Abstract
Purpose of Review
IA (invasive aspergillosis) caused by azole-resistant strains has been associated with higher clinical burden and mortality rates. We review the current epidemiology, diagnostic, and therapeutic strategies of this clinical entity, with a special focus on patients with hematologic malignancies.
Recent Findings
There is an increase of azole resistance in Aspergillus spp. worldwide, probably due to environmental pressure and the increase of long-term azole prophylaxis and treatment in immunocompromised patients (e.g., in hematopoietic stem cell transplant recipients). The therapeutic approaches are challenging, due to multidrug-resistant strains, drug interactions, side effects, and patient-related conditions.
Summary
Rapid recognition of resistant Aspergillus spp. strains is fundamental to initiate an appropriate antifungal regimen, above all for allogeneic hematopoietic cell transplantation recipients. Clearly, more studies are needed in order to better understand the resistance mechanisms and optimize the diagnostic methods to identify Aspergillus spp. resistance to the existing antifungal agents/classes. More data on the susceptibility profile of Aspergillus spp. against the new classes of antifungal agents may allow for better treatment options and improved clinical outcomes in the coming years. In the meantime, continuous surveillance studies to monitor the prevalence of environmental and patient prevalence of azole resistance among Aspergillus spp. is absolutely crucial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The mold Aspergillus spp. was identified by an Italian priest Micheli in 1729, who named it after the shape of an Aspergillum (sprinkler of holy water) [1]. The classification of this mold is quite challenging. Since many informal classifications with no international consensus in the last years were proposed, such as “species complexes “ or “cryptic species,” the use of the classical taxonomy according to their morphology and phylogenetic relationships (6 subgenera, 27 sections, and 87 series) seems to be more reasonable [2, 3, 4]. Invasive aspergillosis (IA) is the most common invasive fungal disease (IFD) caused primarily by A. fumigatus, followed by A. flavus, A. terreus, and A. niger. [5] Prolonged neutropenia, hematopoietic cell transplantation (HCT), intensive chemotherapy, graft-versus-host disease (GVHD), and high-dose corticosteroids are classical risk factors for IA [6]. In the last decades, the development of new therapies, such as inhibitors of tyrosine kinase (e.g. ibrutinib) or Janus-kinase, checkpoint-inhibitors, and CAR-modified T-cells (due to the use of steroids and tocilizumab for the prevention of cytokine release syndrome), has also been associated with higher risk for IA [7, 8, 9]. Among solid organ transplant (SOT), lung transplant recipients have the highest risk of IA. [10, 11]
Furthermore, patients in the intensive care unit patients or infected with SARS-CoV-2 and patients with advanced liver cirrhosis or under long systemic corticosteroid therapy are also at risk for IA. [12, 13, 14]
Considering the increasing number of patient populations at risk for IA, higher numbers of patients are exposed to broad-spectrum azoles, such as voriconazole, posaconazole, or isavuconazole, either as prophylaxis or treatment [15, 16, 17, 18, 19]. However, prolonged and expanded use of broad-spectrum azoles in clinical practice, as well as in the environment, might have contributed to an important increase in azole resistance worldwide [20, 21]. Azole-resistant Aspergillus strains have been associated with therapeutic failure and mortality rates as high as 90% [22]. In this article, we review the current trends in the epidemiology and clinical impact of antifungal-resistant Aspergillus spp.
Epidemiology of Azole-Resistant A. fumigatus
Azole-resistant A. fumigatus (ARAF) strains caused by the mutations TR34/L98H or TR46/Y121F/T289A have been reported worldwide [23]. The first case of ARAF was reported in the late 1980s in the Netherlands, and since then, increased rates of azole resistance have been reported in all continents, except for Antarctica (Fig. 1) [24]. Due to variability in agricultural use of azole-containing pesticides, scarce routine surveillance programs, and limited availability of routine susceptibility testing, there is a lack of relevant, detailed epidemiological data [25]. This could explain, in part, the enormous variability of ARAF prevalence in different countries [26]. The SCARE-Network, a multicenter study from 22 centers (19 European and 4 non-European sites), showed an overall ARAF-prevalence of 3.2% (ranging from 0 to 26%), with the predominance of the mutation TR34/L98H between 2009 and 2011 [26]. The Netherlands have reported one of the highest ARAF-prevalence in Europe, with a significant increase from 1.7–6% in the period 1997–2007 to 8–15% between 2013 and 2018 (TR34/L98H and TR46/Y121F/T289A mutations accounting for most cases) [27, 28]. In Denmark, ARAF prevalence was reported to be 6.1%, based on a national surveillance program between 2018 and 2020 [29]. A Belgian one-year retrospective multicenter study showed an ARAF prevalence of 5.5% [30]. In Spain, the estimated prevalence is between 1.2 and 6.6% [31, 32]. Study groups from Germany and Italy reported similar rates of azole-resistant A. fumigatus in cystic fibrosis patients, as well as in patients with hematological malignancies, 5.3–9 and 1.1–1.3%, respectively. [33, 34, 35, 36] Lazzarini et al. showed an azole resistance prevalence of 6.25% in Italian clinical samples [37]. Similarly, in France ARAF has been reported in 0.85% of hematological malignancy patients and 1.8% in the general population [38, 39]. In Portugal, Poland, and Turkey, the resistance rates in clinical isolates and samples were 2.6, 4.1, and 3.3% respectively. [40, 41, 42] Environmental isolates were reported to be azole resistant in 6% of cases in the UK and 1% of cases in Greece [43, 44]. In Switzerland, the TR34/L98H mutation was first reported in 2018, in environmental A. fumigatus strains initially, and later in two patients with cystic fibrosis [45]. Based on a recently published surveillance study on ARAF in clinical samples in Switzerland, ARAF prevalence was found to be about 1.1%. [46]
In the USA, the first reported TR34/L98H mutation was reported in 2016 [47]. Between 2015 and 2017 a passive surveillance program showed an ARAF prevalence of 1.4% [48]. Canada seems to have for the moment low rates of azole resistance, with a prevalence in clinical samples of 0.2%. In contrast, in Latin America, data are scarce. A Peruvian prospective cohort study in patients with chronic pulmonary aspergillosis showed a resistance prevalence of 2%, and a 1% resistance prevalence was recently reported in Brazil [49, 50]. Environmental isolates from Colombia showed a resistance prevalence of 9.3% [51]. In Mexico and Argentina, recent studies reported a resistance prevalence of 4.7% and 14%, respectively. [52, 53] In the African continent, data are also limited. Some data are suggesting ARAF prevalence of 1.3% in clinical samples and up to 17.1% in the environmental setting [54]. Resistance prevalence in Vietnam (environmental samples), Iran (environmental samples), China, Taiwan, Pakistan, Thailand, Japan, and India were 65, 18, 4.4, 7.5, 6.6, 3.2, 2.9, and 4.3%, respectively. [22, 23, 55, 56, 57, 58, 59, 60, 61, 62] In Australia, only 2% of clinical isolates of A. fumigatus were reported to be azole resistant [63]. In South Korea, no resistance strains were found until 2015. [64]
Resistance in Aspergillus fumigatus “Cryptic” Species
The section A. fumigatus includes “cryptic” species causing IA, albeit associated with higher mortality rates [65]. “Cryptic” species are probably underestimated, since the conventional diagnostic methods are not often able to recognize them, and only DNA sequencing permits accurate identification and classification. The resistance mechanisms and specific mutations are mostly still unknown for these species, but there are some homologies with A. fumigatus. [65] The most frequent cryptic A. fumigatus species is A. lentulus, first described in 2004 in allogeneic HCT recipients [66]. It is mostly found in immunocompromised patients with hematological disease, SOT recipients or patients treated with high-dose systemic corticosteroids [67]. Although A. lentulus represents < 3% of all A. fumigatus spp. in clinical specimens, it could account for 10–30% of misidentified/sub-categorized ARAF [65, 68]. Mutations in the Cyp51A gene (as for A. fumigatus) are probably responsible for the development of azole resistance in A. lentulus. [69] Since this species has a low susceptibility to multiple antifungals, including azoles and echinocandins, treatment options are often limited [68]. A. (Neosartorya)udagawae, isolated for the first time in 1995, accounts only for a small percentage of IA cases but, as A. lentulus, is often resistant to voriconazole and amphotericin B [65, 70]. Other rare “cryptic” species in the section fumigatus include A. viridinutans/felis and A. fischeri/thermomutatus. [65]
Epidemiology of Azole-Resistant Non-fumigatus Aspergillus Species
A large Spanish study showed a high prevalence of non-fumigatus species in clinical samples (A. fumigatus accounted for less than 50%) [31]. Overall, A. flavus, A. terreus, A. tubigensis, A. niger, and A. nidulans represented 8.4, 8.1, 6.8, 6.5, and 2.5%, respectively, of all clinical samples in this population-based survey [31]. On the contrary, an American study in transplant recipients reported a higher prevalence of A. flavus (13.3%), followed by A. niger (6.0%) and A. terreus (5.0%) [71]. The prevalence of “cryptic” species between all identified Aspergillus sections was of 10% and 12% in the two previously cited studies, respectively. [31, 71] A. flavus is worldwide the second cause of IA after A. fumigatus, with higher prevalence reported in sub- and tropical countries like India, Pakistan, and Sudan [72, 73, 74, 75]. For instance, in India, 47% of all IA in ICU patients with no classical risk factors were caused by A. flavus (39.4% A. fumigatus) [75]. Azole resistance has been rarely reported in A. flavus strains [72]. A. terreus accounts for a minority of IA infections, but with a prevalence as high as 30% among IA cases in specific geographical regions such as Houston, Texas (USA) and Innsbruck, Tyrol (Austria) [76, 77]. Recent epidemiological data from Italy suggest a prevalence of A. terreus in hematological patients of 4.8% [36]. Posaconazole resistance has been found in 13.7% of all A. terreus isolates in Germany, 12.5% in the UK, and 10% in Austria, worldwide. A total of 5.4% of all section Terrei isolates were posaconazole-resistant; voriconazole and itraconazole resistance was rare and mostly found in the “cryptic” species of this section such as A. citrinoterreus and A. alabamensis. [78] Since the MICs for voriconazole (2 microgramm/mL) are higher than posaconazole (0.25 microgramm/mL) for this section, resistance to voriconazole is rare. Azole-resistance is extremely important for this species, due to the limited alternative treatment options for A. terreus, considering the amphotericin-B resistance, which is likely related to drug uptake reduction and higher catalase activity [79]. A. citrinoterreus is reported to be the most common « cryptic» species in the section Terreus (8.4%), followed by A. hortai (2.6%) and A. alabamensis (1.6%) [78]. Azole resistance remains rare in the cryptic species of the Terrei Sect. [78] A. niger is considered to be of lower virulence in comparison to other Aspergillus spp. with incidence in transplant recipients between 0.048 and 0.16%, as reported by the TRANSNET group [80, 81]. A Belgian single-center study has showed a small number (16 cases) of IA caused by A. niger complex over a 7-year period [82]. The “cryptic” species A. tubingensis was responsible for 5 of these cases [82]. A. tubingensis as A. awamori/welwitschiaceae is known to have higher triazole MICs limiting the available treatment options [83]. A. ustus with the “cryptic” species A. calidoustus and A. pseudodeflectus are rare causes of IA, with a recent literature review showing 67 reported cases of probable/proven IA worldwide due to A. ustus complex [84]. Half of these cases were breakthrough IA in patients receiving azole-based antifungal prophylaxis, consistent with other reports suggesting increasing detection of this pathogen in the setting of long-term azole prophylaxis [84, 85]. Since resistance to azole of these species is variable, rates of therapeutic failure and mortality are high [84]. Also, A. nidulans with the “cryptic”species A. sublatus, A. quadrilineatus is a very rare cause of IA, described mostly in patients with the chronic granulomatous disease (estimated to cause 35% of all IA in this patients subgroup), observed in osteomyelitis and in patients receiving itraconazole prophylaxis [86, 87, 88]. Azole resistance is not common in the section A. nidulans. [87]
Mechanisms of Azole and Other Antifungal Resistance
The pathogenesis of azole resistance is complex and multi-factorial. Moreover, most of the studies have been conducted in A. fumigatus, and data are missing for other species. More studies are needed, considering the important clinical burden of these infections [89]. First, single point mutations in the cyp51 gene (mostly amino-acid substitutions in CYP51A, such as G54, G138, M220, G448, L98H, Y121F, and T289A) can reduce the affinity between azoles and their targets [90, 91, 92]. These mutations are often associated with long-term azole administration [22]. For instance, mutations in the cyp51C gene are associated with high voriconazole minimal inhibitory concentrations (MIC) in A. flavus. [93, 94] Furthermore, cyp51A gene mutations may probably be the reason for A. lentulus azole-resistance [65]. Second, tandem repeat mutations of 34 bp (TR34), 46 bp (TR46), or 53 bp (TR53) in the promoter region of A. fumigatus cyp51A or other type of mutations in different genes could possibly induce an overexpression of cyp51, which increases the azole concentrations needed to inhibit fungal growth (since azoles are binding to cyp51 protein in order to block the formation of ergosterol) [95, 96, 97]. This type of mutation is thought to be associated with environmental azole resistance, since the massive use of azole-based fungicides in agriculture could provoke cross-resistance with triazoles [24, 98]. Such mutations have been described in azole-naive, but also in patients on long-term azole treatment, highlighting the complexity of the different types of resistance mechanisms [99]. Finally, multidrug efflux pumps could lead to lower intracellular drug concentrations and azole resistance, although more data are required to better describe this resistance mechanism [97, 100, 101]. Other possible mechanisms include cellular stress response, drug enzymatic degradation, and bio-film formation. [92, 102]
Diagnosis of Azole-Resistance
The diagnosis of azole resistance is based on the phenotypic measurement of MIC, which is the threshold to differentiate a resistant from a susceptible strain. MICs are used together with pharmacokinetic/pharmacodynamic (PK/PD) data to determine the clinical breakpoints (CBPs), which are susceptibility predictors [103, 104, 105]. The gold standard to assess the MIC is the broth microdilution assays standardized by the Clinical and Laboratory Standards Institute (CLSI) or the European Committee on Antimicrobial Susceptibility Testing (EUCAST), which are the two major classification systems used for antimicrobial susceptibility [103, 104, 105]. Of note, EUCAST has established CBPs for different drugs for A. fumigatus, A. flavus, A. nidulans, A. niger, and A. terreus, while CLSI has proposed only voriconazole CBPs for A. fumigatus. [105] Otherwise, CLSI uses epidemiological cut-off values (ECVs) to differentiate among wild-type susceptible and non-wild-type strains, which are not predictors of clinical outcomes [106]. Overall, CLSI and EUCAST recommendations are similar, despite methodological differences [107]. Other complementary phenotypic diagnostic tests include calorimetric endpoint or agar-based methods that use MIC strips. These tests are easier to perform and comparable to the EUCAST/CLSI microdilution standard, but they also need a positive culture. [1, 26]
Genotypic testing for azole resistance is based mostly on PCR methods, targeting directly the most frequent point mutations in the cyp51A gene and its promoter and the tandem repeat insertions [1, 25, 108]. Currently, there are three different commercial kits used in Europe for the genotypic detection of azole resistance [109]. However, not all mutations are reported; hence sensitivity remains low and those PCR assays target only A. fumigatus-related mutations [1]. Pyrosequencing can also be used for detecting resistance, using the detection of light that is released during nucleotide incorporation into the amplifying DNA, but it is not often available [110]. MALDI-TOF could be also used for detecting azole resistance, but data on molds are largely missing [111]. Eventually, whole genome sequencing (WGS) has the highest resolution for detecting mutations in A. fumigatus and could be used for different other species. Due to high costs, long turn-around time, and high-level expertise needed, its utility remains very limited. [1, 112]
Special Clinical Considerations for Hematopoietic Stem Cell Transplant Recipients and Patients with Hematologic Malignancies
The incidence of IA in patients with acute myeloid leukemia or allogeneic HCT recipients has ranged between 5 and 15%. [6, 113, 114]
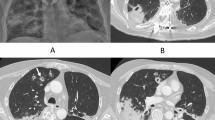
Allogeneic HCT recipients with IA due to azole-resistant Aspergillus spp. present clinically similar to patients infected with non-resistant strains, usually with a pulmonary infection, followed by sinusonasal and cerebral IA [115]. Rapid detection of azole resistance is fundamental, since infections caused by these strains are associated with higher mortality, between 88 and 100% [116, 117, 118]. Comparative studies between azole resistant and susceptible strains of Aspergillus spp. in IA showed a 21–31% higher mortality in the azole resistant group [116, 119]. As already mentioned, phenotypic diagnostic tests that require culture growth often miss “cryptic” species and the rate of culture-positivity varies between different patient groups [120, 121]. Clinical suspicion for resistant Aspergillus spp. should be rapidly raised in the context of a lack of clinical and biological (e.g., persistence of high galactomannan plasmatic levels) response to the administered therapy.
Antifungal Treatment Considerations
The cornerstone of IA treatment is broad-spectrum triazoles, including voriconazole, isavuconazole, and posaconazole [15, 16, 122, 123, 124, 125]. Different factors, such as prior use of azole prophylaxis, local epidemiology of azole-resistance, co-morbidities, site of infection, the severity of clinical presentation, and co-infections with other fungi, may impact the choice of antifungal agent used, particularly before microbiological results become available [6, 126]. For azole-resistant Aspergillus strains, there are no controlled clinical trial data; hence treatment recommendations are based mostly on expert opinion [22]. Latest treatment recommendations suggest avoiding an azole as empirical treatment if the local azole-resistance prevalence is > 10% and consider using either amphotericin-B lipid formulations or a combination of voriconazole with an echinocandin [16, 127, 128, 129]. However, there is a lack of clinical evidence to support this approach, particularly considering that the cut-off of 10% of azole resistance is arbitrary. However, this approach may be justified, considering the lack of availability of rapid molecular diagnostic tools in most centers, which could lead to significant delays in appropriate treatment initiation. If resistance rates are less than 5%, resistance investigation may be warranted only in case of treatment failure; however, with a prevalence between 5 and 10%, routine resistance testing is recommended [13]. The right timing for transition to oral antifungal treatment, when susceptibility testing is not available, is unclear. The European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines strongly recommend for the treatment of voriconazole-resistant (MIC > 2 mg/ml) IA amphotericin-B lipid formulation monotherapy or a combination of voriconazole or isavuconazole with an echinocandin [14]. Even if the MIC of posaconazole is 0.5 mg/l, a possible step-down therapy with oral posaconazole with a targeted plasmatic level > 3.3 mg/l has been suggested as a possible treatment option. [130, 131, 132]
As mentioned above, resistance testing may not always be feasible, because of the lack of culture growth and isolation difficulties for cryptic species in specific patient subgroups. In these cases, diagnosis of possible resistance is predominately based on clinical suspicion and treatment should always be discussed with the local infectious disease team. The “cryptic” species for the section A. fumigatus, such as A. udagawae, A. thermomutatus, and A. lentulus, show high MICs for all azole drugs, and A. lentulus and A. udagawae have higher MICs also for amphotericine-B products [65, 133, 134]. Isavuconazole seems to be active against A. lentulus and A. udagawae, although data are very limited. [63]
Concerning the therapy for non-fumigatus Aspergillus spp., voriconazole is the first-line therapy for A. flavus. [70] Echinocandins could be used in combination with voriconazole or alone when no other treatment options are available in the rare cases of azole resistance [70]. Since posaconazole resistance is common for A. terreus and his “cryptic” species, voriconazole and itraconazole are the preferred antifungal molecules [16, 135]. Liposomal amphotericin-B should be avoided [135]. “Cryptic” species of the A. niger section (example given A. tubigensis) are often resistant to the triazoles; for this reason, liposomal amphotericine B is preferred [136]. The optimal antifungal therapy for A. ustus is still not elucidated due to the absence of clinical trials. ESCMID recommend the use of amphotericin-B products, since often these infections are breakthrough IA under posaconazole or voriconazole prophylaxis [14]. Isavuconazole, which shows lower MICs, could have a potential role in the therapy of this Sect. [137]
New antifungal molecules could play a role in the treatment of azole-resistant IA in the future. For example, ibrexagungerp shows an activity against azole-resistant isolates of A. calidoustus and A. terreus, if used in combination with liposomal amphotericin-B or azole [138]. Rezafungin has displayed some activity against azole-resistant Aspergillus spp. in animal models [139]. Fosmanogepix, VL-2397, and olorofim have also demonstrated a potent activity against azole-resistant strains. 140, 141 While more clinical data are necessary to better define the role of those new molecules in the management of IA due to “cryptic” and azole-resistant Aspergillus spp., the thus far reported MIC data of some of them suggest that they may represent an important tool in the management of those infections.
Conclusions
There is an increase in azole resistance worldwide probably due to environmental phenomena (massive use of azole-containing fungicide in agriculture) and due to the increase of long-term azole prophylaxis and treatment in immunocompromised patients. IA caused by those strains has been associated with higher clinical burden and mortality rates. Rapid recognition of resistant Aspergillus spp. strains is fundamental to initiate an appropriate antifungal regimen in allogeneic HCT recipients and patients with hematologic malignancies. Clearly, more studies are needed in order to better understand the resistance mechanisms and to optimize the diagnostic methods to identify Aspergillus spp. resistance to the existing antifungal agents/classes. Currently, therapeutic approaches are challenging, due to multidrug-resistance strains, drug interactions, side effects, and patient-related conditions. More data on the susceptibility profile of Aspergillus spp. against the new classes of antifungal agents, which are in phase I–III clinical trials, may allow for better treatment options and improved clinical outcomes in the coming years. In the meantime, continuous surveillance studies to monitor the prevalence of environmental and patient prevalence of azole resistance among Aspergillus spp. is absolutely crucial.
References
Arastehfar A et al. Aspergillus fumigatus and aspergillosis: from basics to clinics. Stud Mycol. 2021;100:100115.
Houbraken J, et al. Classification of Aspergillus, Penicillium, Talaromyces and related genera (Eurotiales): an overview of families, genera, subgenera, sections, series and species. Stud Mycol. 2020;95:5–169.
Wiederhold NP, Locke JB, Daruwala P, Bartizal K. Rezafungin (CD101) demonstrates potent in vitro activity against Aspergillus, including azole-resistant Aspergillus fumigatus isolates and cryptic species. J Antimicrob Chemother. 2018;73:3063–7.
dos Santos RAC et al. Genomic and phenotypic heterogeneity of clinical isolates of the human pathogens Aspergillus fumigatus, Aspergillus lentulus, and Aspergillus fumigatiaffinis. Front. Genet. Front Genet. 2020;11:459.
Lass-Flörl C. How to make a fast diagnosis in invasive aspergillosis. Med Mycol. 2019;57:S155–60.
Douglas AP, et al. Consensus guidelines for the diagnosis and management of invasive aspergillosis, 2021. Intern Med J. 2021;51:143–76.
Teh BW, et al. Consensus guidelines for antifungal prophylaxis in haematological malignancy and haemopoietic stem cell transplantation, 2021. Intern Med J. 2021;51:67–88.
Hill JA, et al. Infectious complications of CD19-targeted chimeric antigen receptor–modified T-cell immunotherapy. Blood. 2018;131:121–30.
Ghez D, et al. Early-onset invasive aspergillosis and other fungal infections in patients treated with ibrutinib. Blood. 2018;131:1955–9.
Neofytos D, et al. Epidemiology, outcomes, and mortality predictors of invasive mold infections among transplant recipients: a 10-year, single-center experience. Transpl Infect Dis Off J Transplant Soc. 2013;15:233–42.
Neofytos D, et al. Epidemiology, risk factors and outcomes of invasive aspergillosis in solid organ transplant recipients in the Swiss Transplant Cohort Study. Transpl Infect Dis. 2021;20:e12898.
Bassetti M, et al. Performance of existing definitions and tests for the diagnosis of invasive aspergillosis in critically ill, adult patients: a systematic review with qualitative evidence synthesis. J Infect. 2020;81:131–46.
Koehler P, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis. 2021;21:e149–62.
Prattes J, et al. Invasive aspergillosis in patients with underlying liver cirrhosis: a prospective cohort study. Med Mycol. 2017;55:803–12.
Patterson TF, et al. Practice guidelines for the diagnosis and management of Aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis Off Publ Infect Dis Soc Am. 2016;63:e1–60.
Ullmann AJ, et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect. 2018;24:e1–38.
Ullmann AJ, et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med. 2007;356:335–47.
Cornely OA, et al. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med. 2007;356:348–59.
Dadwal SS, et al. American Society of Transplantation and Cellular Therapy Series, 2: management and prevention of Aspergillosis in hematopoietic cell transplantation recipients. Transplant Cell Ther. 2021;27:201–11.
Hendrickson JA, Hu C, Aitken SL, Beyda N. Antifungal resistance: a concerning trend for the present and future. Curr Infect Dis Rep. 2019;21:47.
Verweij PE, Chowdhary A, Melchers WJG, Meis JF. Azole resistance in Aspergillus fumigatus: can we retain the clinical use of mold-active antifungal azoles? Clin Infect Dis Off Publ Infect Dis Soc Am. 2016;62:362–8.
Chowdhary A, Sharma C, Meis JF. Azole-resistant Aspergillosis: epidemiology, molecular mechanisms, and treatment. J Infect Dis. 2017;216:S436–44.
Burks C, Darby A, Londoño LG, Momany M, Brewer MT. Azole-resistant Aspergillus fumigatus in the environment: identifying key reservoirs and hotspots of antifungal resistance. PLOS Pathog. 2021;17:e1009711.
Garcia-Rubio R, Cuenca-Estrella M, Mellado E. Triazole resistance in Aspergillus species: an emerging problem. Drugs. 2017;77:599–613.
Pasula S, Chandrasekar PH. Azole resistance in Aspergillus species: promising therapeutic options. Expert Opin Pharmacother. 2021;22:2071–8.
van der Linden JWM, et al. Prospective multicenter international surveillance of azole resistance in Aspergillus fumigatus. Emerg Infect Dis. 2015;21:1041–4.
Snelders E, et al. Emergence of azole resistance in Aspergillus fumigatus and spread of a single resistance mechanism. PLOS Med. 2008;5:e219.
Lestrade PPA, et al. Paradoxal trends in azole-resistant Aspergillus fumigatus in a national multicenter surveillance program, the Netherlands, 2013–2018. Emerg Infect Dis. 2020;26:1447.
Risum M, et al. Azole resistance in Aspergillus fumigatus. The first 2-year’s data from the Danish National Surveillance Study, 2018–2020. Mycoses. 2022;65:419–28.
Vermeulen E, et al. Nationwide surveillance of azole resistance in Aspergillus diseases. Antimicrob Agents Chemother. 2015;59:4569–76.
Alastruey-Izquierdo A, et al. Population-based survey of filamentous fungi and antifungal resistance in Spain (FILPOP Study). Antimicrob Agents Chemother. 2013. https://doi.org/10.1128/AAC.00383-13.
Escribano P, et al. Azole resistance survey on clinical Aspergillus fumigatus isolates in Spain. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2021;27(1170):e1-1170.e7.
Seufert R, et al. Prevalence and characterization of azole-resistant Aspergillus fumigatus in patients with cystic fibrosis: a prospective multicentre study in Germany. J Antimicrob Chemother. 2018;73:2047–53.
Steinmann J, et al. Emergence of azole-resistant invasive aspergillosis in HSCT recipients in Germany. J Antimicrob Chemother. 2015;70:1522–6.
Prigitano A, et al. Triazole resistance in Aspergillus fumigatus isolates from patients with cystic fibrosis in Italy. J Cyst Fibros Off J Eur Cyst Fibros Soc. 2017;16:64–9.
Prigitano A, et al. Prospective multicentre study on azole resistance in Aspergillus isolates from surveillance cultures in haematological patients in Italy. J Glob Antimicrob Resist. 2020;22:231–7.
Lazzarini C, et al. Azole resistance in Aspergillus fumigatus clinical Isolates from an Italian culture collection. Antimicrob Agents Chemother. 2015;60:682–5.
Alanio A, et al. Low prevalence of resistance to azoles in Aspergillus fumigatus in a French cohort of patients treated for haematological malignancies. J Antimicrob Chemother. 2011;66:371–4.
Choukri F, et al. Prospective evaluation of azole resistance in Aspergillus fumigatus clinical isolates in France. Med Mycol. 2015;53:593–6.
Pinto E et al. Aspergillus species and Antifungals susceptibility in clinical setting in the north of Portugal: cryptic species and emerging azoles resistance in A. fumigatus. Front Microbiol. 2018;9:1656.
Nawrot U, et al. Detection of Polish clinical Aspergillus fumigatus isolates resistant to triazoles. Med Mycol. 2018;56:121–4.
Ener B, et al. Frequency of azole resistance in clinical and environmental strains of Aspergillus fumigatus in Turkey: a multicentre study. J Antimicrob Chemother. 2022;77:1894–8.
Tsitsopoulou A et al. Determination of the prevalence of triazole resistance in environmental Aspergillus fumigatus strains isolated in South Wales, UK. Front Microbiol. 2018;9:1395.
Siopi M, et al. Nationwide surveillance of azole-resistant Aspergillus fumigatus environmental isolates in Greece: detection of pan-azole resistance associated with the TR46/Y121F/T289A cyp51A mutation. J Antimicrob Chemother. 2020;75:3181–8.
Riat A, Plojoux J, Gindro K, Schrenzel J & Sanglard D. Azole resistance of environmental and clinical Aspergillus fumigatus isolates from Switzerland. Antimicrob Agents Chemother. 2018;62(4):e02088-17.
Ragozzino S et al. Distribution of Aspergillus species and prevalence of azole resistance in respiratory samples from Swiss tertiary care hospitals. Open Forum Infect Dis. 2021;9(2):ofab638.
Wiederhold NP, et al. First detection of TR34 L98H and TR46 Y121F T289A Cyp51 mutations in Aspergillus fumigatus isolates in the United States. J Clin Microbiol. 2016;54:168–71.
Berkow E. L et al. Detection of TR34/L98H CYP51A Mutation through passive surveillance for azole-resistant Aspergillus fumigatus in the United States from 2015 to 2017. Antimicrob Agents Chemother. 2018;62(5):e02240-17.
Bustamante B, Illescas LR, Posadas A, Campos PE. Azole resistance among clinical isolates of Aspergillus fumigatus in Lima-Peru. Med Mycol. 2020;58:54–60.
Pontes, L et al. Aspergillus fumigatus clinical isolates carrying CYP51A with TR34/L98H/S297T/F495I substitutions detected after four-year retrospective azole resistance screening in Brazil. Antimicrob Agents Chemother. 2020;64(3):e02059-19.
Alvarez-Moreno, C et al. Azole-resistant Aspergillus fumigatus harboring TR34/L98H, TR46/Y121F/T289A and TR53 mutations related to flower fields in Colombia. Sci Rep. 2017;7:45631.
Gonzalez-Lara MF, et al. Azole resistance and cyp51A mutation screening in Aspergillus fumigatus in Mexico. J Antimicrob Chemother. 2019;74:2047–50.
Devoto TB, et al. High prevalence of triazole-resistant Aspergillus fumigatus sensu stricto in an Argentinean cohort of patients with cystic fibrosis. Mycoses. 2020;63:937–41.
Amona, FM et al. Triazole resistance in Aspergillus fumigatus isolates in Africa: a systematic review. Med Mycol. 2022;60(8):myac059.
Khojasteh, S et al. Five-year surveillance study of clinical and environmental Triazole-Resistant Aspergillus fumigatus isolates in Iran. Mycoses. 2023;66(2):98–105.
Lockhart SR, et al. Azole resistance in Aspergillus fumigatus isolates from the ARTEMIS global surveillance study is primarily due to the TR/L98H mutation in the cyp51A gene. Antimicrob Agents Chemother. 2011;55:4465–8.
Deng S, et al. Triazole phenotypes and genotypic characterization of clinical Aspergillus fumigatus isolates in China. Emerg Microbes Infect. 2017;6:e109.
Wang H-C, et al. Prevalence, mechanisms and genetic relatedness of the human pathogenic fungus Aspergillus fumigatus exhibiting resistance to medical azoles in the environment of Taiwan. Environ Microbiol. 2018;20:270–80.
Perveen I, Sehar S, Naz I, Ahmed S. Prospective evaluation of azole resistance in Aspergillus fumigatus clinical isolates in Pakistan. In: Proceedings of Seventh Advances Against Aspergillosis conference. Manchester, UK: Aspergillus and Aspergillosis; 2016.
Toyotome T, et al. Prospective survey of Aspergillus species isolated from clinical specimens and their antifungal susceptibility: a five-year single-center study in Japan. J Infect Chemother. 2020;26:321–3.
Tangwattanachuleeporn M, et al. Prevalence of azole-resistant Aspergillus fumigatus in the environment of Thailand. Med Mycol. 2017;55:429–35.
Duong T-MN, et al. Azole-resistant Aspergillus fumigatus is highly prevalent in the environment of Vietnam, with marked variability by land use type. Environ Microbiol. 2021;23:7632–42.
Talbot JJ, et al. Surveillance for azole resistance in clinical and environmental isolates of Aspergillus fumigatus in Australia and cyp51A homology modelling of azole-resistant isolates. J Antimicrob Chemother. 2018;73:2347–51.
Jung IY, et al. Identification of fungal species and detection of azole-resistance mutations in the Aspergillus fumigatus cyp51A gene at a South Korean hospital. Yonsei Med J. 2020;61:698–704.
Lamoth, F. Aspergillus fumigatus-related species in clinical practice. Front Microbiol. 2016;7:683.
Balajee SA, Weaver M, Imhof A, Gribskov J, Marr KA. Aspergillus fumigatus variant with decreased susceptibility to multiple antifungals. Antimicrob Agents Chemother. 2004;48:1197–203.
Nematollahi S, Permpalung N, Zhang SX, Morales M & Marr K A. Aspergillus lentulus: an under-recognized cause of antifungal drug-resistant Aspergillosis. Open Forum Infect Dis. 2021;8(8):ofab392.
Yagi K, et al. Invasive pulmonary aspergillosis due to Aspergillus lentulus in an adult patient: a case report and literature review. J Infect Chemother. 2019;25:547–51.
Tateno M, et al. Examination of Cyp51A-mediated azole resistance in Aspergillus lentulus using CRISPR/Cas9 genome editing. Med Mycol J. 2022;63:27–35.
Sugui JA, et al. Neosartorya udagawae (Aspergillus udagawae), an emerging agent of Aspergillosis: how different is it from Aspergillus fumigatus? J Clin Microbiol. 2010;48:220–8.
Balajee SA, et al. Molecular identification of Aspergillus species collected for the Transplant-Associated Infection Surveillance Network. J Clin Microbiol. 2009;47:3138–41.
Rudramurthy SM, Paul RA, Chakrabarti A, Mouton JW, Meis JF. Invasive Aspergillosis by Aspergillus flavus: epidemiology, diagnosis, antifungal resistance, and management. J Fungi. 2019;5:55.
Abdalla MH. Prevalence of airborne Aspergillus flavus in Khartoum (Sudan) airspora with reference to dusty weather and inoculum survival in simulated summer conditions. Mycopathologia. 1988;104:137–41.
Rotjanapan P, et al. Epidemiology and clinical characteristics of invasive mould infections: a multicenter, retrospective analysis in five Asian countries. Med Mycol. 2018;56:186–96.
Chakrabarti A, et al. Epidemiology and clinical outcomes of invasive mould infections in Indian intensive care units (FISF study). J Crit Care. 2019;51:64–70.
Risslegger B, et al. A prospective international Aspergillus terreus survey: an EFISG, ISHAM and ECMM joint study. Clin Microbiol Infect. 2017;23(776):e1-776.e5.
Lass-Flörl C, Dietl A-M, Kontoyiannis DP, Brock M. Aspergillus terreus species complex. Clin Microbiol Rev. 2021. https://doi.org/10.1128/CMR.00311-20.
Zoran T et al. Azole-resistance in Aspergillus terreus and related species: an emerging problem or a rare phenomenon? Front Microbiol. 2018;9:516.
Blum G, et al. New insight into amphotericin B resistance in Aspergillus terreus. Antimicrob Agents Chemother. 2013;57:1583–8.
Pappas PG, et al. Invasive fungal infections among organ transplant recipients: results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Clin Infect Dis. 2010;50:1101–11.
Kontoyiannis DP, et al. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001–2006: overview of the Transplant-Associated Infection Surveillance Network (TRANSNET) Database. Clin Infect Dis. 2010;50:1091–100.
Vermeulen E, et al. Invasive Aspergillus niger complex infections in a Belgian tertiary care hospital. Clin Microbiol Infect. 2014;20:O333–5.
Howard SJ, Harrison E, Bowyer P, Varga J, Denning DW. Cryptic species and azole resistance in the Aspergillus niger complex▿. Antimicrob Agents Chemother. 2011;55:4802–9.
Glampedakis E, et al. Invasive Aspergillosis due to Aspergillus section Usti: a multicenter retrospective study. Clin Infect Dis. 2021;72:1379–85.
Lamoth F, Chung SJ, Damonti L, Alexander BD. Changing epidemiology of invasive mold infections in patients receiving azole prophylaxis. Clin Infect Dis. 2017;64:1619–21.
King J, Henriet SSV & Warris A. Aspergillosis in chronic granulomatous disease. J Fungi (Basel). 2016;2(2):15.
Chrenkova V, et al. Proven invasive pulmonary aspergillosis in stem cell transplant recipient due to Aspergillus sublatus, a cryptic species of A. nidulans. Mycopathologia. 2018;183:423–9.
Henriet SSV, Verweij PE, Warris A. Aspergillus nidulans and chronic granulomatous disease: a unique host–pathogen interaction. J Infect Dis. 2012;206:1128–37.
Salsé M, et al. Multicentre study to determine the Etest epidemiological cut-off values of antifungal drugs in Candida spp. and Aspergillus fumigatus species complex. Clin Microbiol Infect. 2019;25:1546–52.
Garcia-Rubio R, et al. Insight into the significance of Aspergillus fumigatus cyp51A polymorphisms. Antimicrob Agents Chemother. 2018. https://doi.org/10.1128/AAC.00241-18.
Pérez-Cantero, A., Martin-Vicente, A., Guarro, J., Fortwendel, J. R. & Capilla, J. Analysis of the contribution of cyp51 genes to azole resistance in Aspergillus section Nigri with the CRISPR-Cas9 technique. Antimicrob Agents Chemother. 2023;65(5):e01996-20.
Pérez-Cantero A, López-Fernández L, Guarro J, Capilla J. Azole resistance mechanisms in Aspergillus: update and recent advances. Int J Antimicrob Agents. 2020;55:105807.
Paul RA, et al. Magnitude of voriconazole resistance in clinical and environmental isolates of Aspergillus flavus and investigation into the role of multidrug efflux pumps. Antimicrob Agents Chemother. 2018. https://doi.org/10.1128/AAC.01022-18.
Liu W, et al. The T788G mutation in the cyp51C gene confers voriconazole resistance in Aspergillus flavus causing Aspergillosis. Antimicrob Agents Chemother. 2012;56:2598–603.
Snelders E, et al. Genotype–phenotype complexity of the TR46/Y121F/T289A cyp51A azole resistance mechanism in Aspergillus fumigatus. Fungal Genet Biol. 2015;82:129–35.
Paul S, Diekema D, Moye-Rowley WS. Contributions of both ATP-binding cassette transporter and Cyp51A proteins are essential for azole resistance in Aspergillus fumigatus. Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/AAC.02748-16.
Paul S et al. AtrR is an essential determinant of azole resistance in Aspergillus fumigatus. mBio. 2019;10(2):e02563-18. https://doi.org/10.1128/mBio.02563-18.
Zhang J, et al. Evolution of cross-resistance to medical triazoles in Aspergillus fumigatus through selection pressure of environmental fungicides. Proc R Soc B Biol Sci. 2017;284:20170635.
Hare RK et al. In vivo selection of a unique tandem repeat mediated azole resistance mechanism (TR120) in Aspergillus fumigatus cyp51A, Denmark - Volume 25, Number 3—March 2019 - Emerging Infectious Diseases journal - CDC. Emerg Infect Dis. 2019;25(3):577–580. https://doi.org/10.3201/eid2503.180297.
Perlin DS, Shor E, Zhao Y. Update on antifungal drug resistance. Curr Clin Microbiol Rep. 2015;2:84–95.
Meneau I, Coste AT, Sanglard D. Identification of Aspergillus fumigatus multidrug transporter genes and their potential involvement in antifungal resistance. Med Mycol. 2016;54:616–27.
Rybak J M et al. Mutations in hmg1, challenging the paradigm of clinical triazole resistance in Aspergillus fumigatus. mBio. 2019;10(2):e00437-19. https://doi.org/10.1128/mBio.00437-19.
Berkow EL, Lockhart SR & Ostrosky-Zeichner L. Antifungal susceptibility testing: current approaches. Clin Microbiol Rev. 2020;33(3):e00069-19.
Arendrup MC, Cuenca-Estrella M, Lass-Flörl C, Hope WW. EUCAST technical note on Aspergillus and amphotericin B, itraconazole, and posaconazole. Clin Microbiol Infect. 2012;18:E248–50.
Arendrup MC, et al. EUCAST technical note on isavuconazole breakpoints for Aspergillus, itraconazole breakpoints for Candida and updates for the antifungal susceptibility testing method documents. Clin Microbiol Infect. 2016;22(571):e1-571.e4.
Espinel-Ingroff A, Turnidge J. The role of epidemiological cutoff values (ECVs/ECOFFs) in antifungal susceptibility testing and interpretation for uncommon yeasts and moulds. Rev Iberoam Micol. 2016;33:63–75.
Espinel-Ingroff A, Cuenca-Estrella M, Cantón E. EUCAST and CLSI: working together towards a harmonized method for antifungal susceptibility testing. Curr Fungal Infect Rep. 2013;7:59–67.
Jenks JD, Spiess B, Buchheidt D, Hoenigl M. (New) methods for detection of Aspergillus fumigatus resistance in clinical samples. Curr Fungal Infect Rep. 2019;13:129–36.
Scharmann U, et al. Evaluation of three commercial PCR assays for the detection of azole-resistant Aspergillus fumigatus from respiratory samples of immunocompromised patients. J Fungi. 2021;7:132.
van der Torre MH, Novak-Frazer L & Rautemaa-Richardson R. Detecting azole-antifungal resistance in Aspergillus fumigatus by pyrosequencing. J Fungi (Basel). 2020;6(1):12.
Gitman MR, et al. Antifungal susceptibility testing of Aspergillus spp. by using a composite correlation index (CCI)-based matrix-assisted laser desorption ionization-time of flight mass spectrometry method appears to not offer benefit over traditional broth microdilution testing. J Clin Microbiol. 2017;55:2030–4.
Puértolas-Balint F et al. Revealing the virulence potential of clinical and environmental Aspergillus fumigatus isolates using whole-genome sequencing. Front Microbiol. 2019;10:1970.
Mariette C, et al. Epidemiology of invasive fungal infections during induction therapy in adults with acute lymphoblastic leukemia: a GRAALL-2005 study. Leuk Lymphoma. 2017;58:586–93.
Roth, R. S. et al. Invasive mold infections in Allogeneic hematopoietic cell transplant recipients in 2020: have we made enough progress? Open Forum Infect Dis. 2021;9(1):ofab596.
Bergeron A, et al. The strategy for the diagnosis of invasive pulmonary aspergillosis should depend on both the underlying condition and the leukocyte count of patients with hematologic malignancies. Blood. 2012;119:1831–7.
Lestrade PP, et al. Voriconazole resistance and mortality in invasive aspergillosis: a multicenter retrospective cohort study. Clin Infect Dis. 2019;68:1463–71.
Koehler P, et al. Epidemiology of invasive aspergillosis and azole resistance in patients with acute leukaemia: the SEPIA study. Int J Antimicrob Agents. 2017;49:218–23.
Resendiz-Sharpe A, et al. Prevalence of voriconazole-resistant invasive aspergillosis and its impact on mortality in haematology patients. J Antimicrob Chemother. 2019;74:2759–66.
Chong GM, et al. PCR-based detection of Aspergillus fumigatus Cyp51A mutations on bronchoalveolar lavage: a multicentre validation of the AsperGenius assay® in 201 patients with haematological disease suspected for invasive aspergillosis. J Antimicrob Chemother. 2016;71:3528–35.
van de Veerdonk FL, et al. Influenza-associated aspergillosis in critically ill patients. Am J Respir Crit Care Med. 2017;196:524–7.
Lestrade PP, et al. Epidemiology of invasive aspergillosis and triazole-resistant Aspergillus fumigatus in patients with haematological malignancies: a single-centre retrospective cohort study. J Antimicrob Chemother. 2018;73:1389–94.
Tissot F, et al. ECIL-6 guidelines for the treatment of invasive candidiasis, aspergillosis and mucormycosis in leukemia and hematopoietic stem cell transplant patients. Haematologica. 2017;102:433–44.
Herbrecht R et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002;347(6):408–15. https://doi.org/10.1056/NEJMoa020191.
Maertens JA, et al. Isavuconazole versus voriconazole for primary treatment of invasive mould disease caused by Aspergillus and other filamentous fungi (SECURE): a phase 3, randomised-controlled, non-inferiority trial. The Lancet. 2016;387:760–9.
Maertens JA, et al. Posaconazole versus voriconazole for primary treatment of invasive aspergillosis: a phase 3, randomised, controlled, non-inferiority trial. The Lancet. 2021;397:499–509.
Dragonetti G, Criscuolo M, Fianchi L, Pagano L. Invasive aspergillosis in acute myeloid leukemia: are we making progress in reducing mortality? Med Mycol. 2017;55:82–6.
Schauwvlieghe AFAD, et al. The diagnosis and treatment of invasive aspergillosis in Dutch haematology units facing a rapidly increasing prevalence of azole-resistance. A nationwide survey and rationale for the DB-MSG 002 study protocol. Mycoses. 2018;61:656–64.
Schauwvlieghe AFAD, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir Med. 2018;6:782–92.
Verweij PE, et al. International expert opinion on the management of infection caused by azole-resistant Aspergillus fumigatus. Drug Resist Updat. 2015;21–22:30–40.
Wiederhold NP, Verweij PE. Aspergillus fumigatus and pan-azole resistance: who should be concerned? Curr Opin Infect Dis. 2020;33:290–7.
Schauwvlieghe AFAD, et al. High-dose posaconazole for azole-resistant aspergillosis and other difficult-to-treat mould infections. Mycoses. 2020;63:122–30.
Seyedmousavi S, Mouton JW, Melchers WJG, Brüggemann RJM, Verweij PE. The role of azoles in the management of azole-resistant aspergillosis: from the bench to the bedside. Drug Resist Updat. 2014;17:37–50.
Talbot JJ et al. cyp51A Mutations, extrolite profiles, and antifungal susceptibility in clinical and environmental isolates of the Aspergillus viridinutans species complex. Antimicrob Agents Chemother. 2019;63(11):e00632-19.
Imbert, S et al. Multicentric analysis of the species distribution and antifungal susceptibility of cryptic isolates from Aspergillus section Fumigati. Antimicrob Agents Chemother. 2020;64(12):e01374-20.
Lass-Flörl C. Treatment of infections due to Aspergillus terreus species complex. J Fungi. 2018;4:83.
Pérez-Cantero A, López-Fernández L, Guarro J & Capilla J. New insights into the Cyp51 contribution to azole resistance in Aspergillus section Nigri. Antimicrob Agents Chemother. 2019;63(7):e00543-19.
Glampedakis E, et al. Efficacy of antifungal monotherapies and combinations against Aspergillus calidoustus. Antimicrob Agents Chemother. 2018. https://doi.org/10.1128/AAC.01137-18.
Rivero-Menendez O, Soto-Debran JC, Cuenca-Estrella M & Alastruey-Izquierdo A. In vitro activity of ibrexafungerp against a collection of clinical isolates of Aspergillus, including cryptic species and Cyp51A mutants, using EUCAST and CLSI methodologies. J Fungi (Basel). 2021;7(3):232.
Miesel L, Lin K-Y, Ong V. Rezafungin treatment in mouse models of invasive candidiasis and aspergillosis: insights on the PK/PD pharmacometrics of rezafungin efficacy. Pharmacol Res Perspect. 2019;7:e00546.
Shaw KJ, Ibrahim AS. Fosmanogepix: a review of the first-in-class broad spectrum agent for the treatment of invasive fungal infections. J Fungi. 2020;6:239.
Kirchhoff L, Dittmer S, Buer J, Rath P-M, Steinmann J. In vitro activity of olorofim (F901318) against fungi of the genus, Scedosporium and Rasamsonia as well as against Lomentospora prolificans, Exophiala dermatitidis and azole-resistant Aspergillus fumigatus. Int J Antimicrob Agents. 2020;56:106105.
Funding
Open access funding provided by University of Geneva D.N. has received research support from MSD and Pfizer and consulting fees from MSD, Pfizer, Basilea, and Gilead.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bosetti, D., Neofytos, D. Invasive Aspergillosis and the Impact of Azole-resistance. Curr Fungal Infect Rep 17, 77–86 (2023). https://doi.org/10.1007/s12281-023-00459-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-023-00459-z