Abstract
Introduction
Chopart injuries can be allocated into 4 broad groups, ligamentous injury with or without dislocation and fracture with or without dislocation, which must occur at the talonavicular joint (TNJ) and/or calcaneocuboid joint (CCJ). Chopart dislocations are comprised of pure-dislocations and fracture-dislocations. We aim to review the literature, to enable evidence-based recommendations.
Methods
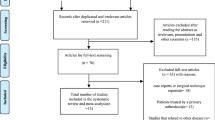
A literature search was conducted to identify relevant articles from the electronic databases, PubMed, Medline and Scopus. The PRISMA flow chart was used to scrutinise the search results. Articles were screened by title, abstract and full text to confirm relevance.
Results
We identified 58 papers for analysis, 36 case reports, 4 cohort studies, 4 case series and 14 other articles related to the epidemiology, diagnosis, treatment and outcomes of Chopart dislocations. Diagnostic recommendations included routine imaging to contain computed tomography (CT) and routine examination for compartment syndrome. Treatment recommendations included early anatomical reduction, with restoration and maintenance of column length and joint congruency. For both pure-dislocations and fracture-dislocations urgent open reduction and internal fixation (ORIF) provided the most favourable long-term outcomes.
Conclusions
Chopart dislocations are a complex heterogenous midfoot injury with historically poor outcomes. There is a relative paucity of research discussing these injuries. We have offered evidence-based recommendations related to the clinical and surgical management of these rare pathologies.
Similar content being viewed by others
Introduction
The midtarsal or transverse-tarsal joint, is otherwise known eponymously as the Chopart joint, after French surgeon François Chopart described an amputation through the articulation between the hindfoot and the midfoot [1]. The Chopart joint is made up of the TNJ and calcaneocuboid joint CCJ. The TNJ makes up part of the coxa pedis (talocalcaneonavicular joint) which enables pronation and supination of the tarsus [2]. The CCJ provides approximately 25° of rotation for hindfoot eversion and inversion [3]. The Chopart joint enables hindfoot pivot, allowing the forefoot to remain inverted or everted on heel inversion, locking the Chopart joint, stabilizing the midfoot during gait push-off phase [4]. Thus, the Chopart joint is fundamental for normal foot function and requires strong ligamentous support. The TNJ is supported superiorly by the dorsal talonavicular ligament and medial limb of the bifurcate ligament and inferiorly by the spring ligament (calcaenonavicular ligament) comprised of the medioplantar oblique, inferoplantar longitudinal and superomedial components [4]. The CCJ is supported superiorly by the dorsal calcaneocuboid ligament and the lateral limb of the bifurcate ligament and inferiorly by the short plantar ligament (plantar calcaneocuboid ligament) [4].
The cyma line (Fig. 1) represents the Chopart joint and can be observed via dorsoplantar and lateral views [5], where radiological discrepancy indicates pathology. Therefore, Initial imaging should start with radiographs in 3 views dorsoplantar, lateral and oblique [6]. Oblique views are optimal for visualising fractures of the anterior calcaneal process [4].
Chopart injuries can be allocated into 4 broad groups, ligamentous injury with or without dislocation and fracture with or without dislocation, which must occur at the TNJ and/or CCJ. Chopart dislocations include both pure-dislocations and fracture-dislocations. Pure-dislocations are defined as dislocation of the navicular and/or cuboid without associated fracture. Fracture-dislocations are defined as dislocation of the navicular and/or cuboid with associated fracture of one or more of talus, navicular, calcaneus or cuboid including avulsion fractures. Dislocation of both the TNJ and CCJ simultaneously, may be referred to as a complete Chopart dislocation. Swivel dislocations typically result from medial or lateral deforming forces causing TNJ and/or CCJ dislocation and the calcaneus ‘swivels’ on an intact talocalcaneal ligament [7]. We have provided radiological examples of a Chopart fracture (Fig. 2) and fracture-dislocation (Fig. 3). We have also provided an explanation of Main and Jowett’s landmark classification [8] of Chopart injuries, with a focus on dislocations (Table 1).
Aims
We aim to review the literature to provide evidence-based recommendations for the diagnosis and management of Chopart dislocations, to improve outcomes for future patients. We also aim to gain further insight into the incidence and aetiology, prognostic factors and management options for these rare injuries.
Methods
Study selection
The electronic databases PubMed, Medline and Scopus were utilised. A preliminary search with no inclusion or exclusion criteria was carried out to gauge the amount of existing literature. This demonstrated a relatively low quantity of existing papers and as a result the set inclusion and exclusion criteria were broad. We included any papers relating to acute traumatic Chopart dislocations and/or Chopart fracture-dislocations in the adult population (Table 2). We excluded papers that were not accessible from the authors online catalogue and any papers not published in English to mitigate translational errors. A literature search was undertaken to identify all related papers. Two search term strings, one anatomical and one related to the type of injury, were combined to narrow down the search to related papers. Applied search terms included “Chopart joint”, “Midtarsal joint”, “Dislocation” and “Fracture-dislocation”. The search identified 181 papers on PubMed/Medline and 280 on Scopus. The PRISMA flow chart was used to scrutinise the initial search results (Table 3). Duplicates were removed and abstracts from these papers were screened for relevance. Articles were selected based on relevance to the topic area and title of the review. The full text of each study was then assessed, and any further non-suitable papers excluded in accordance with the inclusion and exclusion criteria.
Results
We identified 58 papers for review, 36 case reports, 4 cohort studies, 4 case series and 14 other papers related to the epidemiology, diagnosis, treatment and outcomes of Chopart dislocations and fracture-dislocations.
Cohort studies and case series
Incidence and aetiology
A retrospective epidemiology cohort study by Ponkilainen et al. of 307 midfoot injuries suggests the incidence of midfoot injury to be 12.1/100,000/year and Chopart injury to be 2.2/100,000/year [16]. Motor vehicle accidents (MVA) are the primary aetiology for Chopart dislocations are more common in males [6, 12]. Richter et al. found 16% of 155 midfoot fractures were Chopart fracture-dislocations [12]. A follow-up study conducted of 110 Chopart-dislocations, 25% were found to be pure-dislocations, 55% fracture-dislocations and 20% combined Chopart-Lisfranc fracture-dislocations [6]. A recent study of 128 Chopart joint injuries found only 5 patients (3.7%) had pure-dislocations and the most frequent fracture-dislocation was transnavicular/transcuboidal in 21% of cases [15]. The average age was 36.8 years (5 studies) (Table 4).
Diagnosis
5/7 studies did not report method of diagnosis. Of the two studies that did, XR plus CT scanning was used. One reported delayed diagnosis for more than 24 h in 22.1% of the 122-patient cohort [15]. In the second, two injuries were initially missed after inspection of plain films and injury severity was underestimated in three injuries prior to CT scanning (Table 4) [5].
Management
83% of 60 Fracture-dislocations were managed with ORIF ± external fixation [6]. 19 of 28 pure-dislocations were managed initially with closed reduction, although six of these required additional internal fixation and one external fixation [6]. Compartment syndrome requiring fasciotomy was reported in 11.6% of 155 midfoot injuries [12], 9.4% of 128 Chopart injuries [15] and 25.5% of 110 Chopart dislocations [12]. Zero percent of pure-dislocations, 5% of fracture-dislocations and 25% (2 studies, n = 48) of combined Chopart-lisfranc fracture-dislocations required primary amputation [6, 12]. 7/128 Chopart injuries required primary arthrodesis and 4.7% of cases required late fusion at the Chopart joint [15].
Outcomes
Average AOFAS score for each Chopart injury classification across the cohorts and case series reviewed (Table 4). Isolated Chopart fractures: 81.0 (1 study, n = 18). Chopart fracture-dislocations: 70.3 (3 studies, n = 54). Chopart pure-dislocations: 79.0 (1 study, n = 14). Combined Chopart-Lisfranc fracture dislocations: 58.0 (2 studies, n = 26).
Richter et al. reported Isolated Chopart fractures had significantly better AOFAS-Midfoot scores than Chopart fracture-dislocations [12]. The highest scores in all groups were achieved in those fractures treated with early ORIF. No significant differences in the scores were found for age, gender or aetiology. Radiographic comparison of Chopart fracture-dislocation (n = 15) against isolated Chopart fracture (n = 18) at an average follow up of 9 years. Incorrect medial column length 27% vs 6%. Incorrect lateral column length 20% vs 11%. Abnormal longitudinal arch shape 40% vs 22%. Arthritic changes 67% vs 33% [12]. There was a high correlation correct column length and good functional outcomes [12]. Furthermore, Mittlmeier et al. found the loss of foot column length had a substantial influence on gait quality and the severity of post-traumatic arthritis had no significant influence [11].
In a follow up study by Richter et al. focussed on Chopart dislocations, those who underwent internal fixation following closed reduction had significantly worse outcomes than those who underwent ORIF in the first place [6]. No significant differences in functional outcomes were found between age, gender or methods of internal fixation when comparing screws and/or K-wires [6]. AOFAS scores were significantly lower in MVA than in non-MVA and in open injuries versus closed. Polytrauma, associated fractures and delayed surgery > 1 day from injury were also significant negative prognostic factors. Those with compartment syndrome had significantly better outcomes, however these patients all had expedited surgery within 24 h [6].
Rammelt et al. followed up 75 Chopart injuries for an average of 10.2 years [15]. ORIF led to significantly better results that closed reduction and percutaneous fixation across all Chopart injuries including pure-dislocations and fracture-dislocations [15]. Only 4% of 128, Chopart injuries were pure-dislocations which had significantly inferior Foot Function Index and AOFAS scores than patients with Chopart fractures or fracture–dislocations [15]. Negative prognostic factors included, high injury severity score, work-related accidents, open and multiple fractures, pure-dislocations, staged surgery, delay of treatment > 4 weeks, post-operative infection and primary or secondary fusion [15].
Van Dorp et al. presented 7 patients with Chopart dislocations [5]. The mean AOFAS score was 72 and the mean VAS score for patient satisfaction was 7.1/10 at an average 31.3 month follow-up [5]. 4/7 patients still experienced pain or limitation of daily activities at follow-up [5]. Another case series by Kosters et al. saw 6 patients with Chopart fracture-dislocations report a mean AOFAS of 66, half of patients were found to have post-traumatic arthritis and one patient had pathological medial column length, at a median follow-up of 2.6 years [14]. Eight malunited Chopart fracture-dislocations underwent secondary anatomic reconstruction, on average 10 months following injury [13]. Seven patients had joint sparing reconstruction with ORIF, and one TNJ arthrodesis. The mean AOFAS pre-operatively and at 2-year follow-up were 38.8 and 80.8 respectively, (p < 0.0001). Active inversion/eversion of the foot (total coronal plane motion) averaged 18° preoperatively and 41° at follow-up, excluding the TNJ fusion [13].
Case reports—Chopart pure-dislocation
Twelve case reports of pure-dislocations were identified for review (Appendix Table 5). The average age was 39.1 with a 3:1 male to female ratio. Half of injuries were caused by MVA and One third were precipitated by falls. 5/12 were complete Chopart dislocations. 5/12 reports were isolated swivel dislocations of the navicular (4 medial, 1 lateral), which was most frequently dislocated in isolation (7/12). The CCJ was not found to dislocate in isolation. The plantar ecchymosis sign was not reported in any cases. Imaging most frequently consisted of XR plus CT (7/12). In nine cases, closed reduction was attempted which failed in four. Of the five cases treated with closed reduction, three were managed non-operatively. Seven out of twelve cases underwent open reduction with additional internal fixation of five and arthrodesis of two. Follow up was provided for 10 cases between six and 76 months. Five of these had significant long-term complications, which ranged from pain on prolonged standing, to pes planus and midfoot arthritis.
Case reports—Chopart fracture-dislocation
24 case reports of Chopart fracture-dislocations were identified (Appendix Table 6). The average age was 34.8 with a 2.4:1 male to female ratio. The most common aetiology was MVA in 10 reports. According to dislocation type, 13 were TNJ dislocations, 6 CCJ dislocations and 5 complete Chopart dislocations. The calcaneus was most commonly fractured (13/24), followed by the navicular (10/24), cuboid (7/24) and talus (4/24). Eleven reports used XR alone for diagnosis, 13 used additional CT. Two Chopart fracture-dislocations were initially missed on XR. The plantar ecchymosis sign was reported in two cases. Where closed reduction was attempted, 7/18 failed. 11 cases were successfully reduced, although 8 required surgical fixation. Thirteen cases had open reduction, definitive management was ORIF for 11 and arthrodesis for 2. Follow up ranged from 3.5 months to 5 years with 2 cases lost to follow-up. 13/22 cases had sequalae, ranging from pain to pes planus and malunion. 3/22 of cases required further surgery. Eight cases had definitive treatment more than 48 h after injury, six of these had complications at follow-up. Seven out of twenty-four cases provided AOFAS scores between 3.5 and 24 months, with a mean score of 87.7.
Discussion
Clinical signs
The plantar ecchymosis sign (PES) describes a central midfoot plantar ecchymosis that is pathognomic for relevant midfoot injuries indicating rupture of strong plantar ligaments and resulting haematoma [17]. PES has been recorded following calcaneal fractures [18], Lisfranc [19] and Chopart injuries [20]. PES was not reported in the cohort studies or case series reviewed, although 2/36 case reports reported the PES. The PES is a rarely reported but valuable clinical sign indicating underlying midfoot injury, CT is encouraged where PES is positive and radiographs negative. Clinicians should carefully examine and palpate the entire foot alongside confirming the neurovascular status and have a high index of suspicion for compartment syndrome which is common in Chopart injuries [12, 15], especially dislocations [6].
Imaging
The wider literature has shown, up to 41% of Chopart injuries are missed at first presentation [5]. Haapamaki et al. found plain radiographs alone missed 33% of fractures in Chopart injuries [21]. From Van Dorp et al. Case series of 9 Chopart dislocations, 2 were initially missed from XR alone and the severity of injury was underestimated for 3 prior to CT, alongside this 2/24 fracture-dislocations from case reports were initially missed on XR (Appendix Table 6). Furthermore Rammelt et al. found pure-dislocations to be very rare (4%) and encourage CT scanning to rule out associated fracture [15]. This is in concordance with Almeida et al. who found a significant improvement in identifying additional Chopart fractures missed on XR with CT [22]. Furthermore, CT allows reconstructive modelling to determine the degree of dislocation [4]. We recommend CT to be included in the diagnostic workup of all suspected Chopart injuries.
Management and outcomes
For Chopart dislocations including pure-dislocations and fracture-dislocations, initial ORIF provides better outcomes than closed reduction prior to internal fixation [6]. Closed reduction alone was found to have statistically similar outcomes to operative treatment [6], however, 6 of 14 pure-dislocations required internal fixation following closed reduction and therefore should have undergone ORIF initially. Due to the risk of requiring internal fixation following closed reduction, urgent ORIF is advised and closed reduction should be discouraged. Furthermore, closed reduction is challenging, often fails and repeated attempts may cause further damage [23]. For Chopart injuries in general including isolated fractures, fracture-dislocations and pure-dislocations, Rammelt et al. found over a 10-year follow up that ORIF generates significantly better results than closed reduction and percutaneous fixation [15]. It is important to note that according to Rammelt et al. [15] pure-dislocations had the worst prognosis, however, AOFAS scores were not provided and could not be included in the average across studies.
Maintenance of foot column length significantly improves gait quality [11]. We agree with Van Dorp et al. that correct alignment of the foot axes and correct length of medial and lateral columns should be a major goal of therapy [5], these have been regularly incorrect at follow up, thus this should be addressed peri-operatively and corrected where possible. For malunited Chopart fracture-dislocations, secondary reconstruction improves outcomes in suitable patients otherwise joint fusion is required [13]. Arthrodesis is implemented in late presentations [24], in patients with diabetic arthropathy [25], or when other treatment strategies have failed where arthrodesis can prevent midfoot collapse [26]. TNJ Arthrodesis can reduce the Chopart joint range of motion by 50% and is a negative prognostic factor [15], so is considered a last resort [27]. Soft tissue condition can help to dictate treatment methods, where external fixation can maintain reduction during soft tissue healing [15, 28] and maintain column length with unstable ORIF [29]. Patients with Chopart pure-dislocations and fracture-dislocations require long term follow-up to monitor for complications which were common [5, 14].
Limitations
There was marked heterogeneity of the reviewed studies in terms of injury pattern, injury classification, treatment modality and outcome reporting which led to difficulties in performing systematic review, which was our original intention. This was coupled with the paucity of research on this topic due to the rarity of the injury itself.
Conclusion
This review focussed on Chopart dislocations. Pure-dislocations appear to have inferior outcomes due to the high energy required to disrupt the strong ligamentous anatomy at the Chopart joint. There is a general consensus that closed reduction often fails and leads to poorer outcomes, even if followed by ORIF. Besides joint reconstruction, restoring and maintaining the medial and lateral foot columns is essential to obtain reasonable results. CT and compartment syndrome evaluation is highly recommended. Urgent ORIF ± external fixation is the management of choice for pure-dislocations and fracture-dislocations. Negative prognostic markers included, severity of injury, delayed or staged treatment, arthrodesis and MVA.
References
Wolf JH (2000) Francois Chopart (1743–1795) – inventor of the partial foot amputation at the transtarsal articulation. Orthop Traumatol 8(4):314–317
Kou JX, Fortin PT (2009) Commonly missed peritalar injuries. J Am Acad Orthop Surg 17(12):775–786
Walter WR, Hirschmann A, Alaia EF, Tafur M, Rosenberg ZS (2019) Normal anatomy and traumatic injury of the midtarsal (Chopart) joint complex: an imaging primer. Radiographics 39(1):136–152
Walter WR, Hirschmann A, Tafur M, Rosenberg ZS (2018) Imaging of Chopart (midtarsal) joint complex: normal anatomy and posttraumatic findings. AJR Am J Roentgenol 211(2):416–425
Van Dorp KB, de Vries MR, van der Elst M, Schepers T (2010) Chopart joint injury: a study of outcome and morbidity. J Foot Ankle Surg 49(6):541–545
Richter M, Thermann H, Huefner T, Schmidt U, Goesling T, Krettek C (2004) Chopart joint fracture-dislocation: initial open reduction provides better outcome than closed reduction. Foot Ankle Int 25(5):340–348
Pillai A, Chakrabarti D, Hadidi M (2006) Lateral swivel dislocation of the talo-navicular joint. Foot Ankle Surg 12:39–41
Main BJ, Jowett RL (1975) Injuries of the midtarsal joint. J Bone Joint Surg Br 57(1):89–97
Klaue K (2004) Chopart fractures. Injury 35(Suppl 2):SB64-70
Lasanianos NG, Kanakaris NK (2015) Midtarsal bones chopart joint dislocations. Trauma and orthopaedic classifications. Springer, London, pp 383–386
Mittlmeier T, Krowiorsch R, Brosinger S, Hudde M (1997) Gait function after fracture-dislocation of the midtarsal and/or tarsometatarsal joints. Clin Biomech (Bristol, Avon) 12(3):S16–S17
Richter M, Wippermann B, Krettek C, Schratt HE, Hufner T, Therman H (2001) Fractures and fracture dislocations of the midfoot: occurrence, causes and long-term results. Foot Ankle Int 22(5):392–398
Rammelt S, Zwipp H, Schneiders W, Heineck J (2010) Anatomic reconstruction of malunited Chopart joint injuries. Eur J Trauma Emerg Surg 36(3):196–205
Kösters C, Bockholt S, Müller C, Winter C, Rosenbaum D, Raschke MJ, Ochman S (2014) Comparing the outcomes between Chopart, Lisfranc and multiple metatarsal shaft fractures. Arch Orthop Trauma Surg 134(10):1397–1404
Rammelt S, Missbach T (2023) Chopart joint injuries: assessment, treatment, and 10-year results. J Orthop Trauma 37(1):e14–e21
Ponkilainen VT, Laine HJ, Mäenpää HM, Mattila VM, Haapasalo HH (2019) Incidence and characteristics of midfoot injuries. Foot Ankle Int 40(1):105–112
Rammelt S (2014) Chopart and lisfranc fracture-dislocations. In: Bentley G (ed) European surgical orthopaedics and traumatology: the EFORT textbook. Springer Berlin Heidelberg, Berlin, Heidelberg, pp 3835–3857
Richman JD, Barre PS (1986) The plantar ecchymosis sign in fractures of the calcaneus. Clin Orthop Relat Res 207:122–125
Ross G, Cronin R, Hauzenblas J, Juliano P (1996) Plantar ecchymosis sign: a clinical aid to diagnosis of occult Lisfranc tarsometatarsal injuries. J Orthop Trauma 10(2):119–122
Dewar FP, Evans DC (1968) Occult fracture-subluxation of the midtarsal joint. J Bone Joint Surg Br 50(2):386–388
Haapamaki VV, Kiuru MJ, Koskinen SK (2004) Ankle and foot injuries: analysis of MDCT findings. AJR 183:615–622
Almeida RR, Mansouri M, Tso DK, Johnson AH, Lev MH, Singh AK, Flores EJ (2018) The added value of cross-sectional imaging in the detection of additional radiographically occult fractures in the setting of a Chopart fracture. Emerg Radiol 25(5):513–520
Honeycutt MW, Perry MD (2019) The Chopart variant dislocation: plantar dislocation of the cuboid and navicular. Foot Ankle Orthop 4(3):2473011419876262
Kumar A, Gaba S, Digge VK, Gautam D (2020) Neglected medial swivel talonavicular dislocation treated with arthrodesis: a case report and literature review. J Clin Orthop Trauma 11(3):474–478
Ansari MAQ (2016) Isolated complete dislocation of the tarsal navicular without fracture: a rare injury. Ci Ji Yi Xue Za Zhi 28(3):128–131
Arain AR, Adams CT, Haddad SF, Moral M, Young J, Desai K, Rosenbaum AJ (2020) Diagnosis and treatment of peritalar injuries in the acute trauma setting: a review of the literature. Adv Orthop 2020:1852025
Johnstone AJ, Maffulli N (1998) Primary fusion of the talonavicular joint after fracture dislocation of the navicular bone. J Trauma 45(6):1100–1102
Klaue K (2010) Treatment of Chopart fracture-dislocations. Eur J Trauma Emerg Surg 36(3):191–195
Kutaish H, Stern R, Drittenbass L, Assal M (2017) Injuries to the Chopart joint complex: a current review. Eur J Orthop Surg Traumatol 27(4):425–431
Jung KJ, Lee HS, Chang HJ, Lee YK, Yeo ED, Won SH, Cho HK, Ryu A, Lee DW, Kim WJ (2021) Pure isolated medial talonavicular joint dislocation following low-energy trauma: a case report. J Int Med Res 49(4):3000605211004697
Datt N, Rao AS, Rao DV (2009) Medial swivel dislocation of the talonavicular joint. Indian J Orthop 43(1):87–89
Genena A, Abouelela A, Fadel MH (2021) A case report with review of literature of a rare variant of midfoot dislocations (mid-Chopart dislocation): combined naviculo-cuneiform and calcaneo-cuboid dislocation. Foot (Edinb) 47:101806
Puthezhath K, Veluthedath R, Kumaran CM, Patinharayil G (2009) Acute isolated dorsal midtarsal (Chopart’s) dislocation: a case report. J Foot Ankle Surg 48(4):462–465
Ip KY, Lui TH (2006) Isolated dorsal midtarsal (Chopart) dislocation: a case report. J Orthop Surg (Hong Kong) 14(3):357–359
Harris AP, Gil JA, Goodman AD, Nacca CR, Borenstein TR (2016) Acute plantar midtarsal dislocation with intercuneiform dislocation: case study, diagnosis and management. J Orthop 14(1):26–29
Inal S, Inal C (2013) An unusual variety of simultaneous fracture dislocation pattern: medial swivel dislocation of talonavicular joint with displaced fractures of the fourth and fifth metatarsals. J Foot Ankle Surg 52(4):501–504
Ruthman JC, Meyn NP (1988) Isolated plantar midtarsal dislocation. Am J Emerg Med 6(6):599–601
Kapila R, Verka PS, Garg RS, Ahmed M (2015) Lateral swivel dislocation of the hindfoot: a case report and literature review. J Foot Ankle Surg (Asia-Pacific) 2(1):41–43
Dhole KP, Bandebuche AR, Marathe NA, Date S, Raj A (2020) An unusual midfoot dislocation involving naviculocuneiform and calcaneocuboid joint following low-energy injury: a case report. J Orthop Case Rep 10(6):41–43
Donthi SR, Veerappa LA (2021) Dorsal Chopart’s fracture dislocation - a rare injury. Foot (Edinb) 48:101834
Kanwat H, Mittal S, Trikha V (2021) Neglected medial swivel dislocation of talonavicular joint with calcaneus, cuboid and 5th metatarsal fractures - a case report. J Clin Orthop Trauma 15:168–171
González IS, García MM (2016) Missed Chopart dislocation. The importance of being aware of midtarsal injuries. An Sist Sanit Navar 39(1):153–158
Layson JT, Afsari A, Peterson T, Knesek D, Best B (2021) A fixed, unreducible, unstable medial swivel dislocation of the talonavicular joint with associated navicular fracture. Case Rep Orthop 2021:9959830
Hagino T, Tonotsuka H, Ochiai S, Hamada Y (2009) Fracture of the anterior extremity of calcaneus together with calcaneocuboid joint dislocation. Arch Orthop Trauma Surg 129(12):1673–1676
Davis AT, Dann A, Kuldjanov D (2013) Complete medial dislocation of the tarsal navicular without fracture: report of a rare injury. J Foot Ankle Surg 52(3):393–396
Alayed IS (2021) Combined midfoot dislocation involving the naviculocuneiform and calcaneocuboid joints: a case report. Egypt J Hosp Med 83(1):1017–1020
Rao H (2012) Complete open dislocation of the navicular: a case report. J Foot Ankle Surg 51(2):209–211
Samoladas E, Fotiades H, Christoforides J, Pournaras J (2005) Talonavicular dislocation and nondisplaced fracture of the navicular. Arch Orthop Trauma Surg 125(1):59–61
Schildhauer TA, Nork SE, Sangeorzan BJ (2003) Temporary bridge plating of the medial column in severe midfoot injuries. J Orthop Trauma 17(7):513–520
Harris AP, Johnson J, Waryasz GR (2016) Isolated dorsal dislocations of the talonavicular and calcaneocuboid articulations (Chopart joints) from a low-energy mechanism. Am J Emerg Med 34(8):1733.e1–4
Fares A, Orfeuvre B, Al Ezz MA, Pailhe R (2022) An unusual midfoot injury pattern: navicular-cuneiform and calcaneal-cuboid fracture-dislocation. Trauma Case Rep 1(41):100679
Alhadhoud MA, Alsiri NF, Mohammad DA, Ibrahim A, Aboubakr MK, Abdulghany M, Fathy A (2022) Open fracture dislocation of the calcaneocuboid and naviculocuneiform joints: a case report. Trauma Case Rep 38:100611
Puente CA et al (1996) Tarsal fracture dislocation with plantar dislocation of the navicular: a case study. Foot Ankle Int 17(2):111–113
Algouaiz A, Alharbi J, Alwayil A, Alattas M (2021) Medial talonavicular dislocation with nondisplaced navicular fracture: a case report. Int J Surg Case Rep 85:106276
Mathesul AA, Sonawane DV, Chouhan VK (2012) Isolated tarsal navicular fracture dislocation: a case report. Foot Ankle Spec 5(3):185–187
Williams DP, Hanoun A, Hakimi M, Ali S, Khatri M (2009) Talonavicular dislocation with associated cuboid fracture following low-energy trauma. Foot Ankle Surg 15(3):155–157
Powell E, LaBella M (2011) Swivel-type dislocation of the talonavicular joint: a case report. Foot Ankle Online J 4(6):3
Kummer A, Crevoisier X, Eudier A (2020) Calcaneocuboid and naviculocuneiform dislocation: an unusual injury of the midfoot. Case Rep Orthop 2020:8818823
Schmitt JW, Werner CM, Ossendorf C, Wanner GA, Simmen HP (2011) Avulsion fracture of the dorsal talonavicular ligament: a subtle radiographic sign of possible Chopart joint dislocation. Foot Ankle Int 32(7):722–726
Viegas GV (2000) Midtarsal joint dislocations: acute and chronic management with review of literature and case presentation. Foot 10(4):198–206
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
None required, review paper.
Informed consent
None required, review paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Metcalfe, T.S.N., Aamir, J. & Mason, L.W. Chopart dislocations: a review of diagnosis, treatment and outcomes. Arch Orthop Trauma Surg 144, 131–147 (2024). https://doi.org/10.1007/s00402-023-05040-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05040-4