Abstract
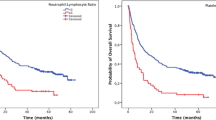
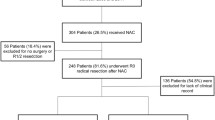
To study the role of the absolute lymphocyte count (ALC), absolute monocyte count (AMC), platelet count (PLT), lymphocyte–monocyte ratio (LMR) and the platelet–lymphocyte ratio (PLR) in the prognosis of primary gastrointestinal diffuse large B cell lymphoma (PGI-DLBCL). We retrospectively analyzed the prognostic value of the ALC, AMC, PLT, LMR, PLR at diagnosis in 173 PGI-DLBCL patients through histopathological examination from March 2009 to February 2015. In total, 173 patients with histopathological diagnosis of PGI-DLBCL in this study, the median age was 51 years (range 12–90 years), median follow-up time was 44 months (range 7–89 months). In univariate analysis, age <60 years, B symptoms, Lugano stage I–II, low international prognostic index (IPI) or low age-adjusted international prognostic index (aaIPI), normal lactate dehydrogenase (LDH), normal β2-microglobulin (β2m), Hb ≥ 11 g/dL, ALC ≥ 1.5 × 109/L, AMC ≤ 0.50 × 109/L, LMR ≥ 2.5, PLR ≤ 170 were related with superior overall survival (OS) and progression-free survival (PFS) (p ≤ 0.05). Multivariate analysis suggested that ALC, LMR, LDH were related with PFS (p ≤ 0.05). Similarly, age and LMR were related with OS (p ≤ 0.05). The parameters (ALC, AMC, LMR, PLR) may be valuable prognostic factors in PGI-DLBCL patients. LMR, PLR at diagnosis are expected to be independent prognostic factors for PGI-DLBCL patients.


Similar content being viewed by others
References
Delfa Radic-Krito APP, Ostojic S, Vrhovac R, Kardum-Skelin I, Jakcs B (2010) Primary gastrointestinal non-Hodgkin lymphoma in adults: clinicopathologic and survival characteristics. Coll Antropol 34(2):413–417
Erkurt MA, Aydogdu I, Kuku I, Kaya I, Basaran Y (2009) Clinicopathologic characteristics and therapeutic outcomes of primary gastrointestinal non-Hodgkin’s lymphomas: 10 years of experience from a single center in eastern Anatolia. Med Princ Pract 18(5):399–406
Feng J, Wang W, Wang J, Jing H, Jijun W, Liu Y, Zhao W, Ke X (2014) Clinicopathological characteristics and prognostic analysis of 92 cases with primary gastrointestinal diffuse large B-cell lymphoma. Zhonghua Xue Ye Xue Za Zhi 35(4):288–294
Gunaldi M, Goksu S, Erdem D, Gunduz S, Ozdem Y, Inan YO, Tiken E, Kahraman S, Inan YO, Genc TB, Yildirim M (2015) Prognostic impact of platelet/lymphocyte and neutrophil/lymphocyte ratios in patients with gastric cancer: a multicenter study. Int J Clin Exp Med 8(4):5937–5942
Zhang S, Wang L, Yu D, Shen Y, Cheng S, Zhang L, Qian Y, Shen Z, Li Q, Zhao W (2015) Localized primary gastrointestinal diffuse large B cell lymphoma received a surgical approach: an analysis of prognostic factors and comparison of staging systems in 101 patients from a single institution. World J Surg Oncol 13:246
Zhao H, Zhang LE, Guo S, Yuan T, Xia B, Zhang L, Zhang Y (2015) Overexpression of DNA methyltransferase 1 as a negative independent prognostic factor in primary gastrointestinal diffuse large B-cell lymphoma treated with CHOP-like regimen and rituximab. Oncol Lett 9(5):2307–2312
Li YL, Gu KS, Pan YY, Jiao Y, Zhai ZM (2014) Peripheral blood lymphocyte/monocyte ratio at the time of first relapse predicts outcome for patients with relapsed or primary refractory diffuse large B-cell lymphoma. BMC Cancer 14(1):1
Lia YL, Gu KS, Panb YY, Jiaob Y, Zhaia ZM (2014) The lower peripheral blood lymphocyte/monocyte ratio assessed during routine follow-up after standard first-line chemotherapy is a risk factor for predicting relapse in patients with diffuse large B-cell lymphoma. Leuk Res 38(3):323–328
Hu P, Shen H, Wang G, Zhang P, Liu Q, Du J (2014) Prognostic significance of systemic inflammation-based lymphocyte–monocyte ratio in patients with lung cancer: based on a large cohort study. PLoS One 9(10):e108062
Lin B, Chen C, Qian Y, Feng J (2015) Prognostic role of peripheral blood lymphocyte/monocyte ratio at diagnosis in diffuse large B-cell lymphoma: a meta-analysis. Leuk Lymphoma 9(56):1–6
Chen L, Zhang F, Sheng XG, Zhang SQ (2015) Decreased pretreatment lymphocyte/monocyte ratio is associated with poor prognosis in stage Ib1–IIa cervical cancer patients who undergo radical surgery. Onco Targets Ther 8:1355–1362
Wang T, Gui W, Shen Q (2010) Primary gastrointestinal non-Hodgkin’s lymphoma: clinicopathological and prognostic analysis. Med Oncol 27(3):661–666
Azambuja D, Natkunam Y, Biasoli I (2011) Lack of association of tumor-associated macrophages with clinical outcome in patients with classical Hodgkin’s lymphoma.pdf. Ann Oncol 23(3):736–742
Porrata LF, Ristow K, Colgan JP, Habermann TM, Witzig TE, Inwards DJ, Ansell SM, Micallef IN, Johnston PB, Nowakowski GS, Thompson C, Markovic SN (2012) Peripheral blood lymphocyte/monocyte ratio at diagnosis and survival in classical Hodgkin’s lymphoma. Haematologica 97(2):262–269
Huang Y, Feng JF (2015) Low preoperative lymphocyte–monocyte ratio predicts poor cancer-specific survival in patients with esophageal squamous cell carcinoma. Onco Targets Ther 8:137–145
Koh YW, Kang HJ, Park C, Yoon DH, Kim S, Suh C, Go H, Kim JE, Kim CW, Huh J (2012) The ratio of the absolute lymphocyte count to the absolute monocyte count is associated with prognosis in Hodgkin’s lymphoma: correlation with tumor-associated macrophages. Oncologist 17:871–880
Shibutani M, Maeda K, Nagahara H (2015) Prognostic significance of the lymphocyte-to-monocyte ratio in patients with metastatic colorectal cancer. World J Gastroenterol 21(34):9966–9973
Jia J, Zheng X, Chen Y, Wang L, Lin L, Ye X, Chen Y, Chen D, Dettke M (2015) Stage-dependent changes of preoperative neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in colorectal cancer. Tumor Biol 36:9319–9325
Li F, Hu H, Gu S (2015) Platelet to lymphocyte ratio plays an important role in prostate cancer’s diagnosis and prognosis. Int J Clin Exp Med 8(7):11746–11751
Li X, Han Z, Cheng Z, Yu J, Yu X, Liang P (2015) Clinical significance of preoperative platelet-to-lymphocyte ratio in recurrent hepatocellular carcinoma after thermal ablation: a retrospective analysis. Int J Hyperth 31:758–763
Sun W, Zhang L, Luo M, Hu G, Mei Q, Liu D, Long G, Hu G (2015) Pretreatment hematologic markers as prognostic factors in patients with nasopharyngeal carcinoma: Neutrophil-lymphocyte ratio and platelet–lymphocyte ratio. Head Neck 38(51):E1332–E1340
Shirai Y, Shiba H, Sakamoto T, Horiuchi T, Haruki K, Fujiwara Y, Futagawa Y, Ohashi T, Yanaga K (2015) Preoperative platelet to lymphocyte ratio predicts outcome of patients with pancreatic ductal adenocarcinoma after pancreatic resection. Surgery 158(2):360–365
Rosenwald A, Wright G, Chan WC, Connors JM, Campo E, Fisher RI, Gascoyne RD, Muller-Hermelink HK, Smeland EB, Giltnane JM, Hurt EM (2002) The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N Engl J Med 346(25):1937–1947
Haarer CF, Roberts RA, Frutiger YM, Grogan TM, Rimsza LM (2006) Immunohistochemical classification of de novo, transformed, and relapsed diffuse large B-cell lymphoma into germinal center B-cell and nongerminal center B-cell subtypes correlates with gene expression profile and patient survival. Arch Pathol Lab Med 130(12):1819–1824
Nyman HA, Karjalainen-Lindsberg M, Taskinen ML, Berglund M, Amini RM, Blomqvist C, Enblad G, Leppa S (2007) Prognostic impact of immunohistochemically defined germinal center phenotype in diffuse large B-cell lymphoma patients treated with immunochemotherapy. Blood 109(11):4930–4935
Acknowledgments
I would like to express my gratitude to all those who helped me during the writing of this thesis. I gratefully acknowledgement the help of my supervisor, Dr. Xiaofang Wang, for her constant encouragement and guidance. Also, I owe much to Miss Li Zang for her valuable suggestion and critiques which are of help and important in making the thesis a reality. This research was supported by grants from the National Natural Science Foundation of China (No. 81272562).
Funding
This study was funded by the National Natural Science Foundation of China (Grant Number 81272562).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Zhao, P., Zang, L., Zhang, X. et al. The Lymphocyte–Monocyte Ratio and the Platelet–Lymphocyte Ratio at Diagnosis as Independent Prognostic Factors in Primary Gastrointestinal Diffuse Large B Cell Lymphoma. Indian J Hematol Blood Transfus 33, 333–341 (2017). https://doi.org/10.1007/s12288-016-0720-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-016-0720-9