Abstract
Introduction
Risankizumab (RZB) and ustekinumab (UST), interleukin (IL)-23 and IL-12/23 inhibitors, respectively, are approved treatments for moderately to severely active Crohn’s disease (CD); direct comparison between the two is ongoing. We indirectly compared efficacy of RZB versus UST using data from phase 3 trials (RZB: NCT03104413; NCT03105128; NCT03105102; UST: NCT01369329; NCT01369342; NCT01369355).
Methods
Matching-adjusted indirect comparison was conducted using individual patient-level data from RZB trials and published aggregated data from UST trials. During induction, patients received RZB 600 mg intravenous (IV) at weeks 0, 4, and 8 or a single dose of UST 6 mg/kg IV at week 0. During maintenance, patients received RZB 180 or 360 mg subcutaneous (SC) or UST 90 mg SC every 8 or 12 weeks to 52 weeks. Outcomes included proportion of patients achieving Crohn’s Disease Activity Index (CDAI) response (decrease of ≥ 100 points or total score < 150) or remission (CDAI ≤ 150) and endoscopic improvement (measured by the Simple Endoscopic Score in CD [SES-CD]; response, ≥ 50% reduction from baseline; remission, SES-CD ≤ 2) following induction/baseline.
Results
Higher proportions of patients achieved clinical and endoscopic outcomes with RZB vs. UST induction treatment, resulting in significantly (p ≤ 0.05) greater percent differences (95% confidence intervals) between groups for CDAI remission (15% [5%, 25%]) and endoscopic response (26% [13%, 40%]) and remission (9% [0%, 19%]). Following maintenance, rates of CDAI remission were similar (range − 0.3% to − 5.0%) for RZB vs. UST. Differences for endoscopic response and remission ranged from 9.3% to 27.7% and 11.6% to 12.5%, respectively; differences were significant (p < 0.05) for endoscopic response for both doses of RZB compared to UST 12-week dosing.
Conclusions
This indirect comparison demonstrated higher rates of clinical and endoscopic outcomes during induction for RZB compared to UST; CDAI remission following maintenance was comparable. Direct comparisons of RZB and UST are warranted to validate these findings.
Plain Language Summary
Using individual patient-level data from risankizumab and aggregated data from ustekinumab phase 3 Crohn’s disease trials, we indirectly compared efficacy of risankizumab and ustekinumab to determine whether rates of improvement in disease symptoms (clinical) and endoscopic outcomes differed between treatments. Findings showed that clinical and endoscopic outcomes were more frequently achieved for patients receiving risankizumab versus ustekinumab after induction, while most maintenance outcomes were comparable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Risankizumab (RZB), a targeted interleukin (IL)-23 inhibitor, was recently approved for use in patients with moderately to severely active Crohn’s disease (CD); direct comparisons to ustekinumab in CD is currently being conducted (NCT04524611) |
This study indirectly compared efficacy of RZB with ustekinumab (UST), an IL-12/23 inhibitor, using phase 3 clinical trial data; outcomes assessed were CD Activity Index (CDAI) response and remission, as well as endoscopic response and remission as measured by Simple Endoscopic Score in CD (SES-CD) |
What was learned from the study? |
Using matching-adjusted indirect comparison analyses, this study showed that greater proportions of patients receiving RZB versus UST treatment achieved CDAI and endoscopic outcomes after induction, while maintenance treatment was generally comparable |
The findings of this study, which characterized the comparative effectiveness of RZB versus UST, may assist in clinical decision-making, ensuring that appropriate treatments are selected for the patient, thereby increasing the likelihood of achieving treatment targets |
Introduction
Crohn’s disease (CD) is a chronic, progressive inflammatory disease of the gastrointestinal tract, characterized by abdominal pain, diarrhea, fatigue, and weight loss [1,2,3]. Management of CD involves induction and maintenance therapy with the overall goal of improving patient symptoms. Clinical recommendations for treatment of CD, as described in the recent Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) II initiative of the International Organization for the Study of Inflammatory Bowel Diseases (IOIBD), have identified short-term, intermediate, and long-term targets [3]. Induction therapy is intended to improve symptoms and normalize C-reactive protein levels in the short term, after which maintenance therapy is employed to normalize calprotectin levels as an intermediate target [4]. Long-term targets include normalization of patient quality of life, absence of disability, and endoscopic healing [4]. The Crohn’s Disease Activity Index (CDAI) is a measure commonly used to assess patient outcomes and captures symptoms such as abdominal pain, stool frequency, body weight, and extraintestinal complications [5, 6]. In recent years, endoscopy, an objective measure of disease activity, has been used to provide assurance that changes in clinical symptoms align with mucosal improvements [5, 7]. Indeed, STRIDE II recommendations have deemed endoscopic healing as a primary long-term target of treatment, with endoscopic response suitable as a short-term target [4]. Recent guidelines from the US Food and Drug Administration recommend endoscopic outcomes be included in clinical trials for CD, with endoscopic response defined as a 50% reduction in Simple Endoscopic Score for Crohn’s Disease (SES-CD) and remission defined as an SES-CD of 0–2 [8].
Biologics have been shown to be effective in induction of clinical response and clinical remission as measured by CDAI scores [9, 10]. Inhibitors of tumor necrosis factor (TNF) are effective in the treatment of moderately to severely active CD that has failed to respond to conventional therapy [3, 11]. However, approximately a third of patients treated with anti-TNF therapies do not have an initial response to therapy [12]. A relatively recently approved (2016) biologic ustekinumab (UST), an anti-interleukin (IL)-12/23, has emerged as an alternative option that targets a different inflammatory pathway [3, 12,13,14]. Risankizumab (RZB), the first specific IL-23 inhibitor, is the newest biologic therapy on the market after receiving approval for treatment of adults with moderately to severely active CD in the USA, Canada, and the European Union in 2022 [15,16,17]. In two induction trials and one maintenance trial, RZB demonstrated significant improvements compared to placebo (PBO) in both clinical (CDAI) and endoscopic outcomes (measured by SES-CD) [18, 19].
Considering that both UST and RZB have demonstrated efficacy in patients with CD who had previously failed conventional care (CCF) or biologic therapies (BF), evidence characterizing the comparative effectiveness of RZB versus UST is needed to assist in clinical decision-making in the treatment of CD [3, 18, 19]. Moreover, while they have similar mechanisms of action (i.e., IL-23 inhibition), RZB is the first CD therapy to demonstrate endoscopic improvement as a ranked co-primary endpoint [18, 19]. Given the very recent approval of RZB, no direct comparisons to UST in CD have been published. However, indirect treatment comparison (ITC) methods can be used to assess the comparative effectiveness of different treatments [20, 21].
Network meta-analysis (NMA) is a common form of ITC which uses multiple aggregate relative effect measures to synthesize different studies. However, traditional NMA assumes that population characteristics that may influence the outcome of treatment do not differ between studies [20]. To address this limitation, we used matching-adjusted indirect comparison (MAIC) to compare the effectiveness of the two therapies. In MAIC, propensity score weighting of individual patient data (IPD) from one of the studies is used to balance population characteristics that may influence outcomes [21]. While phase 3 studies of RZB and UST were similar in eligibility criteria and study design, key differences may exist between the populations. For example, BF patients in RZB studies may have previous exposure to UST and/or vedolizumab (VDZ), which was exclusionary in UST studies. This study conducted MAICs comparing the effectiveness of RZB versus UST as induction and maintenance therapy for treatment of moderately to severely active CD in adults (CCF and/or BF), focusing on CDAI response and remission, as well as endoscopic response and endoscopic remission. It aims to provide an objective comparison so that clinicians may form their own opinions on when to use UST or RZB given their specific patient’s needs.
Methods
Study Design and Participants
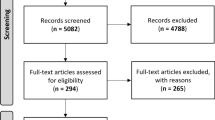
This study used IPD available from the RZB clinical studies ADVANCE, MOTIVATE, and FORTIFY (NCT03104413; NCT03105128; NCT03105102) [18, 19]. Aggregated population characteristics and outcomes data for UST studies were extracted from the UNITI-1, UNITI-2, and IM-UNITI publications (NCT01369329; NCT01369342; NCT01369355) [6, 22]. Outcome definitions in the RZB IPD were modified to match the definitions used in the UST studies to ensure comparability. These definitions differed marginally from the reported phase 3 RZB clinical program for CDAI response and endoscopic outcomes.
MAICs comparing RZB to UST adjusting for between-study population differences in effect modifiers were conducted for all combinations of outcomes, populations, and relevant maintenance dosing variations of RZB and UST based on data availability.
RZB patients included in the analysis were adults diagnosed with CD who were either CCF or BF prior to induction therapy. RZB patients with previous exposure to UST or VDZ were excluded to match the inclusion criteria used in the UST phase 3 program. Additionally, those RZB-treated patients who missed an efficacy measurement or discontinued treatment as a result of COVID-19 were excluded. The following dose groups were included for RZB: 600 mg intravenous (IV) induction at weeks 0/4/8 and 180 or 360 mg subcutaneous (SC) every 8 weeks for maintenance. For UST only published data for the single 6 mg/kg IV loading dose (approved dosing) along with 90 mg SC administered every 8 or 12 weeks for maintenance (Q8W and Q12W, respectively) were included. The UST 6 mg/kg induction dose approximates dosing by weight range (i.e., less than 55 kg, 260 mg; 55–85 kg, 390 mg; greater than 85 kg, 520 mg).
Clinical Outcomes
Analyses for this study included anchored MAICs comparing RZB versus UST for CDAI response, CDAI remission, endoscopic response, and endoscopic remission at induction and maintenance among the different populations (CCF only, BF only, and CCF + BF) and dosing variations when relevant.
Outcome definitions from the UST trials were used. In RZB studies, outcomes were defined as the following: CDAI response, at least a 100-point decrease in CDAI from baseline; endoscopic response, at least 50% decrease in SES-CD from baseline or at least 2-point reduction from baseline for patients with isolated ileal disease and a baseline SES-CD of 4; endoscopic remission, SES-CD ≤ 4 and at least a 2-point reduction from baseline and no subscore greater than 1 in any individual variable. For this analysis, outcome variables in the RZB IPD were recoded on the basis of the underlying CDAI and SES-CD data and the UST definitions. As such, CDAI response was defined as a decrease from baseline of at least 100 points or CDAI < 150 (CDAI remission was defined as a CDAI < 150 in both RZB and UST studies). An endoscopic response was defined as a 50% or greater reduction from baseline in SES-CD score, and endoscopic remission as a total SES-CD score ≤ 2. As a result of limitations of the data reported for UST studies, induction and maintenance MAICs of endoscopic outcomes could only be reported for the CCF + BF population; likewise, there was also no ability to evaluate CDAI response for the maintenance MAICs as it was not reported in UST studies.
Statistical Analysis of Data
The feasibility of conducting the planned analyses was assessed on the basis of review of similarity in design of the RZB and UST studies; inclusion of a common comparator in the studies assessed (allowing for anchored analysis); and completeness of the reported UST data required for the analyses. In the induction studies, the IV PBO arms were considered sufficiently similar to act as an anchor/common comparator; for maintenance studies, the active treatment withdrawal PBO groups were considered the anchor/common comparator.
MAICs were conducted adjusting for differences in treatment effect-modifying variables between the RZB and UST study populations using a structured process that identified matching variables following recommendations from the National Institute for Health Care Excellence (NICE) guidance on MAIC methodology [21]. This process included a targeted literature review to identify factors predictive of the treatment effect of biologic therapies in CD, clinical input, and review of UST pivotal publications [7, 22] and RZB IPD for availability of data on effect-modifying factors. Where effect modifier distributions or values were available, tests of statistical significance of differences between the UST and RZB populations were conducted. RZB patients were weighted such that their mean baseline characteristics matched those reported for the published UST trials for effect-modifying variables. Weights were obtained on the basis of a logistic regression model for the propensity of enrollment in the RZB trial versus the UST trial (weights estimated as the inverse of the propensity), with matched baseline characteristics identified from the structured process described above using a method-of-moments-based matching approach. Treatment effect-modifying variables ultimately used in the matching included duration of disease categories, disease severity (induction baseline CDAI > 300, induction baseline CRP > 0.5 mg/dL), disease phenotype (stenosis current or past), previous biologic failure, and prior number of failed biologics.
Baseline characteristics before and after matching were compared between RZB and UST cohorts using two-sided Wald tests for categorical variables and t tests for continuous variables. The log-odds ratio of RZB versus PBO was estimated along with its 95% confidence interval (CI) and then back-transformed to estimate absolute probabilities of response [21]. Of note, as described in MAIC methodological guidance, estimates of absolute outcomes may be biased if there is substantial imbalance of prognostic factors across the populations, as only effect-modifying factors are adjusted for in anchored MAIC [21].
The relative effect measure of RZB compared to UST was calculated as the difference in the PBO-subtracted response rates for RZB and UST; statistically significant differences (p ≤ 0.05) were assessed using a two-sample test of binomial proportions. Differences in the absolute effect measure were assessed on the basis of comparison of the 95% CI estimated in the MAIC for RZB, and the Wald 95% CI calculated for UST.
To assess the effectiveness of RZB and UST in inducing and maintaining clinical outcomes, a “treat-through” sensitivity analysis was also conducted in the combined CCF + BF population wherein the clinical response rate during induction was multiplied by the clinical remission rate during maintenance. This analysis estimates the expected proportion of patients achieving clinical remission across both induction and maintenance; a full description of this analysis is in Appendix A (Supplementary Material). The PBO-subtracted relative response rates of achieving clinical remission (95% CIs) for RZB- versus UST-treated patients are reported.
Ethical Statement
This study, and each clinical trial included in the analysis, was conducted in accordance with the ethical principles that have their origin in the current Declaration of Helsinki and was consistent with International Conference on Harmonization Good Clinical Practice, Good Epidemiology Practices, and applicable regulatory requirements [7, 18, 19, 22]. This analysis utilized de-identified data from published clinical trial data; thus, no ethics committee approval was required. However, each individual trial included in this analysis was approved by independent ethics committees or institutional review boards at each study site and all patients (or parents/legal guardians for adolescent patients) provided written informed consent before enrolling in each clinical trial [7, 18, 19, 22].
Results
Patient Demographics
Baseline characteristics before and after matching for effect modifiers among patients receiving RZB or UST induction are presented in Table 1 for induction and Tables 2 and 3 for maintenance analyses. A full list of patient demographics and clinical characteristics prior to and after matching is provided in Supplementary Materials (Tables S1–S3). Briefly, after matching, the RZB groups closely aligned with the UST groups, with similar disease durations, similar rates of ileal disease involvement, CDAI severity, and prior failure of TNF inhibitors. The effective sample size for the RZB-treated groups ranged from 146 to 325 in induction and 138–194 in maintenance, with the largest impact on the BF population because patients with prior UST/VDZ were excluded.
Rates of Response and Remission Following Induction Therapy
Following induction therapy with RZB or UST, a higher proportion of patients, in all populations and active treatment groups, achieved CDAI and endoscopic outcomes as compared to PBO (Fig. 1). Among CCF, BF, and CCF + BF populations, absolute and relative (i.e., PBO-adjusted) effect measures for CDAI response and remission favored RZB (Fig. 1a–c).
Rates of response and remission following induction therapy with RZB (600 mg) or UST (6 mg/kg). *p ≤ 0.05 for RZB versus UST. Relative effect measures are shown as the percent difference between treatment groups; absolute effect measures are the proportions of patients achieving each outcome in each treatment group. BF biologic failure, CCF conventional care failure, CDAI Crohn’s Disease Activity Index, IV intravenous, PBO placebo, RZB risankizumab, UST ustekinumab
Among the CCF population, the absolute proportion of RZB-treated patients achieving clinical remission was significantly greater than UST-treated patients (56.3% vs. 40.2%; p ≤ 0.05; Fig. 1a). More RZB-treated BF patients achieved clinical response (64.0% vs. 37.8%; p ≤ 0.05) and remission (46.8% vs. 20.9%; p ≤ 0.05) compared with UST-treated patients (Fig. 1b). Likewise, a greater proportion of CCF + BF patients achieved clinical response (66.5% vs. 47.0%, p ≤ 0.05) and clinical remission (53.9% vs. 29.7%; p ≤ 0.05), endoscopic response (45.5% vs. 21.7%, p ≤ 0.05), and endoscopic remission (19.4% vs. 8.4%; p ≤ 0.05) versus UST-treated patients (Fig. 1c, d).
Although numeric differences favored RZB for all clinical outcomes in the analyses, the relative differences reached statistical significance only in the CCF + BF population for clinical remission with 14.6% (95% CI 4.6%, 24.5%; p ≤ 0.05; Fig. 1c) more RZB patients achieving this outcome compared with UST. Likewise, relative effect measures were statistically significant in CCF + BF RZB- vs. UST-treated patients for endoscopic response (26.3% [13.0%, 39.6%]; p ≤ 0.05) and endoscopic remission (9.3% [0.0%, 18.6%]; p ≤ 0.05; Fig. 1d).
Rates of Response and Remission Following Maintenance Therapy
Available data from UST trials only assessed maintenance outcomes among the CCF + BF population. As such, all maintenance results reported for RZB trials included in the analysis are from the CCF + BF population and stratified by UST maintenance dose that the RZB population was matched to (UST 90 mg Q8W: Fig. 2; UST 90 mg Q12W: Fig. S1). However, published rates of endoscopic remission among UST-treated patients were reported as the aggregate of both the 90 mg Q8W and 90 mg Q12W groups and thus are reported in the same manner herein [7].
Rates of response and remission following maintenance therapy with RZB (180 mg or 360 mg) or UST (90 mg Q8W). *p ≤ 0.05 for RZB versus UST. Relative effect measures are shown as the percent difference between treatment groups; absolute effect measures are the proportions of patients achieving each outcome in each treatment group. BF biologic failure, CCF conventional care failure, CDAI Crohn’s Disease Activity Index, PBO placebo, Q8W every 8 weeks, Q12W every 12 weeks, RZB risankizumab, SC subcutaneous, UST ustekinumab
Overall, there were no statistically significant differences in CDAI remission rates (either absolute or relative) between RZB or UST at any dosage (Fig. 2a; Fig. S1a). The placebo-adjusted treatment difference for RZB compared to UST in CDAI remission rates ranged from − 0.3% to − 5.0% for any of the comparisons. Relative effect measures were numerically higher for endoscopic response (treatment difference range 9.3–27.7%) and endoscopic remission (treatment difference range 11.6–12.5%) for RZB compared with UST, regardless of dose (Fig. 2b; Fig. S1b). Likewise, absolute rates for endoscopic response and remission were also higher for RZB-treated patients (Fig. 2b,c; Fig. S1b).
Treat-Through Analyses of Relative Response Rates for CDAI Clinical Remission
Patients receiving maintenance RZB 180 mg had placebo-adjusted treat-through clinical remission (induction CDAI response, maintenance CDAI remission) rates 7.5% (95% CI − 3.9%, 18.0%) and 9.0% (95% CI − 2.3%, 19.4%) greater at the end of maintenance than patients receiving UST Q8W or Q12W, respectively (Table S4). Similarly, those receiving maintenance RZB 360 mg had placebo-adjusted treat-through clinical remission rates 6.6% (95% CI − 4.8%, 16.9%) and 8.7% (− 2.7%, 19.0%) higher than patients receiving UST Q8W or Q12W, respectively (Table S5).
Discussion
Both RZB and UST are now approved for the treatment of moderately-to-severely active CD, although there is limited comparative efficacy data to inform clinical decision-making and the relative positioning of these agents. Furthermore, the trial populations entering the respective phase 3 development programs for RZB and UST were substantively different. To address these limitations, we used MAIC analyses to compare the relative clinical and endoscopic effectiveness of RZB versus UST as induction and maintenance treatments of moderately to severely active CD. There are several important findings from this analysis. First, despite adjustments for differences in effect-modifying characteristics between the RZB and UST populations, clinical outcomes remained similar in the majority of MAICs. However, RZB was relatively more effective in inducing CDAI remission in the combined trial population compared to UST. Second, for endoscopic outcomes, the MAIC analyses favored RZB with significantly more patients achieving endoscopic response and remission at the end of induction in the combined population of CCF + BF patients. Likewise, during maintenance, significantly more patients in both RZB 180 mg and 360 mg groups achieved endoscopic response and remission more frequently than UST.
Similar clinical outcomes, with improved endoscopic outcomes for RZB and UST, may be expected on the basis of the unadjusted absolute clinical trial data informing the MAICs [7, 18, 19, 22]. Indeed, at least 30% of patients in RZB and UST induction and maintenance trials achieved clinical remission and up to 25% achieved endoscopic remission [7, 18, 19, 22]. However, there were key differences in the populations of patients included in these studies, with RZB trials enrolling patients who failed conventional therapies and/or biologic therapies (including UST and vedolizumab) and UST trials focused on those who failed anti-TNF therapies or immunosuppressants [7, 18, 19, 22]. In this analysis, when matching populations that failed anti-TNF therapies, there were marked differences among the two treatments in the proportion of patients in the CCF + BF population that achieved clinical remission, endoscopic response, and endoscopic remission after induction, and endoscopic outcomes after maintenance therapy, which favored RZB compared to UST. The marked differences in improvement during induction therapy are especially important, as achieving clinical improvements early in the treatment course is important and relevant to patients.
The assessment of endoscopic response to therapy has become a key measure in treatment of CD, such that endoscopic healing is now considered a long-term treatment target [4, 5, 7]. ADVANCE, MOTIVATE, and FORTIFY are the first trials to use endoscopic response as a co-primary endpoint rather than secondary or exploratory endpoints, highlighting the growing importance of endoscopic measures. This study showed that a greater proportion of RZB-treated patients achieved endoscopic response, with an overall trend toward endoscopic remission, than UST-treated patients. It is important to note that, in interpreting the results of the endoscopic maintenance analyses, baseline characteristics indicate there was an imbalance in the proportion of patients with prior anti-TNF failure. For example, prior anti-TNF failure was higher in the RZB 360 mg maintenance population (64.1%) than in the endoscopic substudy of UST maintenance (32.1% for Q8W, 31.7% for Q12W). Evidence in CD suggests that prior anti-TNF failure is associated with failure of a second anti-TNF therapy and, a meta-analysis showed that, among patients switching to a second anti-TNF therapy, remission rates depended significantly on the cause for switching [23, 24]. Indeed, remission rates were higher for patients with previous anti-TNF intolerance (61%) than those with primary (30%) or secondary (45%) failure of their previous anti-TNF therapy [24]. The MAIC of maintenance outcomes in CCF + BF patients in this study suggest that the negative association of previous anti-TNF failure with subsequent treatment response may extend to IL-12/23 and/or IL-23 inhibitors. Nonetheless, the results from this study favored RZB over UST in most outcomes.
Strengths of this study include the breadth of populations (CCF, BF, and CCF + BF), outcomes (CDAI response and remission; endoscopic response and remission), and treatment phases (induction and maintenance) that were assessed. Further, to inform the population characteristics adjusted in the analyses, a rigorous process was applied to identify effect-modifying variables, including structured literature review and clinical input from experts, in alignment with methodological guidance [21]. While adjustments to balance population characteristics of the RZB and UST studies required exclusion or lesser weighting of certain subgroups and associated reductions to effective sample size (ESS) of the analytical population, reasonably large samples of patients from the RZB studies were retained in all analyses. The inclusion of endoscopic response and remission as outcomes for comparison in this study may be of particular interest to healthcare providers. Recent consensus clinical recommendations for treatment of CD, as described in the recent STRIDE II initiative of IOIBD, recognize endoscopic healing as the primary long-term target of treatment, and that endoscopic response is a suitable short-term target [4]. While endoscopic measures are recognized as objective assessments, until recently they have been less commonly reported in the evidence base, perhaps because of the relative recency of clinical recommendations for their use and/or heterogeneity in definitions [5, 7, 8]. In this study, we addressed the differences in definitions of endoscopic outcomes between RZB and UST studies by recoding RZB patient-level data according to UST outcome definitions. Despite limited sample sizes and corresponding uncertainty in the UST endoscopic substudy, important numeric (and in certain cases statistically significant) differences in responses rates for endoscopic outcomes were observed. RZB versus PBO endoscopic outcomes consistently improved when matching to UST population characteristics, driven by the higher proportion of the RZB population with prior biologic failure (approximately 60–65% in RZB studies vs. 30–40% in UST studies).
Certain limitations of the analysis include differences in the designs of the studies compared, which might introduce heterogeneity that could not be adjusted for. First, owing to differences in study designs, outcomes compared in the analysis were measured at 8 and 44 weeks in UST induction and maintenance studies, respectively, as compared to measurement at 12 and 52 weeks in RZB studies. Second, enrollment in the maintenance studies of induction responders may also introduce heterogeneity. The MAICs adjusted for imbalances between the populations in potentially “effect-modifying” characteristics, as recommended in methodological guidance, but not for prognostic factors that might affect PBO response rates across trials. Relative effect measures were calculated by subtracting PBO response rates from those for the interventions; any systematic difference between the PBO arms may therefore bias comparison, which could arise from “carryover” influences from induction to the withdrawal PBO arms in maintenance. For example, different response rates in induction or elimination half-lives across therapies may yield a systematic bias in the withdrawal PBO response rates in maintenance. Third, after balancing on matching variables, ESS was reduced; however, across all the MAICs, the ESS reduction for the RZB population did not exceed 50% compared to the population that excluded prior UST/VDZ exposure and COVID-impacted patients, maintaining statistical power for the analysis. As expected, the induction analyses for the BF population had the largest reduction in sample size due to adjustment as the prior UST/VDZ-exposed patients were concentrated in this population. The lowest ESS for RZB-treated patients was 93 in induction analyses, 61 in maintenance RZB 360 mg analyses, and 68 in maintenance RZB 180 mg analyses. Fourth, in maintenance analyses, for both treatments, the PBO groups were actually active drug withdrawal and not a true PBO, which may impact outcomes. Fifth, while this study found some significant differences in endoscopic response and/or remission rates between RZB- and UST-treated patients in the maintenance studies, it is important to note that these results may not be generalizable given the small sample size. Finally, this analysis was limited to indirect comparisons of treatment effectiveness due to potential heterogeneity in adverse event reporting. Both efficacy and safety are important considerations for a benefit/risk assessment in making treatment decisions. Given the limited frequency of safety events, and that matching variables may differ for safety vs. efficacy outcomes, safety outcomes were not compared. However, for reference, safety outcomes for each trial included in this analysis are summarized in Table S6. Head-to-head comparisons of RZB and UST are needed to confirm the results of this analysis and better compare safety outcomes. The Study Comparing Intravenous/Subcutaneous Risankizumab to IV/SC Ustekinumab to Assess Change in Crohn’s Disease Activity Index in Adult Participants With Moderate to Severe Crohn’s Disease (SEQUENCE; NCT04524611) is ongoing and findings from this study may help to differentiate the two treatments in the future.
Conclusion
Anchored MAICs comparing RZB and UST phase 3 clinical studies, adjusting for differences in effect-modifying population characteristics, demonstrated comparative clinical effectiveness (i.e., CDAI remission) and endoscopic effectiveness of RZB versus UST favored RZB. Endoscopic outcomes comparing RZB to PBO consistently improved when analyses were matched to UST population characteristics, driven by the higher proportion of the BF population in the original phase 3 RZB trial.
References
Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn’s disease. Lancet. 2017;389(10080):1741–55. https://doi.org/10.1016/s0140-6736(16)31711-1.
Mehta F. Economic implications of inflammatory bowel disease and its management. Am J Manag Care. 2016;22:10.
Lichtenstein GR, Loftus EV, Isaacs KL, et al. ACG clinical guideline: management of Crohn’s disease in adults. Am J Gastroenterol. 2018;113(4):481–517. https://doi.org/10.1038/ajg.2018.27.
Turner D, Ricciuto A, Lewis A, et al. STRIDE-II: an update on the selecting therapeutic targets in inflammatory bowel disease (STRIDE) initiative of the international organization for the study of IBD (IOIBD): determining therapeutic goals for treat-to-target strategies in IBD. Gastroenterology. 2021;160(5):1570–83. https://doi.org/10.1053/j.gastro.2020.12.031.
Peyrin-Biroulet L, Sandborn W, Sands BE, et al. Selecting therapeutic targets in inflammatory bowel disease (STRIDE): determining therapeutic goals for treat-to-target. Am J Gastroenterol. 2015;110(9):1324–38. https://doi.org/10.1038/ajg.2015.233.
Sandborn WJ, Feagan BG, Hanauer SB, et al. A review of activity indices and efficacy endpoints for clinical trials of medical therapy in adults with Crohn’s disease. Gastroenterology. 2002;122(2):512–30. https://doi.org/10.1053/gast.2002.31072.
Rutgeerts P, Gasink C, Chan D, et al. Efficacy of ustekinumab for inducing endoscopic healing in patients with Crohn’s disease. Gastroenterology. 2018;155(4):1045–58. https://doi.org/10.1053/j.gastro.2018.06.035.
United States Food and Drug Administration. Crohn’s Disease: Developing Drugs for Treatment - Guidance for Industry. 2022. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/crohns-disease-developing-drugs-treatment.
Ford AC, Sandborn WJ, Khan KJ, et al. Efficacy of biological therapies in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(4):644–59, quiz 60. https://doi.org/10.1038/ajg.2011.73.
Kawalec P, Mikrut A, Wiśniewska N, Pilc A. Tumor necrosis factor-α antibodies (infliximab, adalimumab and certolizumab) in Crohn’s disease: systematic review and meta-analysis. Arch Med Sci. 2013;9(5):765–79. https://doi.org/10.5114/aoms.2013.38670.
D’Amico F, Fiorino G, Furfaro F, et al. Patient’s profiling for therapeutic management of inflammatory bowel disease: a tailored approach. Expert Rev Gastroenterol Hepatol. 2020;14(9):765–73. https://doi.org/10.1080/17474124.2020.1772057.
Gisbert JP, Chaparro M. Predictors of primary response to biologic treatment [anti-TNF, vedolizumab, and ustekinumab] in patients with inflammatory bowel disease: from basic science to clinical practice. J Crohns Colitis. 2020;14(5):694–709. https://doi.org/10.1093/ecco-jcc/jjz195.
STELARA (ustekinumab) [package insert]. Horsham, PA: Janssen Biotech, Inc.; 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/761044lbl.pdf.
Janssen-Cilag International NV. Summary of Product Characteristics STELARA (ustekinumab). 2016. https://www.ema.europa.eu/en/documents/product-information/stelara-epar-product-information_en.pdf.
SKYRIZI (risankizumab) [package insert]. North Chicago, IL: AbbVie Inc.; 2022. https://www.rxabbvie.com/pdf/skyrizi_pi.pdf.
SKYRIZI® (risankizumab-rzaa) Receives FDA Approval as the First and Only Specific Interleukin-23 (IL-23) to treat moderately to severely active Crohn's disease in adults [press release]. 17 June 2022 2022.
AbbVie Announces European Commission Approval of SKYRIZI® (risankizumab) for the Treatment of Moderate to Severe Active Crohn's Disease [press release]. 23 November 2022.
D’Haens G, Panaccione R, Baert F, et al. Risankizumab as induction therapy for Crohn’s disease: results from the phase 3 ADVANCE and MOTIVATE induction trials. Lancet. 2022;399(10340):2015–30. https://doi.org/10.1016/s0140-6736(22)00467-6.
Ferrante M, Panaccione R, Baert F, et al. Risankizumab as maintenance therapy for moderately to severely active Crohn’s disease: results from the multicentre, randomised, double-blind, placebo-controlled, withdrawal phase 3 FORTIFY maintenance trial. Lancet. 2022;399(10340):2031–46. https://doi.org/10.1016/s0140-6736(22)00466-4.
Jansen JP, Fleurence R, Devine B, et al. Interpreting indirect treatment comparisons and network meta-analysis for health-care decision making: report of the ISPOR Task Force on Indirect Treatment Comparisons Good Research Practices: part 1. Value Health. 2011;14(4):417–28. https://doi.org/10.1016/j.jval.2011.04.002.
Phillippo D, Ades T, Dias S, et al. NICE DSU Technical Support Document 18: Methods for population-adjusted indirect comparisons in submissions to NICE: NICE Decision Support Unit; 2016.
Feagan BG, Sandborn WJ, Gasink C, et al. Ustekinumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2016;375(20):1946–60. https://doi.org/10.1056/NEJMoa1602773.
Atreya R, Neurath MF, Siegmund B. Personalizing treatment in IBD: Hype or reality in 2020? Can we predict response to anti-TNF? Front Med (Lausanne). 2020;7:517. https://doi.org/10.3389/fmed.2020.00517.
Gisbert JP, Marín AC, McNicholl AG, Chaparro M. Systematic review with meta-analysis: the efficacy of a second anti-TNF in patients with inflammatory bowel disease whose previous anti-TNF treatment has failed. Aliment Pharmacol Ther. 2015;41(7):613–23. https://doi.org/10.1111/apt.13083.
Acknowledgements
Funding
This work/study was funded by AbbVie Inc; AbbVie funded the Advances in Therapy Rapid Service Publication Fee. AbbVie participated in the study design, research, data collection, analysis and interpretation of data, writing, reviewing, and approving the publication. All authors had access to the data results, and participated in the development, review, and approval of this abstract. No honoraria or payments were made for authorship.
Medical Writing and/or Editorial Assistance
Medical writing services provided by Samantha D. Francis Stuart, PhD, of Fishawack Facilitate Ltd, part of Fishawack Health, and funded by AbbVie.
Author Contributions
All authors contributed to drafting and critically revising for intellectual content. Tom O’Connell, Marjorie Crowell, and Jenny Griffith contributed substantially to study conception, acquisition of data, and interpretation of data. Tom O’Connell and Marjorie Crowell contributed substantially to data analysis.
Disclosures
Marla Dubinsky has received consulting fees from AbbVie, Abivax, Astra Zeneca, Bristol Myers Squibb, Eli Lilly, Ferring, Janssen, Merck, Takeda, Pfizer, Prometheus Biosciences, Prometheus Labs. Christopher Ma has received consulting fees from AbbVie, Alimentiv, Amgen, AVIR Pharma Inc, BioJAMP, Bristol Myers Squibb, Celltrion, Ferring, Fresenius Kabi, Janssen, McKesson, Mylan, Takeda, Pendopharm, Pfizer, Prometheus Biosciences Inc., Roche, Sanofi; speaker’s fees from AbbVie, Amgen, AVIR Pharma Inc, Alimentiv, Bristol Myers Squibb, Ferring, Fresenius Kabi, Janssen, Takeda, Pendopharm, and Pfizer; royalties from Springer Publishing; research support from Ferring, Pfizer. Tom O’Connell and Marjorie Crowell are employees of Medicus Economics LLC and were contracted by AbbVie for this study. Jenny Griffith, Ezequiel Neimark, and Kristina Kligys are employees of AbbVie and may own stock.
Compliance with Ethics Guidelines
This study, and each clinical trial included in the analysis, was conducted in accordance with the ethical principles that have their origin in the current Declaration of Helsinki and was consistent with International Conference on Harmonization Good Clinical Practice, Good Epidemiology Practices, and applicable regulatory requirements [7, 18, 19, 22]. This analysis utilized de-identified data from published clinical trial data; thus, no ethics committee approval was required. However, each individual trial included in this analysis was approved by independent ethics committees or institutional review boards at each study site and all patients (or parents/legal guardians for adolescent patients) provided written informed consent before enrolling in each clinical trial [7, 18, 19, 22].
Data Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Dubinsky, M., Ma, C., Griffith, J. et al. Matching-Adjusted Indirect Comparison Between Risankizumab and Ustekinumab for Induction and Maintenance Treatment of Moderately to Severely Active Crohn’s Disease. Adv Ther 40, 3896–3911 (2023). https://doi.org/10.1007/s12325-023-02546-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02546-6