Abstract
Introduction
Risk factors for thromboembolic events in patients with dialysis-dependent chronic kidney disease (CKD) receiving roxadustat are unknown. Iron deficiency has been reported as a risk factor for thrombosis in the general population.
Methods
Thromboembolic events with onset before and after week 12 in patients receiving roxadustat were evaluated in this pooled analysis of four global phase 3 trials, PYRENEES, SIERRAS, HIMALAYAS, and ROCKIES. Baseline risk factors for thromboembolic events were investigated by Cox regression analyses. Nested case-control analyses with matched pairs of case-control data explored the relationship between thromboembolic events and last known laboratory parameters before event onset.
Results
Of 2354 patients, 1026 thromboembolic events were observed in 568 patients. Baseline risk factors found included hemodialysis (vs peritoneal dialysis), advanced age (≥ 65 years), Black race, high high-sensitivity C-reactive protein, and history of thromboembolism, cardiovascular disease, or diabetes. Univariate case-control analyses revealed that high hemoglobin rate of rise (≥ 0.5 g/dL/week; odds ratio [OR] 2.09; 95% confidence interval [CI] 0.98–4.46) showed a trend towards increased risk of thromboembolic events before week 12, and high rate of hemoglobin decline was associated with events after week 12 (< − 0.5 g/dL/week; OR 3.73; 95% CI 1.68–8.27) as compared to stable hemoglobin levels (≥ − 0.1 to < 0.1 g/dL/week). Multivariate case-control analyses showed that low last known hemoglobin level (< 10 g/dL: adjusted OR 1.91; 95% CI 1.04–3.50; vs ≥ 12 g/dL) and low last known transferrin saturation (TSAT < 10%: adjusted OR 3.78; 95% CI 1.71–8.39; vs ≥ 30%) before event onset were associated with events after week 12. In patients with last known TSAT < 30%, higher roxadustat dose was associated with thromboembolic events; however, no association was observed in those with TSAT ≥ 30%.
Conclusions
Among various risk factors for thromboembolic events, it is reasonable to avoid a rapid increase and decline in hemoglobin levels as well as ensure TSAT ≥ 30%, rather than increasing the roxadustat dose.
Graphical Abstract available for this article.
Trial Registration
NCT02278341, NCT02273726, NCT02052310, NCT02174731.
Plain Language Summary
Roxadustat is an oral treatment for patients with anemia, or low hemoglobin levels, due to chronic kidney disease. Thromboembolic events are caused by a blood clot blocking blood vessels, and they have occurred in clinical trials of roxadustat. This analysis evaluated risk factors for thromboembolic events in patients receiving roxadustat to treat anemia of chronic kidney disease who are on dialysis. Two different statistical approaches were used to investigate risk factors for thromboembolic events that occurred before and after 12 weeks of roxadustat treatment. We found that rapid improvement of anemia after starting roxadustat treatment may be associated with an increased risk of thromboembolic events occurring in the first 12 weeks of treatment. In contrast, severe anemia or worsening of anemia was associated with an increased risk of thromboembolic events after week 12. Low iron levels in the blood or greater decline of available iron in the blood from baseline were also detected as risk factors for the events after week 12, suggesting that iron supplementation is important in patients who are iron-deficient. Moreover, thromboembolic events were also associated with older age (≥ 65 years), Black race, high levels of inflammation, and having had a previous thromboembolic event or having a history of cardiovascular disease or diabetes. Some risk factors, such as iron status and hemoglobin levels, can be changed after beginning roxadustat treatment and should be monitored and modified, as needed.
AbstractSection Graphical Abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Roxadustat, an oral hypoxia-inducible factor prolyl hydroxylase inhibitor, is approved in multiple countries and regions for the treatment of anemia of chronic kidney disease (CKD). |
Thromboembolic events have occurred in clinical trials of roxadustat and further information is needed to characterize patients with dialysis-dependent CKD who experienced thromboembolic events following treatment with roxadustat. |
The current post hoc exploratory analysis evaluated patient characteristics and laboratory parameters that may be related to thromboembolic events in patients with anemia of dialysis-dependent CKD treated with roxadustat. |
What was learned from the study? |
In addition to established risk factors, a high hemoglobin rate of rise (≥ 0.5 g/dL/week) may augment the risk of thromboembolic events at the early period of treatment, highlighting the importance of careful monitoring to prevent too rapid of a rise in hemoglobin when initiating roxadustat treatment. |
In contrast, a low hemoglobin level (< 10 g/dL) and rapid decline of hemoglobin (< − 0.5 g/dL/week) were each associated with an increased risk of thromboembolic events after week 12; low transferrin saturation (TSAT) (< 30%) and greater decline of TSAT (> 15%) from baseline were also detected as risk factors for this late period. |
In patients with last known TSAT < 30%, higher roxadustat dose was associated with thromboembolic events; however, no association between dose and events was observed in those with TSAT ≥ 30%. |
Failure to achieve the hemoglobin target level should prompt a search for other causative factors; one option may be iron therapy until reaching TSAT ≥ 30%, rather than increasing the dose of roxadustat. |
Digital Features
This article is published with digital features, including a Graphical Abstract, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.24466201.
Introduction
A common complication of dialysis-dependent (DD) chronic kidney disease (CKD) is anemia. Patients with anemia of DD CKD have an increased risk of cardiovascular events, hospitalization, and mortality [1, 2]. Adults with CKD who have hemoglobin concentrations < 13.0 g/dL (men) or < 12.0 g/dL (women) at multiple examinations meet the criteria for diagnosis of anemia according to the Kidney Disease Improving Global Outcomes (KDIGO) guidelines [3]. Oral or intravenous iron therapy is recommended for patients with anemia of CKD if their transferrin saturation (TSAT) is ≤ 30% and ferritin levels are ≤ 500 ng/mL [3]. The European Renal Best Practice (ERBP) group recommends initiating either oral or intravenous iron therapy in patients with DD CKD when TSAT is < 25% and ferritin is < 300 ng/mL [4]. Treatment with an erythropoiesis-stimulating agent (ESA) in this patient population is commonly used to increase, or maintain, hemoglobin levels to their target range and may include concomitant supplementation with iron therapy [2].
Roxadustat is approved in multiple countries and regions for the treatment of anemia of CKD. Roxadustat, an oral hypoxia-inducible factor prolyl hydroxylase inhibitor (HIF-PHI), raises hemoglobin levels through activation of erythropoiesis and improved iron metabolism. Elevated hepcidin is a cause of iron imbalance observed in patients with CKD, as well as other chronic inflammatory diseases. Roxadustat has been shown to decrease hepcidin levels and thereby improve iron metabolism [2]. Roxadustat has demonstrated efficacy across multiple global phase 3 studies by increasing and/or maintaining hemoglobin levels in patients with anemia of CKD with acceptable tolerability [5,6,7,8].
A recent meta-analysis comprising more than 13,000 patients across 30 studies found that treatment with HIF-PHIs may increase the risk for thromboembolic events compared to treatment with ESAs [9]. Since the analysis by Chen et al. examined patients treated with any HIF-PHI, further information is needed to characterize patients with DD CKD who experienced arterial and/or venous thromboembolic events following administration of roxadustat.
A post hoc analysis of four phase 3 studies in Japan suggested that several patient characteristics and laboratory parameters were related to the occurrence of thromboembolism in patients treated with roxadustat [10]. The objective of the current post hoc analysis was to evaluate the patient characteristics and laboratory parameters that may be related to thromboembolic events in a larger, global population of patients treated with roxadustat.
Methods
Component Studies
This post hoc exploratory analysis pooled data from four phase 3, open-label, randomized, ESA active comparator–controlled clinical trials in patients with anemia of DD CKD: NCT02278341 (PYRENEES), NCT02273726 (SIERRAS), NCT02052310 (HIMALAYAS), and NCT02174731 (ROCKIES) [5,6,7,8]. Patients were enrolled and randomly assigned on a 1:1 basis to receive roxadustat or epoetin alfa in the SIERRAS, HIMALAYAS, and ROCKIES studies and either epoetin alfa or darbepoetin alfa in the PYRENEES study. More details regarding the component studies are available in the Methods section of the electronic supplementary material.
All studies included in this post hoc analysis were conducted in accordance with the ethical principles of the Declaration of Helsinki of 1964 and its later amendments, the International Conference on Harmonisation of Technical Requirements for Pharmaceutical for Human Use guidelines, Good Clinical Practice, and applicable local laws and regulations. Individual study details are available at https://clinicaltrials.gov/ct2/show/NCT02278341, https://clinicaltrials.gov/ct2/show/NCT02273726, https://clinicaltrials.gov/ct2/show/NCT02052310, and https://clinicaltrials.gov/ct2/show/NCT02174731, and their associated publications [5,6,7,8].
As this was a pooled post hoc analysis, approval by an ethics committee for this analysis was not necessary; however, institutional review board approval was obtained prior to initiating each of the included studies. All participants provided written informed consent.
Participants
All eligible patients were adults (≥ 18 years), had anemia of CKD, TSAT ≥ 20%, and serum ferritin ≥ 100 ng/mL, and were receiving either hemodialysis or peritoneal dialysis. Exclusion criteria included recent red blood cell transfusion, prior treatment with roxadustat or another HIF-PHI, active/chronic gastrointestinal bleeding, and anticipated elective surgery with blood loss expected. Patients underwent anticoagulation therapy during dialysis sessions according to standard practice.
Iron Administration Protocols
Oral iron supplementation was permitted for patients in all studies. Intravenous iron therapy was permitted in patients treated with roxadustat if hemoglobin levels did not increase sufficiently after ≥ 2 dose increases, and their TSAT or ferritin levels fell to < 20% or < 100 ng/mL, respectively (ROCKIES, PYRENEES). Intravenous iron therapy was allowed if, in the investigator’s opinion, a patient’s hemoglobin levels had not responded adequately and their TSAT or ferritin levels fell below 20% or 100 ng/mL, respectively (HIMALAYAS, SIERRAS).
Definition of Thromboembolic Events
All preferred terms, selected by Standardized MedDRA Queries, embolic and thrombotic events (narrow), were included as thromboembolic events. An exploratory post hoc analysis conducted using pooled data from four Japanese phase 3 clinical trials [10] suggested that there was a temporary peak in event frequency during the early treatment period (from week 0 to week 8) and more shunt-related events were particularly observed during this period; the event frequency decreased by week 8 and became stable over the period from week 8 to week 16, and then gradually increased until week 52. The breakdown of events differed between the early period and the later period of treatment, with shunt-related events accounting for the majority before week 12, while the proportion of arterial-related events/vein-related events increased after week 12. The factors potentially associated with the incidence of thromboembolic events differed between the early and later period of treatment.
Therefore, all analyses were performed separately for events with onset before and after week 12, the same cutoff time used in the analysis of Japanese phase 3 clinical trials. Thromboembolic events before week 12 were any events with onset before day 85 (exclusive), and events after week 12 were any events with onset after day 85 (inclusive). An event was classified as on-treatment if it occurred on or after day 1 and up to 7 days after the end of treatment.
Analysis Method and Statistical Analysis
Cox regression analysis and nested case-control analysis were used to evaluate the relationship of risk factors with thromboembolic events in patients treated with roxadustat.
Cox Regression Analysis
Time to first onset of thromboembolic events before and after week 12 was analyzed by subgroups using the Kaplan-Meier methodology for each factor, and the association between the thromboembolic events and each factor was tested by a log-rank test. Hazard ratios and 95% confidence intervals (CIs) were calculated using a univariate Cox proportional hazards model for each factor, which included patients’ demographic and clinical characteristics and ESA treatment history. Multivariate Cox regression analysis was performed to further explore the association between selected factors and thromboembolic events, where the hazard ratios and 95% CIs were calculated using a multivariate Cox proportional hazards model.
Nested Case-Control Analysis
Cases were defined as patients with a thromboembolic event and controls were defined as patients without a thromboembolic event. For a patient with an event at a given time point (days from first study drug taken), potential controls who had not experienced a thromboembolic event at the onset time of the case were selected. Controls with similar characteristics, accounting for important confounding variables, were selected from the potential controls using a matching algorithm. Matching variables were selected on the basis of the results from the Cox regression analysis. Cases were matched to up to three controls with the same level of binary matching variables and the smallest Mahalanobis distance of continuous matching variables. The patients who experienced thromboembolic events and their matched controls were compared in terms of the potential risk factors. Last known laboratory parameters, defined by those measured at the last known visit before event onset, were assessed as the potential factors. The numbers and percentages of patients were calculated for binary and categorical factors by case and matched control group. Conditional logistic regression was used to calculate odds ratios (ORs) for cases compared with matched controls with 95% CIs and P values. More details on the methodology are available in the Methods section of the electronic supplementary material.
Restricted cubic spline regression with three knots was used to model a non-linear association between ORs and last known TSAT, where the reference value was set to 30%.
To further explore the association between roxadustat dose and thromboembolic events, last known roxadustat dose was analyzed using restricted cubic spline regression with three knots for subgroups of patients with TSAT ≥ 30% and TSAT < 30%, where the reference value was set to a lower dose level of 150 mg/week to be consistent with a similar analysis in patients treated in Japan with a lower average roxadustat dose [10].
Results
Overview of Thromboembolic Events
The mean age of patients was 55.5 years. Patients treated with roxadustat had a history of diabetes (43.2%), cardiovascular disease (41.9%), and thromboembolism (4.2%). The mean baseline hemoglobin level was 9.83 g/dL. Most patients were on hemodialysis (90.9%) as opposed to peritoneal dialysis (9.1%). Two-thirds of patients had been on dialysis for more than 4 months (68.0%) (Table 1).
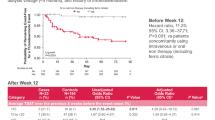
Of the 2354 patients included in this pooled analysis, 1026 thromboembolic events were observed in 568 patients (Fig. 1). There were 154 thromboembolic events that occurred before week 12, and 872 events that occurred after week 12.
Clinical Variables Measured Over Entire Treatment Period
Hemoglobin levels, high-sensitivity C-reactive protein (hsCRP) levels, ferritin levels, and TSAT over the entire treatment period are displayed in Figs. 2 and 3. At most of the time points evaluated, median hemoglobin levels were slightly lower in patients with thromboembolic events compared with those without thromboembolic events. Patients with thromboembolic events had slightly higher median hsCRP levels and lower median TSAT compared with those without thromboembolic events. No notable differences were observed for mean corpuscular volume (MCV) or platelet counts throughout the study period (Fig. S1).
Thromboembolic Events With Onset Before Week 12
Cox Regression Analysis
High body mass index, hemodialysis, history of diabetes, history of cardiovascular disease, low baseline TSAT, and high baseline hsCRP level were associated with increased risk of thromboembolic events (Table S1 in the electronic supplementary material). A racial difference in hazard ratios was observed (Table S1 in the electronic supplementary material).
Multivariate Cox regression analysis for selected factors revealed that hemodialysis (adjusted HR 3.40; 95% CI 1.08–10.74; vs peritoneal dialysis) and high baseline hsCRP (> 0.5 mg/dL: adjusted HR 1.64; 95% CI 1.10–2.43; ≤ 0.5 mg/dL) remained associated with the increased risk of thromboembolic events (Fig. 4a and Table 2).
Nested Case-Control Analysis
The case and control groups were well balanced in terms of matching variables and other baseline characteristics (Table S2 in the electronic supplementary material).
High hemoglobin rate of rise showed a trend towards an increased risk of thromboembolic events (≥ 0.5 g/dL/week: OR 2.09; 95% CI 0.98–4.46; vs − 0.1 to < 0.1 g/dL/week) (Table 3).
Decreased last known TSAT from baseline was associated with increased risk of thromboembolic events (< − 15%: OR 2.76; 95% CI 1.03–7.44; vs ≥ 0%) (Table 4).
Thromboembolic Events With Onset After Week 12
Cox Regression Analysis
Advanced age, Black race, high body mass index, hemodialysis, long dialysis vintage, history of diabetes, history of thromboembolism, history of cardiovascular disease, previous epoetin treatment, ESA conversion, no concomitant iron therapy (oral or IV) use, low baseline ferritin, low baseline TSAT, and high baseline hsCRP were associated with an increased risk of thromboembolic events (Table S1 in the electronic supplementary material).
Multivariate Cox regression analysis for selected factors revealed that advanced age (≥ 65 years: adjusted HR 1.32; 95% CI 1.08–1.62; vs < 65 years), Black race (adjusted HR 1.55, 95% CI 1.22–1.98; vs White race), hemodialysis (adjusted HR 1.72; 95% CI 1.11–2.65; vs peritoneal dialysis), history of diabetes (adjusted HR 1.36; 95% CI 1.11–1.68; vs no history of diabetes), history of thromboembolism (adjusted HR 1.74; 95% CI 1.20–2.53; vs no history of thromboembolism), and history of a cardiovascular event (adjusted HR 1.40; 95% CI 1.15–1.71; vs no history of a cardiovascular event) remained associated with an increased risk of thromboembolic events (Fig. 4b and Table 2).
Nested Case-Control Analysis
The case and control groups were well balanced with respect to matching variables and other baseline characteristics (see Table S3 in the electronic supplementary material).
Univariate conditional logistic regression analyses showed that a high hemoglobin rate of decline, low last known hemoglobin level, low last known TSAT, high last known platelet count, high last known hsCRP, and high last known roxadustat dose were associated with an increased risk of thromboembolic events (Table 5).
Multivariate conditional logistic regression analyses revealed that low last known hemoglobin level (< 10 g/dL: adjusted OR 1.91; 95% CI 1.04–3.50; vs ≥ 12 g/dL) and low last known TSAT (< 10%: adjusted OR 3.78; 95% CI 1.71–8.39; vs ≥ 30%) remained associated with increased risk of thromboembolic events. The multivariate analysis extinguished the significant relationship of platelet count, hsCRP, MCV, and roxadustat dose with thromboembolic events (Table 5).
Restricted cubic spline regression analysis demonstrated that the increased risk of thromboembolic events was observed as last known TSAT declined to < 30% (Fig. 5a). In the subgroup with TSAT < 30%, a higher roxadustat dose was associated with an increased risk of thromboembolic events. However, in the subgroup with TSAT ≥ 30%, no association was observed between roxadustat dose and risk of thromboembolic events (Fig. 5b).
Restricted cubic splines for a last known TSAT and b last known roxadustat dose in subgroups of patients with last known TSAT < 30% and ≥ 30% after week 12. Black line represents the fitted line of a the relationship between the last known TSAT and the estimated odds ratio, and b the relationship between the last known roxadustat dose and the estimated odds ratio. Red dotted lines represent its 95% confidence interval. a The model was adjusted by last known hemoglobin level, log(last known ferritin), last known platelet count, log(last known hsCRP), last known erythrocyte MCV, and last known roxadustat dose. Reference value was set at 30%, including 3 knots. b Reference value was set at 150 mg/week, including 3 knots. hsCRP high-sensitivity C-reactive protein, MCV mean corpuscular volume, TSAT transferrin saturation
Decreases in last known hemoglobin, decreases in last known TSAT, and increases in platelet count from baseline were associated with an increased risk of thromboembolic events (Table 6).
Discussion
This exploratory post hoc analysis found that fluctuations in hemoglobin levels over a relatively short period of time (a trend for hemoglobin rapid increase in the early phase) while hemoglobin decline as well as low Hb levels (< 10 g/dL) in the late phase were associated with thromboembolic events. Low last known TSAT, a marker of circulating iron, was found to be related to thromboembolic events in the late phase. We also confirmed known risk factors for thromboembolic events after week 12, such as advanced age, Black race, and a history of thromboembolism, diabetes, and cardiovascular disease [11,12,13,14].
In the univariate nested case-control analyses, a drop in hemoglobin level (by < − 0.5 g/dL/week), low hemoglobin level (< 10.0 g/dL), low TSAT (< 30%), high platelet count (≥ 30 × 104/µL), high hsCRP level (≥ 1.5 mg/dL), and high roxadustat dose (≥ 600 mg/week) at the last visit before the event were associated with thromboembolic events after week 12. The use of higher doses of roxadustat suggests the presence of other causative factors for anemia, such as inflammation and iron deficiency, which could lead to thrombocytosis [15, 16], and subsequently to thromboembolic events. However, multivariate adjustment extinguished the significant relationship of platelet count, hsCRP level, and roxadustat dose with the events. In contrast, a last known low hemoglobin level and low TSAT level remained significant even after multivariate adjustment. Moreover, a greater decrease of TSAT from baseline (> 15%) was associated with risk of thromboembolic events not only in the late phase but also in the early phase (prior to week 12), after the initiation of roxadustat. Therefore, maintaining circulating iron levels, i.e., preventing iron deficiency, seems to be important for decreasing the risk of events; these results are supported by similar findings from previous population-based studies [17, 18]. Our results expand the KDIGO guidelines recommendation on the use of ESAs that adequate iron stores should be ensured during or prior to treatment [3]. Monitoring iron status as well as hemoglobin levels is recommended in patients with anemia of DD CKD during roxadustat treatment.
The absence of iron therapy was significantly associated with a thromboembolic event after week 12; however, this association was not significant for the events before week 12. In our similar analysis of patients enrolled in clinical trials in Japan who were receiving dialysis and roxadustat, no iron administration was significantly associated with thromboembolic events before week 12 [5,6,7,8, 10, 19, 20]. This difference can be explained by much lower baseline TSAT and ferritin levels in Japanese patients receiving hemodialysis.
Since TSAT is proportional to iron/transferrin, our results align with a report that an increase in transferrin, induced by iron deficiency, is associated with hypercoagulability [21]. The current analysis in patients treated with roxadustat did not find an association between ferritin levels and thromboembolic events. This was in sharp contrast with a report showing that elevated ferritin levels were risk factors for major adverse cardiovascular events (MACE) and all-cause mortality in a hemodialysis population treated with an ESA [22]. This discrepancy probably stems from the different mechanisms of action on erythropoiesis between roxadustat and ESAs. Greater reduction of hepcidin levels by roxadustat as compared to an ESA [19, 23] leads to mobilization of internal iron stores, thereby reducing ferritin levels.
During the later period of treatment, a high roxadustat weekly dose (≥ 600 mg/week) was associated with thromboembolic events in the univariate analysis. However, multivariate adjustment abolished this relationship. Moreover, in a subgroup analysis by last known TSAT value after week 12, this association was diminished in patients with TSAT ≥ 30%. In contrast, in patients with lower iron availability (measured by low TSAT levels < 30%), higher doses were associated with thromboembolic events. Low hemoglobin levels during roxadustat therapy should trigger the investigation for other causes of anemia. In this context, it seems reasonable to prioritize administering iron to maintain TSAT ≥ 30%.
Dialysis vintage was not associated with increased risk of thromboembolic events before week 12. A similar post hoc analysis conducted in patients in Japan observed that patients with CKD who initiated dialysis ≤ 4 months ago had a higher risk for a thromboembolic event before week 12 [10]. Since the thromboembolic events before week 12 in Japanese patients were mostly shunt-related (74%) and shunts for patients in Japan are usually smaller than those of Western patients receiving hemodialysis, these results might be only applicable to patients with small shunts.
This is the first global analysis to explore risk factors for thromboembolic events in patients receiving dialysis and roxadustat. The strengths of our study include that it involved thousands of patients of various races by pooling four randomized, global trials. This enabled us to compare racial differences in the incidence of thromboembolic events. Moreover, an adequate number of thromboembolic events gave us sufficient statistical power to detect risk factors with an OR of < 1.5.
There were some limitations in this study. Owing to the nature of this post hoc analysis of pooled studies, these results should be viewed cautiously as hypothesis-generating. Thrombosis in patients with anemia of CKD is complex and multifactorial, and the analysis may be limited because of confounding, missing data, and clinical correlation between variables such as hemoglobin, iron, and inflammatory markers. The current analysis did not include any comparison data for roxadustat versus ESAs; the safety profiles for ESAs are already established [24,25,26] and a large meta-analysis did not find a significant difference in the incidence of thrombotic events when comparing the use of HIF-PHIs and ESAs in patients with dialysis-dependent and non-dialysis-dependent CKD [27, 28]. Another large meta-analysis suggested a contrasting result that patients treated with HIF-PHIs had a slightly but significantly higher incidence of thrombotic events compared to a combined control group of patients treated with placebo or ESAs, in patients with dialysis-dependent and non-dialysis-dependent CKD [27]. The current pooled analyses were conducted with all thromboembolic events as opposed to a separate analysis of arterial, venous, and shunt-related events, because such event grouping was not available.
Conclusion
Advanced age, Black race, history of thromboembolism or cardiovascular disease, history of diabetes, and high baseline hsCRP are well-established risk factors for thromboembolic events in patients with DD CKD and were confirmed in this post hoc analysis. In addition to established risk factors, high hemoglobin rate of rise (≥ 0.5 g/dL/week) may augment the risk of thromboembolic events at the early period of treatment, highlighting the importance of careful monitoring to prevent too rapid of a rise in hemoglobin when initiating roxadustat treatment. In contrast, a low hemoglobin level (< 10 g/dL) and a decline of hemoglobin (< − 0.5 g/dL/week) were each associated with increased risk of thromboembolic events after week 12. Low TSAT (< 30%) and greater decline of TSAT (> 15%) from baseline were also detected as risk factors for this late period. Failure to achieve the hemoglobin target level should prompt a search for other causative factors; one option may be treating with iron therapy until reaching TSAT ≥ 30%, rather than increasing the dose of roxadustat. The results of this post hoc analysis are supportive of the findings of a similar analysis [10] conducted in patients with DD CKD with anemia in Japan which showed that absence of iron therapy was associated with thromboembolic events.
Data Availability
Researchers may request access to anonymized participant level data, trial level data and protocols from Astellas sponsored clinical trials at www.clinicalstudydatarequest.com. For the Astellas criteria on data sharing see: https://clinicalstudydatarequest.com/Study-Sponsors/Study-Sponsors-Astellas.aspx.
References
Nakhoul G, Simon JF. Anemia of chronic kidney disease: treat it, but not too aggressively. Cleve Clin J Med. 2016;83:613–24.
Locatelli F, Fishbane S, Block GA, Macdougall IC. Targeting hypoxia-inducible factors for the treatment of anemia in chronic kidney disease patients. Am J Nephrol. 2017;45:187–99.
Kidney Disease: Improving Global Outcomes. KDIGO Clinical Practice Guideline for Anemia in Chronic Kidney Disease. Kidney Int Suppl. 2012;2:279–335.
Locatelli F, Barany P, Covic A, et al. Kidney Disease: Improving Global Outcomes guidelines on anemia management in chronic kidney disease: a European Renal Best Practice position statement. Nephrol Dial Transplant. 2013;28:1346–59.
Charytan C, Manllo-Karim R, Martin ER, et al. A randomized trial of roxadustat in anemia of kidney failure: SIERRAS study. Kidney Int Rep. 2021;6:1829–39.
Csiky B, Schomig M, Esposito C, et al. Roxadustat for the maintenance treatment of anemia in patients with end-stage kidney disease on stable dialysis: a European phase 3, randomized, open-label, active-controlled study (PYRENEES). Adv Ther. 2021;38:5361–80.
Fishbane S, Pollock CA, El-Shahawy M, et al. Roxadustat versus epoetin alfa for treating anemia in patients with chronic kidney disease on dialysis: results from the randomized phase 3 ROCKIES study. J Am Soc Nephrol. 2022;33:850–66.
Provenzano R, Shutov E, Eremeeva L, et al. Roxadustat for anemia in patients with end-stage renal disease incident to dialysis. Nephrol Dial Transplant. 2021;36:1717–30.
Chen H, Cheng Q, Wang J, Zhao X, Zhu S. Long-term efficacy and safety of hypoxia-inducible factor prolyl hydroxylase inhibitors in anemia of chronic kidney disease: a meta-analysis including 13,146 patients. J Clin Pharm Ther. 2021;46:999–1009.
Hamano T, Yamaguchi Y, Goto K, et al. Risk factors for thromboembolic events in patients with dialysis-dependent CKD: pooled analysis of phase 3 roxadustat trials in Japan. Adv Ther. 2023.
Molnar AO, Bota SE, McArthur E, et al. Risk and complications of venous thromboembolism in dialysis patients. Nephrol Dial Transplant. 2018;33:874–80.
Anderson F. Risk factors for venous thromboembolism. Circulation. 2003;107:I9–16.
Hsieh MY, Lee CK, Lo CM, et al. Temporal distribution and biological determinants of thrombotic events after interventions for dialysis vascular access. Sci Rep. 2019;9:10720.
Zakai NA, McClure LA. Racial differences in venous thromboembolism. J Thromb Haemost. 2011;9:1877–82.
Streja E, Kovesdy C, Greenland S, et al. Erythropoietin, iron depletion and relative thrombocytosis: a possible explanation for hemoglobin-survival paradox in chronic kidney disease. Am J Kidney Dis. 2008;52:727–36.
Henry DH, Dahl NV, Auerbach MA. Thrombocytosis and venous thromboembolism in cancer patients with chemotherapy induced anemia may be related to ESA induced iron restricted erythropoiesis and reversed by administration of IV iron. Am J Hematol. 2012;87:308–10.
Chang YL, Hung SH, Ling W, et al. Association between ischemic stroke and iron-deficiency anemia: a population-based study. PLoS One. 2013;8:e82952.
Hung SH, Lin HC, Chung SD. Association between venous thromboembolism and iron-deficiency anemia: a population-based study. Blood Coagul Fibrinolysis. 2015;26:368–72.
Chen N, Hao C, Liu BC, et al. Roxadustat treatment for anemia in patients undergoing long-term dialysis. N Engl J Med. 2019;381:1011–22.
Chen N, Hao C, Peng X, et al. Roxadustat for anemia in patients with kidney disease not receiving dialysis. N Engl J Med. 2019;381:1001–10.
Tang X, Fang M, Cheng R, et al. Iron-deficiency and estrogen are associated with ischemic stroke by up-regulating transferrin to induce hypercoagulability. Circ Res. 2020;127:651–63.
Fellstrom B, Eriksson N, Morga A, et al. Assessment of risk factors for cardiovascular events and mortality in dialysis patients in the AURORA study, a retrospective analysis. Nephrol Dial Transplant. 2021. https://doi.org/10.1093/ndt/gfab085.006.
Provenzano R, Besarab A, Wright S, et al. Roxadustat (FG-4592) versus epoetin alfa for anemia in patients receiving maintenance hemodialysis: a phase 2, randomized, 6- to 19-week, open-label, active-comparator, dose-ranging, safety and exploratory efficacy study. Am J Kidney Dis. 2016;67:912–24.
Besarab A. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med. 1998;339:584–90.
Drueke TB. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006;355:2071–84.
Szczech LA, Barnhart HX, Inrig JK, et al. Secondary analysis of the CHOIR trial epoetin-alpha dose and achieved hemoglobin outcomes. Kidney Int. 2008;74:791–8.
Takkavatakarn K, Thammathiwat T, Phannajit J, et al. The impacts of hypoxia-inducible factor stabilizers on laboratory parameters and clinical outcomes in chronic kidney disease patients with renal anemia: a systematic review and meta-analysis. Clin Kidney J. 2023;16:845–58.
Minutolo R, Liberti ME, Simeon V, et al. Efficacy and safety of hypoxia-inducible factor prolyl hydroxylase inhibitors in patients with chronic kidney disease: meta-analysis of phase 3 randomized controlled trials. Clin Kidney J. 2023. https://doi.org/10.1093/ckj/sfad143.
Acknowledgements
We would like to sincerely thank the patients and their family members for their support, as well as the investigators who participated in these trials. We would also like to acknowledge Masataka Morita (Medical Affairs, Astellas Pharma, Inc.), who performed study management, and Tomihisa Kawasaki (Project Management, Development, Astellas Pharma, Inc.), who contributed to study design.
Medical Writing/Editorial Assistance.
Medical writing/editorial support was provided by Lindsay Achzet, PhD, Drayton Hammond, PharmD, and Carol Cadmus, ELS, from Peloton Advantage, LLC, an OPEN Health company, Parsippany, NJ, USA, and funded by the study sponsor, Astellas Pharma, Inc.
Funding
This study was sponsored by Astellas Pharma, Inc. The Rapid Service Fee and the Open Access fee were funded by Astellas Pharma, Inc.
Author information
Authors and Affiliations
Contributions
Study design: Takayuki Hamano, Yusuke Yamaguchi, Tadao Akizawa. Study investigator: Takayuki Hamano, Yusuke Yamaguchi, Kashia Goto, Shaka Martin, Alina Jiletcovici, Frank Dellanna, Tadao Akizawa, Jonathan Barratt. Enrolled patients: Not applicable. Collection and assembly of data: Takayuki Hamano, Yusuke Yamaguchi, Tadao Akizawa. Data analysis: Yusuke Yamaguchi. Data interpretation: All authors. Manuscript preparation: All authors. Manuscript review and revisions: All authors. Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Conflict of Interest
Takayuki Hamano has received grants for physician-initiated research, consulting fees and honoraria for lectures from Astellas Pharma, Inc. Yusuke Yamaguchi is an employee of Astellas Pharma, Inc. Kashia Goto has participated in a company stock ownership plan through Astellas Pharma, Inc. Shaka Martin is an employee of Astellas Pharma, Inc. Alina Jiletcovici has received stock or stock options as a minor shareholder for Eli Lilly and Company and is an employee of Astellas Pharma, Inc. Frank Dellanna has nothing to disclose. Tadao Akizawa has received personal consulting fees from Astellas Pharma, Inc., Kyowa Kirin, Kissei Pharmaceutical, Ono Pharmaceutical, Fuso Pharmaceutical, Torii Pharmaceutical, GlaxoSmithKline, JT Pharmaceutical, Nipro Corporation, Otsuka, Sanwa Kagaku and Bayer and has also received personal payment or honoraria for lectures from Astellas Pharma, Inc., Kyowa Kirin, Kissei Pharmaceutical, Ono Pharmaceutical, Fuso Pharmaceutical I, Torii Pharmaceutical, Chugai Pharmaceutical, Mitsubishi Tanabe, and Bayer. Jonathan Barratt has received fees for invited lectures from Astellas Pharma, Inc.
Ethical Approval
All studies included in this post hoc analysis were conducted in accordance with the ethical principles of the Declaration of Helsinki of 1964 and its later amendments, the International Conference on Harmonisation of Technical Requirements for Pharmaceutical for Human Use guidelines, Good Clinical Practice, and applicable local laws and regulations. As this was a pooled post hoc analysis, approval by an ethics committee for this analysis was not necessary; however, institutional review board approval was obtained prior to initiating each of the included studies. All participants provided written informed consent.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hamano, T., Yamaguchi, Y., Goto, K. et al. Risk Factors for Thromboembolic Events in Patients With Dialysis-Dependent CKD: Pooled Analysis of Four Global Roxadustat Phase 3 Trials. Adv Ther 41, 1553–1575 (2024). https://doi.org/10.1007/s12325-023-02728-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02728-2