Abstract
Introduction
Opioid-induced constipation (OIC) is the most common side effect of opioid treatment. Treatment for OIC typically involves a laxative. However, some patients have an inadequate response to these (laxative inadequate responders, or LIR). This has led to the development of treatments such as naloxegol. This analysis estimates the impact of naloxegol on the health state utility of LIR patients, examines if this utility impact is driven by the change in OIC status, and estimates the utility impact of relief of OIC.
Methods
The analysis was conducted using data from two 12-week randomized controlled trials, KODIAC 4 (ClinicalTrials.gov identifier, NCT01309841) and KODIAC 5 (ClinicalTrials.gov identifier, NCT01323790), plus KODIAC 7 (ClinicalTrials.gov identifier, NCT01395524), a 12-week extension to KODIAC 4. All were designed to assess the efficacy and safety of oral naloxegol (12.5 and 25 mg) compared to placebo. Health state utility data were collected through the EuroQol—five dimensions questionnaire (EQ-5D-3L). Descriptive analysis was undertaken to estimate how EQ-5D utility scores and EQ-5D domain responses varied with treatment, OIC status, and over time. A repeated measure mixed-effects model was used to predict the change from baseline in health state utility score over time.
Results
Compared with placebo, LIR patients treated with naloxegol 25 mg reported a 0.08 improvement in the EQ-5D overall score after 12 weeks of treatment. The analyses also suggest that change in OIC status is a key driver of the impact of OIC treatment on health state utility. When other factors are controlled, relieving OIC is associated with a 0.05 improvement in health state utility, although treatment with naloxegol is associated with an improvement in health state utility over and above the improvement in OIC status.
Conclusion
These analyses suggest that treatment with naloxegol improves patients’ health state utility; driven predominantly by the relief of patients’ constipation.
Funding
AstraZeneca.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic pain is a symptom that accompanies many conditions including joint pain, fibromyalgia, and osteoarthritis [1, 2]. In industrialized countries, opioids are frequently used alternatives for the treatment of moderate-to-severe chronic nonmalignant pain, second only to nonsteroidal anti-inflammatory agents in terms of prescription frequency [3–6]. A total of 365 million opioid prescriptions were made globally in 2005 [1]. One in five people in Europe suffer from moderate-to-severe chronic non-cancer pain; 25–30% of those are prescribed opioids [3, 4, 7, 8]. One in four people in the United States (US) suffer from moderate-to-severe chronic non-cancer pain, and 15–20% of those groups are prescribed opioids [7, 9, 10]. Chronic non-cancer pain affects a quarter of the Canadian population, a third of which are prescribed strong opioids [11, 12].
Opioid-induced constipation (OIC) is the most common side effect of opioid treatment in patients with cancer and non-cancer pain, and all patients using opioids are at risk of developing OIC [1]. OIC typically begins within the first few days of starting an opioid treatment, and although some patients may experience some relief with dose reduction of the opioid, it typically persists for over the treatment duration [1, 13].
The effects of OIC can cause psychological distress, bodily suffering, and social isolation [1, 14, 15]. The symptoms of OIC include rectal and/or lower abdominal pain, abdominal distension, straining during evacuation, bloating, and flatulence [16–18]. Stool impaction is a potential outcome of OIC that occurs when retained stools form large, firm lumps that are impossible to defecate, which in turn may lead to bowel obstruction, stercoral ulcers, and urinary retention [19]. This stage of OIC necessitates manual disimpaction or even surgery. Psychological distress is caused by OIC as a result of the general distress about the constipation itself as well as depressive symptoms and anticipatory anxiety, which may increase over time [16, 20]. The symptoms of OIC have a considerable negative impact on activities of daily living [1, 14]. It has been reported that constipation is even more common source of distress than the pain originally being treated [21]. In some patients, OIC becomes so severe that patients may taper or even discontinue opioid use in an attempt to relieve their discomfort, as they prefer tolerating their pain rather than suffering from continued bowel dysfunction [1, 14, 15, 18, 22–24]. Moreover, in contrast to other opioid-induced side effects (e.g., nausea), patients rarely develop a tolerance to OIC [1, 14, 17].
Utilities are one particular measure of HRQoL used in economic evaluations, representing preferences for states of health, measured on a scale of 0 [death] to 1 [perfect health] [25]. A number of studies have demonstrated low health state utility values for patients with OIC. For instance, a cross-sectional survey of OIC patients in the US, Canada, Germany, and the United Kingdom (UK) estimated that the mean European Quality of Life (EuroQol)—Five Dimensions questionnaire (EQ-5D) index score was 0.49 and the mean EQ-5D Visual Analogue Scale score was 50.6, measured on a scale of 0 [death] to 100 [perfect health] [2]. These EQ-5D values suggest that patients with OIC have lower utility than patients with conditions, such as myocardial infarction, minor stroke, chronic obstructive pulmonary disease, some high-incidence cancers, and even some end-stage cancers, such as prostate and colorectal cancer (mean EQ-5D range of 0.55–0.76) [26–31].
The low health state utility values in patients with OIC are most likely a result of both the chronic pain and the side effects of opioid treatment including OIC. For instance, patients with chronic lower back pain report EQ-5D scores ranging between 0.53 and 0.64 [32, 33], and those with chronic cancer pain who required constipation therapy had a mean EQ-5D score of 0.49 [34]. To quantify the impact of OIC on a patients’ health state utility, a comparison between patients with and without OIC, but who previously had OIC, is required. There is, however, limited published evidence of the impact of OIC on health state utility. A paper by Penning van Beest et al. estimated the EQ-5D in patients with a severe non-curable disease treated with opioids, and found that utility was much higher in those who were constipated than not constipated (0.65 vs. 0.31, respectively) [26]. However, this difference seems unreasonably large, and the study suffers from a number of limitations. It focused on constipation, in general, in opioid users, rather than OIC specifically, and the definition of constipation adopted by the study relied on self-reports of constipation and laxative use. Most importantly, the study was cross-sectional and not designed to assess the causal impact of OIC on health state utility and did not control for other factors that may influence this.
The importance of research to generate quantitative estimates of the impact of OIC on health state utility is underscored by the limited efficacy of standard of care for OIC. Laxatives are typically used as an initial treatment option for OIC in clinical practice; however, studies report between 81% and 94% of patients who take laxatives to treat their OIC exhibited an inadequate response [2, 14, 35]. It is evident therefore that OIC remains a significant issue for pain management with the large proportion of patients who are laxative inadequate responders (LIR), showing a clear unmet need [2].
Patients are likely to have an inadequate response to laxatives because laxatives do not target the mu-opioid receptors to which opioids bind in the gastrointestinal (GI) tract. Opioids disrupt normal motility, sphincter function, and intestinal fluid secretion into the lumen, potentially leading to OIC [36]. This has led to the use of pharmacological agents that work to specifically block the effect of opioids on the GI tract and prevent OIC from occurring, including nonselective opioid antagonists and peripherally acting mu-opioid receptor antagonists (PAMORAs) [19].
Naloxegol is a once daily treatment and is the first oral PAMORA that has been approved in the European Union for OIC. Naloxegol was studied in two, three arm, randomized, controlled, double-blind pivotal trials, KODIAC 4 and KODIAC 5, comparing naloxegol 12.5 mg, naloxegol 25 mg, and placebo in chronic non-cancer pain patients. The primary outcome in both studies was the response to study drug, defined as 3 or more spontaneous bowel movements (SBMs) per week and a change from baseline of 1 or more SBM per week for at least 9 out of the 12 study weeks and 3 out of the preceding 4 study weeks. Naloxegol 25 mg, the dose for which naloxegol received approval, was associated with significantly higher response rates in LIR patients compared with placebo over 12 weeks trials (KODIAC 4, 48.7% vs. 28.8%; KODIAC 5, 46.8% vs. 31.4%) [37].
The objective of the present analysis was to generate rigorous estimates of the impact of once daily 25 mg dose of naloxegol on the health state utility of LIR patients, the population for whom naloxegol has received market authorization in the EU; to examine if this utility impact of naloxegol is driven primarily by the change in OIC status, or whether the treatment has an impact beyond its impact on OIC status; and lastly to examine the utility impact of relief of OIC.
Methods
Data Sources
The KODIAC trial program was designed to assess the efficacy and safety of naloxegol 12.5 and 25 mg in adult patients with OIC with the EQ-5D being collected in three studies in the program. The primary objective of both KODIAC 4 and 5 (ClinicalTrials.gov identifier, NCT01309841 and NCT01323790, respectively) was to evaluate the response of patients over a 12-week treatment period (see “Introduction”), and the EQ-5D as an exploratory analysis. For these analyses, the data from the naloxegol 25 mg and placebo arms in the two trials were pooled, as the studies were of replicate design; both enrolled outpatients with non-cancer pain, aged 18–84, and were designed to ensure that ≥50% of the patients randomized were LIR at baseline. Across the two trials all arms had similar demographic and clinical characteristics enabling pooling, and this consistency was present in both the overall and LIR populations [38]. Moreover, the EQ-5D scores across trials were similar. In KODIAC 4, the placebo arm had a mean (with standard deviation) of 0.55 (0.31) and for naloxegol 25 mg of 0.60 (0.26). In KODIAC 5, the placebo arm had a baseline EQ-5D of 0.57 (0.29) and in the naloxegol 25 mg arm of 0.54 (0.31). Across trials the baseline EQ-5D was 0.56 (0.29) for the placebo arm and 0.57 (0.29) for the naloxegol 25 mg arm. KODIAC 4 and 5 were supplemented with data from KODIAC 7 (ClinicalTrials.gov identifier, NCT01395524), a 12-week extension study of patients completing the KODIAC 4 study, designed to assess the maintained efficacy and safety of naloxegol 12.5 mg and 25 mg in comparison with placebo in patients with OIC and non-cancer related pain.
Measures
The analysis was based upon the population of patients who were LIR, a subset of intent-to-treat population [37], in correspondence with the EU label. These patients were those who had reported taking at least one laxative class for a minimum of four days within the two-week period prior to the screening visit concurrent with at least moderately severe symptoms of OIC (i.e., incomplete bowel movements, hard stools, straining, or false alarms).
In this analysis, OIC was defined as having fewer than 3 SBMs per week in any of the 2 weeks in the preceding 4-week rolling period. Non-OIC was defined as having 3 or more SBMs per week in at least 3 weeks out of the preceding 4-week rolling period. Patients with insufficient data where an OIC or non-OIC response could not be determined were excluded from the analyses. This definition varied from the primary end point used in the trials (see introduction), which required responders to not only achieve a certain number of SBMs per week, but also a minimum change in the number of SBMs per week. This simplified the analysis, allowing estimates of utility based on constipation status, rather than change in that status. Data to measure OIC status were available at each of Weeks 4–12 in the KODIAC 4 and 5 studies. Data on OIC status was not collected in KODIAC 7.
Health state utility was measured using the EQ-5D. First, the EQ-5D, a generic QoL instrument, was collected in all three trials. The EQ-5D is a self-administered, generic assessment tool developed by the EuroQol Group, a network of international research teams, and consists of questions on five dimensions of health (i.e., mobility, self-care, pain/discomfort, usual activities, and anxiety/depression). The questionnaire was completed by patients at baseline, Week 4, and Week 12 in the KODIAC 4 and 5 studies and Weeks 16 and 24 in the KODIAC 7 study. Patient responses to the EQ-5D questionnaire were converted into utility values on a 0–1 scale, where 0 represents death and 1 represents perfect health, using a tariff estimated from surveys of the UK general population [39] and in accordance with the recommendation of the National Institute for Health and Care Excellence.
Analyses
The objective of the analysis was to estimate the impact of naloxegol 25 mg (from here on referred to as ‘naloxegol’) on the health state utility of LIR patients. This encompasses estimating how EQ-5D utility index scores (from here on referred to as ‘utility score’) and EQ-5D domain responses varied with treatment (naloxegol vs placebo), OIC status, and over time. To compare variables, t tests were run on continuous variables and Fisher’s exact tests were run on categorical variables, with no multiple testing corrections being undertaken. For such analyses, we assessed the absolute score differences between the arms at week 4 and 12 so to see the added benefits over time of both naloxegol and in having relief from OIC. A mixed model repeated measures model with random intercepts was used to predict the change from baseline in utility score over time. Specifically, changes in utility score were estimates at Weeks 4 and 12. Predictors tested in the model were: time (weeks), age, gender, race, body mass index, duration of opioid use, treatment, baseline utility, and OIC status. To account for the possibility that the impact of treatment on utility may vary over time, a treatment-time interaction variable was also included in the model. The final model included variables relevant to the objectives of the paper; OIC status, treatment, and time-treatment interaction, plus other variables whose association with the change in utility score was statistically significant (p < 0.1) in univariate regression models. The model was performed using SAS version 9.4, SAS Institute Inc, Cary, NC.
The studies were conducted in accordance with the Declaration of Helsinki of 1964, as revised in 2013, and the International Conference on Harmonisation. An ethics committee or institutional review board at each study site approved the final study protocol and informed consent form. All patients provided written informed consent at screening, before any study procedures were performed.
Results
The baseline characteristics of LIR patients in KODIAC 4 and KODIAC 5 are reported in Table 1.
Utility among LIR patients in the placebo arm was demonstrably lower than among patients in naloxegol arm at Week 12 and when pooling across Weeks 4 and 12 (Table 2). Relative to placebo, the improvement in health state utility associated with treatment with naloxegol was 0.08 (p < 0.05) at Week 12.
Table 3 shows how patient responses to the five separate dimensions of the EQ-5D varied with treatment in the LIR population. Higher proportions of patients with “Moderate” or “Severe” problems were consistently observed with placebo across the five dimensions with most notable improvements relative to placebo in the mobility and anxiety/depression domains.
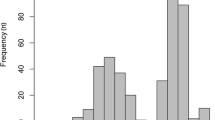
Figure 1 shows the impact of treatment on the domains of the EQ-5D over the 12 weeks of the KODIAC 4 and 5 trials combined. A general trend was demonstrated in both treatment and placebo arms, with increases in the proportion of patients reporting “no problems”, and a drop in the proportion of patients reporting “some problems”. The increase in the proportion of patients who had “no problems” was consistently greater for naloxegol patients than placebo patients.
Table 4 evaluates if a patient’s OIC status results in a difference in health state utility. It shows that there is a substantial utility gain associated with relieving OIC of 0.07 (p = 0.0025).
The effect of treatment and OIC status on utility score, which was identified in Tables 2 and 4, respectively, are likely to be related. Table 5, below, presents the mean utility score of patients when segregated by treatment, time and OIC status.
Table 5 supports the observation that by Week 12, health state utility improves as a result of treatment with naloxegol. There is a health state utility difference of 0.07 (0.67 vs. 0.60) between naloxegol and placebo patients who are non-OIC at week 12, and a health state utility difference of 0.06 (0.60 vs. 0.54) between naloxegol and placebo patients who are OIC at Week 12. However, this difference in utility between treatment groups is no longer statistically significant when the change in OIC status is considered. To further examine this time and treatment effect, a regression analyses was undertaken.
Table 6 shows how responses to the five separate dimensions of the EQ-5D varied with treatment and OIC status in the LIR population. In Table 3, which did not distinguish between OIC status following treatment, there was a statistically significant impact of treatment on anxiety/depression, and a borderline statistically significant impact on mobility. These treatment impacts are no longer observed in patients who are still constipated after treatment. However, the treatment impact is still observed in patients who are non-OIC after treatment, suggesting that naloxegol may reduce anxiety/depression and improve mobility, over and above any impact on these dimensions reflected in the measure of OIC status.
The analysis reported in Table 7 broadly supports the observations above that the key driver of health state utility is OIC status along with baseline utility, but a time and treatment effect does exist. When controlling for other relevant factors, it is estimated that relieving OIC is associated with a 0.05 health state utility improvement. The analysis also identifies a significant treatment-time interaction effect (p = 0.024), suggesting that naloxegol at Week 12 generates a utility improvement over and above its impact on OIC status.
Impact of treatment on health state utility was also captured in KODIAC 7. Table 8 suggests that the impact of treatment observed at 12 weeks is maintained to Week 16, though this impact is minimally observed at Week 24. It is important to note that these observations should be treated cautiously; they are based on the subset of participants who completed the KODIAC 4 trial and were rolled into the KODIAC 7 extension study. Consequently, the sample is small and subject to selection bias.
Discussion
These analyses demonstrate the utility benefits of treating OIC in LIR patients with naloxegol 25 mg. On a scale of 0–1, where 0 represents death and 1 perfect health, patients treated with this, saw a 0.08 improvement in health state utility at 12 weeks after treatment, relative to placebo. Recent studies concluded that opioid antagonists improve OIC-related symptoms. For instance, there is evidence that naloxone in combination with oxycodone generates improvements in the Bowel Function Index [41]. The current study adds to this literature by observing health state utility improvements in the EQ-5D. As well as being a validated instrument, and providing data compatible with the needs of those undertaking cost-utility analysis, the EQ-5D is a generic instrument which has the advantage of generating utility estimates comparable with those generated for many other indications.
Although we have demonstrated an impact on utility levels, an appropriate, indication specific, estimate of a minimum important difference (MID) is not in the published literature. Analyses in patients with OIC need to be undertaken to define this. Although Coretti et al. [42] concludes that there is a great amount of heterogeneity in estimates of MIDs due to variations in study populations and methodologies and in the absence of such an estimate, it is useful to observe that a 0.08 improvement represents a 14% improvement on the baseline utility of patients in trial, and is equivalent to the utility loss from the long-term consequences of a moderate stroke, profound hearing loss with ringing, or a dislocated shoulder [43].
When a baseline utility score and OIC status were controlled for, the effect of treatment alone on health state utility disappears though treatment-time effect remains, suggesting that naloxegol has a lasting impact on utility over and above its impact on OIC status. This may point to the limitation of the binary measure of OIC improvement adopted in the study. The definition of OIC reflected recognized best practice, drawing on the Rome III diagnostic criteria for functional constipation [44]. However, this measure would potentially miss some of the impact of treatment on health state utility if there is an improvement in OIC symptoms and the number of SBMs beyond that captured by the measure of OIC status. This caveat is supported by the trial data. In both KODIAC 4 and KODIAC 5, patients who were not constipated experienced more SBMs when on naloxegol than on placebo. Further work should be undertaken to explore the impact of changes in numbers of SBMs on utility score.
The analyses also suggest that change in OIC status is the most impactful driver of the improvement of OIC treatment on utility. When other factors are controlled, relieving OIC is associated with a 0.05 improvement in health state utility. This estimate of the impact of OIC on utility is lower than those previously reported in the literature [26], reflecting the limitations in the methods adopted in previous studies and the lack of face validity of their findings. Nevertheless, even at this lower level, the impact of OIC on utility points to an important burden of illness and the need for effective treatments for patients with OIC.
The analysis of changes in the dimensions of the EQ-5D instrument suggest that the utility gain associated with naloxegol is primarily a result of improved mobility and reduced anxiety/depression, due to relief of OIC symptoms. No statistically significant change in the pain dimension of the EQ-5D instrument was observed, which was not unexpected given naloxegol being a treatment for OIC. However, a disadvantage of the EQ-5D is that its health state descriptive system is not always designed to be sensitive to certain medical conditions [45]. The EQ-5D describes only 5 dimensions, and has been shown to be less sensitive to conditions, such as vision problems [46–50], diabetes, and arthritis. This could potentially lead to underestimation of the impact of indications on utility. For instance, the EQ-5D may miss the impact of OIC on social functioning. This concern has often led to the use of disease-specific instruments and mapping exercises to create utility scores based upon these disease specific instruments. One disease specific instrument developed for constipation is the Patient Assessment of Constipation Quality of Life questionnaire. This provides a brief but comprehensive assessment of the burden of constipation on patients’ everyday functioning and well-being [51]. It is the most frequently used instrument to assess health related quality of life in patients with chronic constipation and is validated in this disease, but has not been specifically validated in patients with OIC [22].
Finally, it should be reiterated that the EQ-5D was not the primary endpoint in the KODIAC trials. Consequently, the trials were not prospectively powered for these endpoints, and we need to be cautious when using secondary and exploratory endpoints to assess the impact of treatment. However, this caution should be offset against the positive result obtained on the primary endpoint, response, and the fact that response is a key driver of the improvement in health state utility observed with naloxegol.
Conclusion
Treatment of chronic pain with opioids is associated with many challenges, with OIC being an important factor due to its impact upon daily activities and health state utility. These analyses suggest that treatment with naloxegol improves patients’ health state utility, and this is primarily driven by a change in the status of OIC.
References
Panchal SJ, Muller-Schwefe P, Wurzelmann JI. Opioid-induced bowel dysfunction: prevalence, pathophysiology and burden. Int J Clin Pract. 2007;61:1181–7.
Coyne KS, LoCasale RJ, Datto CJ, Sexton CC, Yeomans K, Tack J. Opioid-induced constipation in patients with chronic noncancer pain in the USA, Canada, Germany, and the UK: descriptive analysis of baseline patient-reported outcomes and retrospective chart review. Clinicoecon Outcomes Res. 2014;6:269–81.
Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287–333.
Reid KJ, Harker J, Bala MM, Truyers C, Kellen E, Bekkering GE, et al. Epidemiology of chronic non-cancer pain in Europe: narrative review of prevalence, pain treatments and pain impact. Curr Med Res Opin. 2011;27:449–62.
Sng BL, Schug SA. The role of opioids in managing chronic non-cancer pain. Ann Acad Med Singapore. 2009;38:960–6.
Ueberall MA, Mueller-Schwefe GH. Development of opioid-induced constipation: post hoc analysis of data from a 12-week prospective, open-label, blinded-endpoint streamlined study in low-back pain patients treated with prolonged-release WHO step III opioids. J Pain Res. 2015;8:459–75.
Annunziata K FD, Janning S, Williams R, Bell T. Constipation is a predominant side effect of opioid treatment for persistent pain. In: American Pain Society, 25th Annual Meeting, San Antonio, Texas; 2006.
Langley PC. The prevalence, correlates and treatment of pain in the European Union. Curr Med Res Opin. 2011;27:463–80.
Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010;11:1230–9.
Toblin RL, Mack KA, Perveen G, Paulozzi LJ. A population-based survey of chronic pain and its treatment with prescription drugs. Pain. 2011;152:1249–55.
Boulanger A, Clark AJ, Squire P, Cui E, Horbay GL. Chronic pain in Canada: have we improved our management of chronic noncancer pain? Pain Res Manag. 2007;12:39–47.
Moulin DE, Clark AJ, Speechley M, Morley-Forster PK. Chronic pain in Canada–prevalence, treatment, impact and the role of opioid analgesia. Pain Res Manag. 2002;7:179–84.
Mancini I, Bruera E. Constipation in advanced cancer patients. Support Care Cancer. 1998;6:356–64.
Bell TJ, Panchal SJ, Miaskowski C, Bolge SC, Milanova T, Williamson R. The prevalence, severity, and impact of opioid-induced bowel dysfunction: results of a US and European Patient Survey (PROBE 1). Pain Med. 2009;10:35–42.
Hjalte F, Berggren AC, Bergendahl H, Hjortsberg C. The direct and indirect costs of opioid-induced constipation. J Pain Symptom Manage. 2010;40:696–703.
Dhingra L, Shuk E, Grossman B, Strada A, Wald E, Portenoy A, et al. A qualitative study to explore psychological distress and illness burden associated with opioid-induced constipation in cancer patients with advanced disease. Palliat Med. 2013;27:447–56.
Goodheart CR, Leavitt SB. Managing Opioid-Induced Constipation in Ambulatory-Care Patients. http://paincommunity.org/blog/wp-content/uploads/Managing_Opioid-Induced_Constipation.pdf. Pain Treatment Topics 2006; August: 1–9. Accessed Dec 2014.
Epstein RS, Cimen A, Benenson H, Aubert RE, Khalid M, Sostek MB, et al. Patient preferences for change in symptoms associated with opioid-induced constipation. Adv Ther. 2014;31:1263–71.
Müller-Lissner S. Opioid-induced constipation—mechanisms, relevance and management. http://www.touchophthalmology.com/sites/www.touchoncology.com/files/migrated/articles_pdfs/lissner.pdf. Eur Gastroenterol Hepatol Rev 2010; 6: 54–7. Accessed Jan 2015.
Annemans L. Pharmacoeconomic impact of adverse events of long-term opioid treatment for the management of persistent pain. Clin Drug Investig. 2011;31:73–86.
McMillan SC. Presence and severity of constipation in hospice patients with advanced cancer. Am J Hosp Palliat Care. 2002;19:426–30.
Camilleri M. Opioid-induced constipation: challenges and therapeutic opportunities. Am J Gastroenterol. 2011;106:835–42 (quiz 43).
Gupta S, Patel H, Sarangpur S, Mody R. Impact of opioid-induced constipation on opioid therapy management among chronic opioid users based on a patient survey (abstract). American Pain Society. 2014;15(4):S6.
Holzer P. New approaches to the treatment of opioid-induced constipation. Eur Rev Med Pharmacol Sci. 2008;12(Suppl 1):119–27.
National Institute for Health and Care Excellence (NICE). Process and methods guides: Guide to the methods of technology appraisal 2013. London: NICE; 2013. http://www.nice.org.uk/article/pmg9/resources/non-guidance-guide-to-the-methods-of-technology-appraisal-2013-pdf. Accessed May 2014.
Penning-van Beest FJ, van den Haak P, Klok RM, Prevoo YF, van der Peet DL, Herings RM. Quality of life in relation to constipation among opioid users. J Med Econ. 2010;13:129–35.
Sullivan PW, Slejko JF, Sculpher MJ, Ghushchyan V. Catalogue of EQ-5D scores for the United Kingdom. Med Decis Making. 2011;31:800–4.
Bennett L, Zhao Z, Barber B, Zhou X, Peeters M, Zhang J, et al. Health-related quality of life in patients with metastatic colorectal cancer treated with panitumumab in first- or second-line treatment. Br J Cancer. 2011;105:1495–502.
Farkkila N, Torvinen S, Roine RP, Sintonen H, Hanninen J, Taari K, et al. Health-related quality of life among breast, prostate, and colorectal cancer patients with end-stage disease. Qual Life Res. 2014;23:1387–94.
Hirsh V, Cadranel J, Cong XJ, Fairclough D, Finnern HW, Lorence RM, et al. Symptom and quality of life benefit of afatinib in advanced non-small-cell lung cancer patients previously treated with erlotinib or gefitinib: results of a randomized phase IIb/III trial (LUX-Lung 1). J Thorac Oncol. 2013;8:229–37.
Luengo-Fernandez R, Gray AM, Bull L, Welch S, Cuthbertson F, Rothwell PM, et al. Quality of life after TIA and stroke: ten-year results of the Oxford vascular study. Neurology. 2013;81:1588–95.
Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ. 2004;13:873–84.
Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al. Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain. Health Technol Assess. 2005;9:iii–iv, ix–x, 1–109.
Ahmedzai SH, Leppert W, Janecki M, Pakosz A, Lomax M, Duerr H, et al. Long-term safety and efficacy of oxycodone/naloxone prolonged-release tablets in patients with moderate-to-severe chronic cancer pain. Support Care Cancer. 2015;23:823–30.
Guijarro P, Alonso-Babarro A, Viqueira A, Fernandez G. Economic burden of opioid induced constipation in Spain. Value Health. 2010;13:A369.
Brock C, Olesen SS, Olesen AE, Frokjaer JB, Andresen T, Drewes AM. Opioid-induced bowel dysfunction: pathophysiology and management. Drugs. 2012;72:1847–65.
Chey WD, Webster L, Sostek M, Lappalainen J, Barker PN, Tack J. Naloxegol for opioid-induced constipation in patients with noncancer pain. N Engl J Med. 2014;370:2387–96.
Tack J, Lappalainen J, Diva U, Tummala R, Sostek M. Efficacy and safety of naloxegol in patients with opioid-induced constipation and laxative-inadequate response. United Eur Gastroenterol J. 2015;3:471–80.
EuroQoL Group. EQ-5D FAQs. Rotterdam: EuroQol Research Foundation; 2014. http://www.euroqol.org/faqs.html. Accessed May 2014.
World Health Organization (WHO). WHO’s cancer pain ladder for adults. 2016. http://www.who.int/cancer/palliative/painladder/en/. Accessed Oct 2014.
Morlion B, Clemens KE, Dunlop W. Quality of life and healthcare resource in patients receiving opioids for chronic pain: a review of the place of oxycodone/naloxone. Clin Drug Investig. 2015;35:1–11.
Coretti S, Ruggeri M, McNamee P. The minimum clinically important difference for EQ-5D index: a critical review. Expert Rev Pharmacoecon Outcomes Res. 2014;14:221–33.
World Health Organization (WHO). WHO methods and data sources for global burden of disease estimates 2000-2011. 2013. http://www.who.int/healthinfo/statistics/GlobalDALYmethods_2000_2011.pdf. Accessed Feb 2016.
Rome Foundation. Rome III Diagnostic Criteria for Functional Gastrointestinal Disorders. Raleigh, NC: Rome Foundation; 2006. http://www.romecriteria.org/assets/pdf/19_RomeIII_apA_885-898.pdf. Accessed Sept 2014.
Brazier J, Deverill M. A checklist for judging preference-based measures of health related quality of life: learning from psychometrics. Health Econ. 1999;8:41–51.
Aspinall PA, Johnson ZK, Azuara-Blanco A, Montarzino A, Brice R, Vickers A. Evaluation of quality of life and priorities of patients with glaucoma. Invest Ophthalmol Vis Sci. 2008;49:1907–15.
Bozzani FM, Alavi Y, Jofre-Bonet M, Kuper H. A comparison of the sensitivity of EQ-5D, SF-6D and TTO utility values to changes in vision and perceived visual function in patients with primary open-angle glaucoma. BMC Ophthalmol. 2012;12:43.
Chisholm D, Healey A, Knapp M. QALYs and mental health care. Soc Psychiatry Psychiatr Epidemiol. 1997;32:68–75.
Donaldson C, Atkinson A, Bond J, Wright K. Should QALYs be programme-specific? J Health Econ. 1988;7:239–57.
Kobelt G, Jonsson B, Bergstrom A, Chen E, Linden C, Alm A. Cost-effectiveness analysis in glaucoma: what drives utility? Results from a pilot study in Sweden. Acta Ophthalmol Scand. 2006;84:363–71.
Marquis P, De La Loge C, Dubois D, McDermott A, Chassany O. Development and validation of the patient assessment of constipation quality of life questionnaire. Scand J Gastroenterol. 2005;40:540–51.
Acknowledgments
The study, this resulting manuscript, article processing charges and the open access fee were funded by AstraZeneca. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Disclosures
Richard Lawson, Fred King, and Ali Cimen are employees of AstraZeneca, which funded this project. Kevin Marsh and Arman Altincatal are employees of Evidera, which provides consulting and other research services to pharmaceutical, device, government, and nongovernment organizations. In their salaried positions, Dr. Marsh and Mr. Altincatal work with a variety of companies and organizations and are precluded from receiving payment or honoraria directly from these organizations for services rendered. Evidera received funding from AstraZeneca for this project.
Compliance with Ethics Guidelines
The studies were conducted in accordance with the Declaration of Helsinki of 1964, as revised in 2013, and the International Conference on Harmonisation. An ethics committee or institutional review board at each study site approved the final study protocol and informed consent form. All patients provided written informed consent at screening, before any study procedures were performed.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/0BD4F0605E3DE0E1.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Lawson, R., King, F., Marsh, K. et al. Impact of Treatment with Naloxegol for Opioid-Induced Constipation on Patients’ Health State Utility. Adv Ther 33, 1331–1346 (2016). https://doi.org/10.1007/s12325-016-0365-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-016-0365-y