Abstract
Objectives
The primary objective of this study was to predict healthcare cost trajectories for patients with newly diagnosed acute myeloid leukemia (AML) receiving allogeneic hematopoietic cell transplantation (alloHCT), as a function of days since chemotherapy initiation, days relative to alloHCT, and days before death or last date of insurance eligibility (LDE). An exploratory objective examined patients with AML receiving chemotherapy only.
Methods
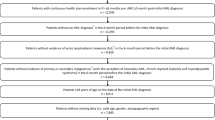
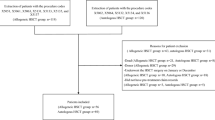
We used Optum’s de-identified Clinformatics® Data Mart Database to construct cumulative cost trajectories from chemotherapy initiation to death or LDE (through 31 December 2014) for US patients aged 20–74 years diagnosed between 1 March 2004 and 31 December 2013 (n = 187 alloHCT; n = 253 chemotherapy only). We used generalized additive modeling (GAM) to predict expected trajectories and bootstrapped confidence intervals (CIs) at user-specified intervals conditional on dates of alloHCT and death or LDE relative to chemotherapy initiation.
Results
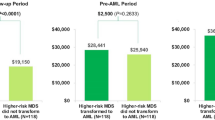
Expected costs (in 2017 values) for a hypothetical patient receiving alloHCT 60 days after chemotherapy initiation and followed for 5 years were $US572,000 (95% CI 517,000–633,000); $US119,000 (95% CI 51,000–192,000); $US102,000 (95% CI 0–285,000); $US79,000 (95% CI 0–233,000), for years 1–4, respectively, and either $US494,000 (95% CI 212,000–799,000) or $US108,000 (95% CI 0–230,000) in year 5, whether the patient died or was lost to follow-up on day 1825, respectively.
Conclusions
Rates of cost accrual varied over time since chemotherapy initiation, with accelerations around the time of alloHCT and death. GAM is a potentially useful approach for imputing longitudinal costs relative to treatment initiation and one or more intercurrent, clinical, or terminal events in randomized controlled trials or registries with unrecorded costs or for dynamic decision–analytic models.





Similar content being viewed by others
Data Availability Statement
Optum’s de-identified Clinformatics® Data Mart Database is commercially available. According to the terms of the data purchase agreement, the dataset used in this study cannot be shared. Analysis code is available at: https://github.com/djvanness/pharmacoecon_GAM_AML.
Notes
Corporate members.
References
Schiffer C, Anastasi J. Classification of acute myeloid leukemia. UpTodate. 2019. https://www.uptodate.com/contents/classification-of-acute-myeloid-leukemia. Accessed 23 Dec 2019.
BeTheMatch.org. Acute myeloid leukemia (AML). 2019. https://bethematch.org/patients-and-families/about-transplant/diseases-treated-by-transplant/acute-myeloid-leukemia/. Accessed 23 Dec 2019.
O’Donnell MR, Tallman MS, Abboud CN, Altman JK, Appelbaum FR, Arber DA, et al. Acute myeloid leukemia, version 3.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017;15:926–57.
Preussler JM, Denzen EM, Majhail NS. Costs and cost-effectiveness of hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2012;18:1620–8.
Majhail NS, Mau L-W, Denzen EM, Arneson TJ. Costs of autologous and allogeneic hematopoietic cell transplantation in the United States: a study using a large national private claims database. Bone Marrow Transplant. 2013;48:294.
Majhail NS, Mothukuri JM, Brunstein CG, Weisdorf DJ. Costs of hematopoietic cell transplantation: comparison of umbilical cord blood and matched related donor transplantation and the impact of posttransplant complications. Biol Blood Marrow Transplant. 2009;15:564–73.
Khera N, Zeliadt SB, Lee SJ. Economics of hematopoietic cell transplantation. Blood. 2012;120:1545–51.
Ashfaq K, Yahaya I, Hyde C, Andronis L, Barton P, Bayliss S, et al. Clinical effectiveness and cost-effectiveness of stem cell transplantation in the management of acute leukaemia: a systematic review. Health Technol Assess. 2010;14:1–141.
Yang H, Huang S, Zhu C-Y, Gao L, Zhu H-Y, Lv N, et al. The superiority of allogeneic hematopoietic stem cell transplantation over chemotherapy alone in the treatment of acute myeloid leukemia patients with mixed lineage leukemia (MLL) rearrangements. Med Sci Monit. 2016;22:2315–23.
Leunis A, Blommestein HM, Huijgens PC, Blijlevens NM, Jongen-Lavrencic M, Uyl-de Groot CA. The costs of initial treatment for patients with acute myeloid leukemia in the Netherlands. Leuk Res. 2013;37:245–50.
Van de Velde AL, Beutels P, Smits EL, Van Tendeloo VF, Nijs G, Anguille S, et al. Medical costs of treatment and survival of patients with acute myeloid leukemia in Belgium. Leuk Res. 2016;46:26–9.
Preussler JM, Meyer CL, Mau L-W, Majhail NS, Denzen EM, Edsall KC, et al. Healthcare costs and utilization for patients age 50–64 years with acute myeloid leukemia treated with chemotherapy or with chemotherapy and allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2017;23:1021–8.
Neumann PJ, Sanders GD, Russell LB, Siegel JE, Ganiats TG. Cost-effectiveness in health and medicine. New York: Oxford University Press; 2016.
Bramley T, Antao V, Lunacsek O, Hennenfent K, Masaquel A. The economic burden of end-of-life care in metastatic breast cancer. J Med Econ. 2016;19:1075–80.
Fletcher SA, Cronin AM, Zeidan AM, Odejide OO, Gore SD, Davidoff AJ, et al. Intensity of end-of-life care for patients with myelodysplastic syndromes: findings from a large national database. Cancer. 2016;122:1209–15.
Chastek B, Harley C, Kallich J, Newcomer L, Paoli CJ, Teitelbaum AH. Health care costs for patients with cancer at the end of life. J Oncol Pract. 2012;8:75s–80s.
Huynh TN, Kleerup EC, Wiley JF, Savitsky TD, Guse D, Garber BJ, et al. The frequency and cost of treatment perceived to be futile in critical care. JAMA Intern Med. 2013;173:1887–94.
Earle CC, Landrum MB, Souza JM, Neville BA, Weeks JC, Ayanian JZ. Aggressiveness of cancer care near the end of life: is it a quality-of-care issue? J Clin Oncol. 2008;26:3860–6.
Barlow WE. Overview of methods to estimate the medical costs of cancer. Med Care. 2009;47:S33–6.
Guy GP, Ekwueme DU, Yabroff KR, Dowling EC, Li C, Rodriguez JL, et al. Economic burden of cancer survivorship among adults in the United States. J Clin Oncol. 2013;31:3749–57.
Brown ML, Riley GF, Schussler N, Etzioni R. Estimating health care costs related to cancer treatment from SEER-Medicare data. Med Care. 2002;40:IV104–17.
Yabroff KR, Lamont EB, Mariotto A, Warren JL, Topor M, Meekins A, et al. Cost of care for elderly cancer patients in the United States. J Natl Cancer Inst. 2008;100:630–41.
Mariotto AB, Robin Yabroff K, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. 2011;103:117–28.
Li L, Wu C-H, Ning J, Huang X, Shih Y-CT, Shen Y. Semiparametric estimation of longitudinal medical cost trajectory. J Am Stat Assoc. 2018;113:582–92.
Liu L. Joint modeling longitudinal semi-continuous data and survival, with application to longitudinal medical cost data. Stat Med. 2009;28:972–86.
Liu L, Wolfe RA, Kalbfleisch JD. A shared random effects model for censored medical costs and mortality. Stat Med. 2007;26:139–55.
Wilson LS, Tesoro R, Elkin EP, Sadetsky N, Broering JM, Latini DM, et al. Cumulative cost pattern comparison of prostate cancer treatments. Cancer Interdiscip Int J Am Cancer Soc. 2007;109:518–27.
Levy JF, Rosenberg MA. A latent class approach to modeling trajectories of health care cost in pediatric cystic fibrosis. Med Decis Mak. 2019;39:593–604.
Karnon J. Alternative decision modelling techniques for the evaluation of health care technologies: Markov processes versus discrete event simulation. Health Econ. 2003;12:837–48.
Williams C, Lewsey JD, Mackay DF, Briggs AH. Estimation of survival probabilities for use in cost-effectiveness analyses: a comparison of a multi-state modeling survival analysis approach with partitioned survival and Markov decision-analytic modeling. Med Decis Mak. 2017;37:427–39.
Hauser TH, Ho KK. Accuracy of on-line databases in determining vital status. J Clin Epidemiol. 2001;54:1267–70.
da Graca B, Filardo G, Nicewander D. Consequences for healthcare quality and research of the exclusion of records from the Death Master File. Circ Cardiovasc Qual Outcomes. 2013;6:124–8.
Preussler JM, Mau L-W, Majhail NS, Meyer CL, Denzen EM, Edsall KC, et al. Administrative claims data for economic analyses in hematopoietic cell transplantation: challenges and opportunities. Biol Blood Marrow Transplant. 2016;22:1738–46.
Hastie T. gam: Generalized additive models. 2019. https://CRAN.R-project.org/package=gam. Accessed 7 Nov 2019.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2019. https://www.r-project.org/. Accessed 7 Nov 2019.
Reps JM, Rijnbeek PR, Ryan PB. Identifying the DEAD: development and validation of a patient-level model to predict death status in population-level claims data. Drug Saf. 2019;42:1377–86.
Funk MJ, Westreich D, Wiesen C, Stürmer T, Brookhart MA, Davidian M. Doubly robust estimation of causal effects. Am J Epidemiol. 2011;173:761–7.
Hastie T, Tibshirani R. Generalized additive models for medical research. Stat Methods Med Res. 1995;4:187–96.
Dominici F, McDermott A, Zeger SL, Samet JM. On the use of generalized additive models in time-series studies of air pollution and health. Am J Epidemiol. 2002;156:193–203.
Setodji CM, Scheuner M, Pankow JS, Blumenthal RS, Chen H, Keeler E. A graphical method for assessing risk factor threshold values using the generalized additive model: the multi-ethnic study of atherosclerosis. Health Serv Outcomes Res Methodol. 2012;12:62–79.
Webster T, Vieira V, Weinberg J, Aschengrau A. Method for mapping population-based case-control studies: an application using generalized additive models. Int J Health Geogr. 2006;5:26.
Pullenayegum EM, Wong HS, Childs A. Generalized additive models for the analysis of EQ-5D utility data. Med Decis Mak. 2013;33:244–51.
Jansen JP. Network meta-analysis of survival data with fractional polynomials. BMC Med Res Methodol. 2011;11:61.
Tsujitani M, Tanaka Y. Analysis of heart transplant survival data using generalized additive models. Comput Math Methods Med. 2013;2013:609857.
Royston P, Parmar MK. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat Med. 2002;21:2175–97.
Freeman SC, Carpenter JR. Bayesian one-step IPD network meta-analysis of time-to-event data using Royston–Parmar models. Res Synth Methods. 2017;8:451–64.
Blough DK, Ramsey SD. Using generalized linear models to assess medical care costs. Health Serv Outcomes Res Methodol. 2000;1:185–202.
Harre FE, Lee KL, Pollock BG. Regression models in clinical studies: determining relationships between predictors and response. J Natl Cancer Inst. 1988;80:1198–202.
Duan N, Manning WG, Morris CN, Newhouse JP. A comparison of alternative models for the demand for medical care. J Bus Econ Stat. 1983;1:115–26.
Mullahy J. Much ado about two: reconsidering retransformation and the two-part model in health econometrics. J Health Econ. 1998;17:247–81.
Acknowledgements
The authors thank Kellene Bergen for her contributions to data interpretation and members of the CIBMTR® (Center for International Blood and Marrow Transplant Research®) statistical review panel for their helpful comments and suggestions.
Disclosure
CIBMTR® (Center for International Blood and Marrow Transplant Research®) is a research collaboration between the National Marrow Donor Program®/Be The Match® and the Medical College of Wisconsin. CIBMTR® is supported primarily by Public Health Service Grant/cooperative agreement 5U24CA076518 from the National Cancer Institute (NCI), the National Heart, Lung and Blood Institute (NHLBI), and the National Institute of Allergy and Infectious Diseases (NIAID); Grant/cooperative agreement 1U24HL138660 from NHLBI and NCI; contract HHSH250201700006C with the Health Resources and Services Administration/Department of Health and Human Service (HRSA/DHHS); Grants N00014-17-1-2388, N00014-17-1-2850, and N00014-18-1-2045 from the Office of Naval Research; and Grants from Adaptive Biotechnologies, Amgen, Inc.,Footnote 1 anonymous donation to the Medical College of Wisconsin, Astellas Pharma US, Atara Biotherapeutics, Inc., Be the Match Foundation, bluebird bio, Inc.,1 Bristol Myers Squibb Oncology,1 Celgene Corporation,1 Chimerix, Inc.,1 CytoSen Therapeutics, Inc.,1 Fred Hutchinson Cancer Research Center, Gamida Cell Ltd., Gilead Sciences, Inc., HistoGenetics, Inc., Immucor, Incyte Corporation,1 Janssen Scientific Affairs, LLC, Jazz Pharmaceuticals, Inc.,1 Karius, Inc., Karyopharm Therapeutics, Inc., Kite Pharma,1 Inc., Medac, GmbH, Mediware,1 The Medical College of Wisconsin, Merck & Co., Inc.,1 Mesoblast,1 MesoScale Diagnostics, Inc., Millennium, the Takeda Oncology Co., Miltenyi Biotec, Inc.,1 Mundipharma EDO, National Marrow Donor Program, Novartis Pharmaceuticals Corporation, PCORI, Pfizer, Inc.,1 Pharmacyclics, LLC,1 PIRCHE AG, Sanofi Genzyme,1 Seattle Genetics,1 Shire, Spectrum Pharmaceuticals, Inc., St. Baldrick’s Foundation, Swedish Orphan Biovitrum, Inc., Takeda Oncology,1 and University of Minnesota. The views expressed in this article do not reflect the official policy or position of the National Institute of Health, the Department of the Navy, the Department of Defense, Health Resources and Services Administration (HRSA) or any other agency of the US Government. The Health Services Research program is supported in part by Health Resources and Services Administration contract no. HHSH234200637018C. The views expressed in this article do not reflect the official policy or position of the Health Resources and Services Administration or the National Marrow Donor Program®/Be The Match®.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Lih-Wen Mau, Jaime M. Preussler, Linda J. Burns, Susan Leppke, Christa L. Meyer, and Tatenda Mupfudze report employment by the National Marrow Donor Program®/Be The Match® in connection with the work; Navneet S. Majhail and Navneet S. Majhail report consulting income from Anthem Inc., Mallinckrodt, Nkarta, and Inctye for unrelated work; Wael Saber and Patricia Steinert report employment by the Center for International Blood and Marrow Transplant Research; David J. Vanness reports compensation from the National Marrow Donor Program®/Be The Match® for this work and consulting income from Novartis, Merck, CHEORS (Complete Health Economics Outcomes and Research Solutions), Medical Decision Modeling Inc., and Bristol-Myers Squibb for unrelated work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mau, LW., Preussler, J.M., Burns, L.J. et al. Healthcare Costs of Treating Privately Insured Patients with Acute Myeloid Leukemia in the United States from 2004 to 2014: A Generalized Additive Modeling Approach. PharmacoEconomics 38, 515–526 (2020). https://doi.org/10.1007/s40273-020-00891-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-020-00891-w