Abstract
Aims
Low-density lipoprotein cholesterol (LDL-C) reduction in hypercholesterolemia patients at very high cardiovascular (CV) risk is essential in preventing future CV events. The objective was to assess the perception on hypercholesterolemia management in secondary prevention in Germany.
Methods
PROCYON was a two-part online survey, including a patient questionnaire as well as a physician questionnaire.
Results
A total of 109 general practitioners, internists, and cardiologists participated. The current ESC/EAS recommendation for high-risk patients is followed by 19.3% of the physicians. The majority (80.7%) reported an LDL-C target failure rate of at least 30%. More than two thirds (71.6%) have stated treating less than half of their patients with the maximum approved statin dose. The survey included 1696 secondary prevention patients. The majority (86.7%) consult their general practitioner for hypercholesterolemia; 54.0% consult a cardiologist (multiple answers allowed). Most patients (87.0%) were receiving lipid-lowering medication. Among these, 800 (54.2%) reported improved LDL-C levels since diagnosis, 569 (38.6%) reported no improvement, and 106 (7.2%) had no information. Of the treated patients with (N’ = 800) and without (N’ = 569) improvement, 34.3% vs. 37.3% were on their initial drug and dose, 24.8% vs. 23.7% received multiple drug therapy, 48.9% vs. 48.9% reported a dose change, and 16.1% vs. 14.2% had discontinued at least one drug (multiple answers). Disease knowledge was rated as good or very good by 29.8% of patients.
Conclusion
PROCYON demonstrated insufficient ESC/EAS guideline implementation regarding target levels and therapeutic escalation strategies. Furthermore, a lack of specialist involvement and patient education was identified.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Secondary prevention in patients with previous cardiovascular (CV) events is essential as the re-event risk can be considerably high depending on the number of risk factors |
The PROCYON survey data were analyzed to identify potential gaps in the management of hypercholesterolemia in secondary prevention and potential differences between primary and secondary prevention in clinical practice in Germany |
Screening efforts were found to be insufficient with more than half of hypercholesterolemia patients in secondary prevention being identified upon a CV event only |
Recommended target levels for secondary prevention were reported to be adhered to by one fifth of physicians only, the maximum approved statin dose is rarely applied, and more than one third of patients reported no improvement of their Low-density lipoprotein cholesterol (LDL-C) levels |
Despite the high risk of fatal re-events in secondary prevention, disease management is almost as insufficient as in primary prevention and urgently needs to be optimized |
Introduction
Low-density lipoprotein cholesterol (LDL-C) is a known risk factor for atherosclerotic cardiovascular disease (ASCVD) [1]. A linear correlation between LDL-C levels and cardiovascular (CV) events has been established [2]. Mendelian randomization studies suggest that an LDL-C reduction of 50% reduces the absolute risk for CVD over 10 years by 20% to 43%, depending on the baseline LDL-C level [2]. Therefore, LDL-C lowering is an integral part of the 2019 guidelines of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) for the management of dyslipidemias [3]. The guideline recommends aligning the intensity of medical intervention to the individual level of CV risk. Secondary prevention patients with previous ASCVD belong to the very high-risk group [3]. The 3-year risk of re-events was estimated to be 3.5% even in patients without any additional risk indicators and increases with the number of risk factors, reaching a 3-year risk of re-events as high as 58.6% in patients with seven or more risk indicators [4]. For these patients, an LDL-C reduction of ≥ 50% and an LDL-C target level of < 55 mg/dl are recommended [3].
However, LDL-C targets often remain unattained. According to the DA VINCI study, only 18% of very high-risk patients currently achieve the ESC/EAS 2019 target levels in Europe [5]. Even if the previous version of the recommendations is considered (< 70 mg/dl for very high-risk patients), the target was achieved in only 39% according to the DA VINCI study [5] and in 18% of the patients according to a systematic review [6]. In view of the available pharmacotherapeutic options in 2021, however, poor target achievement is remarkable. According to a simulation study applying the 2019 ESC/EAS recommendations, a target level of < 55 mg/dl could be reached by > 90% of the patients with available lipid-lowering drugs [7].
The present survey aimed to identify possible reasons for insufficient target attainment in hypercholesterolemia management in secondary prevention patients in Germany. Results of a primary prevention population have been published previously [8].
Methods
Data Collection
PROCYON was a two-part online survey on disease perception, awareness, burden, and management of hypercholesterolemia consisting of a patient survey and a physician survey. Details on inclusion criteria, patient and physician recruitment, and the questionnaires have been published previously [8].
Shortly, patients had to be ≥ 18 years of age, currently living in Germany, and diagnosed with hypercholesterolemia. The web-based questionnaire of the patient survey included up to 37 questions on hypercholesterolemia-related medical history, comorbidities, adherence, and disease awareness. Patient self-activation was measured using the PAM-13 Patient Activation Measure by Insignia Health [9]. It defines four stages of activation, with 1 being the lowest level of activation and 4 being the highest [10]. Patient data were anonymized, and only aggregated data are presented.
The physician survey included general practitioners as well as resident cardiologists and internists, who treat at least 50 patients with hypercholesterolemia and are in charge for hypercholesterolemia-related treatment decisions. The online questionnaire included up to 33 questions on LDL-C-associated risk perception, guideline awareness, patient management, and treatment decisions. No individual patient data were collected in the physician survey.
The survey has been conducted in accordance with all relevant guidelines and regulations applicable in Germany. There is no local requirement for an ethics committee approval or written informed consent for survey research. All patients participated voluntarily, and informed consent to data collection, processing and analysis was obtained electronically from all subjects prior to the survey. Patient data were anonymized and aggregated for analysis. All physicians gave voluntary consent before participation.
Statistics
Patients and physicians who answered all questions were included in the analysis. The present analysis included secondary prevention patients with prior myocardial infarction, stroke, peripheral arterial occlusive disease, or bypass surgery.
Descriptive statistics are shown for all patient and physician characteristics. Categorical variables were summarized using frequency counts and percentages. Continuous variables were summarized as means including standard deviations and medians. No formal statistical testing for group comparisons was performed.
Results
Physicians’ Perspective
In total, 109 physicians participated in the survey. Characteristics, details on medical experience and responsibilities, and results regarding general awareness of LDL-C importance have been published previously [8].
The current ESC/EAS recommendation for an LDL-C target level of 55 mg/dl in combination with a 50% reduction in high-risk patients is adhered to by 19.3% of the physicians (n = 21), with the highest rate among cardiologists (n = 7; 30.4% of all cardiologists), followed by general practitioners (n = 7; 16.7% of all general practitioners) and internists (n = 7; 15.9% of all internists). Two thirds (n = 71; 65.1%) aim at a sole target of 55 mg/dl LDL-C, and 28.4% (n = 31) aim at a sole target of 50% LDL-C reduction.
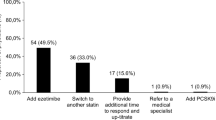
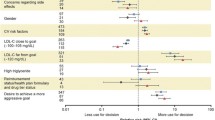
The majority of physicians (n = 88; 80.7%) reported an LDL-C target failure rate in high-risk patients of at least 30%. An attainment rate of at least 75% among their patients was reported by 21 physicians (19.3%; 9 general practitioners, 7 internists and 5 cardiologists). On the one hand, most of the physicians (n = 75; 68.8%) reported that statin intolerability hindered LDL-C target attainment in < 20% of their patients. On the other, the majority (n = 78; 71.6%) described treating less than half of their patients with the maximum approved dose.
Patients’ Health Care Setting
The survey was completed by 5494 patients; 1696 constitute the secondary prevention population. The median age of secondary prevention patients was 64.5 years, 42.5% were female, 7.8% had genetically confirmed familial hypercholesterolemia (FH), and the most common comorbidities were hypertension, obesity, and diabetes type 2 (Table 1). More than half of the patients with ASCVD (58.0%) received their hypercholesterolemia diagnosis during CV-related hospitalization and only 34.9% during routine check-ups. The median time since diagnosis was 10.0 years. Most patients (86.7%) currently consult their general practitioner for their hypercholesterolemia; 54.0% consult a cardiologist (multiple answers were allowed, i.e., some patients consulted a GP and a cardiologist). One third (32.8%) have LDL-C assessments twice per year, and 45.1% at least once per quarter (Table 1).
Patients’ Treatment Status
Most patients (n = 1475; 87.0%) were receiving lipid-lowering medication. More than half (54.2%) of these treated patients stated that their LDL-C has improved since diagnosis, 569 (38.6%) reported no improvement, and 106 (7.2%) had no information (Table 2). Of the treated patients with (N’ = 800) and without (N’ = 569) improvement, in both groups approximately one third of patients were on their initial drug and dose, one sixth discontinued at least one drug, half reported a dose change, and one quarter received multiple drug therapy (Table 2).
Compliance, Patient Information, and Activation
The treating physician was mentioned as the most common source of information by 1298 patients (76.5%) followed by online resources (n = 714; 42.1%). Half of patients (n = 783; 46.2%) rated the information they received from their physician as good or very good, 35.6% (n = 603) as sufficient. Patient groups were rarely used as a source of information (n = 66; 3.9%).
One quarter of patients (n = 505; 29.8%) rated their knowledge about elevated LDL-C as good or very good. Approximately one third of patients (n = 602; 35.5%) knew their current LDL-C level. Less than half of patients (n = 679; 40.0%) knew their target LDL-C level, and most these patients (n = 569; 83.8%) considered it important or very important to achieve their target.
Of note, diet is the most important factor for LDL-C reduction according to half of the patients, followed by LDL-C-lowering drugs and physical activity (Fig. 1). The most frequently reported adaption since diagnosis was the introduction of medication, followed by change of dietary habits, increased physical activity, and tobacco abstinence (Fig. 2). More than two thirds of the patients (69.8%) receiving lipid-lowering therapy considered their LDL-C medication as important as other medications, and 16.8% considered it more important (Table 3).
Almost all treated patients (95.0%) reported to take their medication as regularly or nearly as regularly as prescribed, and 15.0% had discontinued at least one medication. Of the patients who discontinued medication, 34.4% stopped it on their own motivation. Side effects were reported as the most common reason for medication discontinuation. In total, 45.8% of the treated patients had experienced side effects, with muscle pain being most frequently reported (Table 3).
Half of the patients (n = 816; 48.1%) were satisfied with their current treatment. One third was worried about their elevated LDL-C levels (n = 539; 31.8%), and some patients wished to receive another therapy form (n = 308; 18.2%) or were bothered by the need for frequent drug administration (n = 271; 16.0%). A patient activation (PAM) level of 3 or 4 was reached by 71.6% of the patients (Fig. 3).
Discussion
PROCYON suggests that most patients in secondary prevention receive pharmacotherapy. However, on patients’ impression LDL-C levels improved in only half of the patients since diagnosis despite receiving pharmacological treatment. Thus, it can be assumed that a large proportion of patients with hypercholesterolemia and prior ASCVD was insufficiently treated and at a higher risk of recurrent CV events. US registry data showed that insufficient treatment is common with 52.7% of patients in secondary prevention being untreated or treated on a lower intensity than recommended [11]. The US registry GOULD, a large US registry with > 5000 ASCVD patients whose LDL-C was insufficiently controlled or who received a PCSK9 inhibitor and 113 physician providers, demonstrated that the lipid-lowering therapy was intensified in only 17.1% of patients with ASCVD and LDL-C levels > 70 mg/dl over the next 2 years [12]. Consequently, several studies reported a lack of target attainment in clinical practice. A German cohort study including > 14,000 ASCVD patients treated with moderate to high-intensity statins by general practioners and specialists identified an attainment failure rate of 80.5% for a target of < 70 mg/dl [13]. The cross-sectional, observational DYSIS study with almost 60,000 statin-treated outpatients in 30 countries across Europe, the Middle East, Africa, Asia, and Canada showed that German patients exhibited the lowest level of target attainment [14]. Data obtained in the German LIMA study and in the Turkish EPHESUS registry further add to this notion as only 7% to 10% of LIMA patients and 18% of EPHESUS patients attained LDL-C levels < 70 mg/dl at any point during follow-up [15, 16]. These data highlight an urgent need for improvement in German patient care to increase target attainment rates, especially in light of the intensified target levels within the EAS/ESC 2019 guidelines compared to the previous version. PROCYON points to possible reasons for insufficient target attainment in secondary prevention.
According to PROCYON, only two thirds of physicians implemented current guideline recommendation with respect to target LDL-C levels. Furthermore, despite being insufficiently treated, a relevant proportion of patients did not undergo treatment escalation, i.e., dose escalation, treatment switch, or combination therapy.
However, early escalation of treatment is essential as the target attainment rate increases with the intensity of drug therapy. This is mostly important given that patients with a previous CV event have a median estimated 10-year risk for recurrent events of 17% that increases to 30% or higher in patients with elevated LDL-C levels [17]. LDL-C reduction of 50% reduces the absolute risk for CVD over 10 years by 50% [2]. In the DA VINCI study, among very high-risk patients goal attainment rate according to ESC/EAS 2019 was only 14% with statin monotherapy, 37% with ezetimibe combination therapy, and 57% with PCSK9 inhibitor combination therapy [5]. This is in sharp contrast to the theoretical potential of available therapies. A recently published simulation study based on the SWEDEHEART register in Sweden suggested that > 90% of patients could reach the target levels with statins, ezetimibe, and PCSK9 inhibitors [7]. However, half of the patients in secondary prevention would require PCSK9 inhibitors, and the authors concluded that this might constitute a financial burden to health systems [7]. Therefore, requirements for reimbursement and the fact that in Germany PCSK9 inhibitor treatment can only be initiated by certain specialties such as cardiology, nephrology, endocrinology, angiology, and lipidology might be another obstacle for target attainment. In PROCYON, general practitioners and internists are involved in the management of secondary prevention patients, while cardiologists are only seen by half of the patients. In addition, data published by Barter et al. suggest that physicians in Germany seem to be reluctant to implement the ESC/EAS 2019 LDL-C target level recommendations. Barter et al. have reported a target level of 129 mg/dl in clinical practice in Germany and identified uncertainties related to the safety of statin therapy as well as the safety of very low LDL-C levels. The authors concluded that there is a high need for educational programs to increase awareness of the current evidence on dyslipidemia management [18]. This is further supported by the German S3 guideline on cardiovascular rehabilitation, which follows the EAS/ESC 2019 recommendations regarding LDL-C target levels [19]. The German S3 guideline on management of stroke patients, which has been published only recently in 2022 by DEGAM (Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin), also affirms a reduction to values recommended by EAS/ESC [20].
Given that statin intolerance was identified as a minor problem by the physicians in PROCYON, it remains unclear why the majority of physicians in PROCYON escalate statins to the maximum tolerated dose in only half of their patients. In a German cohort study with LDL-C target attainment in only 10% of high-risk patients, 63% of the treating physicians thought they had reached the individual LDL-C goal in a subjective assessment [21]. Incomplete utilization of the potential of lipid-lowering drugs might be a consequence of the flawed self-assessment. Interdisciplinary patient management could overcome these issues and needs to be strengthened. In this respect, lipidological competence centers and networks as suggested by Heigl et al. deserve increased attention [22]. In PROCYON, 5.5% of patients were referred to a lipid clinic. The German healthcare system intends that patients should initially see a GP for medical consultation. The latter then refers patients to the relevant specialist, e.g., to a cardiologist if cardiological diagnostic work-up or regular cardiological follow-up is required. This was reflected in PROCYON, where 86.7% of patients consulted GPs, and 54.0% see a cardiologist. At present only a minority of patients with lipid disorders are referred to lipid clinics. In general, most patients in secondary prevention could probably benefit by referrals to lipid clinics and tighter cooperation between GPs and lipid clinics could probably result in a significant improvement in secondary prevention. Therefore, the German Lipid Association (DGFF) already promotes the training and qualification as a certified lipidologist [22]. Networking of lipidologists, GPs, and specialists will increase awareness and target attainment each region.
From a patients’ perspective, the present survey implies a lack of knowledge on the disease and individual target levels in more than half of the patients. This could potentially result in a lack of risk awareness, neglect of the importance of adequate treatment, and poor patient activation and adherence. Accordingly, insufficient patient education has previously been shown to be negatively related to health outcomes in hypercholesterolemia [23]. Similar to the results of PROCYON, a recent observational study reported that a relevant proportion of patients consider diet and exercise as more important than drug therapy and ignore the need for continuous treatment [24]. As a consequence, 63% of the secondary prevention patients discontinued their medication in that study [24], whereas in PROCYON, adherence was higher with a patient-reported discontinuation rate of only 15%, mainly due to side effects. Adherence is also impacted by incorrect or insufficient treatment advice [25]. Misinformation on drug side effects and beliefs of medication overuse might play a role in adherence of hypercholesterolemia patients as was found by Hagger et al. in a model analysis of patients’ generalized beliefs about medication and treatment [26]. Moreover, statin discontinuation has been demonstrated to increase CV mortality in a French study [27] and Danish study, where the increase was shown to be related to negative statin-related news releases [28]. Inappropriate patient awareness of the importance of pharmacotherapy and misinformation hampers the achievement of treatment goals.
The need for patient education is substantiated by results of the GOULD registry, which identified substantial knowledge gaps with respect to the disease and its treatment. Two thirds of participating physicians felt that nonadherence was primarily due to a lack of awareness of the importance of drug treatment. Less than one third of patients knew that their lipid-lowering medication was prescribed to reduce their CV risk, and two thirds did not know their current LDL-C level or their LDL-C goal [29]. The authors discussed that addressing these educational gaps could improve treatment adherence and thereby reduce the risk of recurrent events. [29]. The GOULD registry findings are well in line with the current PROCYON patient-reported results and underline that those efforts should be made to increase awareness of the disease and the importance of drug therapy. There have been attempts to improve secondary prevention in Germany. One example is the “Auf Ziel” campaign, initiated in several German clinics by the DGFF, which aimed to achieve LDL-C targets in patients with ST-elevation myocardial infarction (STEMI). The interdisciplinary cohort study “Jena auf Ziel” [30] has been initiated to investigate and support LDL-C target attainment in patients after STEMI. Two strategies were combined to ensure optimal target achievement: (1) early combination therapy and (2) patient education, activation, and empowerment. Patients will be encouraged and enabled to play a key role in the transition from inpatient to outpatient care and in successful target achievement. In addition, the study involves interdisciplinary networking efforts, between cardiologists, lipidologists, and general practitioners. The study showed that by using this strategy, 80% of patients attained LDL-C targets already at the first post-discharge follow-up on a combination of atorvastatin 80 mg and ezetimibe 10 mg [30]. Schäfer et al. followed a standard-operating procedure for secondary prevention to get STEMI patients on LDL-C targets [31]. They initiated high-intensity statin therapy upon admission in almost all patients, and those with LDL-C > 3.1 mmol/l were additionally treated with ezetimibe 10 mg. As a result, more than the half of patients achieved an LDL-C target < 1.4 mmol/l. Another strategy is the so-called “virtual lipid clinics,” a practice which was implemented in Spain by García et al. [32]. The authors reported successful LDL-C target attainment (in > 80% patients) in the setting of virtual lipid clinics, where patients were followed-up by phone call.
Furthermore, patients should be motivated to become more active in disease management, as PAM13 results showed that there is room for improvement. Farmalarm, a smartphone app developed for stroke patients, is an example of successful use of an application for patient activation. The rate of patients in control of their hypercholesterolemia was significantly higher in the group using Farmalarm compared to the control group [33]. Mobile apps are also implemented in other studies, aiming to improve the secondary prevention and adherence to lipid-lowering therapy, such as American Heart Association’s Cholesterol CarePlan [34] and afterAMI study [35].
Moreover, patient organizations and self-help groups can provide further support, especially in patients with homozygous or heterozygous FH [36, 37]. Patients affected by a genetically determined disease often feel left alone with their diagnosis. Networking with other patients can be particularly helpful to master everyday life, to overcome disease-associated difficulties, and to gain knowledge about the disease and treatment options. Within patient organizations or self-help groups, patients can find mutual help and motivation [36, 37]. Patient groups were underrepresented as a source of information in PROCYON; therefore, their role should be strengthened.
It also has to be considered that a major CV event is traumatic, and psychological issues are common in these patients. The results of a cohort study revealed that approximately 30% of patients in secondary prevention had moderate or high psychological distress. Furthermore, it was shown that patients with higher levels of psychological distress were less likely to be adherent to their medications [38]. Another cohort study found that statin-treated patients with frequent somatic anxiety-related symptoms had a 33% increased risk of nonadherence to the therapy compared to those without. The authors assumed that patients with anxiety may be overly vigilant toward statin side effects, resulting in an increased discontinuation rate [39]. Psychological distress in secondary prevention patients therefore must be addressed to improve treatment and prognosis.
Finally, CV events still have an in-hospital mortality of about 10% and account for 1.2 billion euros (2.5%) of in-hospital health expenses in Germany [40]. Early screening for hypercholesterolemia could help to identify high-risk individuals. PROCYON identified insufficient screening efforts, as more than half of hypercholesterolemia patients in secondary prevention were identified upon a CV event. Therefore, standard routine hypercholesterolemia screening must be consistently implemented in clinical practice and abnormal values must be given the necessary attention. Physicians’ and patients’ awareness about the relevance of early screening has to be established. The situation has already improved, as screening for hypercholesterolemia has just recently become reimbursable in Germany as part of the routine check-up in young adults once between 18 and 34 years of age and every 3 years afterwards [41]. However, earlier screening is supported by data on the high prevalence of elevated LDL-C levels in preschool children as early as 5 years of age [42]. Routine screening for early detection of hypercholesterolemia has to be followed by effective primary prevention. Previously published results of PROCYON on primary prevention have identified issues in this area [8].
Limitations of the survey have been described previously [8]. Shortly, except for PAM-13, no validated questionnaire was available to support the study objective. Therefore, the results need to be interpreted carefully and need further confirmation. Nevertheless, the present results provide valuable insight on potential issues in management of patients with hypercholesterolemia in clinical practice. Furthermore, web-based medical surveys are prone to a potential participation bias with better education and health state among respondents compared to non-respondents [43]. Survey results might further be biased by social desirability [44], and participants with higher self-activation might be overrepresented. Survey participation of patients was not encouraged by incentives. Physicians received a small expense allowance; however, only a minor response bias is expected.
Conclusion
In summary, PROCYON implies insufficient LDL-C target attainment despite frequent control assessments. From the physicians’ perspective, insufficient implementation of guidelines with respect to target levels and therapeutic strategies might be one reason. A potentially flawed self-assessment of the treating physicians and differing treatment targets among different guidelines further add to the problem. From the patients’ perspective, insufficient education on the disease and related treatment goals resulting in a lack of activation and patient empowerment might be involved. Strategies to overcome these issues include intensified interdisciplinary networking and professional education as well as patient activation programs and involvement of patient organizations.
References
Ference BA, Graham I, Tokgozoglu L, Catapano AL. Impact of lipids on cardiovascular health: JACC health promotion series. J Am Coll Cardiol. 2018;72(10):1141–56. https://doi.org/10.1016/j.jacc.2018.06.046.
Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38(32):2459–72. https://doi.org/10.1093/eurheartj/ehx144.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88. https://doi.org/10.1093/eurheartj/ehz455.
Bohula EA, Bonaca MP, Braunwald E, et al. Atherothrombotic risk stratification and the efficacy and safety of vorapaxar in patients with stable ischemic heart disease and previous myocardial infarction. Circulation. 2016;134(4):304–13. https://doi.org/10.1161/CIRCULATIONAHA.115.019861.
Ray KK, Molemans B, Schoonen WM, et al. EU-wide cross-sectional observational study of lipid-modifying therapy use in secondary and primary care: the DA VINCI study. Eur J Prev Cardiol. 2020. https://doi.org/10.1093/eurjpc/zwaa047.
Bruckert E, Parhofer KG, Gonzalez-Juanatey JR, et al. Proportion of high-risk/very high-risk patients in Europe with low-density lipoprotein cholesterol at target according to European guidelines: a systematic review. Adv Ther. 2020;37(5):1724–36. https://doi.org/10.1007/s12325-020-01285-2.
Allahyari A, Jernberg T, Hagstrom E, Leosdottir M, Lundman P, Ueda P. Application of the 2019 ESC/EAS dyslipidaemia guidelines to nationwide data of patients with a recent myocardial infarction: a simulation study. Eur Heart J. 2020;41(40):3900–9. https://doi.org/10.1093/eurheartj/ehaa034.
Beier L, Wolf M, Willfeld K, Weingaertner O. Patient and physician reported perception on hypercholesterolemia management in primary prevention in Germany: results from a nationwide online survey. Adv Ther. 2022. https://doi.org/10.1007/s12325-022-02266-3.
Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918–30. https://doi.org/10.1111/j.1475-6773.2005.00438.x.
Insignia Health: Patient Activation Measure® (PAM®). https://www.insigniahealth.com/products/pam-survey (2019). Accessed 19 February 2021.
Navar AM, Wang TY, Li S, et al. Lipid management in contemporary community practice: results from the provider assessment of lipid management (PALM) registry. Am Heart J. 2017;193:84–92. https://doi.org/10.1016/j.ahj.2017.08.005.
Cannon CP, de Lemos JA, Rosenson RS, et al. Use of lipid-lowering therapies over 2 years in GOULD, a registry of patients with atherosclerotic cardiovascular disease in the US. JAMA Cardiol. 2021. https://doi.org/10.1001/jamacardio.2021.1810.
Fox KM, Tai MH, Kostev K, Hatz M, Qian Y, Laufs U. Treatment patterns and low-density lipoprotein cholesterol (LDL-C) goal attainment among patients receiving high- or moderate-intensity statins. Clin Res Cardiol. 2018;107(5):380–8. https://doi.org/10.1007/s00392-017-1193-z.
Gitt AK, Lautsch D, Ferrieres J, et al. Contemporary data on low-density lipoprotein cholesterol target value attainment and distance to target in a cohort of 57,885 statin-treated patients by country and region across the world. Data Brief. 2016;9:616–20. https://doi.org/10.1016/j.dib.2016.09.037.
Gitt AK, Sonntag F, Jannowitz C, et al. Better lipid target achievement for secondary prevention through disease management programs for diabetes mellitus and coronary heart disease in clinical practice in Germany. Curr Med Res Opin. 2016;32(3):417–26. https://doi.org/10.1185/03007995.2015.1120715.
Mert GO, Basaran O, Mert KU, et al. The reasons of poor lipid target attainment for secondary prevention in real life practice: Results from EPHESUS. Int J Clin Pract. 2019;73(9):1–9. https://doi.org/10.1111/ijcp.13358.
Kaasenbrood L, Boekholdt SM, van der Graaf Y, et al. Distribution of estimated 10-year risk of recurrent vascular events and residual risk in a secondary prevention population. Circulation. 2016;134(19):1419–29. https://doi.org/10.1161/CIRCULATIONAHA.116.021314.
Barter PJ, Yamashita S, Laufs U, et al. Gaps in beliefs and practice in dyslipidaemia management in Japan, Germany, Colombia and the Philippines: insights from a web-based physician survey. Lipids Health Dis. 2020;19(1):131. https://doi.org/10.1186/s12944-020-01265-z.
AWMF. S3-Leitlinie zur kardiologischen Rehabilitation (LL-KardReha) im deutschsprachigen Raum Europas, Deutschland, Österreich, Schweiz (D-A-CH), Langversion - Teil 1, 2019 AWMF Registernummer: 133/001. 2020.
DEGAM: Schlaganfall. S3-Leitlinie. Available from: https://www.degam.de/files/Inhalte/Leitlinien-Inhalte/Dokumente/DEGAM-S3-Leitlinien/053-011_Schlaganfall/Archiv/053-011l_LL%20Schlaganfall_Inhaltsverzeichnis%20ge%C3%A4ndert.pdf. https://www.degam.de/files/Inhalte/Leitlinien-Inhalte/Dokumente/DEGAM-S3-Leitlinien/053-011_Schlaganfall/Archiv/053-011l_LL%20Schlaganfall_Inhaltsverzeichnis%20ge%C3%A4ndert.pdf Accessed 27.07.2022.
Laufs U, Karmann B, Pittrow D. Atorvastatin treatment and LDL cholesterol target attainment in patients at very high cardiovascular risk. Clin Res Cardiol. 2016;105(9):783–90. https://doi.org/10.1007/s00392-016-0991-z.
Heigl F, Pflederer T, Schettler V, et al. Lipidological competence centres and networks: future perspectives to improve healthcare of patients with disorders of lipid metabolism. Atheroscler Suppl. 2017;30:63–71. https://doi.org/10.1016/j.atherosclerosissup.2017.05.014.
Mulder J, Galema-Boers AMH, de Jong-Verweij LM, Hazelzet JA, Roeters van Lennep JE. The development and first results of a health-related outcomes set in familial hypercholesterolemia (FH) patients: Knowledge is health. Atherosclerosis. 2020;293:11–7. https://doi.org/10.1016/j.atherosclerosis.2019.11.030.
Dogan V, Basaran O, Ozlek B, et al. Evaluation of perceptions, knowledge and compliance with guidelines in real-life practice: a survey on the under-treatment of hypercholesterolemia. Turk Kardiyol Dern Ars. 2019;47(7):599–608. https://doi.org/10.5543/tkda.2019.39293.
Kinnear FJ, Wainwright E, Perry R, et al. Enablers and barriers to treatment adherence in heterozygous familial hypercholesterolaemia: a qualitative evidence synthesis. BMJ Open. 2019;9(7): e030290. https://doi.org/10.1136/bmjopen-2019-030290.
Hagger MS, Hardcastle SJ, Hu M, et al. Effects of medication, treatment, and behavioral beliefs on intentions to take medication in patients with familial hypercholesterolemia. Atherosclerosis. 2018;277:493–501. https://doi.org/10.1016/j.atherosclerosis.2018.06.010.
Giral P, Neumann A, Weill A, Coste J. Cardiovascular effect of discontinuing statins for primary prevention at the age of 75 years: a nationwide population-based cohort study in France. Eur Heart J. 2019;40(43):3516–25. https://doi.org/10.1093/eurheartj/ehz458.
Nielsen SF, Nordestgaard BG. Negative statin-related news stories decrease statin persistence and increase myocardial infarction and cardiovascular mortality: a nationwide prospective cohort study. Eur Heart J. 2016;37(11):908–16. https://doi.org/10.1093/eurheartj/ehv641.
Arnold SV, Cannon CP, de Lemos JA, et al. What do US physicians and patients think about lipid-lowering therapy and goals of treatment? Results from the GOULD registry. J Am Heart Assoc. 2021. https://doi.org/10.1161/JAHA.120.020893.
DGFF (Lipid-Liga). DGFF (Lipid-Liga) startet Kampagne „Auf Ziel“ mit Kick-Off „Jena auf Ziel“. 2021.
Schafer A, Sanchez Martinez C, Flierl U, Leitolf H, Tillmanns J, Bauersachs J. Standardized secondary prevention in patients with ST-elevation myocardial infarction. Eur J Prev Cardiol. 2022;28(18):e35–8. https://doi.org/10.1093/eurjpc/zwaa078.
Garcia RV, Garcia JEP, Navas WD, Salmeron DM, Mateos DB. Impact of a virtual lipid clinic on lipid-lowering therapy, LDL cholesterol levels, and outcomes in patients with acute coronary syndrome. J Clin Lipidol. 2022. https://doi.org/10.1016/j.jacl.2022.07.009.
Requena M, Montiel E, Baladas M, et al. Farmalarm. Stroke. 2019;50(7):1819–24. https://doi.org/10.1161/STROKEAHA.118.024355.
Woringer M, Dharmayat KI, Greenfield G, Bottle A, Ray KK. American Heart Association’s cholesterol careplan as a smartphone-delivered web app for patients prescribed cholesterol-lowering medication: protocol for an observational feasibility study. JMIR Res Protoc. 2019;8(1): e9017. https://doi.org/10.2196/resprot.9017.
Krzowski B, Peller M, Boszko M, et al. Mobile app and digital system for patients after myocardial infarction (afterAMI): study protocol for a randomized controlled trial. Trials. 2022;23(1):522. https://doi.org/10.1186/s13063-022-06463-x.
BAG Selbsthilfe e.V. Mit Gesundheitsselbsthilfe mehr für Prävention erreichen. Handreichung herausgegeben von der BAG SELBSTHILFE, verfasst von Petra Schmidt-Wiborg. Geringfügig bearbeitete Webfassung der Druckbroschüre. Düsseldorf. 2014.
Mullin GE. Patient education: the value of support groups. Nutr Clin Pract. 2010;25(5):555–7. https://doi.org/10.1177/0884533610379855.
Welsh J, Paige E, Banks E, Joshy G, Brieger D, Korda RJ. Psychological distress and medication use for secondary prevention of cardiovascular events: evidence from a large-scale population-based cohort study. J Psychosom Res. 2019;124: 109748. https://doi.org/10.1016/j.jpsychores.2019.109748.
Korhonen MJ, Pentti J, Hartikainen J, Kivimaki M, Vahtera J. Somatic symptoms of anxiety and nonadherence to statin therapy. Int J Cardiol. 2016;214:493–9. https://doi.org/10.1016/j.ijcard.2016.04.003.
Freisinger E, Fuerstenberg T, Malyar NM, et al. German nationwide data on current trends and management of acute myocardial infarction: discrepancies between trials and real-life. Eur Heart J. 2014;35(15):979–88. https://doi.org/10.1093/eurheartj/ehu043.
Gemeinsamer Bundesausschuss. Richtlinie des Gemeinsamen Bundesausschusses über die Gesundheitsuntersuchungen zur Früherkennung von Krankheiten (Gesundheitsuntersuchungs-Richtlinie). 2021.
Kordonouri O, Lange K, Boettcher I, et al. New approach for detection of LDL-hypercholesterolemia in the pediatric population: The Fr1dolin-Trial in Lower Saxony. Germany Atherosclerosis. 2019;280:85–91. https://doi.org/10.1016/j.atherosclerosis.2018.11.011.
Arafa AE, Anzengruber F, Mostafa AM, Navarini AA. Perspectives of online surveys in dermatology. J Eur Acad Dermatol Venereol. 2019;33(3):511–20. https://doi.org/10.1111/jdv.15283.
Taddicken M. Methodeneffekte von Web-Befragungen: Soziale Erwünschtheit vs. Soziale Entkontextualisierung. In: Weichbold M, Bacher J, Wolf C, editors. Umfrageforschung: Herausforderungen und Grenzen. Wiesbaden: VS Verlag für Sozialwissenschaften; 2009. p. 85–104.
Acknowledgements
We thank the participants of the survey.
Funding
Open Access funding enabled and organized by Projekt DEAL. The survey, medical writing support, and the journal’s Rapid Service and Open Access Fees were funded by Novartis Pharma GmbH.
Medical Writing and Other Assistance
Medical writing support was provided by Dr. Karin Eichele (mediwiz). Clariness GmbH provided services for programming, hosting, recruitment, and analysis of the survey. Both service providers were funded by Novartis Pharma GmbH.
Author contributions
LB and KS designed and implemented the survey. OW contributed to the development of the survey. KS, LB, and OW contributed to the analysis and interpretation of the results and to the writing of the manuscript. UM and MW aided in interpreting the results and commented on the manuscript.
Disclosures
OW received lecture fees and honoraria for adboards from Sanofi-Aventis, AMGEN, Berlin-Chemie, Amarin Therapeutics, Novartis, Akcea Therapeutics, Pfizer and Hexal GmbH. UM received speaker fees from the German Lipid Assosiation (DGFF), honoraria for advisory boards from Sanofi and non-financial support/cooperation from Novartis. The affiliation has changed during the completion of the manuscript. The new affiliation is Department of Cardiology, Charité Universitätsmedizin Berlin, Berlin, Germany. MW has received honoraria from Daiichi-Sankyo Deutschland GmbH. LB and KS are employees of Novartis Pharma GmbH.
Compliance with Ethics Guidelines
The survey has been conducted in accordance with all relevant guidelines and regulations applicable in Germany. There is no local requirement for an ethics committee approval or written informed consent for survey research. All patients participated voluntarily and informed consent to data collection, processing and analysis was obtained electronically from all subjects prior to the survey. Patient data were anonymized and aggregated for analysis. All physicians gave voluntary consent before participation.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Makhmudova, U., Wolf, M., Willfeld, K. et al. Different Perspectives of Patients and Physicians on LDL-C Target Achievement in the Treatment of Hypercholesterolemia: Results on Secondary Prevention from the German PROCYON Survey. Adv Ther 40, 460–473 (2023). https://doi.org/10.1007/s12325-022-02357-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02357-1