Abstract
Purpose
The management of overriding distal forearm fractures is still controversial. This study aimed to evaluate the efficacy of immediate closed reduction and cast immobilization (CRCI) at the emergency department (ED) using equimolar nitrous oxide (eN2O2) as conscious sedation, and without the use fluoroscopic assistance.
Methods
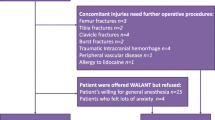
Sixty patients with overriding distal forearm fracture were included in the study. All procedures were performed in the ED without fluoroscopic assistance. Antero-posterior and lateral wrist radiographs were taken after CRCI. Follow-up radiographs were taken 7 and 15 days post-reduction, and at cast removal to evaluate callus formation. Depending on the radiological outcome, two groups of patients could be identified: Group 1 (satisfactory reduction and maintenance of alignment) and Group 2 (poor reduction or secondary displacement requiring further manipulation and surgical fixation). Group 2 was additionally divided into Group 2A (poor reduction) and Group 2B (secondary displacement). Pain was assessed using Numeric Pain Intensity (NPI) score, while functional outcome was measured according to Quick DASH questionnaire.
Results
Mean age at the time of injury was 9.2 ± 2.4 years (range, 5–14). Twenty-three (38%) patients were aged between 4 and 9 years old, 20 (33%) patients between 9 and 11, 11 (18%) patients between 11 and 13, and 6 (10%) patients between 13 and 14. The mean follow-up time was 45.6 ± 12 months (range, 24–63). Satisfactory reduction with maintenance of alignment was achieved in 30 (50%) patients (Group 1). Re-reduction was performed in the remaining 30 (50%) patients (Group 2) due to poor reduction (Group 2A) or secondary displacement (Group 2B). No complications related to the administration of eN2O were recorded.
No statistically significant difference could be identified between the three groups for any clinical variable (Quick DASH and NPI).
Conclusion
Overriding distal forearm fractures may be safely treated with CRCI at ED using eN2O2 as conscious sedation. However, fluoroscopic assistance during CRCI might significantly improve the quality of reduction thus avoiding further treatment as the lack of relaxed muscle can restrain reduction.




Similar content being viewed by others
References
Chung KC, Spilson SV, Arbor A (2001) The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am 26(5):908–915
Hove LM, Brudvik C (2008) Displaced paediatric fractures of the distal radius. Arch Orthop Trauma Surg 128:55–60
Brudvik C, Hove LM (2003) Childhood fractures in bergen, norway : identifying high-risk groups and activities. J Pediatr Orthop 23:629–634
Alemdaroglu KB, Iltar S, Cimen O, Uysal M, Alagöz E, Atlihan D (2008) Risk factors in redisplacement of distal radial fractures in children. J Bone Joint Surg Am 90:1224–1230
Zamzam MM, Khoshhal KID (2005) Displaced fracture of the distal radius in children: factors responsible for redisplacement after closed reduction. J Bone Joint Surg Br 87(6):841–843
Sengab A, Krijnen P, Birgitta I (2020) Risk factors for fracture redisplacement after reduction and cast immobilization of displaced distal radius fractures in children : a meta - analysis. Eur J Trauma Emerg Surg 46(4):789–800
Mcquinn AG, Phys B, Jaarsma RL (2012) Risk Factors for redisplacement of pediatric distal forearm and distal radius fractures. J Pediatr Orthop 32:687–692
Fenton P, Nightingale P, Hodson J, Luscombe J (2012) Factors in redisplacement of paediatric distal radius fractures. J Pediatr Orthop B 21:127–130
Ozcan M, Memisoglu S, Copuroglu C, Saridogan K (2010) Percutaneous Kirschner Wire fixation in distal radius metaphyseal fractures in children : does it change the overall outcome ? Hippokratia 14(4):265–270
Yang BW, Waters P (2019) Conscious sedation and reduction of fractures in the paediatric population: an orthopaedic perspective. J Child Orthop 13(3):330–333
Betham C, Harvey M, Cave G (2011) Manipulation of simple paediatric forearm fractures: a time-based comparison of emergency department sedation with theatre-based anaesthesia. N Z Med J 124(1344):46–53
Kurien T, Price KR, Pearson RG, Dieppe C, Hunter JB (2016) Manipulation and reduction of paediatric fractures of the distal radius and forearm using intranasal diamorphine and 50% oxygen and nitrous oxide in the emergency department: a 2. 5-year study. Bone Jt J 98-B:131–213
Pierantoni S, Alberghina F, Cravino M, Paonessa M, Canavese F, Andreacchio A (2020) Functional and radiographic outcomes of Gartland type II supracondylar humerus fractures managed by closed reduction under nitrous oxide as conscious sedation. J Pediatr Orthop B 29(2):117–125
Paneru SR, Rijal R, Shrestha BP, Nepal P, Khanal GP, Karn NK et al (2010) Randomized controlled trial comparing above- and below-elbow plaster casts for distal forearm fractures in children. J Child Orthop 4(3):233–237
Seiler M, Heinz P, Callegari A, Dreher T, Staubli G, Aufdenblatten C (2020) Short and long-arm fiberglass cast immobilization for displaced distal forearm fractures in children: a randomized controlled trial. Int Orthop 45:759–768
Webb GR, Galpin RD, Armstrong DG (2006) Comparison of short and long arm plaster casts for displaced fractures in the distal third of the forearm in children. J Bone Jt Surg Am 88(1):9–17
Patel SP, Anthony SG, Zurakowski D, Didolkar MM, Kim PS, Wu JS et al (2014) Radiographic scoring system to evaluate union of distal radius fractures. J Hand Surg Am 39(8):1471–1479
Fisher JS, Kazam JJ, Fufa D, Bartolotta RJ (2019) Radiologic evaluation of fracture healing. Skeletal Radiol 48(3):349–361
De Courtivron B (1995) Spontaneous correction of the distal forearm fractures in children. In: European Pediatric Orthopaedic Society Annual Meeting. Brussels
Chess DG, Hyndman JC, Leahey JL, Brown DC, Sinclair AM (1994) Short arm plaster cast for distal pediatric forearm fractures. J Pediatr Orthop 14:211–213
Pavone V, Vescio A, Lucenti L, Chisari E, Canavese F, Testa G (2020) Analysis of loss of reduction as risk factor for additional secondary displacement in children with displaced distal radius fractures treated conservatively. Orthop Traumatol Surg Res 106(1):193–198
Iltar S, Alemdaroğlu KB, Say F, Aydoğan NH (2013) The value of the three-point index in predicting redisplacement of diaphyseal fractures of the forearm in children. Bone Jt J 95-B(4):563–567
Beaton DE, Wright J, Katz JN (2005) Development of the QuickDASH : comparison of three item-reduction approaches. J Bone Joint Surg Am 87(5):1038–1046
Canavese F, Athlani L, Marengo L, Rousset M, Rouel-Rabiau N, Samba A et al (2014) Evaluation of upper-extremity function following surgical treatment of displaced proximal humerus fractures in children. J Pediatr Orthop B 23(2):144–149
Marengo L, Andreacchio A, Alberghina F, Dimeglio A, Canavese F (2018) Functional outcome of displaced intercondylar fractures of the humerus in children and adolescents. J Pediatr Orthop B 27(2):121–127
Tsze DS, Hirschfeld G, von Baeyer CL, Suarez LE, Dayan PS (2019) Changes in pain score associated with clinically meaningful outcomes in children with acute pain. Acad Emerg Med 26(9):1002–1013
Adrian M, Wachtlin D, Kronfeld K, Sommerfeldt D, Wessel LM (2015) A comparison of intervention and conservative treatment for angulated fractures of the distal forearm in children (AFIC): study protocol for a randomized controlled trial. Trials 30(16):437
Crawford SN, Lee LSK, Izuka BH (2012) Closed treatment of overriding distal radial fractures without reduction in children. J Bone Jt Surg Am 94:246–252
Voto SJ, Weiner DS, Leighley B (1990) Redisplacement after closed reduction of forearm fractures in children. J Pediatr Orthop 10:79–84
Kong L, Lu J, Zhou Y, Tian D, Zhang B (2020) Incidence and risk factors for redisplacement after closed reduction and instant rigid cast immobilization for paediatric distal radius fractures : a case control study. J Orthop Surg Res 15(1):140
Miller BS, Taylor B, Widmann RF, Bae DS, Snyder BD, Waters PM (2005) Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: a prospective, randomized study. J Pediatr Orthop 25(4):490–494
Bae DS (2008) Pediatric distal radius and forearm fractures. J Hand Surg Am 33(10):1911–1923
Gayet S, Bernit E, Sati H, Veit V, Mazodier K, Schleinitz N et al (2009) Pain prevention with fixed 50 % nitrous oxide—oxygen mixture during bone-marrow biopsy. Rev Med Interne 30(3):208–214
Annequin D, Carbajal R, Chauvin P, Gall O, Tourniaire B, Murat I (2000) Fixed 50% nitrous oxide oxygen mixture for painful procedures: a french survey. Pediatrics 105(4):E47
Coté CJ, Karl HW, Notterman DA, Weinberg JA, McCloskey C (2000) Adverse sedation events in pediatrics: analysis of medications used for sedation. Pediatrics 106(4):633–644
Bhatia M, Housden PH (2006) Re-displacement of paediatric forearm fractures: role of plaster moulding and padding [Injury 37:259-68]. Erratum Inj 37:801
Malviya A, Tsintzas D, Mahawar K, Bache CE, Glithero PR (2007) Gap index: a good predictor of failure of plaster cast in distal third radius fractures. J Pediatr Orthop B 16:48–52
van Egmond PW, Schipper IB, van Luijt PA (2012) Displaced distal forearm fractures in children with an indication for reduction under general anesthesia should be percutaneously fixated. Eur J Orthop Surg Traumatol 22:201–207
Sankar WN, Beck NA, Brewer JM, Baldwin KD, Pretell JA (2011) Isolated distal radial metaphyseal fractures with an intact ulna : risk factors for loss of reduction. J Child Orthop 5:459–464
Wendling Keim DS, Wieser B, Dietz HG (2015) Closed reduction and immobilization of displaced distal radial fractures. Method of choice for the treatment of children. Eur J Trauma Emerg Surg 41(4):421–428
Hang JR, Hutchinson AF, Hau RC (2011) Risk Factors associated with loss of position after closed reduction of distal radial fractures in children. J Pediatr Orthop 31:501–506
Zimmermann R, Gschwentner M, Kralinger F, Arora R, Gabl M, Pechlaner S (2004) Long-term results following pediatric distal forearm fractures. Arch Orthop Trauma Surg 124:179–186
Colaris JW, Hein J, Biter LU, de Vries MR, van de Ven CP, Bloem RM et al (2013) Re-displacement of stable distal both-bone forearm fractures in children : a randomised controlled multicentre trial. Injury 44(4):498–503
Mclauchlan GJ, Cowan B, Annan IH, Robb JE (2002) Management of completely displaced metaphyseal fractures of the distal radius in children. J Bone Jt Surg Br 84-B:413–417
Ramoutar DN, Shivji FS, Rodrigues JN, Hunter JB (2015) The outcomes of displaced paediatric distal radius fractures treated with percutaneous Kirschner wire fixation : a review of 248 cases. Eur J Orthop Surg Traumatol 25(3):471–476
Zeng ZK, Liang WD, Sun YQ, Jiang PP, Li D, Shen Z et al (2018) Is percutaneous pinning needed for the treatment of displaced distal radius metaphyseal fractures in children? Medicine (Baltimore) 97(36):e12142
Acknowledgements
The authors have no relevant financial or non-financial interests to disclose.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rava, A., Alberghina, F., Cravino, M. et al. Closed reduction and cast immobilization of overriding distal forearm fractures under nitrous oxide as conscious sedation without the use of imaging control. Musculoskelet Surg 107, 413–421 (2023). https://doi.org/10.1007/s12306-023-00785-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-023-00785-y