Abstract
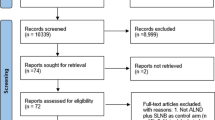
Various surgical energy devices are used for axillary lymph-node dissection. However, those that reduce seroma during axillary lymph-node dissection are unknown. We aimed to determine the best surgical energy device for reducing seroma by performing a network meta-analysis to synthesize the current evidence on the effectiveness of surgical energy devices for axillary node dissection for breast cancer patients. We searched MEDLINE, Embase, CENTRAL, ClinicalTrials.gov, and World Health Organization International Clinical Trials Platform Search Portal. Two reviewers independently selected randomized controlled trials (RCTs) comparing electrosurgical bipolar vessel sealing (EBVS), ultrasonic coagulation shears (UCS), and conventional techniques for axillary node dissection. Primary outcomes were seroma, drained fluid volume (mL), and drainage duration (days). We analyzed random-effects and Bayesian network meta-analyses. We evaluated the confidence of each outcome using the CINeMA tool. We registered with PROSPERO (CRD42022335434). We included 34 RCTs with 2916 participants. Compared to the conventional techniques, UCS likely reduces seroma (risk ratio [RR], 0.61; 95% credible interval [CrI], 0.49–0.73), the drained fluid volume (mean difference [MD], − 313 mL; 95% CrI − 496 to − 130), and drainage duration (MD − 1.79 days; 95% CrI − 2.91 to − 0.66). EBVS might have little effect on seroma, the drained fluid volume, and drainage duration compared to conventional techniques. UCS likely reduce seroma (RR 0.44; 95% CrI 0.28–0.69) compared to EBVS. Confidence levels were low to moderate. In conclusion, UCS are likely the best surgical energy device for seroma reduction during axillary node dissection for breast cancer patients.




Similar content being viewed by others
Data availability
The datasets analyzed in this study are available from the corresponding author (J. Watanabe, m06105jw@jichi.ac.jp) upon reasonable request.
References
American Cancer Society. Breast cancer facts and figures. [cited 2022 November 18]. Available from: https://www.cancer.org/research/cancer-facts-statistics/breast-cancer-facts-figures.html
Gradishar WJ, Anderson BO, Abraham J, Aft R, Agnese D, Allison KH, et al. Breast Cancer, Version 3.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2020;18:452–78.
Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, André F, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol. 2020;31:1623–49.
Morrow M, Strom EA, Bassett LW, Dershaw DD, Fowble B, Giuliano A, et al. Standard for breast conservation therapy in the management of invasive breast carcinoma. CA Cancer J Clin. 2002;52:277–300.
Shima H, Kutomi G, Sato K, Kuga Y, Wada A, Satomi F, et al. An optimal timing for removing a drain after breast surgery: a systematic review and meta-analysis. J Surg Res. 2021;267:267–73.
Cheng H, Clymer JW, Sadeghirad B, Ferko NC, Cameron CG, Amaral JF. Performance of Harmonic devices in surgical oncology: an umbrella review of the evidence. World J Surg Oncol. 2018;16:2.
Pergialiotis V, Kontzoglou K, Dimitroulis D, Vlachos D-EG, Routsolias P, Vlachos GD. Electrosurgical bipolar vessel sealing during axillary lymphadenectomy: a systematic review and meta-analysis. Breast Dis. 2015;35:5–11 (content.iospress.com).
Zhang Z, Li L, Pang Y, Li Q, Guo C, Wang Y, et al. Comparison of harmonic scalpel and conventional technique in the surgery for breast cancer: a systematic review and meta-analysis. Indian J Cancer. 2018;55:348–58.
Manouras A, Markogiannakis H, Genetzakis M, Filippakis GM, Lagoudianakis EE, Kafiri G, et al. Modified radical mastectomy with axillary dissection using the electrothermal bipolar vessel sealing system. Arch Surg. 2008;143:575–80. (discussion 581).
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Citationchaser. [cited 2022 November 18]. Available from: https://estech.shinyapps.io/citationchaser/?fbclid=IwAR0m29-j74QVVZ7iedxcd7xAARlTYFjvwkkXdMTNPeYP7d_wPvIYNYdVCAk
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019:l4898.
Higgins JPT TJ. Cochrane handbook for systematic reviews of interventions Version 6.3.2022. [cited 2022 November 18]. Available from: https://training.cochrane.org/handbook/current
Salanti G, Ades AE, Ioannidis JPA. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64:163–71.
Owen RK, Bradbury N, Xin Y, Cooper N, Sutton A. MetaInsight: an interactive web-based tool for analyzing, interrogating, and visualizing network meta-analyses using R-shiny and netmeta. Res Synth Methods. 2019;10:569–81.
Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JPT. Evaluating the quality of evidence from a network meta-analysis. PLoS ONE. 2014;9: e99682.
Böhm D, Kubitza A, Lebrecht A, Schmidt M, Gerhold-Ay A, Battista M, et al. Prospective randomized comparison of conventional instruments and the Harmonic Focus(®) device in breast-conserving therapy for primary breast cancer. Eur J Surg Oncol. 2012;38:118–24.
CINeMA: Confidence in network meta-analysis. Bern: Institute of Social and Preventive Medicine; 2017 [Internet]. [cited 2022 May 20]. Available from: https://cinema.ispm.unibe.ch/
Nikolakopoulou A, Higgins JPT, Papakonstantinou T, Chaimani A, Del Giovane C, Egger M, et al. CINeMA: an approach for assessing confidence in the results of a network meta-analysis. PLoS Med. 2020;17: e1003082.
Lumachi F, Basso SMM, Santeufemia DA, Bonamini M, Chiara GB. Ultrasonic dissection system technology in breast cancer: a case-control study in a large cohort of patients requiring axillary dissection. Breast Cancer Res Treat. 2013;142:399–404.
Khaled I, Saad I, Soliman H, Faisal M. Intraoperative and postoperative outcomes of Harmonic Focus versus monopolar electrocautery after neoadjuvant chemotherapy in breast conservative surgery: a comparative study. World J Surg Oncol. 2021;19:325.
Hahl J. Contact Nd-YAG laser in mastectomy and axillary evacuation: a prospective randomized study. Lasers Med Sci. 1991;6:205–8 (Springer Science and Business Media LLC).
Kriwanek S, Armbruster C, Blauensteiner W, Dinstl K, Schemper M. Results of a controlled study of CO2 laser vs conventional technique in breast cancer. Lasers Med Sci. 1993;8:133–9 (Springer Science and Business Media LLC).
Wyman A, Rogers K. Randomized trial of laser scalpel for modified radical mastectomy. Br J Surg. 1993;80:871–3.
Zafar S, Khan MA, Rafiq U, Mahmood N. ComparisonoOf axillary drain output in conventional and advanced compressive energy source like ultrasonic scalpel and Ligasure dissection of axilla in breast cancer surgery. J Ayub Med Coll Abbottabad. 2021;33:431–6.
Lumachi F, Burelli P, Basso SMM, Iacobone M, Ermani M. Usefulness of ultrasound scissors in reducing serous drainage after axillary dissection for breast cancer: a prospective randomized clinical study. Am Surg. 2004;70:80–4.
Abul Nagah, Tarek, Lotfy. Comparative study between using harmonic scalpel and electrocautery in modified radical mastectomy. Bioceram Dev Appl. researchgate.net; 2007; Available from: https://www.researchgate.net/profile/Galal-Abulnagah/publication/268005631_COMPARATIVE_STUDY_BETWEEN_USING_HARMONIC_SCALPEL_AND_ELECTROCAUTERY_IN_MODIFIED_RADICAL_MASTECTOMY/links/55bc878a08ae092e9660c070/COMPARATIVE-STUDY-BETWEEN-USING-HARMONIC-SCALPEL-AND-ELECTROCAUTERY-IN-MODIFIED-RADICAL-MASTECTOMY.pdf
Antonio M, Pietra T, Domenico LG, Massimo D, Ignazio R, Antonio N, et al. Does LigaSureTM reduce fluid drainage in axillary dissection? A randomized prospective clinical trial. Ecancermedicalscience [Internet]. ecancer Global Foundation; 2007 [cited 2022 November 18];1. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3223974/
Kontos M, Kothari A, Hamed H. Effect of harmonic scalpel on seroma formation following surgery for breast cancer: a prospective randomized study. J BUON. 2008;13:223–30.
Khater. Harmonic scalpel as a single instrument in modified radical mastectomy. Is it more cost effective than electrocautery and ligature. Egypt J Surg. researchgate.net; 2010; Available from: https://www.researchgate.net/profile/Ashraf-Khater/publication/228765542_HARMONIC_SCALPEL_AS_A_SINGLE_INSTRUMENT_IN_MODIFIED_RADICAL_MASTECTOMY_IS_IT_MORE_COST_EFFECTIVE_THAN_ELECTROCAUTERY_AND/links/5479f4d20cf2a961e487adf4/HARMONIC-SCALPEL-AS-A-SINGLE-INSTRUMENT-IN-MODIFIED-RADICAL-MASTECTOMY-IS-IT-MORE-COST-EFFECTIVE-THAN-ELECTROCAUTERY-AND.pdf
Kozomara D, Galić G, Brekalo Z, Sutalo N, Kvesić A, Soljić M. A randomised two-way comparison of mastectomy performed using harmonic scalpel or monopolar diathermy. Coll Antropol. 2010;34(Suppl 1):105–12.
Russo AL. Axillary dissection using a new ultrasonic device. EJC Suppl. infona.pl; 2010; Available from: https://www.infona.pl/resource/bwmeta1.element.elsevier-4bd5b6e4-0cdd-336e-918f-7247de25a706
Cortadellas T, Córdoba O, Espinosa-Bravo M, Mendoza-Santin C, Rodríguez-Fernández J, Esgueva A, et al. Electrothermal bipolar vessel sealing system in axillary dissection: a prospective randomized clinical study. Int J Surg Elsevier. 2011;9:636–40.
Ramesh RS, Manjunath S, Shivakumar K, Philip R, Selvan S. Use of ultrasonic shears in patients with breast cancer undergoing axillary dissection-a pilot study. Indian J Surg Oncol. 2011;2:156–8.
Yilmaz KB, Dogan L, Nalbant H, Akinci M, Karaman N, Ozaslan C, et al. Comparing scalpel, electrocautery and ultrasonic dissector effects: the impact on wound complications and pro-inflammatory cytokine levels in wound fluid from mastectomy patients. J Breast Cancer. 2011;14:58–63.
Iovino F, Auriemma PP, Ferraraccio F, Antoniol G, Barbarisi A. Preventing seroma formation after axillary dissection for breast cancer: a randomized clinical trial. Am J Surg. 2012;203:708–14.
He Q, Zhuang D, Zheng L, Fan Z, Zhou P, Zhu J, et al. Harmonic focus versus electrocautery in axillary lymph node dissection for breast cancer: a randomized clinical study. Clin Breast Cancer. 2012;12:454–8.
Nespoli L, Antolini L, Stucchi C, Nespoli A, Valsecchi MG, Gianotti L. Axillary lymphadenectomy for breast cancer. A randomized controlled trial comparing a bipolar vessel sealing system to the conventional technique. Breast. 2012;21:739–45 (Elsevier).
Anlar B, Karaman N, Dogan L, Ozaslan C, Atalay C, Altinok M. The effect of harmonic scalpel, electrocautery, and scalpel use on early wound complications after modified radical mastectomy. Eur Surg. 2013;45:286–90 (Springer Science and Business Media LLC).
Rohaizak M, Khan FJ, Jasmin JS, Mohd Latar NH, Abdullah SSN. Ultracision versus electrocautery in performing modified radical mastectomy and axillary lymph node dissection for breast cancer: a prospective randomized control trial. Med J Malaysia. 2013;68:204–7.
Mori T, Abe H, Kawai Y, Murakami K, Akabori H, Yamaguchi T, et al. Prospective, randomized trial comparing harmonic scalpel and electrocautery in breast surgery. J Clin Orthod Wolters Kluwer. 2013;31:e12014–e12014.
Khan S, Khan S, Chawla T, Murtaza G. Harmonic scalpel versus electrocautery dissection in modified radical mastectomy: a randomized controlled trial. Ann Surg Oncol. 2014;21:808–14.
Manjunath S, Ramesh RS, Shivakumar K, Goel V. Ultrasonic shears versus electrocautery in axillary dissection for breast cancer-a randomized controlled trial. Indian J Surg Oncol. 2014;5:95–8.
Tukenmez M, Agcaoglu O, Aksakal N, Destek S, Cabioglu N, Barbaros U, et al. The use of Ligasure vessel sealing system in axillary dissection; effect on seroma formation. Chirurgia. 2014;109:620–5.
Malik ZI. Axillary dissection in mastectomy: ultracision vs monopolar electrocautry. Age. pjmhsonline.com; 2015; Available from: https://pjmhsonline.com/2015/oct_dec/pdf/1328%20%20%20Axillary%20Dissection%20in%20Mastectomy%20Ultracision%20vs%20Monopolar%20Electrocautry.pdf
Nawaz A, Waqar S, Khan A, Mansoor R, Butt UI, Ayyaz M. Harmonic scalpel versus electrocautery in axillary dissection in carcinoma breast. J Coll Physicians Surg Pak. 2015;25:870–3.
Seki T, Hayashida T, Takahashi M, Jinno H, Kitagawa Y. A randomized controlled study comparing a vessel sealing system with the conventional technique in axillary lymph node dissection for primary breast cancer. Springerplus. Springer; 2016;5:1004.
Militello G, De Marco P, Falco N, Kabhuli K, Mascolino A, Licari L, et al. Is it really useful the harmonic scalpel in axillary dissection for locally advanced breast cancer? A case series G. Chir. 2016;37:262–5.
Mittal P, Kumar A, Kaur S, Pandove PK, Singla RL, Singh J. A comparative study of the use of harmonic scalpel versus unipolar cautery in modified radical mastectomy. Niger J Surg. 2017;23:20–5.
Okamura N. Utility of LigaSure (TM) vessel-sealing device in axillary dissection for breast cancer surgery: a randomized single center study. Res. Assoc Cancer Res. 2017.
Shanmugam S, Govindasamy G, Hussain SA, Rao PSH. Axillary dissection for breast cancer using electrocautery versus ultrasonic dissectors: a prospective randomized study. Indian J Cancer. 2017;54:543–6.
Archana A, Sureshkumar S, Vijayakumar C, Palanivel C. Comparing the harmonic scalpel with electrocautery inreducing postoperative flap necrosis and seroma formation after modified radical mastectomy in carcinoma breast patients: a double-blind prospective randomized control trail. Cureus. 2018;10: e2476.
Faisal M, Fathy H, Shaban H, Abuelela ST, Marie A, Khaled I. A novel technique of harmonic tissue dissection reduces seroma formation after modified radical mastectomy compared to conventional electrocautery: a single-blind randomized controlled trial. Patient Saf Surg. 2018;12:8.
Salama AMF, Nawar AM, Zayed ME, Essa MS. Evaluation of ultrasonic axillary dissection in preservation of intercostobrachial nerve and lymphatic sealing in breast cancer patients: randomized controlled trial. Ann Med Surg (Lond). 2020;60:255–60.
Shaukat A, Anjum MA. Comparison of axillary lymph node dissection by using ligasure vessel sealing system vs conventional thread ligation in patients undergoing modified radical mastectomy for carcinoma of breast. Ann Punjab Med Coll (APMC). 2020;14:254–8 (apmcfmu.com).
Deori A, Gupta N, Gupta AK, Yelamanchi R, Agrawal H, Durga CK. A prospective randomised controlled study comparing ultrasonic dissector with electrocautery for axillary dissection in patients of carcinoma breast. Malays J Med Sci. 2021;28:97–104.
Park HS, Lee J, Kim JY, Park JM, Kwon Y. A prospective randomized study to compare postoperative drainage after mastectomy using electrosurgical bipolar systems and conventional electro-cautery. J Breast Cancer. 2022;25:307–17.
Zahid A, Javed T, Kaleem M, Andrabi WI, Jamil T, Qureshi SS, et al. Comparison of seroma formation with harmonic scalpel versus monopolar electrocautery in axillary dissection following modified radical mastectomy. Pak J Med Health Sci. 2022;16:198–198 (pjmhsonline.com).
Adrien C, Katia M, Marie-Lucile B, Alice R, Claire B, Roman R. Prevention of lymphocele or seroma after mastectomy and axillary lymphadenectomy for breast cancer: systematic review and meta-analysis. Sci Rep. 2022;12:10016.
Konishi T, Fujiogi M, Niwa T, Morita K, Matsui H, Fushimi K, et al. Comparison of outcomes after differentiated thyroid cancer surgery performed with and without energy devices: a population-based cohort study using a nationwide database in Japan. Int J Surg. 2020;77:198–204.
Piemontese A, Galvain T, Swindells L, Parago V, Tommaselli G, Jamous N. Budget impact analysis of HARMONIC FOCUS™+ Shears for mastectomy and breast-conserving surgery with axillary lymph node dissection compared with monopolar electrocautery from an Italian hospital perspective. PLoS ONE. 2022;17: e0268708.
Xue DQ, Qian C, Yang L, Wang XF. Risk factors for surgical site infections after breast surgery: a systematic review and meta-analysis. Eur J Surg Oncol. 2012;38:375–81.
Douay N, Akerman G, Clément D, Malartic C, Morel O, Barranger E. Seroma after axillary lymph node dissection in breast cancer. Gynecol Obstet Fertil. 2008;36:130–5.
Robertson SA, Rusby JE, Cutress RI. Determinants of optimal mastectomy skin flap thickness. Br J Surg. 2014;101:899–911.
Kuroi K, Shimozuma K, Taguchi T, Imai H, Yamashiro H, Ohsumi S, et al. Pathophysiology of seroma in breast cancer. Breast Cancer. 2005;12:288–93.
Acknowledgements
The authors would like to thank Dr. Ahmed M. F. Salama, Dr. Mohammed Faisal, Dr. Subbiah Shanmugam, and Dr. Okamura for providing us with details of their study.
Funding
This study received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, JW and YK; methodology, JW, YK, AK, AM, MS, MS, MH, JK, and NS; software, JW and YK; validation, JW, YK, AK, AM, and SM; formal analysis, JW and YK; investigation, JW, YK, AK, AM, MS, MS, MH, JK, and NS; resources, JW, data curation, JW, YK, AK, and AM; writing—original draft preparation, JW; writing—review and editing, YK, AK, AM, MS, MS, MH, JK, and NS; visualization, JW and YK; supervision, MS, MS, MH, JK, and NS; project administration, JW, YK, JK, and NS; funding acquisition, JW All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Watanabe, J., Kataoka, Y., Koike, A. et al. Efficacy and safety of surgical energy devices for axillary node dissection: a systematic review and network meta-analysis. Breast Cancer 30, 531–540 (2023). https://doi.org/10.1007/s12282-023-01460-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-023-01460-7