Abstract
Reliable monitoring of one’s response to exercise intensity is imperative to effectively plan and manage training, but not always practical in impact sports settings. This study aimed to evaluate if an inexpensive mobile cardio-respiratory monitoring system can achieve similar performance to a metabolic cart in estimating rated perceived exertion. Eight adult men volunteered to perform treadmill tests under different conditions. Cardiorespiratory data were collected using a metabolic cart and an instrumented oral-cavity device, as well as their ratings of perceived exertion. Pearson correlation corrected for repeated measurements and stepwise regression analysis were used to observe the relationship between the cardiorespiratory features and the ratings of perceived exertion and determine the proportion of the variance of exertion that could be explained by the measurements. Minute ventilation was found to be the most associated variable to perceived exertion, closely followed by a novel metric called the audio minute volume, which can be collected by the oral-cavity device. A generalised linear model combining minute ventilation, audio minute volume, heart rate and respiration rate accounted for 64% of the variance in perceived exertion, whilst a model with only audio minute volume accounted for 56%. Our study indicates that minute ventilation is key to estimating perceived exertion during indoor running exercises. Audio minute volume was also observed to perform comparably to a lab-based metabolic cart in estimating perceived exertion. This research indicates that mobile techniques offer the potential for real-world data collection of an athlete’s physiological load and estimation of perceived exertion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Fatigue is defined as the “sensations of tiredness and associated decrements in muscular performance and function” [1]. It comprises behavioural, metabolic and mental effects that can affect the physical performance of participants [2]. Fatigue is best described in terms of losing maximum or potential performance due to activity, where performance is carefully described in terms of, e.g. force, speed or power [3]. Monitoring fatigue is crucial for evaluating real-world performance and it allows for a better understanding of its effects in different activities, especially in athletic performance [4].
Within team sports, fatigue is a risk factor for injuries [5,6,7,8]. Studies in injury patterns in football suggest that musculoskeletal injuries are more likely towards the end of each half of a match [9, 10]. However, it is a constant challenge for coaches, doctors and physiotherapists to prescribe sufficient training load for an athlete while minimising overtraining and risk of injury [11]. Inter-individual variations in response to exercise may result in some athletes at risk of overtraining and others unstimulated in response to similar prescribed exercise [12,13,14]. Understanding one’s response to exercise intensity is imperative to effectively plan and manage training.
Several metrics and scales exist to measure human fatigue and its effects [15]. The Borg Rated Perceived Exertion (RPE) scale is widely used for monitoring the conscious perception of exertion [16]. It ranges from “6” to “20” where multiplying the RPE score by ten would indicate the corresponding resting heart rate (HR) of a normal healthy adult man in beats per minute. Borg also developed the Category-Ratio (CR) scales Borg CR10 ranging from “0” to “10” [17]. The Borg scales are recognised for measuring whole-body exertion, muscle pain and strain [8]. Higher RPE levels typically indicate higher levels of perceived physiological stress and fatigue. Mental fatigue also affects RPE and can impact overall performance in physical tasks whilst having no changes in the metabolic response of the body. These results indicate a high connection between RPE, motivation and cognitive depletion [2]. This renders RPE highly sensitive to subjective perturbations. Nevertheless, its use is well-established in sports science and occupational health [14, 18, 19].
RPE is a metric for quantifying the conscious sensation of exertion [20]. Whilst RPE is often linked to the level of physical effort (how intense or strenuous a physical task is), it captures holistically other stressors beyond physical effort [21]. In practice, however, RPE is a subjective measure that requires direct surveying, which therefore limits its use for monitoring an athlete's health. The American College of Sports Medicine warrants further investigation into the use of subjective metrics to prescribe specific training intensities [22]. RPE also demands a series of training and familiarisation sessions between athletes and coaches to consistently rate the training load, limiting its use by elite and especially non-elite athletes [23,24,25,26]. Finally, any subjective metric of athletic effort is impractical during competitions. For these reasons, it would be desirable to be able to identify detectable factors that underpin the RPE and estimate it through the use of ubiquitous measurement systems. Considering that the RPE scale was inspired by the HR response of the body under physical stress, it is not surprising that HR can act as a good proxy for RPE. However, the variation in HR can be multi-factorial [27, 28]. The interpretation of HR alone to reflect the internal load of an athlete may not be straight forward [28, 29]. Other physiological factors also affect the individual’s perception of effort. Minute ventilation (VE) has also been known to be associated with physical stressors. VE depends on both respiration rate (Rf) and tidal volume (VT) [30, 31]. For lower levels of exercise, the VT normally changes first and as the activity level increases, Rf starts to respond. There is evidence that Rf or other respiratory factors may be associated with fatigue measured as RPE. Nicolo et al. reported that Rf may be insightful at monitoring exertion during cycling and football exercises [21, 32, 33]. Nevertheless, the exact association between Rf and RPE could differ based on the mode of exercise due to locomotor–respiratory coupling effect [31].
Given that RPE cannot be directly measured in real-time and that there is a need to monitor physical as well as perceived effort during activities, it is important to evaluate the physiological response to the load that occur in training and competition scenarios. Portable versions of metabolic carts, frequently used in laboratory tests, have been used in outdoors sports scenarios [13, 34]. Impact sports such as Australian Football and Rugby rely on HR as a physiological measure during competition due to the high costs and the difficulties in safely capturing other metabolic signals [19]. Nevertheless, the training load applied to athletes may not be fully explained by the measures available in these environments [21].
We aim to compare the estimation of RPE response based on cardiorespiratory parameters collected from commercial metabolic carts and an inexpensive mobile instrumented oral-based device. Considering that VE, Rf and VT are associated with RPE, we speculate that proxy measurements of these parameters extracted from the participants' breathing audio response could also be associated with RPE. As VE is a product of Rf and VT we propose to also examine the RPE association of a novel metric, audio minute volume (aVE) comprised of the Rf and the intensity of the breathing audio. A three-stage treadmill test designed to collect metabolic and RPE responses of athletes while running. The collected cardiorespiratory parameters and their associated RPE will be examined first by studying the correlation between RPE and each metabolic variable. Second, a generalised linear model (GLM) was used as a tool to identify metabolic variables that are important for understanding RPE. The ultimate aim of this study is to demonstrate the feasibility of tracking athletic performance and fatigue based on signals obtainable from an inexpensive mobile device.
2 Materials and methods
2.1 Participants
For this study, data were collected from eight healthy male volunteers. The participants were all recreational athletes from contact sports and were familiarised with the use of mouthguards. The participants had an age range of 20–39 years, 72–120 kg and height 170–187 cm. All participants were informed of the general purpose of the study and gave written consent. The experimental protocols were approved by the Research Ethics Committee of the University of Oxford (R43470/RE001). Our participants were self-declared healthy and capable of carrying out the intense activity required.
2.2 Familiarisation session
A preliminary data-acquisition session was performed in an outdoor setting, where the participants were asked to wear both an instrumented oral-cavity device for respiratory audio recording and a portable metabolic cart. The participants were then asked to perform the 20 m multi-stage fitness test, also known as the beep test [35], running between lanes marked with the RPE Borg CR10 scale with verbal anchors [36]. Participants were instructed to step on the lane with the RPE level that best corresponded to their overall fatigue level at each running round (see Fig. 1). RPE “0”, omitted from the lines, was assumed to be scored when participants step out of the line beyond the RPE “1” score. Both end lines were filmed and RPE level at each running round was recorded. This session did not include acquisition of all required data for the final study and was used primarily for the participants to familiarise with the use of the oral-cavity device, the metabolic cart and the RPE Borg CR10 scale with verbal anchors. Data from this session were not used for drawing any major conclusions for this study.
a Experimental setup for the outdoor familiarisation session. Subjects were asked to perform the 20 m multi-stage fitness test between two lines with RPE CR10 lanes [35]. Both lines were recorded for posterior analysis of the RPE. b Lanes with the RPE CR10 with verbal anchors [36]. The participants had to step at the lane that best correspond to their RPE level at each stage of the test
2.3 Experimental protocol
Al least 48 h after the familiarisation session, the participants performed the experimental protocol containing three running tests: a maximal oxygen consumption (VO2Max) test, a time-to-exhaustion test and an interval test. Participants were asked to wear both the instrumented oral-cavity device for respiratory audio recording and a metabolic system from 2 min before the start of the activity until 2 min after the end of each test. Between each test, the participants had 10 min of recovery (of which 6 min without wearing any systems). All tests were completed on a Woodway PPS55 Sport treadmill. Each participant was familiarised with the equipment before the experiments.
The RPE Borg CR10 scale with verbal anchors [36] was placed in front of the treadmill at a readable distance from the participants. Prior to the session start, participants stretched and warmed up by running on the treadmill at their own selected pace for up to 10 min. Participants were informed of the experimental protocol and on how to assess RPE during exercise. They were requested to score their overall fatigue level either by pointing to the RPE scale or by showing the score count with their hands. The participants were asked to score their RPE level every 30 s and were also encouraged to notify the researchers of their fatigue level whenever they felt it had changed.
Following the warm-up, the participants’ VO2Max were tested under an incremental speed test. The treadmill’s speed profile was set initially at 9 km/h with a 0.75 km/h increase every minute. The end of the test was signalled by the participant when they could no longer continue the activity. VO2Max was validated by two or more of the following: a plateau in oxygen consumption, a respiratory exchange ratio > 1.15, an RPE > 9, and HR within ± 10 beats/min of the age-predicted maximum. The final speed increment recorded before the end of the test was termed the VO2Max speed and was used in subsequent tests. During the time-to-exhaustion test, the participants were asked to run at their VO2Max speed for as long as possible. During the interval test, the participants were asked to complete five 1-min intervals at their VO2Max speed, with a 30 s rest between each interval.
2.4 Measurements of metabolic variables
Respiratory data were obtained using a Metamax MetaLyzer 3B-R3 metabolic system (Cortex Metamax, Germany) in the breath-by-breath (B × B) modality. Data was collected through a V2 series face mask (Hans Rudolph Incorporated, Kansas, USA) and fed to the cart via a cable connection.
Calibrations were undertaken following the manufacturer’s guidelines. The application and fitting of the face mask were completed as stated by the instructions for use.
HR data were captured using a POLAR H1 heart rate monitor (Polar NV, Finland) positioned on the thorax of the participant, using an elastic strap.
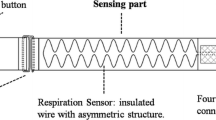
A personalised instrumented oral-cavity device was made for each participant. The device comprised of the commercially available STEVAL-STLKT01V1 development board (STMicroelectronics, Switzerland) housed in ethylene–vinyl acetate and positioned in the palate of the participant's oral cavity (Fig. 2). This device contains an ARM Cortex-M4 microprocessor (STM32L476JGY, STMicroelectronics, Switzerland) capable of running at up to 80 MHz, a Bluetooth 4.2 network processor (BlueNRG-MS, STMicroelectronics, Switzerland), a digital microphone (MP34DT05-A, STMicroelectronics, Switzerland) with a 64 dB signal-to-noise ratio and − 26 dBFS ± 3 dB sensitivity, and SD memory card slot. Breathing audio was sampled at 8 kHz and 16 bits per sample. The development board also contains a battery charger and a 100 mAh rechargeable lithium-ion battery, which was charged to full capacity before encapsulation for each testing series. The housing was made from the dental casts of each participant using a thermoforming process, to obtain a tight fit. The audio was recorded as WAV files in the SD Card and later recovered by the authors.
Data alignment of the instrumented device and the metabolic cart were achieved by asking the participants to hold a breath for 5 s immediately before the start of each test, as this was a respiratory event that could be visually identified on both systems.
2.5 Signal processing
All data processing were performed posterior to the experiments. The aVE was calculated by obtaining the product of the audio volume amplitude and the Rf. Rf can also be obtained from the audio data through signal processing methods [37,38,39,40,41], although this process demands a validation that is beyond the aims of this study. For this reason, only the Rf from the metabolic cart, the gold standard, was used for the following analysis. Preliminary testing identified noise related to stepping and movement to be under 100 Hz, as well as those related to coughing and speech to be above 400 Hz. Breathing audio was isolated with a second-order Butterworth band-pass filter with corner frequencies at 100 and 400 Hz. The audio volume amplitude was calculated using the RMS of the audio samples during the breath period as indicated by the metabolic system.
In all the tests, Rf (breaths/min), VE (l/min), VT (l/breath), oxygen volume (VO2, ml min−1 kg−1) HR (beats/min), and aVE (audio intensity/min) were recorded.
Readings resulting from spurious breathing events were filtered out using the localised mean and standard deviation [42]. The filtered data were interpolated to 1-s intervals and averaged in 10-s bins [21].
After the pre-processing, the maximum VO2 value was obtained at the last minute of each test per participant, named VO2peak. The reference for all the other parameters (HRpeak, VEpeak, VTpeak, Rfpeak, and aVEpeak) was obtained at the time point when the participants achieved their VO2peak. All parameters were normalised using the individual’s peak values.
2.6 Statistical analysis
Pearson correlation analysis with the repeated observation correction [43] was calculated and examined for correlations between RPE and each metabolic variable. Next, a simple generalised linear model was built using stepwise regression method performed on all the data. The prediction terms were added to or removed from the model based on the model deviance. A normal distribution was determined and a P value < 0.05 was considered statistically significant. This model was applied to understand how RPE variance is explained under the assumption of linearity and independence of the predictors.
3 Results
3.1 Exercise outcomes
All participants were able to complete the VO2Max test to volitional fatigue. However, not all test sets by all participants were successfully recorded with the measurement systems. One time-to-exhaustion and one interval test were not performed by one participant, due to a minor injury. Another interval test and VO2Max test from two other participants were excluded, due to technical problems in the recording equipment. A total of five complete test sets and three incomplete sets were used for data analysis (see Table, Online Resource 1, for pre-processed data). Corrupted test data from any participant were excluded from the final analysis. Cardiorespiratory and physical endpoints are in Table 1.
3.2 Relationship to cardiorespiratory measures
Pearson correlation analyses were performed to indicate which of the physiological predictors were more closely associated with RPE. Within-participant variability biases were eliminated using the repeated observation corrections [43]. VE showed the highest correlation to RPE (r = 0.843), followed by aVE (r = 0.831), Rf (r = 0.774), HR (r = 0.770), VO2 (r = 0.705) and VT (r = 0.381). All results were significant (P-value < 0.05).
3.3 Perceived exertion modelling
All data points from all tests associated with each RPE score were binned together to form the boxplots of predictors against RPE (Fig. 3). This data aggregation did not differentiate recovery and exercise moments. The stepwise regression analysis was performed to build a GLM and assess how much the predictors account for the variance in the RPE. When using all the available predictors, both from mobile sources and from the metabolic cart the final univariate GLM consisting of the determinants and their interactions that best predict maximal RPE follows the equation RPE ~ 1 + VE + aVE + HR + VO2. The model yielded an adjusted coefficient of determination (R2) of 0.640, Akaike information criterion of 2230.58, a root mean-squared error of 1.6202, a normalised root mean-squared error of 16.20%, and included VE, VO2, HR and aVE with P-value at < 0.01. VE appeared the most significant and accounted for about 58.4% of the variability in RPE. aVE and HR came next as second and third most significant predictors, respectively, and accounted each for an additional 2.3% of the variance. Finally, VO2 was the least significant predictor added and accounted for under 1% of the variance in the data. When restricting the possible predictors to only aVE, the resulting model yielded an R2 of 0.568, an Akaike information criterion of 2334.12, a root mean-squared error of 1.7851 and a normalised root mean-squared error of 17.85%. (see Table, Online Resource 2, for information on the GLM models).
Boxplot of the normalised metabolic data and the Borg CR10 Rating of Perceived Exertion (RPE) levels. Heart rate (HR), respiration frequency (Rf), minute ventilation (VE), tidal volume (VT), oxygen volume (VO2), and audio minute volume (aVE) are normalised by their value at the moment of VO2Max. VO2Max was defined as the maximum value of VO2 in the last minute of any test of each athlete
4 Discussion
This study compared strategies for capturing cardiorespiratory parameters and estimating RPE during running exercises. We compared the data acquired from a metabolic card and an oral-based monitoring system. A novel metric, aVE, that can be measured by an instrumented oral-cavity device was introduced. RPE was used to quantify the fatigue felt by the participant. Using the Pearson correlation analysis and the generalised linear model approach, VE was found to be the most important metabolic parameter for characterising fatigue. It has the highest correlation of all parameters (r = 0.843) and accounts for about 58% of the RPE variance. VE can be combined with HR, aVE, and VO2 in a linear model to estimate about 64% of RPE’s variance. Our results also indicate that aVE is the second most important metabolic parameter both in correlation (r = 0.831) and in explanation of variability of RPE. Note that aVE and HR are parameters that can be measured using inexpensive mobile systems. This preliminary result indicates that such monitoring devices may be useful to estimate the physiological response to exercise. In addition to this result, an R2 of 0.513 was found for a model that just includes aVE indicating that it can be used to some extent for RPE prediction.
Our outcomes corroborate the association between cardiorespiratory parameters with RPE suggested by Nicolo et al. indicating that breathing parameters (including VE and Rf) are more significant than HR for explaining RPE during various tests of changing intensity for cyclists and football players [21, 32, 33, 44, 45]. We also found that HR, although not as relevant as VE and aVE, can still be useful for explaining RPE. This result corroborates the results of Zinoubi et al. showing that HR is highly correlated with RPE when compared across continuous and alternating intensity exercises [46].
This research shows that an oral-based monitoring system could be used in competition scenarios of impact sports and provide insights into the player’s fatigue. A device capable of monitoring respiratory rate can be applied to track physical effort to theoretically improve the immediate response to athlete fatigue in the field. Such a device has the potential to provide truly ubiquitous sensing within contact sports creating new opportunities in player management. This approach is less expensive than the use of portable metabolic carts and it could be combined with HR, positional and inertial sensors to better inform coaches and reduce training imbalances among the athletes.
The designed test protocol was intentionally physically exhausting for the participants to enable capturing data points more evenly across all fatigue levels rather than just at the lower level. This approach allowed higher confidence in the model predictions, especially for the higher fatigue levels. However, since all the exercises were performed in 1 day, results for individuals’ variations in different test days could not be extrapolated. Also, the accumulated fatigue limited the performance of the participants, especially during the time-to-exhaustion test, which required the participants to run at VO2Max speed just 10 min after running the VO2Max test until volitional exhaustion. It is important to note that during our study, participants were requested to score their overall fatigue level and not their current effort level. For this reason, the RPE scores provided may be different from “0” when the participants are in recovery. Indeed, this is noticeable in the RPE levels reported during the rest periods of the interval test, where participants were reporting increasingly higher RPE levels in rest as the test progressed. This phenomenon was expected by the authors based on the experimental protocol chosen. This study design adds a bias towards the measurement of fatigue instead of the measurement of effort, which limits its direct comparison with some of the results of other studies.
Regarding the perceived exertion, it can be noted that no single variable can explain all the variance observed in RPE. RPE is a subjective metric that includes the whole-body experience and is likely to encompass more than just objective physiological predictors [36]. RPE was shown vary during different formats of rugby-specific training while maximum HR and time spend above 85% of maximum HR have no significant difference [47]. This result combined with the studies indicating that session RPE may be a reliable method to quantify intensities of resistance training [48], collision-based team sports [49] and soccer [50] suggest that RPE may offer an ability to monitor anaerobic exertion. These studies, however, do not include respiration based metrics which are better associated with perceived exertion and exercise tolerance than heart rate, blood lactate and oxygen uptake for some experimental conditions, including, muscle damage, muscle fatigue, respiratory muscle fatigue, and prior exercise [51]. Even though a remarkable level of explained variance was reached using solely the respiratory metrics, our study was not designed to analyse in detail the implications of anaerobic exertion. Further studies should be performed to investigate how aVE is affected by resistance training.
It is also important to observe that the tests were performed using recreational athletes. As listed in the exercise outcomes, the peak oxygen consumption, the short duration of the time-to-exhaustion tests (mean just above 3 min under the mean speed of 14.40 km/h) and other performance indicators point to active participants at a non-elite group. Due to limitations of non-elite athletes under acute physical exercise, such as lower perceptual-cognitive performance [52], different exertion response with HR and blood lactate [53] and lower motivation [54], tests comparing elite and non-elite athletes may differ in the relationship between specific cardiorespiratory parameters and the measured RPE.
The small sample size of this study limits the generalisation of the conclusions. further studies are required to better assess how RPE is determined by variables such as HR, Rf, VE and aVE. Training specificity is a well-established construct that highlights that real-world experience might differ from the lab conditions. Most of the participants were recreational impact sports players and not solely focussed on running. Furthermore, data from the outdoor familiarisation session using a different metabolic cart conducted by this group found higher VO2Max values (see beeptest data in Online Resource 1). This resulted in a different relationship between the respiration data and RPE, which could reduce the significance of HR. In this unpublished data, the r between RPE and VE was 0.914, RPE and aVE was 0.921 and RPE and Rf was 0.843. This outdoors test did not include heart rate monitor, which limits the generalisation of its results and does not allow for combined analysis with the treadmill tests. Yet, it further indicates the potential that respiratory parameters can have in estimating RPE as observed by Nicolo et al. [33]. Moreover, it might indicate that these parameters play an even more significant role during on-field applications. More real-world examination of RPE and cardiorespiratory parameters is needed to uncover how they operate in field-specific conditions.
It is speculated that aVE has a significant correlation with RPE due to the association between VE and physical stressors. We have shown that aVE has a higher RPE correlation than Rf and HR and a comparable one to VE. From examining the boxplots in Fig. 2, it can be noted the aVE has a higher variance than VE for similar RPE levels.
The oral-cavity device was able to capture both oral and nasopharyngeal breathing with high quality. We were able to observe a range of breathing effort levels, from the most subtle breathing (below 15 breaths per minute) through to rapid breathing (above 60 breaths per minute). Preliminary analysis performed indicate that nasopharyngeal is still clearly detectable due to the proximity to the emitting source of the sound. We speculate that nasopharyngeal breathing results in lower audio intensities and consequentially lower aVE. Since this breathing mode is only possible at lower RPE levels, aVE would still be suitable to track RPE. Nevertheless, further studies are required to further investigate the effects of nasopharyngeal in the data. Future work on optimising the signal-to-noise ratio will further increase the potential of the device to capture breathing data and of aVE as a useful metric in identifying fatigue from athletes. There is potential to the continued improvement of the mechanical design of the oral-based monitoring system through miniaturising and improved comfort. It is important to highlight, unlike metabolic variables, aVE, in theory, only requires the capture and processing of respiration audio. As a proof-of-concept, Rf from the metabolic cart was used in this study. Future development is needed to improve signal processing and obtain an Rf from the captured audio data as accurate as from the metabolic carts. Once this step is achieved, the oral-based monitoring system can be used alone in scenarios where other measurements are inaccessible, such as on-field data collection in real sports scenarios.
5 Conclusions
This study investigated the relationship between cardiorespiratory measurements and RPE during running and evaluated if parameters obtained from inexpensive, wearable monitors could be used to estimate RPE. It introduces a novel metric (aVE) that has a strong association with RPE and can potentially be used as a metric when the use of portable metabolic carts is not viable. More importantly, this study provides support for the possibility to move continuous and objective monitoring of RPE away from the lab and puts it on the field. This will create an opportunity to better understand player welfare and performance under real-world conditions that relate to the specificity of the physical activity performed.
References
Abbiss CR, Laursen PB (2005) Models to explain fatigue during prolonged endurance cycling. Sport Med 35(10):865–898
Van Cutsem J, Marcora S, De Pauw K, Bailey S, Meeusen R, Roelands B (2017) The effects of mental fatigue on physical performance: a systematic review. Sport Med 47(8):1569–1588. https://doi.org/10.1007/s40279-016-0672-0
Stokes K (2006) Skeletal muscle: from molecules to movement. Br J Sports Med 40(11):950. https://doi.org/10.1136/bjsm.2006.026567
Bergmann JHM, Smith ICH, Mayagoitia RE (2012) Using a body sensor network to measure the effect of fatigue on stair climbing performance. Physiol Meas 33(2):287–296. https://doi.org/10.1088/0967-3334/33/2/287
Halson SL (2014) Monitoring training load to understand fatigue in athletes. Sport Med 44:139–147. https://doi.org/10.1007/s40279-014-0253-z
Meeusen R et al (2013) Prevention, diagnosis, and treatment of the overtraining syndrome: joint consensus statement of the European college of sport science and the American college of sports medicine. Med Sci Sports Exerc 45(1):186–205. https://doi.org/10.1249/MSS.0b013e318279a10a
Johnston RD, Gabbett TJ, Jenkins DG (2013) Influence of an intensified competition on fatigue and match performance in junior rugby league players. J Sci Med Sport 16(5):460–465. https://doi.org/10.1016/j.jsams.2012.10.009
Slobounov S (2008) Fatigue-related injuries in athletes. Injuries in athletics: causes and consequences. Springer, pp 77–95
Woods C, Hawkins R, Hulse M, Hodson A (2002) The football association medical research programme: an audit of injuries in professional football—analysis of preseason injuries. Br J Sports Med 36(6):436–441. https://doi.org/10.1136/bjsm.36.6.436
Ekstrand J, Hägglund M, Waldén M (2011) Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med 45(7):553–558. https://doi.org/10.1136/bjsm.2009.060582
Jones CM, Griffiths PC, Mellalieu SD (2017) Training load and fatigue marker associations with injury and illness: a systematic review of longitudinal studies. Sports Med 47(5):943–974
Borresen J, Lambert MI (2009) The quantification of training load, the training response and the effect on performance. Sport Med 39(9):779–795. https://doi.org/10.2165/11317780-000000000-00000
Impellizzeri FM, Rampinini E, Marcora SM (2005) Physiological assessment of aerobic training in soccer. J Sports Sci 23(6):583–592. https://doi.org/10.1080/02640410400021278
Scott TJ, Black CR, Quinn J, Coutts AJ (2013) Validity and reliability of the session-RPE method for quantifying training in Australian football. J Strength Cond Res 27(1):270–276. https://doi.org/10.1519/JSC.0b013e3182541d2e
Grant S et al (1999) A comparison of the reproducibility and the sensitivity to change of visual analogue scales, Borg scales, and likert scales in normal subjects during submaximal exercise. Chest 116(5):1208–1217. https://doi.org/10.1378/chest.116.5.1208
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sport Exerc 14(5):377–381
Borg G (1990) Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health 16(SUPPL. 1):55–58. https://doi.org/10.5271/sjweh.1815
Au JS, De Zepetnek JOT, MacDonald MJ (2017) Modeling perceived exertion during graded arm cycling exercise in spinal cord injury. Med Sci Sport Exerc 49(6):1190–1196. https://doi.org/10.1249/MSS.0000000000001203
Gallo T, Cormack S, Gabbett T, Williams M, Lorenzen C (2015) Characteristics impacting on session rating of perceived exertion training load in Australian footballers. J Sports Sci 33(5):467–475. https://doi.org/10.1080/02640414.2014.947311
Nicolò A, Passfield L, Sacchetti M (2016) Investigating the effect of exercise duration on functional and biochemical perturbations in the human heart: total work or ‘isoeffort’ matching? J Physiol 594(11):3157–3158. https://doi.org/10.1113/JP272421
Nicolò A, Massaroni C, Passfield L (2017) Respiratory frequency during exercise: the neglected physiological measure. Front Physiol 8:1–8. https://doi.org/10.3389/fphys.2017.00922
Riebe D, Ehrman JK, Liguori G, Magal M (eds) (2018) ACSM’s guidelines for exercise testing and prescription, 10th edn. Wolters Kluwer, Philadelphia
Mauger AR, Huntley T, Fletcher IM (2014) RPE-derived work rates can be accurately produced without external feedback or reference to the RPE scale. Percept Mot Skills 118(2):507–521. https://doi.org/10.2466/27.06.PMS.118k19w7
Soriano-Maldonado A, Romero L, Femia P, Roero C, Ruiz JR, Gutierrez A (2014) A learning protocol improves the validity of the Borg 6–20 RPE scale during indoor cycling. Int J Sports Med 35(5):379–384. https://doi.org/10.1055/s-0033-1353166
Macpherson TW, McLaren SJ, Gregson W, Lolli L, Drust B, Weston M (2019) Using differential ratings of perceived exertion to assess agreement between coach and player perceptions of soccer training intensity: an exploratory investigation. J Sports Sci 37(24):2783–2788. https://doi.org/10.1080/02640414.2019.1653423
Murphy AP, Duffield R, Kellett A, Reid M (2014) Comparison of athlete-coach perceptions of internal and external load markers for elite junior tennis training. Int J Sports Physiol Perform 9(5):751–756. https://doi.org/10.1123/ijspp2013-0364
Massaroni C, Nicolò A, Lo Presti D, Sacchetti M, Silvestri S, Schena E (2019) Contact-based methods for measuring respiratory rate. Sensors 19(4):1–47. https://doi.org/10.3390/s19040908
Buchheit M (2014) Monitoring training status with HR measures: do all roads lead to Rome? Front Physiol 5(February):1–19. https://doi.org/10.3389/fphys.2014.00073
Taffoni F, Rivera D, La Camera A, Nicolò A, Velasco JR, Massaroni C (2018) A wearable system for real-time continuous monitoring of physical activity. J Healthc Eng. https://doi.org/10.1155/2018/1878354
Tipton MJ, Harper A, Paton JFR, Costello JT (2017) The human ventilatory response to stress: rate or depth? J Physiol 595(17):5729–5752. https://doi.org/10.1113/JP274596
Sheel AW, Romer LM (2012) Ventilation and respiratory mechanics. Compr Physiol 2(April):1093–1142. https://doi.org/10.1002/cphy.100046
Nicolò A, Marcora SM, Bazzucchi I, Sacchetti M (2017) Differential control of respiratory frequency and tidal volume during high-intensity interval training. Exp Physiol 102(8):934–949. https://doi.org/10.1113/EP086352
Nicolò A, Montini M, Girardi M, Felici F, Bazzucchi I, Sacchetti M (2020) Respiratory frequency as a marker of physical effort during high-intensity interval training in soccer players. Int J Sports Physiol Perform 15(1):73–80. https://doi.org/10.1123/ijspp.2019-0028
Smekal G et al (2001) A physiological profile of tennis match play. Med Sci Sports Exerc 33(6):999–1005. https://doi.org/10.1097/00005768-200106000-00020
Kolimechkov S (2017) Physical fitness assessment in children and adolescents: a systematic review. Eur J Phys Educ Sport Sci 3(4):65–78. https://doi.org/10.5281/zenodo.495725
Foster C et al (2001) A new approach to monitoring exercise training. J Strength Cond Res 15(1):109–115. https://doi.org/10.1519/00124278-200102000-00019
Dafna E, Rosenwein T, Tarasiuk A, Zigel Y (2015) Breathing rate estimation during sleep using audio signal analysis. In: 37th annual international conference of the IEEE engineering in medicine and biology society (EMBC), vol. 2015. IEEE. pp 5981–5984. https://doi.org/10.1109/EMBC.2015.7319754
Ruinskiy D, Lavner Y (2006) An algorithm for accurate breath detection in speech and song signals. In: IEEE 24th convention of electrical & electronics engineers in Israel, no. 1. IEEE. pp 315–319. https://doi.org/10.1109/EEEI.2006.321091
Igras M, Ziolko B (2013) Wavelet method for breath detection in audio signals. In: IEEE international conference on multimedia and expo (ICME). IEEE. pp 1–6. https://doi.org/10.1109/ICME.2013.6607428
Nam Y, Reyes BA, Chon KH (2016) Estimation of respiratory rates using the built-in microphone of a smartphone or headset. IEEE J Biomed Health Inform 20(6):1493–1501. https://doi.org/10.1109/JBHI.2015.2480838
Castro J, Marti-Puig P (2015) Real-time identification of respiratory movements through a microphone. ADCAIJ Adv Distrib Comput Artif Intell J 3(3):64. https://doi.org/10.14201/adcaij2012116475
Lamarra N, Whipp BJ, Ward SA, Wasserman K (1987) Effect of interbreath fluctuations on characterizing exercise gas exchange kinetics. J Appl Physiol 62(5):2003–2012. https://doi.org/10.1152/jappl.1987.62.5.2003
Sciences H, Bland JM, Altman DG (1995) Statistics notes: calculating correlation coefficients with repeated observations: Part 1—correlation within subjects. Br Med J 310(February):446
Nicolò A, Marcora SM, Sacchetti M (2016) Respiratory frequency is strongly associated with perceived exertion during time trials of different duration. J Sports Sci 34(13):1199–1206. https://doi.org/10.1080/02640414.2015.1102315
Nicolò A, Girardi M, Bazzucchi I, Felici F, Sacchetti M (2018) Respiratory frequency and tidal volume during exercise: differential control and unbalanced interdependence. Physiol Rep 6(21):1–17. https://doi.org/10.14814/phy2.13908
Zinoubi B, Zbidi S, Vandewalle H, Chamari K, Driss T (2018) Relationships between rating of perceived exertion, heart rate and blood lactate during continuous and alternated-intensity cycling exercises. Biol Sport 35(1):29–37. https://doi.org/10.5114/biolsport.2018.70749
Kennett DC, Kempton T, Coutts AJ (2012) Factors affecting exercise intensity in rugby-specific small-sided games. J Strength Cond Res 26(8):2037–2042
Day ML, McGuigan MR, Brice G, Foster C (2004) Monitoring resistance training using the session RPE scale. J strength Cond Res 18(2):353–358
Clarke N, Farthing JP, Norris SR, Arnold BE, Lanovaz JL (2018) Quantification of training load in Canadian football: application of session-RPE in collision-based team sports. J Strength Cond Res 27(8):2198–2205
Impellizzeri FM, Rampinini E, Coutts AJ, Sassi A, Marcora SM (2004) Use of RPE-based training load in soccer. Med Sci Sports Exerc 36(6):1042–1047. https://doi.org/10.1249/01.MSS.0000128199.23901.2F
Nicolò A, Massaroni C, Schena E, Sacchetti M (2020) The importance of respiratory rate monitoring: from healthcare to sport and exercise. Sensors 20(21):1–45. https://doi.org/10.3390/s20216396
Schapschröer M, Lemez S, Baker J, Schorer J (2016) Physical load affects perceptual-cognitive performance of skilled athletes: a systematic review. Sport Med Open 2(1):1–16. https://doi.org/10.1186/s40798-016-0061-0
Kovářová L, Pánek D, Kovář K, Hlinčík Z (2015) Relationship between subjectively perceived exertion and objective loading in trained athletes and non-athletes. J Phys Educ Sport 15(2):186–193. https://doi.org/10.7752/jpes.2015.02029
Halldorsson V, Helgason A, Thorlindsson T (2012) Attitudes, commitment and motivation amongst Icelandic elite athletes. Int J Sport Psychol 43(3):241–254
Acknowledgements
The authors would like to thank Thomas Phillips from Oxford Brookes University for his contribution of ideas towards the experimental protocol. This project was funded by the EPSRC Impact Acceleration Grant EP/R511742/1.
Funding
This project was funded by the EPSRC Impact Acceleration Grant EP/R511742/1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors would like to thank Thomas Phillips from Oxford Brookes University for his contribution of ideas towards the experimental protocol. This project was funded by the EPSRC Impact Acceleration Grant EP/R511742/1. The authors have no conflict of interest to declare. The results of this study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12283_2021_346_MOESM1_ESM.xlsx
Supplementary file 1 This spreadsheet contains the pre-processed data that was used in this study. Each tab of the spreadsheet contains data from a participant perform a 20 m multi-stage fitness test (beeptest), VO2Max, time-to-exhaustion (TTE) or Interval test. Each sheet contains the timestamps, with the corresponding RPE level, HR, Rf, VT, VE, VO2 and aVE. (XLSX 145 KB)
12283_2021_346_MOESM2_ESM.xlsx
Supplementary file 2 This spreadsheet contains the model parameters of the generalized linear model and Spearman correlation used in this report. For the generalized linear model, a range of models were listed. Information including the dataset used to generate each model, the relevant cardiorespiratory parameter that are relevant for that model, the model used, and the corresponding adjusted R2, the Akaike’s Information Criteria, the root mean squared error, and the normalized root mean squared error. (XLSX 18 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Almeida e Bueno, L., Kwong, M.T., Milnthorpe, W.R.F. et al. Applying ubiquitous sensing to estimate perceived exertion based on cardiorespiratory features. Sports Eng 24, 9 (2021). https://doi.org/10.1007/s12283-021-00346-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s12283-021-00346-1