Abstract
Introduction
Transformation of higher-risk myelodysplastic syndromes (MDS) to acute myeloid leukemia (AML) may be associated with increased healthcare resource utilization (HCRU) and costs. To describe this economic impact, HCRU and costs were compared between US patients who experienced transformation to AML and those who did not.
Methods
Using the Optum administrative claims data, this retrospective matched cohort study identified patients (≥ 18 years old) with higher-risk MDS who initiated first-line therapy between January 1, 2008, and June 30, 2019. Patients whose disease transformed to AML were matched 1:1 to patients whose disease did not transform, based on the duration of follow-up. The follow-up period was divided into two periods: pre- (before transformation to AML) and post-AML (after transformation to AML). For patients who did not transform to AML, pre- and post-AML periods were determined using the transformation date of their matched pair. HCRU and total adjusted costs (2019 US dollars, $) were compared between patients who transformed to AML and those who did not.
Results
A total of 118 matched patient pairs were included in the study. The hospitalization rate was significantly higher in patients who transformed than in those who did not during the entire follow-up (58.8% vs. 44.1%; P = 0.0295) and post-AML (47.5% vs. 28.0%; P = 0.0028) periods. Across all periods, supportive care use was significantly higher among patients who transformed to AML vs. patients who did not transform. Adjusted mean monthly costs for patients with higher-risk MDS who transformed to AML were higher than those who did not transform ($25,964 vs. $19,150; P < 0.0001). The observed total cost difference was more notable in the post-AML period ($36,424 vs. $14,860; P < 0.0001).
Conclusions
Patients with higher-risk MDS whose disease transformed to AML incurred significantly higher healthcare costs compared to those whose disease did not transform, highlighting the important need for treatments that prevent or delay transformation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Transformation to acute myeloid leukemia (AML) occurs in approximately 40% of patients with higher-risk myelodysplastic syndromes (MDS). |
AML is considered one of the most expensive cancers to treat, particularly because of costly medical interventions. |
Data on costs associated with transformation to AML among treated patients with higher-risk MDS are limited. |
What was learned from the study? |
The adjusted average total costs per patient per month from initiation of treatment for higher risk MDS were $25,964 for patients who transformed to AML and $19,150 for patients who did not transform in the US. |
The observed cost difference between the two groups was even more notable in the period following transformation to AML. The adjusted average total costs per patient per month during this period were $36,424 for patients who transformed to AML and $14,860 for patients who did not transform in the US in equivalent follow-up. |
Transformation from higher-risk MDS to AML significantly increased healthcare costs, highlighting an important need for treatments that prevent or delay transformation. |
Introduction
Myelodysplastic syndromes (MDS) are a group of hematologic malignancies characterized by ineffective hematopoiesis causing anemia, neutropenia, and thrombocytopenia leading to transfusions, infections, and death [1]. MDS are relatively rare in the US, with approximately 10,000 new cases of MDS diagnosed annually [2]. With a median age at diagnosis of 76 years, MDS is primarily a disease of the elderly [2]. Patients with MDS have a disease course that can range from indolent (i.e., low risk), which has a prolonged life expectancy, to aggressive, which is associated with approximately 40% experiencing transformation to acute myeloid leukemia (AML) [3, 4].
The goals of treatment in patients with MDS include prolonging overall survival (OS), improving blood counts, and improving quality of life (QoL) [5]. Patients with MDS experience frequent and prolonged hospitalizations, frequent outpatient visits, and high healthcare costs [6]. Transfusions are a widely used supportive care approach in patients with MDS, primarily to prevent serious complications of both acute and chronic anemia [7]. Transfusion-dependent patients have worse prognosis and increased costs [7]. Costs related to MDS have been reported to make up approximately 32% of total annual healthcare charges in patients diagnosed with MDS [6]. For patients with higher-risk MDS, the goals of treatment also include a delay in transformation to AML, which occurs in approximately 40% of patients with higher-risk MDS [4, 5, 8]. Transformed AML progresses rapidly and is typically fatal within weeks or months if left untreated [9]. Low-intensity therapy with a hypomethylating agent (HMA), such as azacitidine or decitabine, has been shown to decrease the risk of transformation from higher-risk MDS to AML [10,11,12,13].
AML is considered one of the most expensive cancers to treat, particularly due to costly medical interventions such as stem cell transplant (SCT), lengthy periods of hospitalization required for the delivery of therapy (curative and supportive), and treatment of disease-related complications [14]. A study of 4058 elderly (≥ 65 years of age) patients with AML with Medicare revealed that, despite a very short survival period (median: 2.6 months), patients with AML accrued > $96,000 in healthcare costs following initial AML diagnosis; the largest component of this (76.3%) was inpatient utilization [9].
While studies have separately evaluated the cost of MDS and AML, data on costs associated with transformation to AML among treated patients with higher-risk MDS are limited. This retrospective, matched cohort study was conducted to evaluate the economic impact of the transformation to AML among patients with higher-risk MDS.
Methods
Study Design and Data Source
This study was a retrospective, matched cohort analysis using administrative claims data from the Optum Clinformatics database (Optum). The Optum database includes de-identified data from > 180 million members with private health insurance, who are fully insured through commercial or Medicare Advantage plans. Ethics committee approval was not required for this study due to the retrospective, blinded nature of the data. Included in the data are medical and pharmacy claims, laboratory results, mental health claims, and insurance enrollment information. The core data can be linked to other data sources, such as clinical/electronic medical records data, socioeconomic status data, mortality data, inpatient hospital detail records, and health risk assessment data.
Study Period
Retrospective data from January 1, 2007, to September 30, 2019, were used to conduct the study. The patient identification period, January 1, 2008, to June 30, 2019, was the period during which patients newly diagnosed with higher-risk MDS who received treatment with chemotherapy were identified. The index date was defined as the start date of the first chemotherapy treatment during the patient identification period. The baseline period was considered the 12-month period before the index date. The follow-up period was variable for all patients and included the index date until death, end of continuous enrollment, or end of study (September 30, 2019). The follow-up was further divided into two periods: pre-AML period (before transformation to AML) and post-AML period (after transformation to AML). To determine the pre- and post-AML periods for patients who did not transform to AML, the transformation date of their matched pair was used.
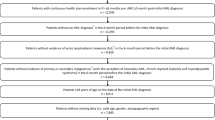
Study Population
The study population consisted of adult patients (≥ 18 years of age) with newly diagnosed higher-risk MDS, who received chemotherapy treatment during the patient identification period. Patients were included in the study if they had ≥ 1 inpatient claim with a higher-risk MDS International Classification of Diseases (ICD)-9/10 diagnosis code (ICD-9-CM code: 238.73; ICD-10 codes: D46.20, D46.21, D46.22) or ≥ 2 outpatient claims with an MDS ICD-9/10 code (the higher-risk MDS code had to either be the first code or within 14 days of the first code); continuous enrollment in medical and pharmacy benefits for 12 months before their higher-risk MDS diagnosis; and evidence of MDS-specific chemotherapy treatment, with or without MDS-directed supportive care in the follow-up period. Patients were excluded if there was evidence of chemotherapy, SCT, other primary cancer, metastatic disease, or AML prior to the higher-risk MDS diagnosis. Any evidence of myelofibrosis during the study period also resulted in exclusion.
Evidence of transformation to AML was assessed during the follow-up period, whereby patients with and without evidence of an AML diagnosis (ICD-9-CM code: 205.0x; ICD-10 codes: C92.0x, C92.5x, C92.6x, C92.9x, C92.A) constituted the study cohorts for the outcome comparison. To assess the economic burden in higher-risk MDS patients with and without transformation to AML, and the economic burden before and after transformation to AML, the resulting patient population who experienced AML transformation was matched 1:1 on follow-up time to those who did not experience AML transformation using the direct matching method. The follow-up time between matched pairs was allowed to vary ± 30 days. Matching on follow-up time allowed for the assessment of outcomes over equivalent time periods between patients who experienced AML transformation and those who did not to avoid survival bias. Matching on other variables or on propensity scores would have reduced the sample size of patients who experienced AML transformation. Instead, differences in baseline characteristics were controlled for using multivariable analyses as described below in the statistical analyses section. Additionally, a subpopulation of matched patient pairs who received azacitidine in first-line treatment was analyzed. In total, the three populations analyzed in this study were the overall unmatched population, overall matched population, and azacitidine matched population.
Study Measures
Baseline Demographic and Clinical Characteristics
Demographic characteristics were assessed on index date, while clinical characteristics were assessed at baseline. Demographics included age, gender, region (Midwest, Northeast, South, West, other/unknown); commercial or Medicare payer type; index year (2008–2019); and length of follow-up, which was calculated as the time between the index date and follow-up end date. The follow-up was captured as a continuous variable in months.
Clinical characteristics included the Charlson comorbidity index, presence of each comorbidity comprising the Charlson comorbidity index score at baseline, and supportive care measured at baseline. All comorbidities were captured using ICD-9-CM and ICD-10-CM diagnosis codes. The supportive care approaches that were reported included any use of granulocyte-macrophage colony-stimulating factor (GM-CSF), erythropoiesis stimulation, or transfusion.
Healthcare Resource Utilization (HCRU)
All-cause HCRU and transfusion episodes were evaluated over the entire follow-up, pre-AML, and post-AML periods. All-cause HCRU categories included medical services, pharmacy services, and transfusion episodes. Medical services included inpatient admission, emergency department visits, outpatient visits, SCT, chemotherapy visits, and supportive care visits. Outpatient prescription fills included subcategories for chemotherapy and supportive care. Transfusion episodes were composed of claims for transfusions with unique dates of service across all settings of care (inpatient admissions, emergency department visits, and outpatient visits).
Healthcare Costs
Healthcare costs were also measured during the entire follow-up, pre-AML, and post-AML periods. Costs comprised the allowed amount and were assessed as all-cause costs, which included all costs incurred during follow-up for any reason. All costs were adjusted to 2019 US dollars using the Bureau of Labor Statistics’ Medical Care Component of the Consumer Price Index.
Total healthcare costs were composed of both medical and pharmacy costs. The two categories were further divided to include outpatient prescription costs in the pharmacy category and inpatient admission, emergency department visits, outpatient physician office visits, other outpatient office visits, SCT, chemotherapy visits, and supportive care visits for the medical costs.
Statistical Analyses
Descriptive statistics were reported for demographics, clinical characteristics, HCRU (follow-up, pre-AML, and post-AML), and costs (follow-up, pre-AML, and post-AML) for patients who did and did not transform to AML. Categorical variables were summarized as counts and proportions, while continuous measures were summarized as means, standard deviations (SD), and medians. Statistical comparison between patients who transformed to AML and patients who did not transform was conducted using McNemar’s test for binary variables or a generalized linear model for categorical variables and paired t-test for continuous variables.
For the overall AML vs. non-AML groups, total costs were assessed to observe the trend before matching patients on follow-up time. Matching on follow-up time allowed for comparison of equivalent periods before and after AML between the two cohorts. For the matched cohorts, total costs across the three periods were further assessed in multivariable analysis. A generalized linear model with gamma distribution and a log link function was used for total, pre-AML, and post-AML total costs. The main independent variable was a binary indicator for transformation to AML, and the model controlled for age, gender, region, index year, insurance type, evidence of capitated payment, and baseline Charlson comorbidity index scores, transfusion, and other supportive care. The results of the cost model were summarized as adjusted costs and 95% CIs around the mean difference.
Results
A total of 393 patients with higher-risk MDS met the study inclusion criteria and comprised the overall population; 145 (36.9%) had evidence of AML transformation during the follow-up period and 248 (63.1%) did not. In the overall population, patients with higher-risk MDS who transformed to AML were slightly younger than patients who did not transform (median age: 73.0 years vs. 76.0 years, respectively). Although the number of patients requiring any supportive care was similar in the group who transformed vs. the group who did not transform (56.6% vs. 53.6%, respectively), the number of patients requiring transfusions was higher in the patients who transformed (47.6% vs. 39.1%, respectively) (Table 4—Supplementary Material).
After matching on follow-up time, 118 matched patient pairs remained and comprised the overall matched population. In this matched population, some baseline characteristics differed between the matched pairs (Table 1); patients who transformed to AML were younger than those who did not transform to AML (71.8 years vs. 76.1 years; P = 0.0004) and fewer patients who transformed to AML had a Charlson comorbidity index score of ≥ 2 compared to those who did not transform to AML (39.8% vs. 51.7%; P = 0.0376). At baseline, similar proportions of patients who did or did not transform to AML received any supportive care (57.6% vs. 56.8%; P = 0.8964) or transfusions (48.3% vs. 43.2%; P = 0.4227). Patients in both groups were followed for a median of approximately 12 months.
In the matched azacitidine population (N = 60), patients who transformed to AML were also younger than those who did not transform to AML (71.2 years vs. 77.2 years; P = 0.0002) (Table 1). Charlson comorbidity index score was similar in both groups. While the proportions of patients using supportive care, including transfusions, were numerically higher among patients who transformed to AML, statistical significance was not reached. The median follow-up time among these patients was approximately 9 months.
Healthcare Utilization
The key healthcare utilization services that differed between the patients who transformed to AML vs. those who did not transform to AML were hospitalization and supportive care use.
Hospitalization
In the overall unmatched population, the rate of hospitalization in the follow-up period was significantly higher in patients who transformed than in those who did not (58.6% vs. 47.2%, respectively; P = 0.0285). In the matched population, the rates of hospitalization was also significantly higher in patients who transformed than in those who did not during the entire follow-up period (58.5% vs. 44.1%; P = 0.0295) (Table 2) and post-AML (47.5% vs. 28.0%; P = 0.0028) (Table 5—Supplementary Material) periods. In the matched azacitidine population, the rates of hospitalization during the follow-up (Table 3) and post-AML (Table 6—Supplementary Material) periods were also higher for patients who transformed to AML compared with those who did not transform to AML. In all populations, no difference in the rate of hospitalization was observed between the two groups in the pre-AML period.
Supportive care
In the matched population, 93.2% of patients who had transformed to AML received supportive care vs. 83.9% of patients who did not transform (P = 0.0343) in the overall follow-up period (Table 2). In the pre- and post-AML periods, more patients who transformed to AML (84.8% and 71.2%, respectively) received supportive care compared to patients who did not transform to AML (73.7%; P = 0.0236 and 51.7%; P = 0.0005, respectively) (Table 5—Supplementary Material). In the matched azacitidine population, similar results on differences in supportive care use between those who transformed vs. those who did not were observed in the pre- and post-AML periods (Table 6—Supplementary Material).
Transfusions were the most commonly used supportive care treatment for patients with higher-risk MDS. In the matched population during the follow-up period, transfusion-related visits (87.3% vs. 68.6%; P = 0.0009 [data not shown in the table of results]) and the mean number of visits per patient per month (1.3 [1.4] vs. 0.6 [1.1]; P < 0.0001) in any setting of care were higher in patients who transformed to AML vs. those who did not. The proportions of patients with transfusion-related visits and mean (SD) number of visits in the pre-AML (77.1% vs. 55.1%; P = 0.0002 and 1.5 [2.3] vs. 0.6 [1.1]; P < 0.0001) and post-AML (69.5% vs. 41.5%; P < 0.0001 and 1.3 [1.6] vs. 0.6 [1.5]; P = 0.0017) periods were higher among patients who transformed to AML compared to patients who did not transform to AML. In the matched azacitidine subgroup, transfusion-related visits were also significantly higher among patients who transformed to AML compared to those who did not across all periods.
Healthcare Costs
In the overall unmatched population, the difference in total healthcare costs during the follow-up period was comparable to the costs observed among the matched population. The average total costs per patient per month in the overall unmatched population were $24,617 for patients who transformed to AML and $18,833 for those who did not transform (Fig. 6A—Supplementary Material). In the matched population, the average total costs per patient per month were $25,207 for patients who transformed to AML and $18,967 for patients who did not transform (Fig. 6B—Supplementary Material).
In the adjusted cost analysis, patients with higher-risk MDS who transformed to AML in the matched population incurred more costs per month than those who did not transform in the entire follow-up period ($25,964 vs. $19,150 per patient per month; P < 0.0001). The observed cost difference was more notable in the post-AML period ($36,424 vs. $14,860; P < 0.0001) (Fig. 1). In the pre-AML period, no significant difference was observed in total costs. For patients who were treated with first-line azacitidine, total costs per patient per month during the follow-up period ($26,633 vs. $17,379; P < 0.0023) and during the post-AML period ($37,951 vs. $13,839: P < 0.0001) remained significantly higher for patients with higher-risk MDS who transformed compared to those who did not transform to AML (Fig. 2).
In the overall follow-up period, the cost drivers in both the group who transformed to AML and the group who did not were outpatient, chemotherapy, and supportive care costs, but only supportive care costs were significantly different between the two groups. Patients who transformed to AML incurred on average $5885 per patient per month in supportive care costs, while patients who did not transform to AML incurred $3582 (P = 0.0080) per patient per month (Fig. 3). Costs associated with transfusions accounted for 81.3% of supportive care costs for patients who transformed to AML and 65.7% of supportive care costs for patients who did not transform to AML ($4789 vs. $2355, respectively; P = 0.0073) (Fig. 3).
In the post-AML period, differences were observed in the hospitalization, chemotherapy, and supportive care costs between the two groups. Hospitalization costs per patient per month were significantly higher for patients who transformed to AML compared to those who did not ($7950 vs. $1796, P = 0.0263) (Fig. 4). Patients who transformed to AML incurred significantly more chemotherapy-related costs compared to those who did not transform to AML ($7724 vs. $3420, P < 0.0084). In patients who transformed to AML, the mean cost of supportive care was $10,098 compared to patients who did not transform, who had a significantly lower mean cost of $2493 (P = 0.0011). The supportive care consisted of transfusion costs of $9701 for transformers and $1679 for non-transformers (Fig. 4).
These same results were observed for the matched azacitidine population, highlighting the burden of transformation to AML on healthcare costs, especially in the post-AML period. Although the hospitalization and supportive care costs were similar between the two groups in the overall follow-up period, in the post-AML period hospitalization, chemotherapy and supportive costs were significantly higher in patients who transformed to AML compared to those who did not transform to AML.
Discussion
This study evaluated the economic burden associated with transformation to AML among patients with higher-risk MDS who received chemotherapy treatment. The results of our matched cohort analysis showed that over a median follow-up time of 12 months, patients with higher-risk MDS who initiated treatment with chemotherapy and were part of a cohort of those who transformed to AML incurred on average $6815 more in total costs per patient per month compared to those in the cohort who did not transform to AML ($25,964 vs. $19,150 per patient per month).
Because approximately 40% of patients with higher-risk MDS transform to AML, which is one of the most expensive cancers to treat because of the costly medical interventions (i.e., transplantation), lengthy hospitalizations, and therapy/disease-related complications such as infections, the delay or prevention of transformation is a notable treatment goal [4, 6, 14, 15]. In our study, when the period following treatment initiation for patients with higher-risk MDS was divided into pre- and post-AML periods, among the cohort of patients in the overall matched population who transformed to AML, total cost of care was notably different in the post-AML period. In the post-AML period, patients with higher-risk MDS who transformed to AML incurred about $21,564 more in total costs per patient per month compared to those who did not transform to AML ($36,424 vs. $14,860 per patient per month).
To our knowledge, this is the first study to evaluate the economic impact of patients with higher-risk MDS who received treatment and subsequently transformed to AML. However, these results are consistent with results seen individually in MDS and AML and in other studies that are similar to ours. Bell et al. reported the mean all-cause total cost of higher-risk MDS treated with chemotherapy to be $17,361 per patient per month, which is similar to that in the cohort who did not experience AML transformation ($18,967) in our study [16]. In a cohort consisting of patients with de novo and antecedent AML who were treated, the mean all-cause total cost per patient per month was $21,055 [17]. The post-AML costs for the cohort who experienced AML transformation in our study are higher likely because our study included only patients with antecedent AML, a subgroup of AML, which is known to be more difficult to treat and has worse outcomes. Another study conducted among patients with MDS treated with HMA using SEER-Medicare data evaluated healthcare costs of MDS overall and also pre- and post-HMA-treatment failure (diagnosis of AML, HMA discontinuation, transfusion dependence, and death) [18]. The mean total all-cause cost was $12,494 per patient per month and the cost post-HMA-treatment failure ($19,242 per patient per month) was $5,433 higher than cost pre-HMA-treatment failure ($13,809 per patient per month) [18]. While treatment failure in the study by Stein et al. was not limited to AML transformation, the trend of increased costs in the period following treatment failure aligns with the increased costs we observed in the period following AML transformation. Patients who have progressed after HMA exposure may be less likely to benefit from continued treatment and should consider alternative treatment strategies [10,11,12,13].
We also specifically considered patients who received azacitidine as their first-line treatment for higher-risk MDS. Azacitidine has previously been associated with an OS benefit in MDS patients [10,11,12]. In our study, even when only considering patients who received azacitidine as their first-line therapy, we still observed higher HCRU and costs in patients who transformed to AML compared to those who did not. This highlights that even those receiving standard of care therapy for higher-risk MDS have an unmet need for improved treatment, which may result in reduced transformation to AML and improvements in HCRU and costs.
While previous evidence pointed to the increased clinical burden of AML, this study demonstrated that this increased clinical burden does translate into a higher economic burden among those patients who transform from higher-risk MDS to AML and further highlights the need for new therapies to delay or prevent transformation from higher-risk MDS to AML.
Limitations
Limitations to this study include those inherent to any retrospective study. Only diagnosis codes were used to identify patients with higher-risk MDS, and a lack of clinical data might have resulted in the inclusion of patients with a wide range of prognostic factors. The patient-matching approach in this study only used follow-up time and did not eliminate differences in the baseline characteristics of the patient groups. However, we conducted an adjusted analysis to address the imbalance in baseline characteristics and the results were consistent with what was observed for the unadjusted part. Indirect costs, such as productivity loss or other out-of-pocket expenses, could not be captured from the Optum claims database. Due to the lengthy data period, there could be a difference in management with chemotherapy between matched cohorts; however, we controlled for a year of treatment initiation in the adjusted analyses. We also observed more patients who experienced AML transformation initiated chemotherapy in earlier years compared to those who did not experience AML transformation (2008 to 2017: 77% vs. 63%, respectively). Given the recent increase in diagnostic testing for patients with AML, the cost of care following AML diagnosis might be underestimated. The results of this study may not be generalizable to a non-commercially insured population, since the Optum database captures data on a commercially insured and Managed Medicare population.
Conclusions
Patients with higher-risk MDS, with or without transformation to AML, incurred high healthcare costs over a median follow-up of approximately 12 months. Transformation from higher-risk MDS to AML significantly increased follow-up healthcare costs, highlighting an important need for treatments that prevent or delay transformation.
References
Komrokji RS, Kulasekararaj A, Al Ali NH, et al. Autoimmune diseases and myelodysplastic syndromes. Am J Hematol. 2016;91(5):E280–3.
Ma X, Does M, Raza A, Mayne ST. Myelodysplastic syndromes: incidence and survival in the United States. Cancer. 2007;109(8):1536–42.
Malcovati L, Della Porta MG, Strupp C, et al. Impact of the degree of anemia on the outcome of patients with myelodysplastic syndrome and its integration into the WHO classification-based Prognostic Scoring System (WPSS). Haematologica. 2011;96(10):1433–40.
Pfeilstocker M, Tuechler H, Sanz G, et al. Time-dependent changes in mortality and transformation risk in MDS. Blood. 2016;128(7):902–10.
Gore S. Classification, treatment goals, and management principles of myelodysplastic syndromes. Cancer Control. 2004;11(S6):S1–6.
Powers A, Faria C, Broder MS, et al. Hematologic complications, healthcare utilization, and costs in commercially insured patients with myelodysplastic syndrome receiving supportive care. Am Health Drug Benefits. 2012;5(7):455–65.
Wood EM, McQuilten ZK. Outpatient transfusions for myelodysplastic syndromes. Hematol Am Soc Hematol Educ Prog. 2020;2020(1):167–74.
Disperati P, Ichim CV, Tkachuk D, et al. Progression of myelodysplasia to acute lymphoblastic leukaemia: implications for disease biology. Leuk Res. 2006;30(2):233–9.
Meyers J, Yu Y, Kaye JA, Davis KL. Medicare fee-for-service enrollees with primary acute myeloid leukemia: an analysis of treatment patterns, survival, and healthcare resource utilization and costs. Appl Health Econ Health Policy. 2013;11:275–86.
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol. 2009;10(3):223–32.
Kantarjian H, Issa JP, Rosenfeld CS, et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer. 2006;106(8):1794–803.
Lübbert M, Suciu S, Baila L, et al. Low-dose decitabine versus best supportive care in elderly patients with intermediate- or high-risk myelodysplastic syndrome (MDS) ineligible for intensive chemotherapy: final results of the randomized phase III study of the European Organisation for Research and Treatment of Cancer Leukemia Group and the German MDS Study Group. J Clin Oncol. 2011;29(15):1987–96.
Silverman LR, Demakos EP, Peterson BL, et al. Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the Cancer and Leukemia Group B. J Clin Oncol. 2002;20(10):2429–40.
Wang HI, Aas E, Howell D, et al. Long-term medical costs and life expectancy of acute myeloid leukemia: a probabilistic decision model. Value Health. 2014;17(2):205–14.
Ostgard LSG, Medeiros BC, Sengelov H, et al. Epidemiology and clinical significance of secondary and therapy-related acute myeloid leukemia: a national population-based cohort study. J Clin Oncol. 2015;33(31):3641–55.
Bell JA, Galaznik A, Blazer M, et al. Economic burden of patients treated for higher-risk myelodysplastic syndromes (HR-MDS) in routine clinical care in the United States. Pharmacoecon Open. 2019;3(2):237–45.
Hagiwara M, Sharma A, Chung KC, et al. Healthcare resource utilization and costs in patients with newly diagnosed acute myeloid leukemia. J Med Econ. 2018;21(11):1119–30.
Stein EM, Bonifacio G, Latrémouille-Viau D, et al. Healthcare resource utilization and costs in patients with myelodysplastic syndromes treated with hypomethylating agents: a SEER-Medicare analysis. J Med Econ. 2021;24(1):234–43.
Acknowledgements
Funding
This study, including the journal’s Rapid Service and Open Access fees, was funded by Takeda Development Center Americas, Inc. (TDCA), Lexington, MA.
Medical Writing Assistance
We would like to acknowledge Sarah Castelo, PharmD, BCOP, of Xcenda LLC for medical writing support, which was funded by Takeda Development Center Americas, Inc. (TDCA).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Augustina Ogbonnaya, Eileen Farrelly, and Aditya Raju. Strategic oversight was provided by Vamsi Kota, Bridgette Kanz Schroader, Fjoralba Kristo, and Mehul Dalal. All authors commented on all versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Vamsi Kotais a consultant for Takeda Development Center Americas, Inc. Mehul Dalaland Fjoralba Kristoare employees of Takeda Development Center Americas, Inc. Augustina Ogbonnaya, Eileen Farrelly, Bridgette Kanz Schroader, and Aditya Rajuare employees of Xcenda, LLC, and Xcenda, LLC received funding to conduct this study.
Prior Presentation
The 16th International Congress on Myelodysplastic Syndromes in Toronto, Canada, on September 23–26, 2021.
Compliance with Ethics Guidelines
Ethics committee approval was not required for this study because of the retrospective, blinded nature of the data. In addition, permission to use the data for this this study was granted by the data owner.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due to a data use agreement.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.



Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kota, V., Ogbonnaya, A., Farrelly, E. et al. Economic Impact of Transformation to Acute Myeloid Leukemia Among Actively Managed Patients with Higher-Risk Myelodysplastic Syndromes in the United States. Adv Ther 40, 1655–1669 (2023). https://doi.org/10.1007/s12325-022-02370-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02370-4