Abstract
Introduction
Effective hypercholesterolemia management is essential in primary prevention of cardiovascular events. The objective of PROCYON was to assess the perception on hypercholesterolemia management in primary prevention and to identify reasons for insufficient target attainment in clinical practice in Germany.
Methods
PROCYON was a two-part online survey including a patient questionnaire on treatment status and disease knowledge and a physician questionnaire on guideline awareness and patient management. A conjoint analysis on the relative importance of cardiovascular risk factors was incorporated.
Results
Of 3798 primary prevention patients included, 1632 (43.0%) received lipid-lowering medication. Of these, 790 (48.4%) reported improved low-density lipoprotein cholesterol (LDL-C) levels, 670 (41.1%) reported no improvement, and 172 (10.5%) had no information. Of the treated patients with (N′ = 790) and without (N′ = 670) improvement, 52.4% vs. 47.9% were on their initial drug and dose, 8.9% vs. 9.0% received multiple drug therapy, 34.7% vs. 38.8% reported a dose change, and 16.0% vs. 19.4% had discontinued at least one drug (multiple answers). In total, 109 physicians participated. In the conjoint analysis, LDL-C level was attributed the highest relative importance (32.0%), followed by diabetes (24.5%) and systolic blood pressure (15.8%). Lipid-lowering therapy is initiated at an LDL-C level > 150 mg/dl by 63 physicians (57.8%). One third (n = 35; 32.1%) stated that ≥ 60% of their primary prevention patients do not receive lipid-lowering medication.
Conclusion
PROCYON suggests a need for consequent LDL-C target-based treatment implementation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Effective management of hypercholesterolemia is a necessity in primary prevention of cardiovascular events, the leading cause of death in Europe. |
However, recommended target levels are not reached in a large proportion of patients, and therapeutic options are not fully exhausted. |
The objective of PROCYON was to assess the perception on hypercholesterolemia management in primary prevention and to identify reasons for insufficient target attainment in clinical practice in Germany. |
PROCYON suggests a need for improvement regarding guideline awareness and implementation from a physician’s perspective as well as improved risk awareness, disease knowledge, and adherence from a patient’s perspective. |
It can be assumed that adequate and effective interventions for optimization of hypercholesterolemia patient care are urgently needed. |
Introduction
Cardiovascular disease (CVD) is the leading cause of death in Europe [1] and accounted for 35% of all deaths in Germany in 2019 [2]. It is associated with great morbidity [3] and constitutes a significant health economic burden [1].
The 2019 guidelines of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) for the management of dyslipidaemias recommend the validated SCORE system (Systemic Coronary Risk Estimation, http://www.heartscore.org) to assess the 10-year risk of fatal cardiovascular (CV) events. It is based on age, gender, smoking, systolic blood pressure, and total cholesterol [4]. Elevated low-density lipoprotein cholesterol (LDL-C) levels are a major risk factor for coronary heart disease (CHD) [5] and major CV outcomes [6]. LDL-C lowering therefore is an essential part of the 2019 ESC/EAS guidelines for primary prevention of atherosclerotic CVD [4]. The target LDL-C level depends on the risk category: < 116 mg/dl for low-risk, < 100 mg/dl for moderate-risk, < 70 mg/dl and reduction of ≥ 50% for high-risk, and < 55 mg/dl and reduction of ≥ 50% for very-high-risk patients. Primary prevention patients with CHD or diabetes mellitus belong to the very-high-risk and high-risk categories with a 10-year risk of fatal CV events of > 10% and > 5% to ≤ 10%, respectively.
An LDL-C reduction of 1 mmol/l (40 mg/dl) reduced the risk for vascular mortality by 15% in a primary prevention population [7]. The 20-year follow-up of the WOSCOPS study showed the long-term benefits of statin treatment in primary prevention patients with LDL-C ≥ 160 mg/dl. The risk for CHD death was significantly reduced by 28% and the risk for CV death by 25% compared to patients who had initially received placebo. Furthermore, the long-term WOSCOP analysis indicated a higher CV risk as a result of LDL-C-associated cumulative atherosclerotic burden [8].
To achieve the LDL-C target levels, the guidelines recommend lifestyle and pharmacological intervention. The treatment scheme includes a first-line statin-based therapy and a combination of statins with ezetimibe if the target of LDL-C is not attained with the maximally tolerated dose of statins. [4]. Further treatment options for patients insufficiently treated on background statins with or without ezetimibe include the addition of bile acid sequestrants, bempedoic acid or PCSK9 inhibition via PCSK9 antibodies or RNA interference [4]. LDL apheresis can be considered especially in patients with familial hypercholesterolemia (FH) [4]. A simulation suggested that even at high/very high risk, 99.3% of patients could reach an LDL-C level < 70 mg/dl with statins, ezetimibe, and proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors [9] and 90% a target level of < 55 mg/dl [10].
However, real-world data from the DA VINCI study showed that among primary prevention patients only 63% with low risk, 60% with moderate risk, 25% with high risk, and 11% with very high risk reached the 2019 EAS/ECS guideline target levels [11]. Overall, 50–75% of the patients were on low- or moderate-intensity statin monotherapy [11], indicating that therapeutic options were not fully exhausted.
The objective of the present survey was to assess the awareness for current LDL-C lowering strategies in primary prevention and to identify reasons for the discrepancy between the potential of available therapies and target attainment in clinical practice in Germany.
Methods
Data Collection
PROCYON consisted of a patient and a physician survey which were active from September to November 2020 and were accessible through an online data collection tool hosted by Clinlife from Clariness.
Patients were required to meet the following criteria: (1) ≥ 18 years of age; (2) currently living in Germany; (3) diagnosis of hypercholesterolemia. Patients were identified by a service provider through newsletters and social media. Eligibility was screened via a questionnaire, and eligible patients were invited to participate. The web-based questionnaire of the patient survey (see supplementary table S1) included up to 35 questions on hypercholesterolemia-related medical history, comorbidities, medication adherence, side effects, disease knowledge, information generation, disease awareness, and self-activation. Patient self-activation was assessed by the Patient Activation Measure by Insignia Health (PAM-13), a 13-item measure developed to evaluate knowledge, skills and confidence essential to self-management of healthcare [12]. It defines four stages of activation with 1 being the lowest and 4 being the highest level of activation [13].
The following eligibility criteria were applied for the physician survey: (1) resident general practitioner, cardiologist, or internist; (2) treats at least 50 patients with hypercholesterolemia per quarter; (3) is in charge of treatment decisions. It was planned to include about 100 physicians in a 1:1:1 ratio (resident general practitioners, cardiologists, and internists). In total, 14,060 eligible physicians in Germany were contacted by a service provider and invited to participate. The first 100 physicians who signed the participation agreement were to be included. No individual patient data were collected in the physician survey. The online questionnaire included up to 33 questions (see supplementary table S2) on LDL-C relevance, guideline awareness, patient management, and treatment decisions. A conjoint analysis was used to assess the relative importance of risk factors for CVD. Among ten sets with three patient profiles each (see example in supplementary table S3), physicians were requested to determine the profile with the highest CV risk. Patient profiles within one set had identical risk scores but varying risk factors (age, gender, HDL-C, LDL-C, diabetes, smoker, systolic blood pressure) based on the PROCAM score (Prospective Cardiovascular Munster study). The PROCAM score estimates the risk for myocardial infarction using age, LDL-C level, HDL-C level, smoking status, systolic blood pressure, family history of premature myocardial infarction, diabetes mellitus, and triglyceride levels [14].
The authors developed the questionnaires under the guidance of a service provider (Clariness) experienced in the development and conduct of web-based surveys. The authors were responsible for the content development from a medical perspective. Clariness was responsible for the linguistic review (e.g., ensuring layperson understandable language of the patient questionnaire), for optimization of the questionnaire structure (e.g., screening questionnaire to identify the relevant patient population), and for plausibility checks (e.g., regarding correct jump conditions and question visibility to ensure automated navigation to relevant questions only). The conjoint analysis was developed under the guidance of a statistician.
Statistics
Patients and physicians who answered all questions were included in the analysis. The present patient survey analysis included primary prevention patients without myocardial infarction, stroke, peripheral arterial occlusive disease, or bypass surgery. Subgroup analyses of the physician survey by specialization are presented for questions on LDL-C relevance and treatment decisions. Descriptive statistics are shown for the survey data. Categorical variables were summarized using frequency counts and percentages. Continuous variables were summarized as means including standard deviation and medians. No formal statistical testing for group comparisons was performed. For the conjoint analysis, estimates were derived by a proportional hazard model based on a multinomial logit model with the physician's decision as dependent variable and the CVD risk attributes as independent variables. Continuous risk attributes were categorized. The relative importance of CVD risk attributes were calculated. The conjoint analysis was performed with SAS®, version 9.3 (SAS Institute Inc., Cary, NC, USA).
Administration
The survey has been conducted in accordance with all relevant guidelines and regulations applicable in Germany. Ethics approval was waived by the Ethics Committee of the Bavarian Medical Association (Ethik-Kommission der Bayerischen Landesärztekammer) in line with the national guidelines. There is no local requirement for written informed consent for survey research. All patients participated voluntarily, and informed consent to data collection, processing, and analysis was obtained electronically from all subjects prior to the survey. Patient data were anonymized and aggregated for analysis. All physicians gave voluntary consent before participation.
Results
Participants and Health Care Setting
The survey was completed by 5494 patients; 3798 constitute the primary prevention population with a median age of 59.0 years and 70.7% female participants. The most common comorbidity was hypertension (Table 1). Hypercholesterolemia had mostly been diagnosed during routine check-up with a median time since diagnosis of 10.0 years (Table 1). Most patients consult their general practitioner for their hypercholesterolemia with an LDL-C assessment frequency of once a year or less in 53.2% of the patients (Table 1).
In total, 109 physicians participated in the survey. Characteristics and details on medical experience are presented in Table 2. Most physicians (86.2%) stated that they are solely responsible for therapy decisions for hypercholesterolemia patients (Table 2). However, 85 physicians (58.6%) reported a wish for more interdisciplinary cooperation in the management of hypercholesterolemia patients, and 42 (29.0%) expressed a need for interdisciplinary networking and mutual exchange.
Physicians’ Disease Awareness and Guideline Compliance
Most physicians rated LDL-C as an important or very important risk factor and acknowledged its causal relationship with CV risk (Table 4). Agreement on the importance of cumulative LDL-C levels was lower (Table 4). Overall, 102 physicians (93.6%) reported performing routine checks for hypercholesterolemia, and 104 (95.4%) include LDL-C as a routine lipid test parameter.
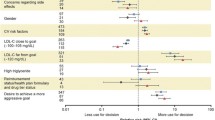
The conjoint analysis risk profiles were assessed by 103 physicians. The attribute with the highest relative importance was the LDL-C level, followed by diabetes, systolic blood pressure, and smoking status (Table 3).
Lipid-lowering therapy is initiated at an LDL-C level of < 125 mg/dl by 20.2%, at 130–150 mg/dl by 22.0%, and at > 150 mg/dl by 57.8% of physicians (Table 4). In total, 60 physicians (55.0%) reported that ≥ 30% of their primary prevention patients are without drug therapy and 35 (32.1%) have ≥ 50% of their primary prevention patients untreated. Results by medical specialization are presented in supplementary table S4.
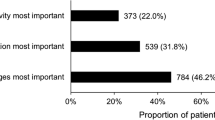
The most common reasons for treatment escalation were target failure within 6 months (n = 67; 61%), a CV event (n = 67; 61.5%), or patient request (n = 30; 27.5%). Treatment is escalated if LDL-C target level is not reached after 8 weeks by 16.7% of the general practitioners, 9.1% of the internists, and 47.8% of the cardiologists (Supplementary Table S4). In case of insufficient treatment or statin intolerance, the most common options are addition of ezetimibe or a switch to another statin (Figs. 1, 2A). Insufficient target attainment is considered to be mostly due to a lack of lifestyle adaption and adherence, followed by side effects and a lack of efficacy (Fig. 2B). Among the different medical specializations, general practitioners consider a lack of lifestyle adaption as most important for not attaining target LDL-C level, while internists and cardiologists consider side effects as well as lack of adherence most important (data not shown). In general, 86 physicians (78.9%) are satisfied or very satisfied with the current treatment options.
Patients’ Treatment Status
Less than half of the primary prevention patients stated that they receive lipid-lowering medication, and half of the treated patients (n = 790, 48.4%) stated that their LDL-C level has improved since diagnosis; 670 patients (41.1%) reported no improvement (Table 5). Of the patients on drug therapy with (N′ = 790) and without (N′ = 670) LDL-C improvement, 52.4% (n = 414) vs. 47.9% (n = 321) were on their initial drug at the same dose, 8.9% (n = 70) vs. 9.0% (n = 60) were on multiple drug therapy, 34.7% (n = 274) vs. 38.8% (n = 260) reported a dose change, and 16.0% (n = 126) vs. 19.4% (n = 130) had discontinued at least one drug (multiple answers allowed). Frequency of LDL-C assessments in treated patients without improvement (N′ = 670) is once a year or less in 259 patients (38.7%) and twice per year or more often in 411 patients (61.3%).
Compliance, Patient Information, and Activation
Physician Perspective
All physicians consider patient information as important or very important for adherence. Overall, 100 physicians (91.7%) stated that they inform patients about LDL-C targets, and 77 (70.6%) identified a need for more patient information material. Regarding their patients’ level of knowledge, 81 physicians (81.0%) answered that their patients know about LDL-C importance, 50 physicians (45.9%) stated that their patients do not take the risk of hypercholesterolemia serious, and 70 physicians (55.0%) assumed a lack of knowledge on the disease.
Patient Perspective
The treating physician was mentioned as the most common source of information by 2453 patients (64.6%). The information received by their physician was rated as good or very good by 1351 patients (35.6%) and as sufficient by 1496 (39.4%). Patient groups are used for information by 63 patients (1.7%); 946 patients (24.9%) say they have good or very good knowledge about LDL-C. The importance of LDL-C reduction for lowering their CV risk is acknowledged by 3234 patients (85.2%). One third of the patients (n = 1242; 32.7%) know their current LDL-C level, and 1006 patients (26.5%) know their target LDL-C, of whom 754 (75.0%) consider it important to achieve the target.
Two third of the patients receiving lipid-lowering therapy consider their LDL-C medication as important as other medications (Table 6). Most patients rated themselves as treatment compliant and reported taking their medication as regularly or nearly as regularly as prescribed (Table 6). The most common reason for treatment discontinuation was side effects (Table 6). Less than one third of the patients (n = 1073; 28.3%) are satisfied with their current treatment. Most are worried about their elevated LDL-C levels (n = 1446; 38.1%), wish to receive another therapy (n = 492; 13.0%), or are bothered by the need for frequent drug administration (n = 431; 11.4%).
The most frequently reported adaptions since diagnosis were dietary changes (2051 patients; 54.0%), followed by an increase in physical activity (1500 patients; 39.5%) and lipid-lowering drug intake (1300 patients; 34.2%). In total, 3402 patients answered the patient activation measure (PAM) questionnaire. The results regarding the achieved PAM levels were as follows: PAM level 4: 442 patients (13.0%); PAM level 3: 2114 patients (62.1%); PAM level 2: 754 patients (22.2%); PAM level 1: 92 patients (2.7%).
Discussion
The PROCYON survey suggests that a high proportion of untreated patients and a lack of patient perceived improvement in LDL-C levels in 41% of patients on drug therapy. This is in line with US registry data, in which 63.9% of the primary prevention patients were untreated or treated on a lower intensity than recommended [15].
In the conjoint analysis, physicians’ assessment of risk factor relevance was in accordance with the ESC/EAS guidelines with elevated LDL-C levels as one of the main factors [4]. Of note, the relative importance of systolic blood pressure in the conjoint analysis was only 15.8%. Although the focus of this analysis was the perception of LDL-C, this needs to be highlighted, given the high importance of a multifactorial approach in primary prevention and the established association of hypertension with CV risk [4].
Regarding LDL-C level reduction, the survey results imply inadequate guideline implementation into clinical practice. Most physicians reported initiating pharmacotherapy for primary prevention only at LDL-C levels > 150 mg/dl. This complies with the 2017 DEGAM (Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin) guideline on counseling on CV prevention in family medicine, which recommends considering statin therapy at LDL-C levels < 195 md/dl only in case of high or very high CV risk [16]. In contrast, the ESC/EAS 2019 guidelines intend a target of < 116 mg/dl even for low-risk patients. Barter et al. reported a target level of 129 mg/dl in clinical practice in Germany and suggested that uncertainties related to statin safety and the safety of very low LDL-C levels might add to the reluctance to adopt the low target recommendations [17]. However, this is only one possible explanation. It has been previously reported that clinical guidelines are often not applied, irrespective of the medical specialty. A scoping review has identified three categories of barriers for guideline implementation. These included personal factors (e.g., physicians’ knowledge and attitudes), guideline-related factors (e.g., layout, access, complexity), and external factors (e.g., lack of resources, lack of collaboration). In accordance, the authors of this review have identified suitable strategies to overcome these issues, including increased educational (e.g., CME, group training), communication and technical efforts (e.g., provision of user-friendly versions of guidelines on mobile devices), establishment of quality circles, improvement of collaboration, and standardization of organizational processes [18].
Furthermore, PROCYON indicated that the frequency of LDL-C assessments might be too low. More than one third of the patients with above-recommended LDL-C levels despite drug therapy undergo LDL-C assessments only once per year or less. An assessment once per year is standard in patients on LDL-C lowering therapy [4], but a higher frequency should be considered until the target level is reached.
In addition, only half of the physicians were fully aware of cumulative LDL-C as a risk correlate of CVD. While pack-years are established to quantify the cumulative impact of smoking, cumulative LDL-C exposure and the associated necessity of early screening and treatment are not fully acknowledged in primary care. Screening for hypercholesterolemia has just recently become reimbursable in Germany once between 18 and 34 years of age. From the age of 35 years onwards routine checks can be performed every 3 years [19]. However, earlier screening is supported by data on the high prevalence of elevated LDL-C levels in preschool children [20].
PROCYON implies that treatment was often not escalated despite inadequate LDL-C reduction. Cardiologists tended to escalate earlier than general practitioners and internists. The reluctance might be attributable to the fact that the 2017 DEGAM guideline recommends a fixed-dose statin treatment instead of a treat-to-target approach and opts against a combination therapy [16].
General practitioners thought that mainly a lack of lifestyle adaption impaired target attainment. However, even dramatic changes can only reduce LDL-C levels by 10–15% [21]. Pharmacological intervention is essential for target attainment.
In contrast to general practitioners, internists and cardiologists considered adherence and tolerability as the most important reasons for missing the target. The high adherence rates reported by patients might reflect a participation bias, with high self-activation in respondents. However, frequent patient-initiated treatment discontinuations rather suggest that patients overestimated their adherence, which is common due to social desirability and memory biases [22]. Improving adherence could constitute a major factor for treatment success with a potential in CHD risk reduction of 52% [23].
Previous studies revealed that negative media information about statins was a major driver of treatment discontinuation [24, 25]. A trusting patient-physician relationship that addresses the patients’ risk perception, existing side effects as well as information gaps allows for correction of misinformation [26]. While the importance of patient information was generally accepted in PROCYON, the lack of knowledge on LDL-C targets and current levels indicate a need for well-composed educational material to support patient-physician communication. The involvement of patient organizations could further add to education and activation. Patients with FH and other severe hereditary lipid disorders in Germany can be referred to the “Cholesterin und Co e.V.” (CholCo.org). For primary prevention patients without hereditary disorders, a patient organization has not been established yet.
The physician survey allows supposing a wish for interdisciplinary networking. Patient management could benefit from professional networks through facilitated transitory processes (i.e., between medical specialists, general practitioners, and lipid ambulances) and diagnosis of rare lipid disorders through lipid competence centers. Furthermore, networks could promote inter- and intradisciplinary exchange and continued training (e.g., qualification as certified “lipidologist”) [27].
The present survey has some limitations. First, except for PAM-13, no validated questionnaire was available to support the study objective. Therefore, the results need to be interpreted carefully and need further confirmation. Nevertheless, the present results provide valuable insight into potential issues in management of patients with hypercholesterolemia in clinical practice. Second, LDL-C levels collected in the patient survey were implausible and could not be interpreted, possibly because of confusion of the units. Patients could choose to enter their LDL-C levels in mg/dl or mmol/l, as both units are used in Germany, depending on regional preference. The documented range in mg/dl was 1.3–1485; the documented range in mmol/l was 0–180,119. Therefore, assessment of LDL-C changes was based on the patients’ perceived LDL-C development only. Third, web-based medical surveys are prone to a participation bias with higher level of education and better health state among the respondents compared to non-respondents [28]. Survey results might further be biased by social desirability [29], and participants with higher self-activation might be overrepresented as only responders who answered all questions were included. Survey participation of patients was not encouraged by incentives. Physicians received a small expense allowance for participation; however, only a minor response bias is expected.
Conclusion
PROCYON implies that adequate and effective interventions for optimization of hypercholesterolemia patient care are urgently needed. PROCYON identified potentials for improvement with respect to guideline awareness and implementation from a physician’s perspective as well as improved risk awareness, disease knowledge, and adherence from a patient’s perspective.
Change history
23 September 2022
A Correction to this paper has been published: https://doi.org/10.1007/s12325-022-02316-w
References
Wilkins E, Wilson L, Wickramasinghe K, et al. European cardiovascular disease statistics 2017. 2017. Available from: https://ehnheart.org/component/attachments/attachments.html?task=attachment&id=3115. Accessed 19 July 2022.
Statistisches Bundesamt (Destatis). Ergebnis 23211-0002. Gestorbene: Deutschland, Jahre, Todesursachen, Geschlecht. Stand: 13.04.2021. 2020.
Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. 2016;37(42):3232–45. https://doi.org/10.1093/eurheartj/ehw334.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88. https://doi.org/10.1093/eurheartj/ehz455.
Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38(32):2459–72. https://doi.org/10.1093/eurheartj/ehx144.
Ference BA, Graham I, Tokgozoglu L, Catapano AL. Impact of lipids on cardiovascular health: JACC health promotion series. J Am Coll Cardiol. 2018;72(10):1141–56. https://doi.org/10.1016/j.jacc.2018.06.046.
Cholesterol Treatment Trialists C, Mihaylova B, Emberson J, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380(9841):581–90. https://doi.org/10.1016/S0140-6736(12)60367-5.
Vallejo-Vaz AJ, Robertson M, Catapano AL, et al. Low-density lipoprotein cholesterol lowering for the primary prevention of cardiovascular disease among men with primary elevations of low-density lipoprotein cholesterol levels of 190 mg/dL or above: analyses from the WOSCOPS (West of Scotland Coronary Prevention Study) 5-year randomized trial and 20-year observational follow-up. Circulation. 2017;136(20):1878–91. https://doi.org/10.1161/CIRCULATIONAHA.117.027966.
Cannon CP, Khan I, Klimchak AC, Reynolds MR, Sanchez RJ, Sasiela WJ. Simulation of lipid-lowering therapy intensification in a population with atherosclerotic cardiovascular disease. JAMA Cardiol. 2017;2(9):959–66. https://doi.org/10.1001/jamacardio.2017.2289.
Allahyari A, Jernberg T, Hagstrom E, Leosdottir M, Lundman P, Ueda P. Application of the 2019 ESC/EAS dyslipidaemia guidelines to nationwide data of patients with a recent myocardial infarction: a simulation study. Eur Heart J. 2020;41(40):3900–9. https://doi.org/10.1093/eurheartj/ehaa034.
Ray KK, Molemans B, Schoonen WM, et al. EU-wide cross-sectional observational study of lipid-modifying therapy use in secondary and primary care: the DA VINCI study. Eur J Prev Cardiol. 2020. https://doi.org/10.1093/eurjpc/zwaa047.
Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918–30. https://doi.org/10.1111/j.1475-6773.2005.00438.x.
Insignia Health: Patient Activation Measure® (PAM®). https://www.insigniahealth.com/products/pam-survey (2019). Accessed Feb 19, 2021.
Assmann G, Cullen P, Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the prospective cardiovascular Munster (PROCAM) study. Circulation. 2002;105(3):310–5. https://doi.org/10.1161/hc0302.102575.
Navar AM, Wang TY, Li S, et al. Lipid management in contemporary community practice: results from the Provider Assessment of Lipid Management (PALM) Registry. Am Heart J. 2017;193:84–92. https://doi.org/10.1016/j.ahj.2017.08.005.
Egidi G, Ludt S, Angelow A, et al. Neue DEGAM-S3 Leitlinie „Hausärztliche Beratung zur kardiovaskulären Prävention“. Z Allg Med. 2017;93(7/8):312–8. https://doi.org/10.3238/zfa.2017.0312-0318.
Barter PJ, Yamashita S, Laufs U, et al. Gaps in beliefs and practice in dyslipidaemia management in Japan, Germany, Colombia and the Philippines: insights from a web-based physician survey. Lipids Health Dis. 2020;19(1):131. https://doi.org/10.1186/s12944-020-01265-z.
Fischer F, Lange K, Klose K, Greiner W, Kraemer A. Barriers and strategies in guideline implementation—a scoping review. Healthcare (Basel). 2016. https://doi.org/10.3390/healthcare4030036.
Gemeinsamer Bundesausschuss. Richtlinie des Gemeinsamen Bundesausschusses über die Gesundheitsuntersuchungen zur Früherkennung von Krankheiten (Gesundheitsuntersuchungs-Richtlinie). 2021.
Kordonouri O, Lange K, Boettcher I, et al. New approach for detection of LDL-hypercholesterolemia in the pediatric population: the Fr1dolin-Trial in Lower Saxony, Germany. Atherosclerosis. 2019;280:85–91. https://doi.org/10.1016/j.atherosclerosis.2018.11.011.
Kelly RB. Diet and exercise in the management of hyperlipidemia. Am Fam Physician. 2010;81(9):1097–102.
Stirratt MJ, Dunbar-Jacob J, Crane HM, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med. 2015;5(4):470–82. https://doi.org/10.1007/s13142-015-0315-2.
Brandts J, Ray KK. Low density lipoprotein cholesterol-lowering strategies and population health: time to move to a cumulative exposure model. Circulation. 2020;141(11):873–6. https://doi.org/10.1161/CIRCULATIONAHA.119.043406.
Dogan V, Basaran O, Ozlek B, et al. Evaluation of perceptions, knowledge and compliance with guidelines in real-life practice: a survey on the under-treatment of hypercholesterolemia. Turk Kardiyol Dern Ars. 2019;47(7):599–608. https://doi.org/10.5543/tkda.2019.39293.
Nielsen SF, Nordestgaard BG. Negative statin-related news stories decrease statin persistence and increase myocardial infarction and cardiovascular mortality: a nationwide prospective cohort study. Eur Heart J. 2016;37(11):908–16. https://doi.org/10.1093/eurheartj/ehv641.
Navar AM, Stone NJ, Martin SS. What to say and how to say it: effective communication for cardiovascular disease prevention. Curr Opin Cardiol. 2016;31(5):537–44. https://doi.org/10.1097/HCO.0000000000000322.
Heigl F, Pflederer T, Schettler V, et al. Lipidological competence centres and networks: future perspectives to improve healthcare of patients with disorders of lipid metabolism. Atheroscler Suppl. 2017;30:63–71. https://doi.org/10.1016/j.atherosclerosissup.2017.05.014.
Arafa AE, Anzengruber F, Mostafa AM, Navarini AA. Perspectives of online surveys in dermatology. J Eur Acad Dermatol Venereol. 2019;33(3):511–20. https://doi.org/10.1111/jdv.15283.
Taddicken M. Methodeneffekte von Web-Befragungen: Soziale Erwünschtheit vs. Soziale Entkontextualisierung. In: Weichbold M, Bacher J, Wolf C, editors. Umfrageforschung: Herausforderungen und Grenzen. Wiesbaden: VS Verlag für Sozialwissenschaften; 2009. pp 85–104.
Acknowledgements
Funding
The survey, medical writing support, as well as the journal’s Rapid Service and Open Access Fees were funded by Novartis Pharma GmbH. Open Access funding enabled and organized by Projekt DEAL.
Medical Writing and Other Assistance
Medical writing support was provided by Dr. Karin Eichele (mediwiz). Clariness GmbH provided services for programming, hosting, recruitment and analysis of the survey.
Author Contributions
Lea Beier and Kathy Willfeld designed and implemented the survey. Oliver Weingaertner contributed to the development of the survey. Kathy Willfeld, Lea Beier and Oliver Weingaertner contributed to the analysis and interpretation of the results and to the writing of the manuscript. Michaela Wolf aided in interpreting the results and commented on the manuscript.
Disclosures
Oliver Weingaertner received lecture fees and honoraria for adboards from Sanofi-Aventis, AMGEN, Berlin-Chemie, Amarin Therapeutics, Novartis, Akcea Therapeutics and Hexal GmbH. Michaela Wolf has received honoraria from Daiichi-Sankyo Deutschland GmbH. Lea Beier and Kathy Willfeld are employees of Novartis Pharma GmbH.
Compliance with Ethics Guidelines
The survey has been conducted in accordance with all relevant guidelines and regulations applicable in Germany. Ethics approval was waived by the Ethics Committee of the Bavarian Medical Association (Ethik-Kommission der Bayerischen Landesärztekammer) in line with the national guidelines. There is no local requirement for written informed consent for survey research. All patients participated voluntarily and informed consent to data collection, processing and analysis was obtained electronically from all subjects prior to the survey. Patient data were anonymized and aggregated for analysis. All physicians gave voluntary consent before participation.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Beier, L., Wolf, M., Willfeld, K. et al. Patient and Physician Reported Perception on Hypercholesterolemia Management in Primary Prevention in Germany: Results from a Nationwide Online Survey. Adv Ther 39, 4315–4329 (2022). https://doi.org/10.1007/s12325-022-02266-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02266-3