Abstract
Introduction
Low health literacy (HL) is consistently associated with worse health outcomes. Routine clinical screening with available instruments is impractical because of added time and effort. Prior findings suggested that signature time may be a reliable alternative measure of HL among general medicine patients.
Methods
Our aim was to assess the screening performance of signature time and explore optimal thresholds for identifying patients with limited HL in a chronically anticoagulated population. English-speaking patients receiving long-term anticoagulation therapy were recruited. HL was assessed using the Short Test of Functional Health Literacy in Adults (STOFHLA). Signature time was measured using a stopwatch. Logistic regression models and receiver-operating characteristic (ROC) curves were used to evaluate the association and accuracy of signature time compared to HL, respectively.
Results
Of 139 enrolled patients, mean age was 60.1 years, 70.5% were African-American, 48.9% reported < $25,000 income, and 27.3% had marginal or inadequate HL. Overall, median time to sign was 6.1 s. Signature time was longest with inadequate HL (median 9.5 s) compared to adequate HL (5.7 s; p < 0.01). Longer signature time was significantly associated with lower HL after adjusting for age and education (aOR 0.77, 95% CI: 0.68–0.88, p < 0.01). Signature time demonstrated high accuracy (area under the curve [AUC] > 0.8) in identifying HL levels. Thresholds of 5.1 s and 9.0 s showed appropriate screening performance in distinguishing patients with adequate vs. marginal and marginal vs. inadequate HL, respectively.
Conclusion
Signature time demonstrated strong screening performance and may offer a quick and practical approach to assessing HL among patients receiving long-term anticoagulation management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out the study? |
Limited health literacy is rarely evaluated in clinical practice because of several factors including time and resource constraints and potential stigmatization of patients |
Urban low-income patients with limited health literacy are more likely to suffer life-threatening complications such as bleeding and clotting events |
What was learned from the study? |
Longer signature time showed high accuracy in identifying patients with limited health literacy |
Patients who require > 9 s to sign clinic documents are more likely to have limited health literacy |
Signature time may offer a quick and practical option for routine health literacy screening |
Introduction
Health literacy (HL) is the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions [1]. A third of US adults are estimated to have low HL [2]. Patients with limited HL tend to have higher hospitalizations, worse medication adherence, lower preventative care use and poorer ability to interpret medical information [3, 4]. Low HL is also associated with worse overall health status and higher all-cause mortality [3]. Patients who are older, have lower income, limited education and multiple chronic conditions, and are non-native English speakers are more likely to have limited HL [5,6,7]. While previous studies explored HL in the general US population, little is known about the state of HL in minority, urban and low-income populations [6, 7]. These same populations are among those most impacted by health disparities and social determinants of health.
Over 4 million people in the US and 7 million worldwide receive long-term anticoagulation management to prevent and treat thromboembolic complications of atrial fibrillation (AF) and venous thromboembolism (VTE) [8]. Anticoagulation management with traditional agents such as warfarin is complex and requires close patient follow-up, frequent monitoring and continuous dose optimization [9, 10]. This is primarily due to warfarin’s unpredictable pharmacologic profile, narrow therapeutic index and significant drug and food interactions [9, 10].
Patients with limited HL are more likely to have suboptimal anticoagulation control, which increases their risk for life-threatening complications such as bleeding and clotting events [11,12,13,14]. Poor HL is also associated with limited anticoagulation-related knowledge and medication non-compliance [12,13,14,15]. Therefore, routine HL screening is essential in this population to assess patients’ understanding of medical information, encourage shared decision-making and ensure optimal health outcomes [16].
Several well-accepted and validated HL measures have been developed and used in research including Short Test of Functional Health Literacy in Adults (S-TOFHLA), Rapid Estimate of Adult Literacy in Medicine (REALM) and Single Item Literacy Screener (SILS) [17]. Implementing routine HL screening in busy clinical practice can be time consuming and resource intensive [17]. While S-TOFHLA, REALM and SILS have been translated to other languages, limited data exist on their validity across various non-English-speaking populations [17]. Evaluating HL with longer instruments can be embarrassing and stigmatizing to some patients [17, 18]. While brief single item measures such as SILS can reduce the stigma, there is potential for bias due to patient self-report [17]. Providers tend to overestimate HL when relying on sociodemographic proxies such as education level and/or employment status [19]. Lastly, there is a paucity of evidence supporting the screening performance of HL measures that can be implemented in routine clinical management of patients receiving long-term anticoagulation.
To overcome barriers for widespread screening, there is a need for quick, objective, less-stigmatizing and easy-to-administer HL measure [20]. Emerging evidence suggests that signature time may be a reliable, alternative option for HL screening [21]. Signature time is defined as the amount of time a person requires to sign their name on health-related documents [21]. To our knowledge, evidence evaluating signature time as a measure of HL has not been replicated to date in a population receiving long-term anticoagulation management. This study was conducted to evaluate the relationship between signature time and HL in an urban, low-income population receiving long-term anticoagulation management. Our aim was to assess the screening performance of signature time and explore optimal thresholds for identifying patients with limited HL.
Methods
Study Design and Participants
A prospective observational study was conducted at an urban outpatient antithrombosis clinic. Patients were prescreened for eligibility using Electronic Health Records (EHR) and enrolled over a 6-month period during regularly scheduled clinic appointments. Eligible patients were English-speaking adults (21 years and older), had history of receiving anticoagulation management with warfarin for a minimum of 3 months and expected to be on warfarin for a minimum of 6 months after enrollment. Patients with terminal diagnosis, life expectancy < 6 months, legal blindness, deafness, dementia, serious cognitive impairment or serious mental illness were excluded. Study measures were collected by two research assistants (RAs) using patient report and Electronic Health Record (EHR) data abstraction. All participants provided written informed consent and HIPAA authorization. Participants received $10 compensation. The study was approved by the institutional review board of the University of Illinois at Chicago.
Study Measures
HL was evaluated at study enrollment visit using the S-TOFHLA instrument [22]. S-TOFHLA is a 7-min, 36-item measure, developed to evaluate health literacy and numeracy based on reading short paragraphs of medical information and responding to relevant questions. S-TOFHLA demonstrated strong reliability with Cronbach alpha of 0.97 [22]. S-TOFHLA has strong support for construct validity based on another HL measure (REALM) [22]. Patients were classified into three levels of health literacy based on S-TOFHLA: inadequate (total score: 0–16), marginal (total score: 17–22) and adequate (total score: 23–36). HL was captured as total continuous score, three-level categorical (inadequate, marginal, adequate) and dichotomous categorical (adequate versus marginal plus inadequate; adequate plus marginal versus inadequate).
Signature time was operationally defined as the time between the pen touching the paper to provide a signature and the pen being lifted off of the paper at the end of the signature [21]. Signature time was measured by RAs using a stopwatch in the large pocket of a white laboratory coat. This was done to prevent calling patients’ attention to the fact that they were being timed, which might lead patients to modify their signature speed. To prevent concerns of deception, patients were informed during the consent process that their signature time would be captured without their knowing as part of the research study. Formal training on signature time measurement was provided to RAs to ensure standardized measurement. As part of the training, a non-commercial computer software program was used to measure the amount of time a stylus was applied on the tablet screen when people signed their name. This was used as an objective measure of signature time. At the same time, RAs measured the signature time using a stopwatch in their pocket. RAs were required to practice with a minimum of ten different people comparing the computer measured signature time with the time they captured on the stopwatch, and inter-rater reliabilities were calculated as an assessment of accuracy. Practice was required until consistencies between the signature time on the stopwatch and computer measured time had a kappa coefficient ≥ 0.90. All RAs completed this process and achieved reliability before recruiting or consenting participants.
Signature time was captured for each participant at two times during enrollment visits: first when they signed the consent form and second when they signed the HIPPA form. For analyses, signature times were averaged and reported in seconds. Other study covariates were assessed at the enrollment visit and included sociodemographic factors, comorbid conditions, medication history and laboratory data.
Statistical Analyses
Proportional odds logistic regression models with odds ratios (OR) and 95% confidence intervals (CI) were utilized to evaluate the association between signature time and health literacy. For proportional odds models, signature time was treated as independent (predictor) variable and three-level health literacy as a dependent (outcome) variable. This was done to replicate a clinical scenario where someone can unobtrusively assess signature time to get a sense of which patients have limited HL without formally integrating the HL measure. Assessing screening accuracy and determining thresholds for signature time to predict HL requires using logistic regression models. These models require the outcome variable to be categorical. HL literacy (measured by STOFHLA) has predetermined categorical thresholds (adequate, marginal, inadequate). Hence, signature time was modeled as predictor and HL as outcome variable. Two receiver-operating characteristic (ROC) curves were computed to assess the screening performance of signature time as a measure of health literacy with S-TOFHLA score treated as the gold standard. ROC curves also evaluated optimal signature time thresholds. First ROC evaluated cutoffs between the highest and middle levels (adequate vs. marginal plus inadequate) and second evaluated cutoffs between the top two and lowest levels (adequate plus marginal vs. inadequate). Screening performance measures were estimated including diagnostic OR with 95% CI, area under the curve (AUC), sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV). Optimal signature time thresholds were selected based on cutoffs with the highest Youden Index (longest distance from uninformative decision line AUC = 0.5) and lowest distance to perfect prediction point (AUC = 1) [23]. SAS macro %rocplot was used to compute ROC curves, optimal thresholds and screening performance measures [24]. Logistic regression models and ROC curves were adjusted for potential confounders. Confounders were defined as factors leading to a ≥ 10% relative change in the effect estimate in univariate analysis. All analyses were conducted using SAS v9.4.
Results
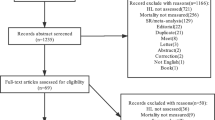
A total of 366 patients fulfilled the inclusion criteria based on initial EHR review (Fig. 1). Major reasons for ineligibility included inadequate anticoagulation duration, being non-English speaking and having serious mental or physical impairments. About 48.3% of eligible patients were approached for inclusion during regularly scheduled clinic appointments over the 6-month enrollment period. The remainder of eligible patients (51.7%) did not present for their regularly scheduled appointments and could not be approached for participation. Of 144 who consented to participate in the study, 139 patients were included in the final analytic sample after excluding patients with missing HL and/or signature time assessments. Several continuous variables did not conform with normal distribution. Therefore, results are presented in medians and IQR for continuous variables.
Of 139 included patients, mean age was 60.1 years, 70.5% were African-American, and 48.9% reported ≤ $25,000 income (Table 1). Most patients (44.6%) reported high school diploma, and 40.3% indicated college degree or equivalent. In terms of medical history, 63% of patients had moderate to severe comorbidity burden and were taking an average of 10.8 prescription medications. Length of anticoagulation management with warfarin was 6.4 years on average. Major reasons for anticoagulation management included VTE (43.9% deep vein thrombosis; 29.5% pulmonary embolism) and AF (30.9%).
Of 139 included patients, 72.7%, demonstrated adequate HL, 7.9% were marginal, and 19.4% were inadequate (Fig. 2). Median (IQR) signature time was 6.1 s (4.7, 8.7). Signature time was moderately correlated with S-TOFHLA total score (r = – 0.38, p < 0.01). Known-group comparisons of signature time by HL level showed significantly longer times for patients with inadequate HL (median 9.5 s) compared to patients with adequate HL (median 5.7 s) (p < 0.01). The difference in signature time for patients with marginal HL vs. each of adequate or inadequate HL was about 2 s; however, this difference did not reach statistical significance. Longer signature time was significantly associated with lower HL based on crude proportional odds regression model (OR: 0.76, 95% CI: 0.67, 0.86, p < 0.01) and model adjusted for age and education level (OR: 0.77; 95% CI: 0.68, 0.88; p < 0.01) (Table 2). Age and education level led to ≥ 10% change in univariate OR and therefore was included in adjusted models. The proportional odds assumption by different levels of HL was not satisfied for age. Therefore, partial proportional odds models were generated to account for non-proportional odds by patient age [25].
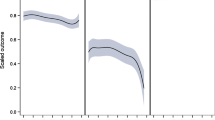
ROC curves were computed to evaluate the screening performance of signature time using logistic regression models adjusted for age and education level (Table 3). Signature time demonstrated good screening performance in differentiating between patients with adequate versus marginal plus inadequate HL (AUC: 0.82, diagnostic OR: 0.79; 95% CI: 0.69, 0.90). Similar performance was observed in distinguishing between patients with adequate plus marginal versus inadequate HL (AUC: 0.83; diagnostic OR: 0.76; 95% CI: 0.65, 0.88). Analysis of optimal signature time thresholds indicated 5.1 s as cutoff between adequate and marginal HL and 9.0 s as cutoff between marginal and inadequate HL. Screening performance of optimal thresholds ranged as follows: sensitivity 82–84%, specificity 81–84%, PPV 93–95% and NPV 54–64%.
Discussion
In a population of low-income minority patients, with high comorbidity burden and long-term anticoagulation management, longer signature time was significantly associated with poorer HL. Signature time demonstrated high accuracy, sensitivity and specificity in distinguishing between higher and lower HL levels as measured by S-TOFHLA. Patients who required < 5 s to sign their name were more likely to have adequate HL. Similarly, patients with signature time > 9 s were more likely to be at inadequate HL level. Our findings are consistent with a previous study by Sharp and colleagues reporting high accuracy of signature time in predicting REALM HL levels in a population of inner city internal medicine patients [21]. This study expands the evidence base for the accuracy of signature time in predicting S-TOFHLA HL levels and in a population receiving specialized anticoagulation management.
Screening HL in patients receiving long-term anticoagulation management is essential to ensure patients’ understanding of medical information, sustain optimal therapeutic control and prevent life-threatening thromboembolic complications [11,12,13,14,15]. This multifactorial relationship can be explained in the context of a conceptual framework by Paasche-Orlow and colleagues [16]. Poorer HL can lead to limited access and utilization of care in terms of non-compliance with clinic and medication schedules and underutilization of preventive care such as immunizations [16]. Patients with limited HL are less likely to practice self-care in terms of physical activity and dietary restrictions [16]. Lastly, worse HL hinders patients’ ability to comprehend medical information and effectivity interact with their providers [16]. Ultimately, these factors can lead to adverse health outcomes such as life-threatening hospitalizations, which can be further exacerbated by access to care barriers and significant underlying comorbidity burden [16].
Despite the development and validation of numerous HL measures, routine screening in clinical practice is limited [17]. Signature time has the potential to overcome practical limitations of widespread HL screening [21]. Since the majority of visits involve patients signing health-related documents, signature time is a practical assessment that can be built into clinic encounters. Signature time can reduce time and resource burden of HL screening with the majority of patients taking < 30 s to sign their name. Signature time may be less likely to induce patient stigma and embarrassment by screening in a discrete manner. Lastly, the accuracy and screening performance of signature time are comparable to well-accepted and validated HL instruments [17].
This study has several limitations. First, there is potential for selection bias due to not being able to recruit patients who were eligible based on EHR review but did not show up for the regularly scheduled appointment. Therefore, findings might not be generalizable to patients with access to care barriers limiting their ability to complete study enrollment or patients who are non-compliant with clinic visits. Second, this study was restricted to English-speaking patients, and the majority of patients were African-American and reported low income. This may limit generalizability of the study to broader populations. Third, S-TOFHLA is a measure of functional HL and might not capture other health-related skills such as oral HL or numeracy [22]. Fourth, this study included a small sample of patients with marginal HL. As a result, our findings may not be fully reflective of this subgroup of patients. Fifth, patients were informed during the consenting stage that their signature time would be captured. Consequently, patients modifying their behavior cannot be ruled out. Sixth, while patients with legal blindness were excluded, eyesight was not evaluated in this study and might have confounded the relationship between signature time and HL. Lastly, this was a single-center experience of patients receiving long-term anticoagulation management. As a result, findings might not generalize to other patient populations.
This study also has several strengths. To our knowledge, this is one of two studies evaluating signature time as a measure of HL. Our findings expand the literature body by replicating previous findings in another widely accepted HL instrument and among a different patient population [21]. Lastly, this is among the few studies that evaluated HL in an economically disadvantaged minority population with significant comorbidity burden [17].
These findings have several practice implications. Signatures are routinely captured in clinical settings. Therefore, signature time is a quick, discrete and practical approach that can help clinicians identify patients with low HL. Identifying high-risk patients can inform clinical interventions to provide tailored patient care and educational material. In other words, this measure can raise providers’ awareness to spend more time with patients and tailor their communication by using teach back methods and suitable education material. Widespread and seamless identification of patients with limited HL has the potential to improve quality of care, reduce errors and improve patient compliance [11,12,13,14,15]. Future studies should evaluate whether longer signature time can predict worse health outcomes. Future work is also warranted to evaluate the psychometric properties of signature time in a larger and more representative sample and explore variations by patient language, race, ethnicity and HL level.
Conclusion
Signature time demonstrated strong accuracy and screening performance in predicting HL levels as measured by S-TOFHLA. Patients spending > 9 s to sign their name are more likely to have inadequate HL. Signature time is an accurate, discrete and quick assessment that has the potential to be incorporated in busy clinical settings. Widespread screening for HL can help clinicians identify patients with limited HL who might benefit from tailored patient care and educational. Future larger studies are warranted to validate signature time and evaluate its ability to predict health outcomes.
References
In: Nielsen-Bohlman L, Panzer AM, and Kindig DA (Eds). Health literacy: a prescription to end confusion. Washington (DC). 2004
Kutner, M., Greenberg, E., Jin, Y., and Paulsen, C. The health literacy of America’s adults: results from the 2003 national assessment of adult literacy (NCES 2006–483). 2006; Available from: http://nces.ed.gov/pubs2006/2006483.pdf
Berkman ND, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107.
Dewalt DA, et al. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19(12):1228–39.
Rikard RV, et al. Examining health literacy disparities in the United States: a third look at the national assessment of adult literacy (NAAL). BMC Public Health. 2016;16(1):975.
Schaffler J, et al. The effectiveness of self-management interventions for individuals with low health literacy and/or low income: a descriptive systematic review. J Gen Intern Med. 2018;33(4):510–23.
Nguyen TH, et al. State of the science of health literacy measures: validity implications for minority populations. Patient Educ Couns. 2015;98:1452–512.
Nutescu EA, et al. Anticoagulation patient self-monitoring in the United States: considerations for clinical practice adoption. Pharmacotherapy. 2011;31(12):1161–74.
Lip GYH, et al. Antithrombotic therapy for atrial fibrillation: CHEST guideline and expert panel report. Chest. 2018;154(5):1121–201.
Kearon C, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315–52.
Estrada CA, et al. Literacy and numeracy skills and anticoagulation control. Am J Med Sci. 2004;328(2):88–93.
Oramasionwu CU, et al. The association of health literacy with time in therapeutic range for patients on warfarin therapy. J Health Commun. 2014;19(Suppl 2):19–28.
Rolls CA, et al. The relationship between knowledge, health literacy, and adherence among patients taking oral anticoagulants for stroke thromboprophylaxis in atrial fibrillation. Cardiovasc Ther. 2017;35(6): e12304.
Tang EO, et al. Relationship between patients’ warfarin knowledge and anticoagulation control. Ann Pharmacother. 2003;37(1):34–9.
Fang MC, et al. Health literacy and anticoagulation-related outcomes among patients taking warfarin. J Gen Intern Med. 2006;21(8):841–6.
Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(Suppl 1):S19-26.
Haun JN, et al. Health literacy measurement: an inventory and descriptive summary of 51 instruments. J Health Commun. 2014;19(Suppl 2):302–33.
Parikh NS, et al. Shame and health literacy: the unspoken connection. Patient Educ Couns. 1996;27(1):33–9.
Kelly PA, Haidet P. Physician overestimation of patient literacy: a potential source of health care disparities. Patient Educ Couns. 2007;66(1):119–22.
Kiechle ES, et al. Comparison of brief health literacy screens in the emergency department. J Health Commun. 2015;20(5):539–45.
Sharp LK, et al. Time to sign: the relationship between health literacy and signature time. Patient Educ Couns. 2013;90(1):18–22.
Baker DW, et al. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42.
Greiner M, Pfeiffer D, Smith RD. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev Vet Med. 2000;45(1–2):23–41.
Plot ROC curve with cutpoint labeling and optimal cutpoint analysis. April 5th, 2020]; Available from: http://support.sas.com/kb/25/018.html#hist.
Peterson B, Harrell FE. Partial proportional odds models for ordinal response variables. J R Stat Soc Ser C-Appl Stat. 1990;39(2):205–17.
Acknowledgements
We thank the Anticoagulation Clinic (ATC) faculty and students for their significant contributions in patient recruitment and data collection (Nancy Shapiro, PharmD; Erika Hellenbart, PharmD, BCPS; James Lee, PharmD, BCACP; Meghan Mccomb, PharmD; Ellen Uppuluri, PharmD; Nina Huynh, PharmD, BCPS; Crissel Arban, PharmD; Jasmine Forrest, PharmD; Ravi Patel, PharmD; Sandra Walko, PharmD).
Funding
Partial funding for this study has been provided by the University of Illinois at Chicago, College of Pharmacy, Office of the Dean, David J. Riback Research Fellowship. The authors funded the Rapid Service and Open Access fees.
Authorship Contributions
Ali Alobaidi contributed to the study design, acquisition and analysis and interpretation of the data, writing and reviewing of the manuscript, and decision to submit manuscript for publication. Connie Yan contributed to the study design, acquisition and analysis of the data, reviewing of the manuscript and decision to submit manuscript for publication. Miranda Kopfman contributed to the study design, acquisition and analysis of the data, reviewing of the manuscript and decision to submit manuscript for publication. Maryam Naveed contributed to the study design, acquisition and analysis of the data, reviewing of the manuscript and decision to submit manuscript for publication. Lisa Sharp contributed to the study design, acquisition and analysis of the data, writing and reviewing of the manuscript and decision to submit manuscript for publication. Edith Nutescu contributed to the study design, acquisition and analysis of the data, writing and reviewing of the manuscript and decision to submit manuscript for publication.
Disclosures
Affiliations for Ali Alobaidi, Connie Yan, Miranda Kopfman, and Maryam Naveed changed after the completion of the study. Ali Alobaidi and Connie Yan are employees of AbbVie and may own stocks/shares in the company. Miranda Kopfman is affiliated with Rush University Medical Center, Chicago, IL. Maryam Naveed is affiliated with the University of Chicago Medicine, Chicago, IL. Lisa K. Sharp, and Edith A. Nutescu have nothing to disclose.
Compliance with Ethics Guidelines
The study was approved by the Institutional Review Board of the University of Illinois at Chicago. All participants provided written informed consent and HIPAA authorization. I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Alobaidi, A., Yan, C.H., Kopfman, M. et al. The Relationship Between Signature Time and Functional Health Literacy: Results from a Prospective Study of an Urban Low-Income Population Receiving Long-Term Anticoagulation. Adv Ther 40, 3926–3936 (2023). https://doi.org/10.1007/s12325-023-02556-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02556-4