Abstract
Background
Subtalar joint dislocation (1% of all dislocations) is the permanent loss of articular relationships in the talonavicular and talocalcaneal joints, without other involvement of the foot. Dislocation can occur medially (85%), laterally (15%), posteriorly (2.5%) and anteriorly (1%). Reduction can be performed by closed or open technique; lateral dislocations often require open reduction because of inclusion of soft tissues or bone fragments. Lateral dislocations are frequently complicated by bone exposure, risk of infection and associated soft tissues injuries.
Aim of the study
The aim of this study is to explain main characteristics and to clarify the most important pitfalls of subtalar dislocations.
Materials and methods
We examined 47 articles published in the last thirty years (389 cases). For each dislocation we reviewed its main characteristics: direction, bone exposure, need for open reduction and for surgical stabilisation, associated injuries and method used for diagnosis.
Results
Medial dislocations (68.1%) has greater incidence compared to lateral ones (27.7%). Bone exposure (44.5%), associated lesions (44.5%) and need for surgical reduction (48.2%) are much more represented in lateral dislocation than in the others.
Conclusions
Subtalar dislocations, especially the lateral one, represent a challenge for surgeons. Lateral subtalar dislocation occurs following high-energy trauma often involving associated injuries. Closed reduction could be unsuccessful and patients must undergo surgical reduction. After reduction CT scan is recommended. Our narrative review confirms these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subtalar (or peritalar) dislocation means the simultaneous and permanent loss of articular relationships in the talonavicular and talocalcaneal joints, without fracture of the talar neck and without tibiotarsal or calcaneocuboid joint involvement.
Described for the first time in 1811 by Judcy and DauFaurest [1], it is a very rare dislocation (1–2% of all dislocations) [2].
Broca described this type of dislocation for the first time and classified it by subdividing it into medial, lateral or posterior forms, based on the position of the foot in relation to the talus [3]. Malaigne and Burger supplemented this classification through the addition of anterior dislocation [4].
Subtalar dislocation occurs most frequently in a medial direction (85%) and less frequently laterally (15%–20%), while posterior (2.5%) and anterior (1%) dislocations are exceptions [5]. In lateral dislocations, the head of the talus is dislocated medially, while the remainder of the foot remains lateral. In medial dislocations, the inverse occurs [6].
Subtalar dislocation primarily affects active young male adults (M:F—6:1), and is frequently associated with fractures of the hindfoot, midfoot and ankle.
Medial dislocation, which is also described as “acquired clubfoot”, is caused by distortive trauma due to forced inversion with the foot in plantar flexed position. The consequent stress to the lateral perimalleolar ligament apparatus causes the rupture of the talocalcaneal and talonavicular ligaments, so that the talus remains correctly positioned in the tibiotarsal joint while the subtalar dislocation occurs.
The term “acquired flatfoot” refers to lateral subtalar dislocation, the second most frequent pattern [7]. In this case, the forces act by stressing the medial side of the foot, causing a forced eversion injury. High-energy trauma is required to cause a lateral subtalar dislocation, which explains the high frequency of associated problems such as fractures or soft tissue injuries (described in the literature with an incidence of up to 40%) [8] and bone exposure. Lateral dislocations are known to be the most difficult to reduce because of the frequent inclusion of soft tissues (such as the posterior tibial tendon, the flexor digitorum longus or the joint capsule) or bone fragments and require surgical reduction in almost all cases. The outcome of lateral dislocations is often less than satisfactory, due to the high frequency of bone exposure and associated injuries [9].
We propose a narrative review of the literature on subtalar dislocations of the last thirty years; the aim of this study is to explain main characteristics and to clarify the most important pitfalls of subtalar dislocations, especially in the more difficult treatment of the lateral ones.
Material and methods
The search for articles was carried out in Pubmed, Scopus, DARE, Proquest and Google Scholar databases using a combination of the following key words: “Subtalar dislocation” and “Lateral”, “Subtalar dislocation” and “Medial”, “Subtalar dislocations” and “Open reduction”, “Subtalar dislocation” and “Lesion”, “Talus” and “Lateral process”.
We searched for articles of the types “case report”, “case series” and “review”.
We considered articles published in the last 30 years, drafted in English.
We considered articles to be suitable where they provided complete information about the following characteristics: direction of the dislocation, bone exposure, any need for open reduction, use of K-wires or external fixators for stabilisation, use of CT check-ups post-reduction, and presence of associated injuries.
Articles which not met these inclusion criteria was eliminated from the review.
Each article meeting the inclusion criteria was analysed critically by two independent reviewers to its methodological quality. In the case of a discrepancy between the assessments made by the reviewers, a third reviewer was involved to resolve the dispute.
Results
Our review considered 47 articles (23 case reports, 17 case series, four reviews and three case reports and reviews), published between 1991 and 2018, covering a total of 389 patients (Table 1).
The results described below are shown in Table 2 (Table 2).
The direction of dislocation was specified in 387 patients out of 389: this showed 265 medial dislocations (68.1%), 108 lateral (27.7%), 9 posterior (2.3%) and 5 anterior (1.3%). In the article by Bibbo et al. [14], the direction of dislocation was not stated for two of the 25 patients because no data could be found in the clinical records.
Dislocations complicated by bone exposure occurred in 107 of 389 patients (27.5%), compared to 282 closed dislocations (72.5%).
The ratio of closed and exposed dislocations is indicatively maintained among medial dislocations (closed: 207–78.1%; exposed: 58–21.9%), posterior (closed: 7–77.8%; exposed: 2–22.2%) and anterior (closed: 4–80%; exposed: 1–20%); while for lateral dislocations, closed (64–58.2%) and exposed (46–41.8%) dislocations are more uniformly distributed.
Reduction in the dislocation was achieved using solely external intervention in 264 patients (68%), while open reduction was required in 124 patients (32%). In one of the five patients in the article by Dimentberg et al. [20], the type of reduction performed was not described.
Once again, this ratio of around 2:1 between closed and open reductions was approximately maintained among medial dislocations (closed: 197–74.6%; open: 67–25.4%), posterior (closed: 7–77.8%; open: 2–22.2%) and anterior (closed: 3–60%; open: 2–40%). In the case of lateral dislocations, however, it was necessary much more frequently to perform open reduction (closed: 57–51.8%; open: 53–48.2%).
To stabilise the reduction, K-wires or external fixators were used in 27 medial dislocations (10.2% of the total number of medial dislocations), 26 lateral (23.6%) and two anterior (40%), and thus a total of 55 cases (14.2% of the total number of dislocations). There were no cases of posterior dislocations that required final stabilisation using K-wires or external fixators.
Of the total of 389 patients, 171 (44%) were described as having one or more associated injuries. These injuries (fractures of the midfoot, hindfoot or ankle and tendon or vasculonervous injuries) were present in 35.5% of medial dislocations (94 cases), 44.5% of lateral dislocations (48 cases), 22.2% of posterior dislocations (two cases) and all five cases of anterior dislocation.
The article by Bibbo et al. [14] does not provide a description of the correspondence between associated injuries (found in 22 cases in 25 patients) and direction of dislocation.
A check-up CT following completion of the reduction manoeuvre was only performed in 63 patients, namely 16.2% of cases (14% of medial dislocations, 18.5% of lateral, 33.3% of posterior and 60% of anterior).
Associated injuries were diagnosed using conventional x-rays in 128 patients of 149 (85.9%) and CT scans in 19 patients of 149 (12.75%). In two cases (fracture of the head of the talus and injury to the posterior tibial tendon and flexor digitorum longus), diagnosis was made directly in the operating theatre. In 22 patients with associated injuries in the Bibbo et al. [14] case series for whom the direction of dislocation is not stated, no indication of the method (x-ray, CT scan) used to make the diagnosis has been provided.
Discussion
The greater complexity of managing lateral dislocation is probably the reason why recent years have seen the attention of authors focused more on these dislocations than on medial forms. In fact, the prevalence of lateral dislocations in our review is almost 30%, compared to 15%–20% reported in the literature.
The purpose of this study is to highlight the most insidious aspects in the diagnosis and treatment of subtalar dislocations, especially the more complicated lateral dislocations.
Indeed, lateral dislocations are made even more challenging by the ease with which the head of the talus is exposed through the medial and skin capsular tissues in a context of high-energy trauma. The technical difficulties associated with reduction are thus increased by the need to ensure meticulous soft tissue handling to prevent insidious infectious complications. Our review confirms this fact: medial dislocations are exposed in 21.9% of cases, while lateral forms are exposed in 41.8%.
The reduction manoeuvre extensively described in the literature involves bending the knee to release the traction of the Achilles tendon on the calcaneus, followed first by accentuating and then inverting the deformity.
We documented a failure of closed reduction in 32% of dislocations. Difficulties in performing reductions are much more evident for lateral dislocations (48.2% of open reductions) than for medial forms (open reduction in 25.4% of cases).
The reduction in subtalar dislocations is often prevented by the inclusion of soft tissues or bone fragments.
In the case of lateral dislocations, inclusions most often involve the posterior tibial tendon, and sometimes the flexor digitorum longus or flexor hallucis longus tendon. In the latter case, it is typical to note the flexion of the first toe as an indirect sign of stretching of the flexor hallucis longus tendon.
In medial dislocations, instead, the extensor retinaculum constitutes the principal obstacle to closed reduction. Less frequently, open reduction is made necessary by the inclusion of the extensor hallucis brevis and the extensor digitorum brevis [54].
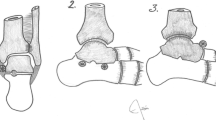
In dislocations complicated by inclusion of tendon or capsular structures or fracture fragments, reduction using external manoeuvres is impractical and it is absolutely necessary to carry out surgical reduction as soon as possible. This involves identifying the interposed structures and moving them away from the subtalar joint (Fig. 1). Awareness of this eventuality is essential in preventing futile attempts at reduction and enabling rapid repositioning of the talus, a factor that strongly influences the risk of avascular necrosis.
With regard to the more complicated lateral dislocations, an x-ray indicator of the difficulty of closed reduction can be seen clearly on the latero-lateral views (Fig. 2, red arrow). As shown in Fig. 2 the empty space between the head of the talus and the tarsal navicular bone is due to the inclusion of the posterior tibial tendon.
Observation of this x-ray sign and an awareness of the main methods for inclusion of the posterior tibial tendon in lateral dislocations [55] (Fig. 3) can facilitate the reduction in lateral dislocations.
Principal methods for inclusion of the posterior tibial tendon in lateral subtalar dislocations [55]
Once the reduction in the dislocation has been achieved, it is not sufficient to take simple x-rays. A CT scan should be performed to exclude misrecognised fractures that can lead to osteoarthritis and chronic instability, especially in the hindfoot [9, 56].
Of the total of 171 fractures associated with the 389 cases in our review, 19 (12.75%) were diagnosed using CT scans.
The fractures most commonly associated with this type of dislocation are those of the body, neck or head of the talus or of the sustentaculum tali or fractures of the lateral process of the talus, also known as a Snowboarder’s fracture. Fractures of the cuboid, navicular and calcaneus bones occur more rarely.
For this aspect also, we can confirm that lateral dislocations are more difficult to manage. According to our review, these forms have associated injuries in 44.5% of cases, compared to 35.5% of medial dislocations.
The duration of immobilisation remains a matter of debate. In the case of uncomplicated dislocations, it is often possible to put weight on the joint after a period of immobilisation lasting three-four weeks. For complicated dislocations, this period is frequently extended to six-eight weeks, depending on the type of associated fractures.
The literature describes a worse prognosis for lateral dislocations compared to medial forms [2] and an unsatisfactory long-term outcome for 10%–32% of lateral dislocations treated conservatively. The only long-term complication described for dislocations without associated fractures or injuries is a limitation of the ROM of the subtalar joint, with consequent difficulty in maintaining balance on uneven surfaces.
On the other hand, the incidence of infections and avascular necrosis is more than 30% in patients with lateral subtalar dislocations complicated by associated fractures or injuries of the soft tissues with or without contamination [57].
Indeed, lateral dislocations are more frequently associated with bone exposure and associated injuries. Furthermore, they more often require open reduction and the use of K-wires to guarantee the stability of the reduction.
In our review, we have deliberately not considered and tabulated the outcomes for the patients screened. In fact, different types of scores have been used in the articles examined to quantify the outcome and often the individual articles have grouped together types of patients who are very different from each other in clinical terms. In our opinion a comparison of the long-term outcome among these groups of patients would not be valuable (for example: outcome for patients with subtalar dislocation associated with bone exposure vs outcome for patients with subtalar dislocation without associated injuries). In four of the studies examined [16, 35, 37, 45], the AOFAS [58] scale was used, but this score has not been validated for this type of injury. Lastly, in many of the articles reviewed, no score has been used to quantify the outcome, but instead a qualitative description has been provided on the basis of the clinical course, making it impossible to compare them with the outcomes of other cases present in the literature.
Our review confirms the greater complexity of managing lateral dislocations compared to medial ones and reports the major pitfalls that must be taken into consideration by the surgeon dealing with this injury.
Change history
24 July 2022
Missing Open Access funding information has been added in the Funding Note
References
Judcy P (1811) Observation d’une luxation metatarsienne. Bull Fac Med Paris 11:81–86
Perugia D, Basile A, Massoni C, Gumina S, Rossi F, Ferretti A (2002) Conservative treatment of subtalar dislocations. Int Orthop 26(1):56–60. https://doi.org/10.1007/s002640100296 (PMID: 11954852)
Zimmer TJ, Johnson KA (1989) Subtalar dislocations. Clin Orthop Relat Res 238:190–194 (PMID: 2910600)
Malgaigne JF, Buerger CG (1856) Die Knochenbrüche und Verrenkungen. Rieger, Stuttgart, p 820
Plewes LW, McKelvey KG (1944) Subtalar dislocation. J Bone Joint Surg Am 26(3):585–588
Monson ST, Ryan JR (1981) Subtalar dislocation JBJS 63A:1156–1158 (PMID: 7276051)
Inokuchi S, Hashimoto T, Usami N (1997) Posterior subtalar dislocation. J Trauma 42(2):310–313. https://doi.org/10.1097/00005373-199702000-00023 (PMID: 9042888)
Goldner JL, Poletti SC, Gates HS 3rd, Richardson WJ. Severe open subtalar dislocations. Long-term results. J Bone Joint Surg Am 1995; 77(7):1075–9 doi: https://doi.org/10.2106/00004623-199507000-00015 PMID: 7608231
Bibbo C, Lin SS, Abidi N, Berberian W, Grossman M, Gebauer G, Behrens FF (2001) Missed and associated injuries after subtalar dislocation: the role of CT. Foot Ankle Int 22(4):324–328. https://doi.org/10.1177/107110070102200409
Azarkane M, Boussakri H, Alayyoubi A, Bachiri M, Elibrahimi A, Elmrini A (2014) Closed medial total subtalar joint dislocation without ankle fracture: a case report. J Med Case Reports 8(1):313. https://doi.org/10.1186/1752-1947-8-313 (PMID: 25240955)
Bak K, Koch JS (1991) Subtalar dislocation in a handball player. Br J Sports Med 25(1):24. https://doi.org/10.1136/bjsm.25.1.24 (PMID: 1913026)
Bali K, Kumar V, Bhagwat K, Rawall S (2011) Closed posterior subtalar dislocation without any associated fracture: a case report and review of the literature. Foot Ankle Surg 17(3):e40–e42. https://doi.org/10.1016/j.fas.2011.04.005 (PMID: 21783063)
Banerjee S, Abousayed MM, Vanderbrook DJ, Bagchi K (2017) Lateral Subtalar dislocation with tarsometatarsal dislocation: a case report of a rare injury. Case Rep Orthop 2017:8090721. https://doi.org/10.1155/2017/8090721 (PMID: 28761771)
Bibbo C, Anderson RB, Davis WH (2003) Injury characteristics and the clinical outcome of subtalar dislocations: a clinical and radiographic analysis of 25 cases. Foot Ankle Int 24(2):158–163. https://doi.org/10.1177/107110070302400210 (PMID: 12627624)
Camarda L, Martorana U, D’Arienzo M (2009) Posterior subtalar dislocation. Orthopedics 32(7):530. https://doi.org/10.3928/01477447-20090527-25 (PMID: 19634836)
Camarda L, Abruzzese A, La Gattuta A, Lentini R, D’Arienzo M (2016) Results of closed subtalar dislocations. Musculoskelet Surg 100(1):63–69. https://doi.org/10.1007/s12306-015-0380-1 (PMID: 26254192)
Chuo CY, Lu CC, Liu PC, Shen WJ (2005) Anterior subtalar dislocation: a case report. Kaohsiung J Med Sci 21(1):40–43. https://doi.org/10.1016/S1607-551X(09)70275-X (PMID: 15754588)
de Palma L, Santucci A, Marinelli M, Borgogno E, Catalani A (2008) Clinical outcome of closed isolated subtalar dislocations. Arch Orthop Trauma Surg 128(6):593–598. https://doi.org/10.1007/s00402-007-0459-8 (PMID: 17909825)
de Palma L, Santucci A, Marinelli M (2008) Irreducible isolated subtalar dislocation: a case report. Foot Ankle Int 29(5):523–526. https://doi.org/10.3113/fai.2008.0523 (PMID: 18510909)
Dimentberg R, Rosman M (1993) Peritalar dislocations in children. J Pediatr Orthop 13(1):89–93. https://doi.org/10.1097/01241398-199301000-00018 (PMID: 8416362)
Edmunds I, Elliott D, Nade S (1991) Open subtalar dislocation. Aust N Z J Surg 61(9):681–686. https://doi.org/10.1111/j.1445-2197.1991.tb00320.x (PMID: 1877937)
Fotiadis E, Lyrtzis C, Svarnas T, Koimtzis M, Akritopoulou K, Chalidis B (2009) Closed subtalar dislocation with non-displaced fractures of talus and navicular: a case report and review of the literature. Cases J. https://doi.org/10.4076/1757-1626-2-8793 (PMID: 19918402)
Gaba S, Kumar A, Trikha V, Das S, Agrawal P (2017) Posterior dislocation of subtalar joint without associated fracture: a case report and review of literature. J Clin Diagn Res. https://doi.org/10.7860/JCDR/2017/27794.10553 (PMID: 29207793)
Garofalo R, Moretti B, Ortolano V, Cariola P, Solarino G, Wettstein M, Mouhsine E (2004) Peritalar dislocations: a retrospective study of 18 cases. J Foot Ankle Surg 43(3):166–172. https://doi.org/10.1053/j.jfas.2004.03.008 (PMID: 15181433)
Giuffrida AY, Lin SS, Abidi N, Berberian W, Berkman A, Behrens FF (2003) Pseudo os trigonum sign: missed posteromedial talar facet fracture. Foot Ankle Int 24(8):642–649. https://doi.org/10.1177/107110070302400813 (PMID: 12956572)
Ghani Y, Marenah K, Kumar PA (2014) Isolated proximal rupture of flexor digitorum longus tendon in a traumatic open subtalar dislocation. Ann R Coll Surg Engl 96(6):e10–e12. https://doi.org/10.1308/003588414X13946184902802 (PMID: 25198961)
Giannoulis D, Papadopoulos DV, Lykissas MG, Koulouvaris P, Gkiatas I, Mavrodontidis A (2015) Subtalar dislocation without associated fractures: Case report and review of literature. World J Orthop 6(3):374–379. https://doi.org/10.5312/wjo.v6.i3.374 (PMID: 25893182)
Hoexum F, Heetveld MJ (2014) Subtalar dislocation: two cases requiring surgery and a literature review of the last 25 years. Arch Orthop Trauma Surg 134(9):1237–1249. https://doi.org/10.1007/s00402-014-2040-6 (PMID: 24993588)
Hui SH, Lui TH (2016) Anterior subtalar dislocation with comminuted fracture of the anterior calcaneal process. BMJ Case Rep. https://doi.org/10.1136/bcr-2015-213835 (PMID: 26887882)
Inokuchi S, Hashimoto T, Usami N, Ogawa K (1996) Subtalar dislocation of the foot. Foot 6(4):168–174. https://doi.org/10.1016/S0958-2592(96)90016-4
Jayaprakash MR, Kulumbi V, Sampagar A, Umarani C (2011) Lateral subtalar dislocation of the foot: a case report. Foot Ankle Online J. https://doi.org/10.3827/faoj.2011.0411.0001
Jerome JT, Varghese M, Sankaran B (2007) Anteromedial subtalar dislocation. J Foot Ankle Surg 46(1):52–54. https://doi.org/10.1053/j.jfas.2006.10.003 (PMID: 17198954)
Jerome JT (2008) Antero-lateral subtalar dislocation. Foot Ankle Surg 14(1):36–39. https://doi.org/10.1016/j.fas.2007.08.002 (PMID: 19083610)
Jerome JTJ, Varghese M, Sankaran B, Thirumagal K (2008) Lateral subtalar dislocation of the foot: a case report. The Foot & Ankle Journal 1(12):2. https://doi.org/10.3827/faoj.2008.0112.0002
Jungbluth P, Wild M, Hakimi M, Gehrmann S, Djurisic M, Windolf J, Muhr G, Kälicke T (2010) Isolated subtalar dislocation. J Bone Joint Surg Am 92(4):890–894. https://doi.org/10.2106/JBJS.I.00490 (PMID: 20360512)
Kanda T, Sakai H, Koseki K, Tamai K, Takeyama N, Saotome K (2001) Anterior dislocation of the subtalar joint: a case report. Foot Ankle Int 22(7):609–611. https://doi.org/10.1177/107110070102200715 (PMID: 11503990)
Karampinas PK, Kavroudakis E, Polyzois V, Vlamis J, Pneumaticos S (2014) Open talar dislocations without associated fractures. Foot Ankle Surg 20(2):100–104. https://doi.org/10.1016/j.fas.2013.12.005 (PMID: 24796827)
Kinik H, Oktay O, Arikan M, Mergen E (1999) Medial subtalar dislocation. Int Orthop 23(6):366–367. https://doi.org/10.1007/s002640050396 (PMID: 10741528)
Krishnan KM, Sinha AK (2003) True posterior dislocation of subtalar joint: a case report. J Foot Ankle Surg 42(6):363–365. https://doi.org/10.1053/j.jfas.2003.09.004 (PMID: 14688779)
Kulambi V, Gaurav M (2014) Lateral subtalar dislocation: a case report. Foot Ankle Online J. https://doi.org/10.3827/faoj.2014.0703.0004
Lasanianos NG, Lyras DN, Mouzopoulos G, Tsutseos N, Garnavos C (2011) Early mobilization after uncomplicated medial subtalar dislocation provides successful functional results. J Orthop Traumatol 12(1):37–43. https://doi.org/10.1007/s10195-011-0126-2 (PMID: 21308390)
McKeag P, Lyske J, Reaney J, Thompson N (2015) Subtalar dislocation secondary to a low energy injury. BMJ Case Rep. https://doi.org/10.1136/bcr-2014-208828 (PMID: 25650063)
Milenkovic S, Mitkovic M, Bumbasirevic M (2006) External fixation of open subtalar dislocation. Injury 37(9):909–913. https://doi.org/10.1016/j.injury.2006.02.051 (PMID:16769070)
Merchan EC (1992) Subtalar dislocations: long-term follow-up of 39 cases. Injury 23(2):97–100. https://doi.org/10.1016/0020-1383(92)90041-p (PMID: 1572724)
Ruhlmann F, Poujardieu C, Vernois J, Gayet LE (2017) Isolated acute traumatic subtalar dislocations: review of 13 cases at a mean follow-up of 6 years and literature review. J Foot Ankle Surg 56(1):201–207. https://doi.org/10.1053/j.jfas.2016.01.044 (PMID: 26947001)
Specchiulli F, Gabrieli R, Di Carlo V, Maiorana B (2007) Peritalar dislocations. Foot 17(1):10–14. https://doi.org/10.1016/j.foot.2006.07.006
Stafford H, Boggess B, Toth A, Berkoff D (2013) Anteromedial subtalar dislocation. BMJ Case Rep. https://doi.org/10.1136/bcr-03-2012-3973 (PMID: 23355551)
Tucker DJ, Burian G, Boylan JP (1998) Lateral subtalar dislocation: review of the literature and case presentation. J Foot Ankle Surg 37(3):239–247. https://doi.org/10.1016/s1067-2516(98)80118-x (PMID: 9638551)
Ruiz Valdivieso T, Miguel Vielba JA, Hernandez Garcia C, Castrillo AV, Alvarez Posadas JI, Sanchez Martin MM (1996) Subtalar dislocation. Int Orthopaed 20(2):83–86. https://doi.org/10.1007/s002640050035
Veltman ES, Steller EJ, Wittich P, Keizer J (2016) Lateral subtalar dislocation: case report and review of the literature. World J Orthop 7(9):623–627. https://doi.org/10.5312/wjo.v7.i9.623 (PMID: 27672576)
Wagner R, Blattert TR, Weckbach A (2004) Talar dislocations. Injury. https://doi.org/10.1016/j.injury.2004.07.010 (PMID: 15315877)
Yglesias B, Andrews K, Hamilton R, Lea J, Shah R, Ebraheim N (2018) Case report: irreducible medial subtalar dislocation with incarcerated anterior talar head fracture in a young patient. J Surg Case Rep. https://doi.org/10.1093/jscr/rjy168 (PMID: 30046437)
Zaraa M, Jerbi I, Mahjoub S, Sehli H, Mbarek M (2017) Irreducible subtalar dislocation caused by sustentaculum tali incarceration. J Orthop Case Rep 7(1):58–60. https://doi.org/10.13107/jocr.2250-0685.688 (PMID: 28630842)
Leitner B (1954) Obstacles to reduction in subtalar dislocations. J Bone Joint Surg Am 36:299–306 (PMID: 13152139)
Mulroy RD (1955) The tibialis posterior tendon as an obstacle to reduction of a lateral anterior subtalar dislocation. J Bone Joint Surg Am 37:859–63 (PMID: 13242616)
Bohay DR, Manoli A 2nd (1996) Occult fractures following subtalar joint injuries. Foot Ankle Int 17(3):164–169. https://doi.org/10.1177/107110079601700309 (PMID: 8919622)
Lancaster S, Horowitz M, Alonso J (1985) Subtalar dislocations: a prognosticating classification. Orthopedics 8(10):1234–1240 (PMID: 2869474)
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15(7):349–353. https://doi.org/10.1177/107110079401500701 (PMID: 7951968)
Funding
Open access funding provided by Università degli Studi di Verona within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
the authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lugani, G., Rigoni, M., Puddu, L. et al. Subtalar dislocation: a narrative review. Musculoskelet Surg 106, 337–344 (2022). https://doi.org/10.1007/s12306-022-00746-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-022-00746-x