secondary analysis of research initially conducted to develop vignettes describing the clinical progression of DMD, with the objective of eliciting utility values for DMD health states for use in economic models [27]. Individuals with cognitive or behavioural disorders that substantially impacted social interaction were excluded from this analysis to gain a clear picture of the social and emotional implications of DMD in the absence of potentially confounding comorbidities. Individuals with autism spectrum disorders, obsessive-compulsive disorder or selective mutism were excluded because of the findings of the previous analysis, which suggested that individuals with these disorders experience different social barriers, and caregiver respondents may have limited insight into their emotional experiences. Individuals with conditions such as mild language delays or attention deficit disorders were not excluded from this qualitative analysis.
Data Collection
Virtual semi-structured interviews were conducted by three interviewers trained in qualitative methods and, with participants’ permission, audio-recorded. Interviews were conducted between November 2020 and February 2021 and lasted from 45 min to 1 h. Participants received an IRB-approved honorarium for their time and expertise.
After reviewing informed consent and assent documents in advance, participants provided verbal consent at the start of the interview. A series of demographic and clinical questions was then administered to classify the present health and functional status of the person living with DMD. Based on current DMD health status, one of three versions of a semi-structured guide was selected. Interview guides differed according to clinical milestones on which the participant was asked to reflect, with one version for ambulatory patients, one for transitional ambulatory or early non-ambulatory patients, and a final interview guide for later non-ambulatory patients requiring ventilation. Definitions of ambulatory status were adapted from the Lowes Lab Ambulatory Status Algorithm (LASA) [28]; see Appendix Table 1 for further details. All three interview guides focused on eliciting patient experiences of living with DMD and understanding the HRQoL impacts of relevant clinical manifestations and symptoms. The content of the interview guides as well as the clinical and demographic questionnaires was informed by literature review and consultation with a clinical expert in DMD (SI). Furthermore, interview materials were iteratively updated based on participant feedback.
Analysis
Thematic analysis was used to explore patterns in participant responses using an iterative and multi-phase process, as described by Braun and Clarke [29, 30]. Given that few qualitative studies have been conducted to explore the social and emotional impacts of living with DMD, a primarily inductive approach was taken to promote the identification of novel and unexpected themes from the data. At the same time, some deductive analysis was deemed beneficial to gain a deeper understanding of certain concepts that have generated discussion in the existing literature, including patient and caregiver perceptions of previously identified key transitions in the DMD clinical course. For instance, LOA is often portrayed as a key milestone in DMD, yet patient and caregiver perspectives of its psychosocial implications are not well understood [31,32,33].
Audio recordings of the interviews were transcribed and transcripts reviewed by members of the research team to ensure accuracy and to promote familiarization with the data. This occurred while data collection was ongoing so that changing knowledge of the patient experience could be applied to future interviews. In addition, members of the research team noted insights with potential relevance to the research question, regarding either individual interviews or the entire dataset, at any time during data collection and analysis. Following data familiarization, two researchers (SMS and AB) coded five initial transcripts, selected to represent a range of experiences and perspectives with respect to respondent type and patient health and functional status. SMS and AB met to discuss and compare codes and to generate ideas about potential patterns in the data. The remaining interview transcripts were coded by AB, with the continuous addition of new codes and refinement of initial codes. Data were coded in Taguette [34] using an experiential orientation [35], which aimed to describe the lived experiences of individuals with DMD and the meaning that individuals and their caregivers attribute to these experiences. Codes were created for all aspects of the data that might contribute understanding to the social and emotional experience of living with DMD. Codes were compared across the full dataset, and then codes and supporting data extracts were grouped into categories that would later form the basis of potential themes. Following the organization of codes and data extracts into categories, themes were constructed, refined and named with input from all members of the research team.
The research team comprised stakeholders committed to therapeutic advancements in DMD, including health outcomes researchers, a clinical expert in DMD, methodological experts in health economics and market access professionals from a biotechnology company developing therapies for DMD. As such, the interpretative lens through which the study findings were contextualized includes health economics frameworks, methodologies exploring “own” versus hypothetical (utility) values and the inclusion of patient and caregiver voice in regulatory and access decision-making to deliver better health outcomes for patients.
Ethics and Reporting Guidelines
The study was performed in accordance with the Declaration of Helsinki and received ethical approval from an independent review board (IntegReview IRB SA200030, Approval date October 21, 2020) prior to initiating recruitment and data collection. All participants provided informed consent for participation and eventual publication of the results. Reporting of findings was conducted in accordance with the Standards for Reporting Qualitative Research guidelines [36].
Results
Sample Characteristics
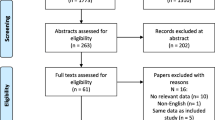
From the sample of 29 participants who completed the initial interviews, data from 19 interviews were included in the analysis. Data from 10 participants were excluded because of comorbid diagnoses of cognitive or behavioral disorders (specifically, autism spectrum disorders, obsessive-compulsive disorder, or selective mutism) that could impact their social interaction, in addition to the effect of DMD. The 19 included participants comprised 12 caregivers, 4 patient-caregiver dyads and 3 patients (Table 1). The median age of patients with DMD was 11 years; as anticipated, median patient age differed by respondent type as caregivers often reported on behalf of younger patients and young men opted to self-report their experiences. Caregiver participants included mothers, fathers and one aunt, all of whom assumed a parental role in the care and upbringing of the individual whose experiences with DMD they described. Six (32%) patients were ambulatory, 3 (16%) were in a transitional ambulatory state, and 10 (53%) were non-ambulatory. Nocturnal ventilation was used by 7 (37%) patients, and 11 (58%) had lost upper limb function. Sixteen (84%) boys and young men living with DMD were students, including three of the seven adults (age ≥ 18 years) with DMD. However, an additional four adults with DMD (57%) were at home without a current daytime occupation.
Themes
Three themes were identified during thematic analysis. Within each theme, multiple subthemes were generated to capture the nuanced, and at times conflicting, ways in which participants described social and emotional challenges of living with DMD as well as sources of strength and resilience. Themes and subthemes are visually mapped in Fig. 1.
Theme 1: Barriers to Social Participation Are Multifaceted
Individual-level barriers related to the clinical status and progression of DMD limit social participation, and these impacts were often compounded by barriers at the societal level. Starting at a young age, barriers related to physical impairments affected participation in activities with peers. Frequently described barriers included symptoms, such as muscle weakness, pain and fatigue, but also emotional barriers such as worry about being “different.” For instance, one participant described how, since being diagnosed with DMD, her son’s interactions with his peers had changed (Table 2, quotation 1). Numerous participants described how their young child wished to take part in outdoor games and physical activities with siblings or peers yet was limited by their strength and endurance (Table 2, quotation 2).
Declining ambulatory function contributes to increasing difficulties in taking part in activities with friends and family (Table 2, quotation 3). However, while physical limitations to participation were frequently described, not all boys living with DMD felt they were missing out. This was because, having always lived with DMD, boys tended to develop interests aligned with their strengths and abilities. Some participants commented that their child was not particularly competitive or interested in sports, indicating preferences for activities such as video games and reading (Table 2, quotation 4).
In addition, boys and young men living with DMD sometimes described themselves, or were described by their parents, as naturally introverted, such that they were satisfied with the social activities in which they partake (Table 2, quotation 5). While it is difficult to know to what extent their interests might differ without DMD, it was made apparent in most interviews that boys and young men living with DMD adapt to their experiences and find enjoyment in their chosen activities.
Loss of ambulation involved adaptation as boys became increasingly dependent on mobility devices, including scooters, manual wheelchairs and power chairs, to get around within their communities. Participant accounts of loss of ambulation illustrated the two-fold impact of mobility devices on social participation. On the one hand, mobility devices could enhance opportunities for participation by allowing individuals to regain some of the independence previously lost while their lower limb function was deteriorating. However, transitioning to full-time wheelchair use was also associated with new challenges related to accessibility, which in some cases limits social participation. Reflecting on the gradual process of losing ambulation, participants described the positive impact of transitioning to a wheelchair (Table 2, quotations 6 and 7). Yet, despite the increased independence provided, participants explained that the wheelchair introduced new barriers to participation, including navigating in certain environments and challenges when visiting the homes of friends or family members (Table 2, quotation 8).
Experiences of social participation among boys and young men with DMD were also influenced by the extent of structures to support social inclusion within communities, which was exemplified by varying accounts of wheelchair accessibility in public spaces or the level of assistance available in schools, among other determinants (Table 2, quotation 9). However, another participant had the contrasting view that because facilities where they lived were not wheelchair accessible, there were places that they were unable to visit as a family.
Moreover, it appeared that social inclusion was particularly lacking during the transition into adulthood, as some young men living with DMD described a narrowing of social opportunities and insufficient social supports to meet their changing needs. Participants related how social opportunities were limited because friends establish working lifestyles in which they are unable to readily fit (Table 2, quotation 10). While some degree of social engagement may be maintained through online connections like multiplayer video games, disease progression was associated with social isolation (Table 2, quotation 11). Conversely, some participants described greater satisfaction with their social participation and activities as they entered adulthood, which highlighted the value of social engagement through education and community involvement during later stages of DMD.
Theme 2: An Emotional Journey Shaped by ‘Inevitable Progression’
Inextricably linked to social participation barriers experienced by boys and young men with DMD were the emotional challenges they faced in coping with their disease, which continued to evolve with advancing age and as their condition progressed. Caregivers indicated that emotional challenges with self-perception and self-esteem are particularly salient among younger boys as they begin to experience decline in lower limb function and how coping with the physical limitations of DMD can be more challenging in the presence of peers (Table 2, quotation 12). Another parent described their child’s emotional struggle during the initial decline in lower limb function and again with the start of using a wheelchair (Table 2, quotation 13) and reflected on the emotional adaptation that they witnessed as time went on (Table 2, quotation 14).
Although accounts of emotional growth and adaptation in relation to loss of ambulation were frequently shared, participants also described new emotional challenges that followed this transition. In particular, the loss of independence that accompanied decline in upper limb function was often considered to be more difficult than the transition to requiring a wheelchair. While use of a wheelchair could facilitate independence, loss of upper limb function was more often framed as a source of ongoing frustration due to a steady decline in ability to independently carry out self-care and leisure activities (Table 2, quotation 15). In addition to feelings of frustration, some individuals expressed worry about the future in relation to loss of upper limb function (Table 2, quotation 16). At times participants also alluded to the emotional hurdles of accepting the clinical trajectory of DMD (Table 2, quotation 17).
Interview responses from both caregivers and patients illustrated remarkable emotional resilience among those living with DMD, and a variety of strategies were described as mechanisms of coping with or adapting to the continuously evolving emotional challenges associated with DMD. Participants described sources of motivation that provided emotional strength to overcome challenges, such as religion or pursuing educational accomplishments (Table 2, quotations 18 and 19). For some participants, finding distractions was described as one way to help keep one’s mind off things. Playing video games or watching television could provide a break from thinking about DMD (Table 2, quotation 20). Moreover, a common idea across many interviews was the need to live in the moment rather than worry about the future (Table 2, quotation 21).
Theme 3: Family Provides Critical Tangible and Emotional Support
As boys and young men faced evolving emotional challenges alongside the progression of DMD, family members provided a constant source of support. Providing unspoken tangible support, whereby families minimize worry about everyday tasks, was an essential means through which this occurred (Table 2, quotation 22). Parents described regularly assisting their children with mobility tasks both within and outside of the home. Help with self-care tasks such as showering, toileting, getting dressed and eating was also frequently relied upon. Parents noted the importance of this type of support for ensuring a sense of safety and security while smoothing the perceived difficulties or setbacks (Table 2, quotation 23).
Despite the support from family members, boys with DMD often desired to be more independent. Parents were conscious of this source of frustration among their sons and described creating opportunities for independence (Table 2, quotation 24). Family members also provided their sons with emotional support and consolation as they lost the physical ability to do things on their own and sought to help them come to terms with needing everyday assistance (Table 2, quotation 25).
However, reliance on family had the potential to become more complex during adolescence or early adulthood. In DMD, loss of independence resulting from decreased upper limb function often coincides with early adolescence—a time that is usually characterized by increased autonomy—and navigating this transition posed a challenge for patients and caregivers alike (Table 2, quotation 26). Although the caregivers in this study did not view their responsibilities as a burden, one participant expressed worry about the impact of caregiving on their parent’s wellbeing (Table 2, quotation 27). Finally, a parent described how their immediate family had become more isolated from other family members and friends who “shy away” from the challenges their family has faced as her teenage son’s disease progressed (Table 2, quotation 28). Yet overall participants described persevering as a family through each new challenge they faced and emphasized how greatly they valued the support system they had developed.
Discussion
In this study, we sought to understand the social and emotional experience of living with DMD from the perspective of patients and their family caregivers. Our results indicate that the process of integrating DMD into one’s day-to-day life is complex and challenging. For example, social impacts of DMD are shaped not only by progressive muscular degeneration that characterizes DMD’s clinical trajectory but also by social barriers, including lack of accessibility in the built environment and challenges related to social inclusion. These findings are consistent with previous research that has identified accessibility and social discrimination as important problems that constrain opportunities for social and community engagement among individuals living with DMD [14, 18, 37]. The experiences of several study participants further suggested that potential participation barriers are compounded as individuals with DMD enter adulthood. Previous qualitative studies have similarly identified a risk of social isolation during this period and called for improved social supports for young men with DMD [15, 18, 19].
The social model of disability, which recognizes the systemic oppression experienced by individuals with disabilities due to framing disability as biomedical problem [38, 39], has been an important theoretical framework in qualitative research in DMD [15, 21, 31, 37, 40]. This model was instrumental in interpreting the experiences described by patients and caregivers in the present study. Yet, as discussed by Abbott and Carpenter, it is equally important to recognize the diversity of experiences among young people with disabilities with respect to physical, sensory and cognitive impairments [15, 31, 40]; in the case of DMD, affected individuals often desire opportunities to speak openly about bodily impairments that contribute to the emotional implications of living with a progressive condition [15, 19, 31, 37].
Our study provides novel insights into nuances of social and emotional experiences among boys with DMD as their ambulatory function declines and as they transition to using a wheelchair. Participants’ accounts emphasize that LOA is not a discrete event but rather a process with multiple phases and varied implications for social participation. Importantly, we found that wheelchair use could enhance participation when contrasted with the mobility challenges individuals previously experienced. Despite challenges that affected social participation at various clinical stages in DMD, interviews conveyed that boys and young men were often highly engaged in activities that provided personal satisfaction. Among other activities, online video games provided both a source of entertainment and a platform for social engagement.
Living with a progressive condition such as DMD requires ongoing adaptation, and while loss of physical function could prompt feelings of embarrassment, sadness or frustration, the boys and young men in this study approached transitions with emotional strength and resourcefulness. Individuals with DMD and their families coped with challenges by living in the moment and through sources of optimism, joy, and achievement in their daily lives. Documenting how the lives of those with DMD are affected from their own perspective is important because people who are not experienced with disabling health conditions often carry assumptions about what it is like to live with them. Research suggests that one reason that public perceptions of disability differ from lived experiences is because the public fails to appreciate the role of patient adaptation and outlook in shaping the experiences of individuals with disabilities [41,42,43]. In particular, studies with individuals who use wheelchairs show that, from the patient perspective, lack of ambulatory function does not always equate to worse HRQoL [19, 41, 44]. This divergence in perspectives on what life is like with a health condition is important, as the opinions of members of the general public on the severity and impact of a health condition are incorporated into healthcare decision-making frameworks when considering access to new medications [45]. These differences in how members of the general public consider the impact of disabling conditions, compared to the lived patient experience, therefore have potentially challenging implications for decision-making around access to new therapies in DMD [46, 47].
Participants in this study presented decline in upper limb function as a greater emotional hurdle to overcome compared to LOA, suggesting that transition from independent upper limb function to dependence on others warrants greater attention and support. Loss of independence appears a particularly difficult outcome of upper limb impairment, which was illustrated using tangible examples such as the inability to perform self-care tasks or engage in leisure activities.
For HRQoL measures to have relevance to DMD, they should reflect constructs identified as important by patients with DMD and their caregivers, such as extent of upper limb function, sense of identity and autonomy. However, as other studies have highlighted, the non-disease-specific measures of HRQoL that are frequently used to inform economic evaluations provide limited coverage of these aspects of function and wellbeing that are of importance to people with DMD [48, 49].
Findings also illustrated the importance of the family as a support system for boys and young men with DMD. Previous research shows that family caregivers also rely on extensive networks for emotional, social and practical support, including information to navigate healthcare systems and financial support to pay for equipment and an array of healthcare costs related to DMD [50]. In addition to helping families meet their sons’ physical and emotional care needs, access to systems of support may provide protection against poor HRQoL outcomes that have been documented among caregivers in DMD [51, 52]. However, this raises concerns about equitable access to these resources, as differences in social capital may influence experiences of caregiving.
Strengths and Limitations
An important strength of this study is its collection of rich data from patients and caregivers reporting on the patient’s behalf, regarding experiences of living with DMD over time. Participants described how DMD impacts currently affect their daily life and also looked back on past experiences and important changes that have occurred. This approach allowed for the discussion to be guided by what participants felt to be the most impactful aspects of DMD at different life stages. While only 19 individuals participated in the interviews, this sample size was deemed robust for obtaining detailed descriptions of psychosocial impacts to allow for sufficient depth of analysis [53]; the sample size was also consistent with other qualitative studies in DMD [19, 54, 55]. A limitation arises from the fact that, despite best efforts to recruit a sample reflecting a wide range of patient ages and clinical statuses, few individuals with highly progressed DMD were enrolled. Although multiple participants shared reflections on the transition into adulthood, certain experiences that are associated with highly progressed DMD, such as cardiac events or the need for daytime ventilation, would have been missed. In addition, most participants were caregivers reporting on behalf of patients, since relatively few patients volunteered and those that did were generally young adults or adolescents. Previous research indicates that individuals living with DMD and their caregivers differ in their impressions of the HRQoL impacts of living with the disease [56, 57]. Therefore, the paucity of data that directly reflect the perspectives of younger patients is an important limitation of this study. One must also consider the features of the reflexive thematic method, which assumes the researcher’s position and contribution is necessary, unavoidable and an integral ingredient of the research process [29, 30]. So, while the views presented reflect one interpretation of the available data, other interpretations are also possible.
Conclusions
This study illustrates the complexities of growing up with DMD and how the psychosocial impacts of this disease are shaped by the progression of symptoms and clinical manifestations alongside a host of other factors including the extent of social barriers, personal growth and adaptation, and family support. Despite the severity of this progressive condition, patients and their families demonstrated strength and resilience and a capacity for optimism and coping through living in the moment. These interviews also provided novel insights about the relative importance of loss of upper limb function vs. LOA and how perceived severity of the transition to needing a wheelchair is often tempered by new opportunities for participation and enhanced independence. Moreover, this study helps us to appreciate the importance and impact of day-to-day moments on the lives of individuals with DMD, whether it be life’s major milestones or simple activities that are taken for granted by most people. These results can help to contextualize quantitative HRQoL data and to ensure that the lived experiences and perspectives of patients and caregivers are accounted for when considering the potential benefits of emerging treatments.
Data Availability
Data not available; qualitative interview data will not be shared in order to protect the identity of the study participants.
References
Wein N, Alfano L, Flanigan KM. Genetics and emerging treatments for Duchenne and Becker muscular dystrophy. Pediatr Clin North Am. 2015;62(3):723–42.
Crisafulli S, Sultana J, Fontana A, Salvo F, Messina S, Trifirò G. Global epidemiology of Duchenne muscular dystrophy: an updated systematic review and meta-analysis. Orphanet J Rare Dis. 2020;15(1):141.
Yiu EM, Kornberg AJ. Duchenne muscular dystrophy. J Paediatr Child Health. 2015;51(8):759–64.
Ryder S, Leadley RM, Armstrong N, et al. The burden, epidemiology, costs and treatment for Duchenne muscular dystrophy: an evidence review. Orphanet J Rare Dis. 2017;12(1):79.
Szabo SM, Salhany RM, Deighton A, Harwood M, Mah J, Gooch KL. The clinical course of Duchenne muscular dystrophy in the corticosteroid treatment era: a systematic literature review. Orphanet J Rare Dis. 2021;16(1):237.
Hendriksen JGM, Vles JSH. Neuropsychiatric disorders in males with Duchenne muscular dystrophy: frequency rate of attention-deficit hyperactivity disorder (ADHD), autism spectrum disorder, and obsessive—compulsive disorder. J Child Neurol. 2008;23(5):477–81.
Uttley L, Carlton J, Woods HB, Brazier J. A review of quality of life themes in Duchenne muscular dystrophy for patients and carers. Health Qual Life Outcomes. 2018;16(1):237.
Powell PA, Carlton J, Woods HB, Mazzone P. Measuring quality of life in Duchenne muscular dystrophy: a systematic review of the content and structural validity of commonly used instruments. Health Qual Life Outcomes. 2020;18(1):263.
Bann CM, Abresch RT, Biesecker B, et al. Measuring quality of life in muscular dystrophy. Neurology. 2015;84(10):1034–42.
Popay J, Williams G. Qualitative research and evidence-based healthcare. J R Soc Med. 1998;91(Suppl 35):32–7.
Germeni E, Vallini I, Bianchetti MG, Schulz PJ. Reconstructing normality following the diagnosis of a childhood chronic disease: does “rare” make a difference? Eur J Pediatr. 2018;177(4):489–95.
Vanagė D, Valickienė RP, Serapinas D. A qualitative systematic review of living with duchenne muscular dystrophy. Soc Inq Well-Being. 2021;19(2):63–82.
Fujino H, Iwata Y, Saito T, Matsumura T, Fujimura H, Imura O. The experiences of patients with Duchenne muscular dystrophy in facing and learning about their clinical conditions. Int J Qual Stud Health Well Being. 2016;11(1):32045.
Gibson BE, Mistry B, Smith B, et al. Becoming men: gender, disability, and transitioning to adulthood. Health (Lond Engl 1997). 2014;18(1):95–114.
Abbott D, Carpenter J. ‘Wasting precious time’: young men with Duchenne muscular dystrophy negotiate the transition to adulthood. Disabil Soc. 2014;29(8):1192–205.
Lindsay S, McAdam L, Mahendiran T. Enablers and barriers of men with Duchenne muscular dystrophy transitioning from an adult clinic within a pediatric hospital. Disabil Health J. 2017;10(1):73–9.
Gibson BE, Young NL, Upshur RE, McKeever P. Men on the margin: a Bourdieusian examination of living into adulthood with muscular dystrophy. Soc Sci Med (1982). 2007;65(3):505–17.
Gibson BE, Zitzelsberger H, McKeever P. ‘Futureless persons’: shifting life expectancies and the vicissitudes of progressive illness. Sociol Health Illn. 2009;31(4):554–68.
Abbott D, Prescott H, Forbes K, Fraser J, Majumdar A. Men with Duchenne muscular dystrophy and end of life planning. Neuromuscular Disord NMD. 2017;27(1):38–44.
Abbott D, Jepson M, Hastie J. Men living with long-term conditions: exploring gender and improving social care. Health Soc Care Commun. 2016;24(4):420–7.
Skyrme S. Living with Duchenne muscular dystrophy: relational autonomy and decision-making. Child Soc. 2016;30(3):220–9.
Szabo SM, Audhya IF, Malone DC, Feeny D, Gooch KL. Characterizing health state utilities associated with Duchenne muscular dystrophy: a systematic review. Qual Life Res. 2020;29(3):593–605.
Perumal AR, Rajeswaran J, Nalini A. Neuropsychological profile of duchenne muscular dystrophy. Appl Neuropsychol Child. 2015;4(1):49–57.
Snow WM, Anderson JE, Jakobson LS. Neuropsychological and neurobehavioral functioning in Duchenne muscular dystrophy: a review. Neurosci Biobehav Rev. 2013;37(5):743–52.
Huang L, Yao Q, Gu X, et al. 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. Lancet. 2021;398(10302):747–58.
Hausmann JS, Vizcaino-Riveros J, Marin AC, et al. Feasibility and efficacy of online strategies to recruit parents of children with rheumatic diseases for research. ACR Open Rheumatol. 2022;4(5):410–6.
Filipovic Audhya I, Szabo S, Bever AE, et al. PCR176 time trade-off utility values for health states characterizing progressive muscular degeneration in Duchenne muscular dystrophy (DMD). Value Health. 2022;25(7):S574.
Reash LLaN. The Lowes Lab Ambulatory Status Algorithm: a new tool to determine ambulatory status. Abigail Wexner Research Institute; 2019.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exercise Health. 2019;11(4):589–97.
Abbott D, Carpenter J. “The things that are inside of you are horrible”: children and young men with Duchenne muscular dystrophy talk about the impact of living with a long-term condition. Child Care Pract. 2015;21(1):67–77.
Williams K, Buesch K, Acaster S. Symptoms and impacts of nonsense mutation Duchenne muscular dystrophy at different stages of ambulation. Future Neurol. 2021;16(1):FNL5.
Szabo S, Filipovic Audhya I, Bever AE, et al. PCR105 the impact of key health state transitions on health-related quality of life (HRQOL) in Duchenne muscular dystrophy (DMD): a qualitative study. Value Health. 2022;25(7):S560–1.
Rampin R, Rampin V. Taguette: open-source qualitative data analysis. J Open Source Softw. 2021;6(68):3522.
Byrne D. A worked example of Braun and Clarke’s approach to reflexive thematic analysis. Qual Quant. 2022;56(3):1391–412.
OBrien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of Recommendations. Acad Med. 2014;89(9): 1245-1251
Skyrme S. In and on their own terms: children and young people’s accounts of life with Duchenne muscular dystrophy. Child Care Pract. 2017;23(1):77–89.
Oliver M. The social model of disability: thirty years on. Disabil Soc. 2013;28(7):1024–6.
Barnes C. Understanding the social model of disability. London: Routledge; 2012.
Abbott D, Carpenter J, Gibson BE, Hastie J, Jepson M, Smith B. Disabled men with muscular dystrophy negotiate gender. Disabil Soc. 2019;34(5):683–703.
Bray N, Noyes J, Harris N, Edwards RT. Defining health-related quality of life for young wheelchair users: a qualitative health economics study. PLoS ONE. 2017;12(6): e0179269.
Ubel PA, Loewenstein G, Jepson C. Whose quality of life? A commentary exploring discrepancies between health state evaluations of patients and the general public. Qual Life Res. 2003;12(6):599–607.
Versteegh MM, Brouwer WBF. Patient and general public preferences for health states: a call to reconsider current guidelines. Soc Sci Med. 1982;2016(165):66–74.
Bartonek Å, Saraste H, Danielsson A. Health-related quality of life and ambulation in children with myelomeningocele in a Swedish population. Acta Paediatr. 2012;101(9):953–6.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: OUP; 2015.
Canadian Agency for Drugs and Technologies in Health [CADTH]. Guidelines for the economic evaluation of health technologies. Ottawa, Canada: CADTH; 2017.
National Institute for Health and Care Excellence [NICE]. Guide to the methods of technology appraisal. London: NICE; 2013.
Powell PA, Carlton J, Rowen D, Brazier JE. Producing a preference-based quality of life measure for people with Duchenne muscular dystrophy: a mixed-methods study protocol. BMJ Open. 2019;9(3): e023685.
Powell PA, Carlton J, Rowen D, Chandler F, Guglieri M, Brazier JE. Development of a new quality of life measure for Duchenne muscular dystrophy using mixed methods. Neurology. 2021;96(19): e2438.
Donnelly CM, Quinlivan RM, Herron A, Graham CD. A systematic review and qualitative synthesis of the experiences of parents of individuals living with Duchenne muscular dystrophy. Disabil Rehabil. 2022;45(8):1285–98.
Glover S, Hendron J, Taylor B, Long M. Understanding carer resilience in Duchenne muscular dystrophy: a systematic narrative review. Chronic Illn. 2018;16(2):87–103.
Landfeldt E, Edström J, Buccella F, Kirschner J, Lochmüller H. Duchenne muscular dystrophy and caregiver burden: a systematic review. Dev Med Child Neurol. 2018;60(10):987–96.
Hammarberg K, Kirkman M, de Lacey S. Qualitative research methods: when to use them and how to judge them. Hum Reprod. 2016;31(3):498–501.
Williams K, Davidson I, Rance M, Boehnke A, Buesch K, Acaster S. Symptoms and impacts of ambulatory nonsense mutation Duchenne muscular dystrophy: a qualitative study and the development of a patient-centred conceptual model. J Patient Rep Outcomes. 2021;5(1):75.
Walker M, Mistry B, Amin R, et al. A qualitative exploration of the priorities and experiences of children with Duchenne muscular dystrophy, their parents, and healthcare professionals around weight management. Disabil Rehabil. 2022;44(26):8234–42.
Lim Y, Velozo C, Bendixen RM. The level of agreement between child self-reports and parent proxy-reports of health-related quality of life in boys with Duchenne muscular dystrophy. Qual Life Res. 2014;23(7):1945–52.
Opstal SLSHv, Jansen M, van Alfen N, de Groot IJM. Health-related quality of life and its relation to disease severity in boys with Duchenne muscular dystrophy: satisfied boys, worrying parents—a case–control study. J Child Neurol. 2013;29(11):1486–95.
Acknowledgements
The authors would like to thank those who took part in this study for sharing their insights and experiences and for contributing their time.
Funding
This study was funded by Sarepta Therapeutics, Inc. (grant number: n/a). Sarepta Therapeutics, Inc. is also funding the journal’s Rapid Service and Open Access Fees.
Author information
Authors and Affiliations
Contributions
Andrea Bever and Alexis Mickle contributed to the collection of data. Analysis and interpretation of the data was led by Andrea Bever with support from Shelagh M. Szabo. Andrea Bever was responsible for drafting the manuscript. All authors contributed to the study design and the critical review of the manuscript. All authors approved the final version of the manuscript. All authors comply with ICMJE guidelines for authorship.
Corresponding author
Ethics declarations
Conflicts of Interest
Ivana Audhya and Katherine Gooch are employees of Sarepta Therapeutics, Inc. and may own stock/options. Shelagh M. Szabo, Andrea Bever and Alexis Mickle are employees of Broadstreet HEOR, which received funds from Sarepta Therapeutics, Inc. to conduct this study. David Feeny, Peter Neumann, and Daniel Malone received consulting fees related to this work. David Feeny has a proprietary interest in Health Utilities Incorporated, Dundas, Ontario, Canada. HUInc. distributes copyrighted Health Utilities Index (HUI) materials and provides methodological advice on the use of HUI. Susan Iannaccone has received research funding or consulting fees from Avexis, Biogen, Fibrogen, Mallinkrodt, Regeneron, Sarepta Therapeutics, Inc., Scholar Rock, PTC Therapeutics, Pfizer, MDA, CureSMA, NIH, Genentech-Roche, and BCBS.
Ethical Approval
The study was performed in accordance with the Declaration of Helsinki and received ethical approval from an independent review board (IntegReview IRB SA200030, Approval date October 21, 2020) prior to initiating recruitment and data collection. All participants provided informed consent for participation and eventual publication of the results. Reporting of findings was conducted in accordance with the Standards for Reporting Qualitative Research guidelines [36]. After reviewing informed consent and assent documents in advance, participants provided verbal consent at the start of the interview.
Additional information
Prior Presentation: Some findings from this study were presented in a poster at the ISPOR conference, May 16–18, 2022, Washington, DC, USA. https://www.ispor.org/heor-resources/presentations-database/presentation/intl2022-3461/115099.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bever, A., Audhya, I., Szabo, S.M. et al. “You Take This Day by Day, Come What May”: A Qualitative Study of the Psychosocial Impacts of Living with Duchenne Muscular Dystrophy. Adv Ther 41, 2460–2476 (2024). https://doi.org/10.1007/s12325-024-02867-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-024-02867-0