Abstract
Introduction
Sodium-glucose cotransporter 2 inhibitors (SGLT2i) have a favorable impact on the kidney function in patients with heart failure (HF), while there is no clear evidence of what factors predict this effect. The aim of the study was to identify plausible predictors for kidney function outcome among patients with HF and investigate their association with SGLT2i.
Methods
We prospectively enrolled 480 patients with type 2 diabetes mellitus (T2DM) treated with diet and metformin and concomitant chronic HF and followed them for 52 weeks. In the study, we determined kidney outcome as a composite of ≥ 40% reduced estimated glomerular filtration rate from baseline, newly diagnosed end-stage kidney disease or kidney replacement therapy. The relevant medical information and measurement of the biomarkers (N-terminal natriuretic pro-peptide, irisin, apelin, adropin, C-reactive protein, tumor necrosis factor-alpha) were collected at baseline and at the end of the study.
Results
The composite kidney outcome was detected in 88 (18.3%) patients of the entire population. All patients received guideline-recommended optimal therapy, which was adjusted to phenotype/severity of HF, cardiovascular risk and comorbidity profiles, and fasting glycemia. Levels of irisin, adropin and apelin significantly increased in patients without clinical endpoint, whereas in those with composite endpoint the biomarker levels exhibited a decrease with borderline statistical significance (p = 0.05). We noticed that irisin ≤ 4.50 ng/ml at baseline and a ≤ 15% increase in irisin serum levels added more valuable predictive information than the reference variable. However, the combination of irisin ≤ 4.50 ng/ml at baseline and ≤ 15% increase in irisin serum levels (area under curve = 0.91; 95% confidence interval = 0.87–0.95) improved the discriminative value of each biomarker alone.
Conclusion
We suggest that low levels of irisin and its inadequate increase during administration of SGLT2i are promising predictors for unfavorable kidney outcome among patients with T2DM and concomitant HF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Positive impact of sodium-glucose cotransporter 2 inhibitors on kidney function in patients with diabetes mellitus and heart failure is variable. |
Worsening kidney function independently affects heart failure outcomes. |
Low irisin serum levels at baseline predicted inadequate improving kidney function during sodium-glucose cotransporter 2 inhibitor administration. |
Low irisin serum levels during treatment added valuable predictive information for poor kidney outcome. |
Introduction
Heart failure (HF) remains one of the leading causes of death among in-patients with known cardiovascular disease (CVD) and chronic kidney disease (CKD) [1]. CKD is associated with poor clinical outcomes in HF regardless of its phenotype and etiology, patient age and comorbidity profile including such confounders as type 2 diabetes mellitus (T2DM) and hypertension [2, 3]. In addition, CKD predicted all-cause and cardiovascular (CV) mortality independently from a presence of HF [4, 5]. Notably, HF and CKD potentiate development and accelerate each other's progression through several common pathophysiologic mechanisms [6]. Cardiac and renal interactions are modulated by inflammatory reactions and cellular immune-mediated mechanisms, biomechanical stress-mediated and neurohumoral responses, changes in metabolic status and impaired hemodynamics [6]. Therefore, there are many unique kidney-specific risk factors including malnutrition, electrolyte and acid-base alterations, bone mineral changes, anemia, uremic toxins and myocardial stunning, which contribute to the decline of kidney function in patients with any HF phenotype [7, 8].
T2DM is a powerful risk factor for both CVD and CKD, which links HF and worsening renal function [9]. However, progression of HF is strongly associated with increased new cases of T2DM as well as T2DM-induced CKD [10, 11]. Conventional management of T2DM including mainly sodium-glucose cotransporter 2 inhibitors (SGLT2i) has been reported to impact clinical events in T2DM patients with HF including all-cause and CV mortality, HF hospitalization and kidney function [12]. Moreover, there is emerging evidence that these agents might be useful even in non-T2DM patients with HF (mainly with reduced [HFrEF] and mildly reduced ejection fraction [HFmrEF] and probably with preserved ejection fraction [HFpEF]) to reduce mortality, HF- and kidney-related events [13, 14].
Although the relationships between improvement of both CV and HF outcomes and the slowed rate of decline in estimated glomerular filtration rate (eGFR) among patients with HF were established in previous clinical studies (the DELIVER [Dapagliflozin and Kidney Outcomes in Patients with Heart Failure with Mildly Reduced or Preserved Ejection Fraction] and EMPA-REG OUTCOME [Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients] trials) [15, 16], there is no clear evidence of what factors predict favorable effect of SGLT2i on kidney function. This is an important clinical question, because in this real-life experience favorable impact of SGLT2i on eGFR and/or albuminuria/proteinuria was noticed in about 30% of the entire patient population and was variable [17]. However, in large clinical trials for SGLT2 inhibitors (EMPA-REG OUTCOME trial [18]; EMPA-KIDNEY trial [19]), numerous variables (i.e., glycated hemoglobin [HbA1c], systolic blood pressure, urea albumin-to-creatinine ratio, hemoglobin, body weight, high- (HDL) and low-density lipoprotein (LDL) cholesterol, uric acid and potassium), which demonstrated their plausible predictive abilities for CV and kidney outcomes, were evaluated. We previously identified the following biomarkers for kidney outcomes: N-terminal natriuretic pro-peptide (NT-proBNP), tumor necrosis factor alpha (TNF-alpha), irisin, apelin, adropin and high-sensitivity C-reactive protein (hs-CRP) [20, 21].
Low-grade inflammatory reaction is a well-known major pathogenic factor, which underlies the association between worsening kidney function/newly diagnosed CKD onset and HF and comorbidity, such as T2DM, abdominal obesity, metabolic abnormalities and atrial fibrillation, through interplay between resident and/or circulating immune cells with renal parenchymal cells [22]. Systemic and local (including microvascular inflammatory) response to kidney injury as well as due to adipose tissue dysfunction reflects the release of pro-inflammatory mediators including CRP and TNF-alpha [23]. They are independently associated with incident HF, progression of the disease and kidney dysfunction [23, 24].
Irisin is a circulating myokine produced in abundance in physiologic conditions by cardiac myocytes and skeletal muscle in response to exercise, whereas several pathophysiologic states, including HF, T2DM, obesity, osteoporosis and CKD, were associated with decreased levels of the hormone in the circulation [25]. Irisin stimulates white adipose tissue cells to induce the browning response, activates thermogenesis, regulates mineral density of bone tissue and cardiac geometry and function, modulates vasodilatation, suppresses inflammation and supports kidney parenchyma survival [26, 27]. Low levels of irisin in chronic HF were found be strong predictors of poor clinical outcomes, hospitalization and death, whereas higher levels of one were noticed in acute myocardial infarction and acute HF I in close connection with CV events [28]. Irisin exerts a tissue-protective effect by supporting the mitochondrial respiration and mitochondrial permeability transition pores, reducing oxidative stresses and apoptosis, protecting against ischemia and reperfusion injury and promoting angiogenesis [29, 30].
Apelin is known as a ligand for the G protein-coupled receptor, which is widely distributed in numerous tissues including heart and kidney [31]. Apelin is involved in pathogenesis of HF, acute kidney injury and CKD through its ability to suppress inflammatory response and modulate proliferation, migration and angiogenesis via nuclear factor-κB (NF-κB) signaling pathway and Akt/extracellular signal-regulated kinase 1 and 2 (ERK1/2) pathway [31, 32]. Apelin-APJ system counteracts the renin-angiotensin-aldosterone system and exerts unique inotropic, anti-apoptotic, anti-ischemic and vasodilatory effects [33, 34]. Low circulating levels of apelin in HFrEF and HFpEF independently predicted the unfavorable clinical outcomes [35, 36]. However, positive impact of conventional management of HF on echocardiographic parameters was closely associated with an increase in serum apelin levels [37].
Adropin is a low-molecular-weight multifunctional peptide produced by various cells and expressed in numerous tissues including heart and kidney [38]. Adropin is considered crucial for energy homeostasis via improving cholesterol metabolism and glucose utilization in mitochondria by improving insulin signaling pathways such as Akt/STAT and glucose transporter 4 receptor activation [38, 39]. Low adropin levels were noticed as an independent risk factor for CV diseases including HF and CKD [40, 41]. The purpose of the study was to identify plausible predictors for kidney function outcome among patients with HF and investigate their association with SGLT2i.
Methods
Patient Population and Study Design
We selected 738 patients with established T2DM from the local database of “Vita Center” (Zaporozhye, Ukraine), composed of > 3500 records of patients with diabetes mellitus and/or HF. Then, we enrolled patients with T2DM with stable HF and well-controlled glycemia. Using inclusion/exclusion criteria, we finally included 489 patients with T2DM and any phenotype of HF (Fig. 1). The study design, basic patient characteristics and primary findings have been previously published [41]. All patients were treated with individually adjusted diet and metformin and had well-controlled T2DM (HbA1c > 6.9%), which did not require insulin therapy. On this occasion, we excluded the patients with T2DM treated with insulin because it previously was found to be a powerful trigger for changes in irisin, adropin and apelin regardless of CKD progression. However, hyperglycemia is the next factor contributing to changes in plasma levels of these biomarkers. Nine patients were excluded from the selection list because of a risk of being lost during the observation period (4 patients with severe ischemia-induced cardiomyopathy, 3 patients with coronary artery bypass grafting and 2 patients with a high risk of symptomatic hypoglycemia). Then, 480 individuals with both T2DM and chronic HF were finally eligible for prospective investigation. The observation period was 52 weeks, during which we pooled objective data of patients and evaluated clinical outcomes.
The study was conducted in close accordance with the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of Zaporozhye Medical Academy of Post-graduate Education (protocol number: 8; date of approval: 10 October 2020). All subjects involved in the study gave their voluntary informed consent.
Collection of Relevant Medical Data and Background Information
Demographic and anthropomorphic data, basic clinical characteristics and comorbidities were collected at baseline. Coronary artery disease [42], CKD [43], HF [44], cardiomyopathies [45], T2DM [46], hypertension [47] and dyslipidemia [48] were evaluated according to current clinical guidelines.
Echocardiography Examination
Echocardiographic and Doppler examinations were performed on all patients by two highly experienced, blinded echocardiographers as described in a previous article [49]. The records were obtained using standard apical two- and four-chamber views at baseline and in 52-week observation intervals. Conventional hemodynamic parameters included left ventricular end-diastolic (LVEDV) and end-systolic (LVESV) volumes, left ventricular ejection fraction (LVEF), left atrial volume (LAV) and LAV to body mass area index, early diastolic blood filling (E) and longitudinal strain ratio (e’) with further calculation of E/e’ index. LVEF was calculated using Simpson's method in line with the recommendation of the American Society of Echocardiography guideline [49]. Left ventricular hypertrophy (LVH) was determined in both sexes according to conventional recommendation [49].
Measurement of Biomarker Levels
The levels of all biomarkers were measured at study entry and 52-week intervals.
Determination of Composite Kidney Outcomes
A previous large clinical study, the EMPA-KIDNEY trial, used the primary outcome for kidney outcome, defined as a composite of 40% decrease in eGFR from baseline, newly diagnosed ESKD (eGFR < 15 ml/min/1.73 m2) or kidney mortality or CV death [50]. In this study, we determined the kidney outcome as a composite of eGFR reduction by 40% from baseline, ESKD or kidney replacement therapy. The eGFR slope was calculated during the observation period as the ratio of change in eGFR from baseline to the end of the study.
Blood Sampling
The blood samples were collected at baseline and at the end of the study. Whole venous blood samples (3–5 ml) were collected in Vacutainer tubes from the fasting patients. Pooled samples were centrifuged (3000 r/min, 30 min); sera were collected and then immediately frozen for further storage at ≤ –70 °C until analysis. All routine biochemical tests were performed using standard biochemical techniques with a Roche P800 analyzer (Basel, Switzerland).
Biomarker Analysis
A total six biomarker levels were evaluated (NT-proBNP, irisin, apelin, adropin, TNF-alpha and hs-CRP). These were quantified in the serum blood samples using commercial enzyme-linked immunosorbent assay (ELISA) kits manufactured by Elabscience (Houston, TX, USA). The intra- and inter-assay coefficients of variation were < 10%.
Glomerular Filtration Rate and Insulin Resistance Determination
Conventional CKD-EPI formula was to estimate the glomerular filtration rate (eGFR) [51]. The Homeostatic Assessment Model of Insulin Resistance (HOMA-IR) was used to evaluate insulin resistance [52].
Statistics
The Kolmogorov-Smirnov test was applied for an evaluation of normality, and the Levene test was used for homogeneity assessment. We presented the continuous variables depending on their distribution as the mean (M) and standard deviation (SD) or median (Me) and 25–75% interquartile range (IQR). Categorical variables were presented as proportions and percentages of the total. The chi-square, Mann-Whitney U and Kruskal-Wallis tests were used to compare the variance depending on their distribution. We calculated Spearman’s correlation coefficient to ascertain the interrelation between variables. Plausible predictors for composite kidney outcome were determined by a univariate logistic regression and backward stepwise multivariate logistic regression. For each predictor, we calculated an odds ratio (OR) and 95% confidence interval (CI). The reliability of predictive models was determined by receiver-operation curve (ROC) analysis along with the calculation of area under the curve (AUC), sensitivity, specificity and likelihood ratio for each predictor. Well-balanced cutoff points for biomarker concentrations were estimated with the Youden test. We compared the incremental prognostic capacities of new biomarkers on a binary predictive model based on estimation of integrated discrimination indices (IDI) and net reclassification improvement (NRI). A two-sided p < 0.05 was considered significant. Variables were tested in V. 23 SPSS (IBM, Armonk, New York, NY, USA) and v. 9 GraphPad Prism (GraphPad Software, San Diego, CA, USA) programs.
Results
The composite kidney outcome (sustained declined in eGFR by 40% from baseline, newly diagnosed ESKD or kidney replacement therapy) was detected in 88 (18.3%) patients of the entire population. Among these individuals, 51 patients demonstrated decline in eGFR by 40% from baseline at the end of the follow-up period, 35 individuals had newly diagnosed ESKD, and consequently two patients required kidney replacement therapy (hemodialysis). For further population analysis, it was divided into two cohorts, respectively (Table 1). However, we did not notice urinary tract infections related to SGLT2 inhibition.
The patient population had median age of 53 (40–67) years and male-to-female proportion of 56.7%/43.3%. The patients had several CV risk factors and concomitant diseases, such as dyslipidemia (80.2%), hypertension (64.0%), stable coronary artery disease (34.6%), any form of atrial fibrillation (21.9%), dilated cardiomyopathy (4.0%), smoking (40.8%), obesity (44.8%), left ventricular (LV) hypertrophy (79.5%) and CKD grade 1–3 (24.6%). Among the patients, 44.2% had HFpEF, 32.5% HFmrEF and 23.3% HFrEF. However, I/II HF NYHA class was detected in 58.6%, and III and IV HF NYHA classes were found in 30% and 11.4% of the patients, respectively. All patients had stable hemodynamics and an average LVEF of 45% (from 34 to 57%) along with moderate dilation of both LV and LV cavities at baseline. Mean LVMMI and LAVI were 138 ± 11 g/m2 and 41 (33–52) ml/m2, respectively. The average eGFR was 74 ± 19 ml/min/1.73 m2; HOMA-IR was 6.95 ± 1.9 units.
All patients received guideline-recommended optimal therapy, which was adjusted to HF phenotype and volemic status, CV risk and comorbidity profiles and fasting glycemia including metformin and diet. The patients from two cohorts did not differ in their age, basic demographics and anthropomorphic parameters. Therefore, we did not notice any differences between the two patient cohorts in presentation of several comorbidities including dyslipidemia, hypertension, dilated cardiomyopathy, abdominal obesity and LV hypertrophy as well as HFmrEF, III HF NYHA class, HOMA-IR, lipid profile and hs-CRP. Contrarily, patients who met the composite endpoint more frequently had stable CAD, paroxysmal/persistent and permanent forms of atrial fibrillation, grade 1–3 CKD, HFrEF and IV HF NYHA class as well as lower HFpEF and I/II HF NYHA class compared with those who did not. However, there were no significant differences between these cohorts in SBP/DBP and LVEF, whereas LVEDV, LVESV, LVMMI, LAVI and E/e` were higher in those with than without the composite endpoint. In addition, individuals with the composite endpoint had higher levels of creatinine, urinary albumin/creatinine ratio, TNF-alpha and NT-proBNP and lower levels of irisin, apelin and adropin than those without the endpoint event. Both cohorts exhibited strict similarity in concomitant medications except for ivabradine, loop diuretics, anticoagulants and statins.
Dynamic Changes in Biomarker Levels in the Patients Included in the Study
Changes in biomarkers levels during the dapagliflozin administration are reported in Fig. 2. We found that hs-CRP decreased non-significantly in individuals with composite endpoint (Δ% = −5.9; from 4.38 mg/l [25–75% IQR = 2.88–7.20 mg/l] to 4.12 mg/l [25–75% IQR = 2.16–6.21 mg/l], p = 0.068), whereas in the patient who did not meet the value we noticed a significant reduction of the concentration (Δ% = −25.3; from 4.10 mg/l [25–75% IQR = 2.35–7.07 mg/l] to 3.06 mg/l [25–75% IQR = 2.07–4.11 mg/l], p = 0.048).
The dynamics of the TNF-alpha levels exhibited strict similarity to hs-CRP. Indeed, in individuals with the composite endpoint, the respective change in levels (Δ%) was −2.4% from 3.37 pg/ml [25–75% IQR = 2.65–4.10 pg/ml] to 3.29 pg/ml [25–75% IQR = 2.55–4.04 pg/ml], p = 0.44), whereas among patients without composite endpoint we found more profound decreases in the concentrations (Δ% = −10.0%; from 2.51 pg/ml [25–75% IQR = 1.52–3.11 pg/ml] to 2.26 pg/ml [25–75% IQR = 1.24–3.34 pg/ml], p = 0.05).
The NT-proBNP levels in peripheral blood significantly decreased (p < 0.001 for all cases) in both cohorts up to 20.1% (from 1625 pmol/ml [25–75% IQR = 860–2240 pmol/ml] to 1285 pmol/ml [25–75% IQR = 578–2006 pmol/ml]) and 24.0% (from 899 pmol/ml [25–75% IQR = 490–1854 pmol/ml] to 683 pmol/ml [25–75% IQR = 375–1089 pmol/ml]), respectively.
Apelin levels increased in both cohorts up to 13.0% (from 3.45 ng/ml [25–75% IQR = 2.17–4.80 ng/ml] to 3.90 ng/ml [25–75% IQR = 2.50–5.54 ng/ml], p = 0.14) and 17.1% (from 5.33 ng/ml [25–75% IQR = 3.34–7.45 ng/ml] to 6.24 ng/ml [25–75% IQR = 4.22–8.16 ng/ml], p = 0.044), respectively.
Levels of irisin significantly (p = 0.012) increased in patients without clinical endpoint (Δ% = + 14.7%, from 6.45 ng/ml [25–75% IQR = 5.21–7.66 ng/ml] to 7.40 ng/ml [25–75% IQR = 6.88–7.92 ng/ml]), whereas in those with composite endpoint the biomarker levels exhibited a decrease in up to 5.1% (from 4.85 ng/ml; 25–75% IQR = 3.32–6.25 ng/ml to 4.60 ng/ml [25–75% IQR = 3.10–5.88 ng/ml]) with borderline statistical significance (p = 0.05).
The levels of adropin in patients who met composite endpoint decreased up to 5.2% (from 2.07 ng/ml [25–75% IQR = 1.80–2.35 ng/ml] to 1.98 ng/ml [25–75% IQR = 1.61–2.27 ng/ml], respectively, p = 0.26). Contrarily, patients without composite endpoint demonstrated parameter growth of about 5.9% (from 2.69 ng/ml [25–75% IQR = 2.10–3.17 ng/ml] to 2.85 ng/ml [25–75% IQR = 2.34–3.11 ng/ml], respectively, p = 0.042).
Spearman’s Correlation Between Biomarker Levels in Peripheral Blood at Baseline and Other Parameters
We established the following associations between variables in the entire patient population (Table 2). Levels of hs-CRP at baseline were positively associated with HF NYHA class, LAVI, HDL-C, body mass index, TNF-alpha and HOMA-IR and negatively correlated with LVEF. There was no sufficient association of hs-CRP with eGFR and urinary albumin/creatinine ratio.
TNF-alpha levels at baseline correlated positively with LAVI, HOMA-IR and hs-CRP and negatively with LVEF. We did not notice significant associations between TNF-alpha levels and age, NT-proBNP, lipid profile, fasting glucose, eGFR and urinary albumin/creatinine ratio.
The NT-proBNP levels were positively associated with HF NYHA class, adropin, E/e’, LAVI and LV hypertrophy and inversely with LVEF, irisin and eGFR.
Irisin levels correlated negatively with NT-proBNP levels, LVEF, HF NYHA class, body mass index, LAVI, fasting plasma glucose, HOMA-IR and HbA1c. We did not find an association of irisin levels with urinary albumin/creatinine ratio.
Apelin levels were negatively associated with LVEF and systolic BP and positively with E/e’, LV hypertrophy, body mass index, HDL cholesterol, HOMA-IR and age. Serum levels of apelin did not correlate with urinary albumin/creatinine ratio and NT-proBNP levels.
The baseline levels of adropin correlated positively with NT-proBNP levels, LAVI, urinary albumin/creatinine ratio, HDL cholesterol and eGFR and negatively with LVEF, chronic HF NYHA class, body mass index, hs-CRP, triglycerides, fasting plasma glucose, HOMA-IR, LDL cholesterol and HbA1c. Adropin levels did not correlate with patient age.
Predictive Value of Circulating Biomarkers for Composite Endpoint in Patients with HF: Results of ROC Curve Analysis
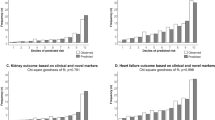
Well-balanced optimal cutoff point for NT-proBNP was detected as 1750 pmol/ml (area under the curve [AUC] = 0.84; 95% CI = 0.74–0.93; sensitivity [Se] = 83.8%, specificity [Sp] = 77.8%; likelihood ratio [LR] = 3.771; p = 0.0001) (Fig. 3).
We found that serum levels of irisin < 4.5 ng/ml predicted composite outcome (AUC = 0.869; 95% CI = 0.82–0.93; Se = 78.3%, Sp = 60.3%; LR = 1.933; p = 0.0001). However, the well-balanced cutoff point of apelin was 3.35 ng/ml (AUC = 0.71; 95% CI = 0.62–0.81; Se = 76.7%, Sp = 84.5%; LR = 5.012; p = 0.0001). The optimal cutoff point of adropin for composite kidney endpoint was 2.1 ng/ml (AUC = 0.87; 95% CI = 0.79–0.94; Se = 82.6%, Sp = 75.0%; LR = 3.304; p = 0.001). TNF-alpha had a cutoff point of 2.95 pg/ml (AUC = 0.73; 95% CI = 0.60–0.88; Se = 85.7%, Sp = 72.4%; LR = 3.107; p = 0.001). Determination of hs-CRP cutoff point was not included in the analysis because there was not a sufficient difference between patient cohorts in the serum levels of these biomarkers.
Predictors for Composite Endpoint in Patients with HF: Uni- and Multivariate Logistic Regression Analysis Adjusted to Urinary Albumin/Creatinine Ratio
In this analysis, we used median value of BMI, age, E/e’ and LAVI as well as cutoff points of baseline levels of NT-proBNP, irisin, adropin, apelin and TNF-alpha, dynamic changes in the biomarkers (decrease in hs-CRP > 25%, in TNF-alpha > 10% and in NT-proBNP > 20%, increase in apelin > 17%, in irisin > 15% and in adropin > 6%) at the end of the study and a presence versus absence of several conditions including treatment with SGLT2i (Table 3).
Univariate logistic regression showed that composite kidney endpoint was predicted by serum levels of NT-proBNP ≥ 1750 pmol/ml (odds ratio [OR] = 1.05; p = 0.044), irisin ≤ 4.5 ng/ml (OR = 1.76; p = 0.001), apelin ≤ 3.35 ng/ml (OR = 1.03; p = 0.046), adropin ≤ 2.10 ng/ml (OR = 1.24; p = 0.001), decrease in NT-proBNP ≤ 20% (OR = 1.07; p = 0.042), increase in irisin ≤ 15% (OR = 1.92; p = 0.001) and in adropin ≤ 6% (OR = 1.37; p = 0.001) as well as E/e’ > 11.0 (OR = 1.06; p = 0.001), LAVI ≥ 41 ml/m2 (OR = 1.08; p = 0.022) and use of SGLT2i (OR = 0.91; p = 0.044).
Multivariate logistic regression revealed that use of SGLT2i (OP = 0.92; p = 0.048), baseline serum levels of irisin ≤ 4.50 ng/ml (OR = 1.51; p = 0.001) and adropin ≤ 2.10 ng/ml (OR = 1.15; p = 0.001) along with and a ≤ 15% increase in the levels of these biomarkers (OR = 1.60; p = 0.001) and ≤ 6% (OR = 1.21; p = 0.001), respectively, remained an independent predictor for composite kidney endpoint.
Comparison of Models
We estimated the AUCs, which revealed that discriminative abilities of irisin ≤ 4.50 ng/ml, adropin ≤ 2.10 ng/ml at baseline and increase in irisin serum levels ≤ 15% were significantly better than the reference predictor (administration of SGLT2i) (Table 4). Moreover, irisin ≤ 4.50 ng/ml at baseline and a ≤ 15% increase in irisin serum levels added more valuable predictive information than the reference variable. However, the combination of irisin ≤ 4.50 ng/ml at baseline and ≤ 15% increase in irisin serum levels (AUC = 0.91; 95% CI = 0.87–0.95) improved the discriminative value of each biomarker alone (AUCirisin = 0.87; 95% CI = 0.82–0.83 and AUCincrease in irisin = 0.89; 95% CI = 0.83–0.96, p < 0.01 for all cases).
Discussion
In this study, we established that decreased levels of irisin (≤ 4.50 ng/ml) and weak increases in it in the circulation (≤ 15% from the baseline level) during SGLT2i administration are likely to be powerful independent predictors of poor kidney outcomes in T2DM patients with any HF phenotype. In addition, we found that the predictive value of irisin was similar to that of adropin, although dynamic changes in irisin in follow-up are considered more valuable compared with the trend of adropin within the same period. Surprisingly, the levels of NT-proBNP at baseline and dynamic changes in the biomarker did not exhibit discriminative potency for kidney outcomes in T2DM patients with HF.
Although previous large clinical trials, which showed SGLT2i efficacy in CKD, yielded many plausible predictors for kidney outcomes, such as body weight, levels of hemoglobin and HbA1c, systolic blood pressure, urea albumin-to-creatinine ratio, HDL cholesterol, LDL cholesterol, serum uric acid and potassium [17,18,19], there was not strong evidence about which of these markers predicted poor kidney outcomes when SGLT2i was administered. In recent post hoc analysis of the randomized EMPEROR-Reduced and EMPEROR-Preserved trials, compared with placebo, SGLT2i empagliflozin reduced HF-related clinical outcomes including hospital admission and CV death regardless of albuminuria levels at baseline as well as diminished progression of microalbuminuria to macroalbuminuria with a slower progressive decline in renal function in patients with chronic HF across a wide range of LVEF regardless of the baseline levels of NT-proBNP [53]. The PARAGON-HF (Prospective Comparison of ARNI with ARB Global Outcomes in HF with Preserved Ejection Fraction) trial showed that patients experiencing HF hospital admission had a significant decline in eGFR directly prior to hospitalization, whereas patients without HF admission had a relatively stable trajectory of eGFR [54]. Overall, there is strong evidence that the eGFR trajectory is associated with HF hospitalization but not with benefits in renal outcomes during HF management [54, 55]. Notably, usually renal function trajectories were similar between the two management arms (active treatment and placebo) and did not correspond to the beneficial effects of agents when HF therapy is guideline recommended [55]. However, pre-specified pooled analysis of combined data from PARADIGM-HF (LVEF ≤ 40%) and PARAGON-HF (LVEF ≥ 45%) showed that sacubitril/valsartan markedly reduced the risk of poor kidney outcomes and slowed declining eGFR compared with valsartan or enalapril alone independent of baseline eGFR in patients with HFrEF and HFpEF [56]. However, the DELIVER (Dapagliflozin Evaluation to Improve the Lives of Patients With Preserved Ejection Fraction Heart Failure) trial showed that baseline UACR or eGFR did not modify the benefit of SGLT2i dapagliflozin on eGFR slope in patients with HFmrEF and HFpEF [15]. Notably, in this trial dapagliflozin was not able to significantly reduce the frequency of the composite kidney outcome, although the overall number of CV deaths or worsening HF was low. Similarly, empagliflozin in the EMPEROR-Preserved trial did not reduce kidney outcome in patients with HF with or without CKD [57]. Finally, UACR, which is an indicator of structural damage of the glomerular filtration barrier, does not provide powerful predictive information on kidney outcomes among patients with HF treated with guideline-recommended therapy [18, 19, 50]. Thus, new promising biomarkers that can predict SGLT2i-related benefit among patients with HF are needed.
We hypothesized the circulating biomarkers, which interfere with cardiac-kidney axis, could play a pivotal role in prediction of worsening kidney function during HF therapy. Indeed, natriuretic peptides (NPs) are not only important biomarkers of biomechanical stress in HF and adverse cardiac remodeling/cardiac hypertrophy with diagnostic and predictive value, but they also protect kidney parenchyma against acute injury and exert adaptive changes in kidney perfusion through vasodilation, regulation of mitochondrial metabolism, glomerular filtration, cell proliferation and migration, apoptosis of glomerular cells, podocytes, endothelial progenitor and mature cells and PDGFR-receptor beta-positive interstitial cells as well as by supporting proximal tubule and capillary integrity [58,59,60]. Overall, NPs have a sufficient protective impact via increasing cyclic guanosine 3’,5’-monophosphate or activation of G-protein, cGMP-dependent protein kinase and sarcoplasmic/endoplasmic reticulum Ca2+-ATPase as a result of binding with their own receptors, which are widely expressed in kidney tissues.
In the study, we did not find that biomarkers such as HbA1c, HOMA-IR, systolic and diastolic BP, HDL cholesterol, LDL cholesterol, serum uric acid and electrolytes, which had been previously reported in some trials as having predictive values for kidney outcomes, had a significant discriminative power for SGLT2i-related kidney function. However, in entire patient population we found that HOMA-IR was higher (6.95 ± 1.9 units) than in other studies such as the Gutenberg Health Study (HOMA-IR = 4.00; IQR 2.52–6.51 units), composed individuals aged 35–74 years with pre-T2DM, T2DM and non-T2DM [61]. In our study, almost 45% of all patients had abdominal obesity, and all included persons had T2DM. Similarly, elevated levels of HOMA-IR may relate not only to these conditions but also to pro-inflammatory activation, which contributed to HF.
Although there is strong evidence that elevated NT-proBNP levels predict poor clinical outcomes in elderly patients with chronic HF within 90 days of acute kidney injury onset and a decreasing trend in the NT-proBNP levels is associated with a lower risk of cardiovascular mortality [62], we did not notice that dynamic changes in NT-proBNP better predicted kidney outcomes in diabetic patients with stable chronic HF than the levels of this biomarker at baseline. Moreover, dynamic trends in irisin and adropin along with baseline levels of the markers led to higher probability for composite kidney endpoints compared with NT-proBNP. On the other hand, hs-CRP and TNF-alpha in hemodynamically stable patients with T2DM who had HF and were at higher risk of newly diagnosed CKD or had established 1–3 stage of CKD were considered insufficient for prediction of kidney outcomes without connection with favorable changes in hemodynamics.
Although other circulating biomarkers, such as irisin, adropin and apelin, were previously found to have anti-inflammatory capabilities, we did not establish sufficient relations between classic inflammatory biomarkers and myokines. Meanwhile, irisin and adropin exhibited significant discriminative ability for composite endpoint, whereas hs-CRP and TNF-alpha did not. These findings require some explanation, perhaps related to the fact that all acute inflammatory phase cytokines showed an increasing trend up to the end of the acute injury stage, stabilizing or declining thereafter [63]. Although the patients with CKD stages 1–3 presented significantly higher levels of hs-CRP and TNF-alpha than patients without CKD, there is no remarkable value of these biomarkers regarding disease progression [63]. Contrarily, a signature of mediatory molecules (irisin, apelin and adropin), which regulate systemic and local inflammatory response, may demonstrate more significant changes in peripheral blood than canonic inflammatory proteins [64]. However, previous clinical studies had found lower levels of adropin, irisin and apelin in patients with HF, T2DM and CKD [29, 30, 32, 36, 38]. Underlying causes that affect levels of adropin, irisin and apelin in T2DM patients with HF are still not clearly understood, while there is a suggestion that pro-inflammatory cytokines and hyperglycemia may negatively influence mRNA expression of these proteins in several target organs including WAT, skeletal muscles, kidney and myocardium [26]. However, increases in plasma levels of these peptides were associated with improved clinical outcomes in individuals with acute myocardial infarction, HF and T2DM [27, 28, 31, 33].
In fact, SGLT2i had a powerful impact on circulating inflammatory mediators, such as CRP and TNF-α [65, 66]. Unfortunately, there is limited evidence regarding an interrelation between changes in inflammatory cytokines and worsening kidney function in T2DM patients with HF treated with SGLT2i [63, 64, 66]. However, the serum levels of irisin may be associated with the presence of albuminuria and reduced eGFR in T2DM patients beyond direct correspondence with the levels of hs-CRP and TNF-α [67]. Finally, an increasing trend in myokines (irisin and apelin) along with elevation of adropin seems to be associated with a stimulatory effect of SGLT2i on sirtuin, which leads to autophagy, ameliorates cellular stress, protects against oxidation and inflammation, and prevents glomerular and tubular injury [68]. This effect is mediated by Na+/H+ exchanger-3 in the kidney, and ketogenesis, which reduces the deteriorating impact of circulating cytokines on kidney parenchyma, thereby protects from worsening kidney function [69].
Another explanation of the findings regarding a positive association between a trend of adropin elevation and lower risk of worsening kidney function is that adropin acts as a suppressor of the tyrosine protein kinase JAK2 (JAK2)/signal transducer and activator of transcription 3 (STAT3) signaling pathway, playing a key role in progression of CKD. For instance, adropin inhibited osteogenic differentiation and the calcification of vascular smooth muscle cells [70]. Thus, SGLT2i, by mediating production of adropin, might prevent accelerating atherosclerosis, worsening kidney parenchyma perfusion and diminish metabolic effects of CKD. Although there are numerous animal and clinical studies on underlying molecular mechanisms of SGLT2i, there is limited clinical evidence, which might elucidate the response of kidney function to SGLT2i and changes in myokine/hepatokine signatures in patients with T2DM who have HF [17, 64, 66, 67].
Taken together, the results of the study first demonstrated that low levels of irisin and adropin at baseline and the increasing trend of their concentrations during the management of HF predicted kidney outcomes significantly better than NT-proBNP and inflammatory proteins. These findings show a need to design and perform novel studies in the near future.
The first study limitation in that we did not concentrate on eGFR slope as a single criterion of renal damage progression and used composite clinical outcome, which included the decrease in eGFR by 40% from baseline, ESKD or kidney replacement therapy. Extending the study follow-up period beyond 52-week observation might be essential for pooling new pre-specified cases and increasing sensitivity of the analysis. However, the sample size of the study was not large enough to separately assay different trends of eGFR in comparison with other biomarkers in connection with clinical kidney endpoints. This issue is considered crucial for large clinical trials in the future. Second, we pre-screened plausible circulating biomarkers, which corresponded to the study's purpose, using the findings from previous large clinical trials as well as our own completed studies. This allowed us to develop a strong system for longitudinal evaluation of biomarker concentrations in follow-up. However, here we did not report a detailed description of cardiac performance changes during 52-week intervals because it would have been too cumbersome. We did not investigate the levels of metabolites and nutrient status at baseline and during follow-up among the patients; however, we recommended following a nutrition plan during the observation period. In addition, the results can only be applied to T2DM patients with well-controlled HbA1c (< 6.9%). Although in this study we evaluated discriminative values of the biomarkers, it remained uncertain whether increased levels of irisin, apelin and adropin were the consequence of improved kidney function and cardiac contractility or increased levels of these hormones, induced by SGLT2i, were causative in preserving heart and kidney function. However, we suggest that irisin seems to be predictive of kidney outcomes in diabetics with HF. We believe that these limitations will not hinder the interpretation of the findings.
Conclusions
The study results revealed that low levels of irisin (≤ 4.50 ng/ml) and its inadequate increase in peripheral blood (≤ 15% from the baseline level) during administration of SGLT2i are promising predictors for unfavorable kidney outcome among T2DM patients with concomitant HF.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Matsushita K, Ballew SH, Wang AY, Kalyesubula R, Schaeffner E, Agarwal R. Epidemiology and risk of cardiovascular disease in populations with chronic kidney disease. Nat Rev Nephrol. 2022;18(11):696–707. https://doi.org/10.1038/s41581-022-00616-6.
Mok Y, Ballew SH, Matsushita K. Chronic kidney disease measures for cardiovascular risk prediction. Atherosclerosis. 2021;335:110–8. https://doi.org/10.1016/j.atherosclerosis.2021.09.007.
Ortiz A, Wanner C, Gansevoort R; ERA Council. Chronic kidney disease as cardiovascular risk factor in routine clinical practice: a position statement by the Council of the European Renal Association. Eur J Prev Cardiol. 2022;29(17):2211–2215. https://doi.org/10.1093/eurjpc/zwac186.
Matsushita K, Kaptoge S, Hageman SHJ, Sang Y, Ballew SH, Grams ME, Surapaneni A, Sun L, Arnlov J, Bozic M, Brenner H, Brunskill NJ, Chang AR, Chinnadurai R, Cirillo M, Correa A, Ebert N, Eckardt KU, Gansevoort RT, Gutierrez O, Hadaegh F, He J, Hwang SJ, Jafar TH, Jassal SK, Kayama T, Kovesdy CP, Landman GW, Levey AS, Lloyd-Jones DM, Major RW, Miura K, Muntner P, Nadkarni GN, Nowak C, Ohkubo T, Pena MJ, Polkinghorne KR, Sairenchi T, Schaeffner E, Schneider MP, Shalev V, Shlipak MG, Solbu MD, Stempniewicz N, Tollitt J, Valdivielso JM, van der Leeuw J, Wang AY, Wen CP, Woodward M, Yamagishi K, Yatsuya H, Zhang L, Dorresteijn JAN, Di Angelantonio E, Visseren FLJ, Pennells L, Coresh J. Including measures of chronic kidney disease to improve cardiovascular risk prediction by SCORE2 and SCORE2-OP. Eur J Prev Cardiol. 2023;30(1):8–16. https://doi.org/10.1093/eurjpc/zwac176.
Li N, Zhang J, Xu Y, Yu M, Zhou G, Zheng Y, Zhou E, He W, Sun W, Xu L, Zhang L. A novel nomogram based on a competing risk model predicting cardiovascular death risk in patients with chronic kidney disease. Front Cardiovasc Med. 2022;9:827988. https://doi.org/10.3389/fcvm.2022.827988.
Schefold JC, Filippatos G, Hasenfuss G, Anker SD, von Haehling S. Heart failure and kidney dysfunction: epidemiology, mechanisms and management. Nat Rev Nephrol. 2016;12(10):610–23. https://doi.org/10.1038/nrneph.2016.113.
Tuegel C, Bansal N. Heart failure in patients with kidney disease. Heart. 2017;103(23):1848–53. https://doi.org/10.1136/heartjnl-2016-310794.
Szlagor M, Dybiec J, Młynarska E, Rysz J, Franczyk B. Chronic kidney disease as a comorbidity in heart failure. Int J Mol Sci. 2023;24(3):2988. https://doi.org/10.3390/ijms24032988.
Damman K, Valente MA, Voors AA, O’Connor CM, van Veldhuisen DJ, Hillege HL. Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J. 2014;35(7):455–69. https://doi.org/10.1093/eurheartj/eht386.
Birkeland KI, Bodegard J, Eriksson JW, Norhammar A, Haller H, Linssen GCM, Banerjee A, Thuresson M, Okami S, Garal-Pantaler E, Overbeek J, Mamza JB, Zhang R, Yajima T, Komuro I, Kadowaki T. Heart failure and chronic kidney disease manifestation and mortality risk associations in type 2 diabetes: a large multinational cohort study. Diabetes Obes Metab. 2020;22(9):1607–18. https://doi.org/10.1111/dom.14074.
Patel RB, Fonarow GC, Greene SJ, Zhang S, Alhanti B, DeVore AD, Butler J, Heidenreich PA, Huang JC, Kittleson MM, Joynt Maddox KE, McDermott JJ, Owens AT, Peterson PN, Solomon SD, Vardeny O, Yancy CW, Vaduganathan M. Kidney function and outcomes in patients hospitalized with heart failure. J Am Coll Cardiol. 2021;78(4):330–43. https://doi.org/10.1016/j.jacc.2021.05.002.
Seferović PM, Coats AJS, Ponikowski P, Filippatos G, Huelsmann M, Jhund PS, Polovina MM, Komajda M, Seferović J, Sari I, Cosentino F, Ambrosio G, Metra M, Piepoli M, Chioncel O, Lund LH, Thum T, De Boer RA, Mullens W, Lopatin Y, Volterrani M, Hill L, Bauersachs J, Lyon A, Petrie MC, Anker S, Rosano GMC. European Society of Cardiology/Heart Failure Association position paper on the role and safety of new glucose-lowering drugs in patients with heart failure. Eur J Heart Fail. 2020;22(2):196–213. https://doi.org/10.1002/ejhf.1673.
Liang B, Li R, Zhang P, Gu N. Empagliflozin for patients with heart failure and type 2 diabetes mellitus: clinical evidence in comparison with other sodium-glucose co-transporter-2 inhibitors and potential mechanism. J Cardiovasc Transl Res. 2023;16(2):327–40. https://doi.org/10.1007/s12265-022-10302-4.
Rao S. Use of sodium-glucose cotransporter-2 inhibitors in clinical practice for heart failure prevention and treatment: beyond type 2 diabetes. A narrative review. Adv Ther. 2022;39(2):845–61. https://doi.org/10.1007/s12325-021-01989-z.
Mc Causland FR, Claggett BL, Vaduganathan M, Desai AS, Jhund P, de Boer RA, Docherty K, Fang J, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Martinez F, Saraiva JFK, McGrath MM, Shah SJ, Verma S, Langkilde AM, Petersson M, McMurray JJV, Solomon SD. Dapagliflozin and kidney outcomes in patients with heart failure with mildly reduced or preserved ejection fraction: a prespecified analysis of the DELIVER randomized clinical trial. JAMA Cardiol. 2023;8(1):56–65. https://doi.org/10.1001/jamacardio.2022.4210.
Kraus BJ, Weir MR, Bakris GL, Mattheus M, Cherney DZI, Sattar N, Heerspink HJL, Ritter I, von Eynatten M, Zinman B, Inzucchi SE, Wanner C, Koitka-Weber A. Characterization and implications of the initial estimated glomerular filtration rate “dip” upon sodium-glucose cotransporter-2 inhibition with empagliflozin in the EMPA-REG OUTCOME trial. Kidney Int. 2021;99(3):750–62. https://doi.org/10.1016/j.kint.2020.10.031.
Capelli I, Ribichini D, Provenzano M, Vetrano D, Aiello V, Cianciolo G, Vicennati V, Tomassetti A, Moschione G, Berti S, Pagotto U, La Manna G. Impact of baseline clinical variables on SGLT2i’s antiproteinuric effect in diabetic kidney disease. Life (Basel). 2023;13(4):1061. https://doi.org/10.3390/life13041061.
Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, Johansen OE, Woerle HJ, Broedl UC, Zinman B; EMPA-REG OUTCOME Investigators. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016; 375(4):323–34. https://doi.org/10.1056/NEJMoa1515920.
EMPA-KIDNEY Collaborative Group. Design, recruitment, and baseline characteristics of the EMPA-KIDNEY trial. Nephrol Dial Transplant. 2022;37(7):1317–29. https://doi.org/10.1093/ndt/gfac040.
Berezin AA, Obradovic AB, Fushtey IM, Berezina TA, Lichtenauer M, Berezin AE. Low plasma levels of irisin predict acutely decompensated heart failure in type 2 diabetes mellitus patients with chronic heart failure. J Cardiovasc Dev Dis. 2023;10:136. https://doi.org/10.3390/jcdd10040136.
Berezin AA, Lichtenauer M, Boxhammer E, Fushtey IM, Berezin AE. Serum levels of irisin predict cumulative clinical outcomes in heart failure patients with type 2 diabetes mellitus. Front Physiol. 2022;13:922775. https://doi.org/10.3389/fphys.2022.922775.
Brennan E, Kantharidis P, Cooper ME, Godson C. Pro-resolving lipid mediators: regulators of inflammation, metabolism and kidney function. Nat Rev Nephrol. 2021;17(11):725–39. https://doi.org/10.1038/s41581-021-00454-y.
Albar Z, Albakri M, Hajjari J, Karnib M, Janus SE, Al-Kindi SG. Inflammatory markers and risk of heart failure with reduced to preserved ejection fraction. Am J Cardiol. 2022;167:68–75. https://doi.org/10.1016/j.amjcard.2021.11.045.
Savic-Radojevic A, Radovanovic S, Pekmezovic T, Pljesa-Ercegovac M, Simic D, Djukic T, Matic M, Simic T. The role of serum VCAM-1 and TNF-α as predictors of mortality and morbidity in patients with chronic heart failure. J Clin Lab Anal. 2013;27(2):105–12. https://doi.org/10.1002/jcla.21570.
Colaianni G, Cinti S, Colucci S, Grano M. Irisin and musculoskeletal health. Ann NY Acad Sci. 2017;1402(1):5–9. https://doi.org/10.1111/nyas.13345.
Berezin AE, Berezin AA, Lichtenauer M. Myokines and heart failure: challenging role in adverse cardiac remodeling, myopathy, and clinical outcomes. Dis Markers. 2021;2021:6644631. https://doi.org/10.1155/2021/6644631.
Ho MY, Wang CY. Role of irisin in myocardial infarction, heart failure, and cardiac hypertrophy. Cells. 2021;10(8):2103. https://doi.org/10.3390/cells10082103.
Hsieh IC, Ho MY, Wen MS, Chen CC, Hsieh MJ, Lin CP, Yeh JK, Tsai ML, Yang CH, Wu VC, Hung KC, Wang CC, Wang CY. Serum irisin levels are associated with adverse cardiovascular outcomes in patients with acute myocardial infarction. Int J Cardiol. 2018;261:12–7. https://doi.org/10.1016/j.ijcard.2017.11.072.
Wang Z, Chen K, Han Y, Zhu H, Zhou X, Tan T, Zeng J, Zhang J, Liu Y, Li Y, Yao Y, Yi J, He D, Zhou J, Ma J, Zeng C. Irisin protects heart against ischemia-reperfusion injury through a SOD2-dependent mitochondria mechanism. J Cardiovasc Pharmacol. 2018;72(6):259–69. https://doi.org/10.1097/FJC.0000000000000608.
Liao Q, Qu S, Tang LX, Li LP, He DF, Zeng CY, Wang WE. Irisin exerts a therapeutic effect against myocardial infarction via promoting angiogenesis. Acta Pharmacol Sin. 2019;40(10):1314–21. https://doi.org/10.1038/s41401-019-0230-z.
Wang X, Zhang L, Li P, Zheng Y, Yang Y, Ji S. Apelin/APJ system in inflammation. Int Immunopharmacol. 2022;109:108822. https://doi.org/10.1016/j.intimp.2022.108822.
Cheng J, Luo X, Huang Z, Chen L. Apelin/APJ system: a potential therapeutic target for endothelial dysfunction-related diseases. J Cell Physiol. 2019;234(8):12149–60. https://doi.org/10.1002/jcp.27942.
Goidescu CM, Vida-Simiti LA. The apelin-APJ system in the evolution of heart failure. Clujul Med. 2015;88(1):3–8. https://doi.org/10.15386/cjmed-380.
Li Y, Lu H, Xu W, Shang Y, Zhao C, Wang Y, Yang R, Jin S, Wu Y, Wang X, Teng X. Apelin ameliorated acute heart failure via inhibiting endoplasmic reticulum stress in rabbits. Amino Acids. 2021;53(3):417–27. https://doi.org/10.1007/s00726-021-02955-3.
Goidescu CM, Chiorescu RM, Diana ML, Mocan M, Stoia MA, Anton FP, Farcaş AD. ACE2 and apelin-13: biomarkers with a prognostic value in congestive heart failure. Dis Mark. 2021;2021:5569410. https://doi.org/10.1155/2021/5569410.
Berezin AA, Fushtey IM, Berezin AE. Discriminative utility of apelin-to-NT-pro-brain natriuretic peptide ratio for heart failure with preserved ejection fraction among type 2 diabetes mellitus patients. J Cardiovasc Dev Dis. 2022;9(1):23. https://doi.org/10.3390/jcdd9010023.
Berezin AA, Fushtey IM, Berezin AE. The effect of SGLT2 inhibitor dapagliflozin on serum levels of apelin in T2DM patients with heart failure. Biomedicines. 2022;10(7):1751. https://doi.org/10.3390/biomedicines10071751.
Ali II, D’Souza C, Singh J, Adeghate E. Adropin’s role in energy homeostasis and metabolic disorders. Int J Mol Sci. 2022;23(15):8318. https://doi.org/10.3390/ijms23158318.
Ghoshal S, Stevens JR, Billon C, Girardet C, Sitaula S, Leon AS, Rao DC, Skinner JS, Rankinen T, Bouchard C, Nuñez MV, Stanhope KL, Howatt DA, Daugherty A, Zhang J, Schuelke M, Weiss EP, Coffey AR, Bennett BJ, Sethupathy P, Burris TP, Havel PJ, Butler AA. Adropin: an endocrine link between the biological clock and cholesterol homeostasis. Mol Metab. 2018;8:51–64. https://doi.org/10.1016/j.molmet.2017.12.002.
Yosaee S, Soltani S, Sekhavati E, Jazayeri S. Adropin—a novel biomarker of heart disease: a systematic review article. Iran J Public Health. 2016;45(12):1568–76.
Berezina TA, Obradovic Z, Boxhammer E, Berezin AA, Lichtenauer M, Berezin AE. Adropin predicts chronic kidney disease in type 2 diabetes mellitus patients with chronic heart failure. J Clin Med. 2023;12(6):2231. https://doi.org/10.3390/jcm12062231.
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, Prescott E, Storey RF, Deaton C, Cuisset T, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407–77. https://doi.org/10.1093/eurheartj/ehz425.
de Boer IH, Khunti K, Sadusky T, Tuttle KR, Neumiller JJ, Rhee CM, Rosas SE, Rossing P, Bakris G. Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association (ADA) and Kidney Disease: Improving Global Outcomes (KDIGO). Diabetes Care. 2022;45:3075–90. https://doi.org/10.2337/dci22-0027.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O et al; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021; 42, 3599–3726. https://doi.org/10.1093/eurheartj/ehab368.
Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, Hagege AA, Lafont A, Limongelli G, Mahrholdt H, McKenna WJ, Mogensen J, Nihoyannopoulos P, Nistri S, Pieper PG, Pieske B, Rapezzi C, Rutten FH, Tillmanns C, Watkins H. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(39):2733–79. https://doi.org/10.1093/eurheartj/ehu284.
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care 2021; 44 (Suppl. S1), S15–S33. https://doi.org/10.2337/dc21-S002.
Williams B, Mancia G, Spiering W, AgabitiRosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104. https://doi.org/10.1093/eurheartj/ehy339.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, Chapman MJ, De Backer GG, Delgado V, Ference BA, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–88. https://doi.org/10.1093/eurheartj/ehz455.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314. https://doi.org/10.1016/j.echo.2016.01.011.
The EMPA-KIDNEY Collaborative Group; Herrington WG, Staplin N, Wanner C, Green JB, Hauske SJ, Emberson JR, Preiss D, Judge P, Mayne KJ, Ng SYA, Sammons E, Zhu D, Hill M, Stevens W, Wallendszus K, Brenner S, Cheung AK, Liu ZH, Li J, Hooi LS, Liu W, Kadowaki T, Nangaku M, Levin A, Cherney D, Maggioni AP, Pontremoli R, Deo R, Goto S, Rossello X, Tuttle KR, Steubl D, Petrini M, Massey D, Eilbracht J, Brueckmann M, Landray MJ, Baigent C, Haynes R. Empagliflozin in patients with chronic kidney disease. N Engl J Med. 2023; 388(2):117–127. https://doi.org/10.1056/NEJMoa2204233.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12. https://doi.org/10.7326/0003-4819-150-9-200905050-00006.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9. https://doi.org/10.1007/BF00280883.
Ferreira JP, Zannad F, Butler J, Filippatos G, Pocock SJ, Brueckmann M, Steubl D, Schueler E, Anker SD, Packer M. Association of empagliflozin treatment with albuminuria levels in patients with heart failure: a secondary analysis of EMPEROR-pooled. JAMA Cardiol. 2022;7(11):1148–59. https://doi.org/10.1001/jamacardio.2022.2924.
Chatur S, Vaduganathan M, Peikert A, Claggett BL, McCausland FR, Skali H, Pfeffer MA, Beldhuis IE, Kober L, Seferovic P, Lefkowitz M, McMurray JJV, Solomon SD. Longitudinal trajectories in renal function before and after heart failure hospitalization among patients with heart failure with preserved ejection fraction in the PARAGON-HF trial. Eur J Heart Fail. 2022;24(10):1906–14. https://doi.org/10.1002/ejhf.2638.
Voors AA, Mulder H, Reyes E, Cowie MR, Lassus J, Hernandez AF, Ezekowitz JA, Butler J, O'Connor CM, Koglin J, Lam CSP, Pieske B, Roessig L, Ponikowski P, Anstrom KJ; Armstrong PW; VICTORIA Study Group. Renal function and the effects of vericiguat in patients with worsening heart failure with reduced ejection fraction: insights from the VICTORIA (Vericiguat Global Study in Subjects with HFrEF) trial. Eur J Heart Fail. 2021;23(8):1313–1321. https://doi.org/10.1002/ejhf.2221.
Mc Causland FR, Lefkowitz MP, Claggett B, Packer M, Senni M, Gori M, Jhund PS, McGrath MM, Rouleau JL, Shi V, Swedberg K, Vaduganathan M, Zannad F, Pfeffer MA, Zile M, McMurray JJV, Solomon SD. Angiotensin-neprilysin inhibition and renal outcomes across the spectrum of ejection fraction in heart failure. Eur J Heart Fail. 2022;24(9):1591–8. https://doi.org/10.1002/ejhf.2421.
Sharma A, Ferreira JP, Zannad F, Pocock SJ, Filippatos G, Pfarr E, Petrini M, Kraus BJ, Wanner C, Packer M, Butler J, Anker SD. Cardiac and kidney benefits of empagliflozin in heart failure across the spectrum of kidney function: insights from the EMPEROR-preserved trial. Eur J Heart Fail. 2023. https://doi.org/10.1002/ejhf.2857.
Okamoto R, Ali Y, Hashizume R, Suzuki N, Ito M. BNP as a major player in the heart-kidney connection. Int J Mol Sci. 2019;20(14):3581. https://doi.org/10.3390/ijms20143581.
Santos-Araújo C, Leite-Moreira A, Pestana M. Clinical value of natriuretic peptides in chronic kidney disease. Nefrologia. 2015;35(3):227–33. https://doi.org/10.1016/j.nefro.2015.03.002.
Heinl ES, Broeker KA, Lehrmann C, Heydn R, Krieger K, Ortmaier K, Tauber P, Schweda F. Localization of natriuretic peptide receptors A, B, and C in healthy and diseased mouse kidneys. Pflugers Arch. 2023;475(3):343–60. https://doi.org/10.1007/s00424-022-02774-9.
Matli B, Schulz A, Koeck T, Falter T, Lotz J, Rossmann H, Pfeiffer N, Beutel M, Münzel T, Strauch K, Wild PS, Lackner KJ. Distribution of HOMA-IR in a population-based cohort and proposal for reference intervals. Clin Chem Lab Med. 2021;59(11):1844–51. https://doi.org/10.1515/cclm-2021-0643.
Hou J, Zhang X, Wu Z, Liu Y, Zhang Y, Zhao J, Wang X, Chen H, Yang G, Ma Q, Cheng Q, Ao Q. Association of serum N-terminal pro-brain natriuretic peptide levels with survival and renal outcomes among elderly patients with acute kidney injury in chronic heart failure. Front Cardiovasc Med. 2023;10:1104787. https://doi.org/10.3389/fcvm.2023.1104787.
Lousa I, Belo L, Valente MJ, Rocha S, Preguiça I, Rocha-Pereira P, Beirão I, Mira F, Alves R, Reis F, Santos-Silva A. Inflammatory biomarkers in staging of chronic kidney disease: elevated TNFR2 levels accompanies renal function decline. Inflamm Res. 2022;71(5–6):591–602. https://doi.org/10.1007/s00011-022-01574-2.
Formigari GP, Dátilo MN, Vareda B, Bonfante ILP, Cavaglieri CR, Lopes de Faria JM, Lopes de Faria JB. Renal protection induced by physical exercise may be mediated by the irisin/AMPK axis in diabetic nephropathy. Sci Rep. 2022;12(1):9062. https://doi.org/10.1038/s41598-022-13054-y.
Sun W, Xing Y, Kong D, Zhang Z, Ma H, Yang L. Meta-analysis of the effect of sodium-dependent glucose transporter 2 inhibitors on C-reactive protein in type 2 diabetes. Medicine (Baltimore). 2022;101(38):e30553. https://doi.org/10.1097/MD.0000000000030553.
Cao Y, Liang N, Liu T, Fang J, Zhang X. Effect of SGLT2 inhibitors and metformin on inflammatory and prognostic biomarkers in type 2 diabetes patients. Endocr Metab Immune Disord Drug Targets. 2023;23(4):530–47. https://doi.org/10.2174/1871530322666220827150054.
Wang R, Liu H. Association between serum irisin and diabetic nephropathy in patients with type 2 diabetes mellitus: a meta-analysis. Horm Metab Res. 2021;53(5):293–300. https://doi.org/10.1055/a-1475-4444.
Huang K, Luo X, Liao B, Li G, Feng J. Insights into SGLT2 inhibitor treatment of diabetic cardiomyopathy: focus on the mechanisms. Cardiovasc Diabetol. 2023;22(1):86. https://doi.org/10.1186/s12933-023-01816-5.
Deschaine B, Verma S, Rayatzadeh H. Clinical evidence and proposed mechanisms of sodium-glucose cotransporter 2 inhibitors in heart failure with preserved ejection fraction: a class effect? Card Fail Rev. 2022;8:e23. https://doi.org/10.15420/cfr.2022.11.
Wang L, Jin F, Wang P, Hou S, Jin T, Chang X, Zhao L. Adropin inhibits vascular smooth muscle cell osteogenic differentiation to alleviate vascular calcification via the JAK2/STAT3 signaling pathway. Biomed Res Int. 2022;2022:9122264. https://doi.org/10.1155/2022/9122264.
Acknowledgements
We thank all patients who gave their voluntary consent to participate in the study and all administrative staff and doctors of the Private Hospital “Vita-Center” for valuable study assistance.
Funding
This research received no external funding. The journal’s fee was waived.
Author information
Authors and Affiliations
Contributions
Conceptualization, Tetiana A. Berezina and Alexander E. Berezin; methodology, Alexander E. Berezin; software, Alexander A. Berezin; validation, Alexander E. Berezin; Ivan M. Fushtey; formal analysis, Tetiana A. Berezina, Alexander A. Berezin; investigation, Tetiana A. Berezina, Alexander A. Berezin; resources, Alexander E. Berezin and Tetiana A. Berezina.; writing—original draft preparation, Alexander A. Berezin; Ivan M. Fushtey; Tetiana A. Berezina; Sergii V. Pavlov and Alexander E. Berezin; visualization, Alexander A. Berezin and Tetiana A. Berezina; supervision, Alexander E. Berezin; project administration, Alexander A. Berezin. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors of the paper (Tetiana A. Berezina, Ivan M. Fushtey, Alexander A. Berezin, Sergii V. Pavlov and Alexander E. Berezin) declare no conflict of interest.
Ethical Approval
The study was conducted in close accordance with the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of Zaporozhye Medical Academy of Post-graduate Education (protocol number: 8; date of approval: 10 October 2020). All subjects involved in the study gave their voluntary informed consent.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Berezina, T.A., Fushtey, I.M., Berezin, A.A. et al. Predictors of Kidney Function Outcomes and Their Relation to SGLT2 Inhibitor Dapagliflozin in Patients with Type 2 Diabetes Mellitus Who Had Chronic Heart Failure. Adv Ther 41, 292–314 (2024). https://doi.org/10.1007/s12325-023-02683-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02683-y