Abstract
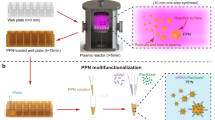
Taxane efficacy in triple negative breast cancer (TNBC) is limited by insufficient tumor accumulation and severe off-target effects. Nanomedicines offer a unique opportunity to enhance the anti-cancer potency of this drug. Here, 1,000 nm × 400 nm discoidal polymeric nanoconstructs (DPN) encapsulating docetaxel (DTXL) and the near infrared compound lipid-Cy5 were engineered. DPN were obtained by filling multiple times cylindrical wells in a poly(vinyl alcohol) template with a polymer mixture comprising poly(lactic-co-glycolic acid) (PLGA) and poly(ethylene glycol) diacrylate (PEG-DA) chains together with therapeutic and imaging agents. The resulting “multi-passage” DPN exhibited higher DTXL loading, lipid-Cy5 stability, and stiffness as compared to the conventional “single-passage” approach. Confocal microscopy confirmed that DTXL-DPN were not taken up by MDA-MB-231 cells but would rather sit next to the cell membrane and slowly release DTXL thereof. Empty DPN had no toxicity on TNBC cells, whereas DTXL-DPN presented a cytotoxic potential comparable to free DTXL (IC50 = 2.6 nM ± 1.0 nM vs. 7.0 nM ± 1.09 nM at 72 h). In orthotopic murine models, DPN accumulated in TNBC more efficiently than free-DTXL. With only 2 mg/kg DTXL, intravenously administered every 2 days for a total of 13 treatments, DTXL-DPN induced tumor regression and were associated to an overall 80% survival rate as opposed to a 30% survival rate for free-DTXL, at 120 days. All untreated mice succumbed before 90 days. Collectively, this data demonstrates that vascular confined multi-passage DPN, biomimicking the behavior of circulating platelets, can efficiently deliver chemotherapeutic molecules to malignant tissues and effectively treat orthotopic TNBC at minimal taxane doses.

Article PDF
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Change history
01 November 2021
Missing funding note during original upload.
References
Perou, C. M.; Sørlie, T.; Eisen, M. B.; van de Rijn, M.; Jeffrey, S. S.; Rees, C. A.; Pollack, J. R.; Ross, D. T.; Johnsen, H.; Akslen, L. A. et al. Molecular portraits of human breast tumours. Nature 2000, 406, 747–752.
Foulkes, W. D.; Smith, I. E.; Reis-Filho, J. S. Triple-negative breast cancer. N. Engl. J. Med. 2010, 363, 1938–1948.
Sørlie, T.; Perou, C. M.; Tibshirani, R.; Aas, T.; Geisler, S.; Johnsen, H.; Hastie, T.; Eisen, M. B.; van de Rijn, M.; Jeffrey, S. S. et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc. Natl. Acad. Sci. USA 2001, 98, 10869–10874.
Kennecke, H.; Yerushalmi, R.; Woods, R.; Cheang, M. C. U.; Voduc, D.; Speers, C. H.; Nielsen, T. O.; Gelmon, K. Metastatic behavior of breast cancer subtypes. J. Clin. Oncol. 2010, 28, 3271–3277.
Bianchini, G.; Balko, J. M.; Mayer, I. A.; Sanders, M. E.; Gianni, L. Triple-negative breast cancer: Challenges and opportunities of a heterogeneous disease. Nat. Rev. Clin. Oncol. 2016, 13, 674–690.
Lee, A.; Djamgoz, M. B. A. Triple negative breast cancer: Emerging therapeutic modalities and novel combination therapies. Cancer Treat. Rev. 2018, 62, 110–122.
Chavez, K. J.; Garimella, S. V.; Lipkowitz, S. Triple negative breast cancer cell lines: One tool in the search for better treatment of triple negative breast cancer. Breast Dis. 2010, 32, 35–48.
Anders, C. K.; Carey, L. A. Biology, metastatic patterns, and treatment of patients with triple-negative breast cancer. Clin. Breast Cancer 2009, 9, S73–S81.
Bourgeois-Daigneault, M. C.; Roy, D. G.; Aitken, A. S.; El Sayes, N.; Martin, N. T.; Varette, O.; Falls, T.; St-Germain, L. E.; Pelin, A.; Lichty, B. D. et al. Neoadjuvant oncolytic virotherapy before surgery sensitizes triple-negative breast cancer to immune checkpoint therapy. Sci. Transl. Med. 2018, 10, eaao1641.
Isakoff, S. J. Triple-negative breast cancer: Role of specific chemotherapy agents. Cancer J. 2010, 16, 53–61.
Cleator, S.; Heller, W. Coombes, R. C. Triple-negative breast cancer: Therapeutic options. Lancet Oncol. 2007, 8, 235–244.
Kloover, J. S.; den Bakker, M. A.; Gelderblom, H.; van Meerbeeck, J. P. Fatal outcome of a hypersensitivity reaction to paclitaxel: A critical review of premedication regimens. Br. J. Cancer 2004, 90, 304–305.
Gelderblom, H.; Verweij, J.; Nooter, K.; Sparreboom, A. Cremophor EL: The drawbacks and advantages of vehicle selection for drug formulation. Eur. J. Cancer 2001, 37, 1590–1598.
Laurentiis, M. D.; Cancello, G.; D’Agostino, D.; Giuliano, M.; Giordano, A.; Montagna, E.; Lauria, R.; Forestieri, V., Esposito, A.; Silvestro, L. et al. Taxane-based combinations as adjuvant chemotherapy of early breast cancer: A meta-analysis of randomized trials. J. Clin. Oncol. 2008, 26, 44–53.
Engels, F. K.; Mathot, R. A.; Verweij, J. Alternative drug formulations of docetaxel: A review. Anti-Cancer Drugs 2007, 18, 95–103.
van der Meel, R.; Sulheim, E.; Shi, Y.; Kiessling, F.; Mulder, W. J. M.; Lammers, T. Smart cancer nanomedicine. Nat. Nanotechnol. 2019, 14, 1007–1017.
Yu, M. K.; Park, J.; Jon, S. Targeting strategies for multifunctional nanoparticles in cancer imaging and therapy. Theranostics 2012, 2, 3–44.
Gradishar, W. J.; Tjulandin, S.; Davidson, N.; Shaw, H.; Desai, N.; Bhar, P.; Hawkins, M.; O’Shaughnessy, J. Phase III trial of nanoparticle albumin-bound paclitaxel compared with polyethylated castor oil-based paclitaxel in women with breast cancer. J. Clin. Oncol. 2005, 23, 7794–7803.
Anselmo, A. C.; Mitragotri, S. Nanoparticles in the clinic: An update. Bioeng. Transl. Med. 2019, 4, e10143.
Maeda, H.; Nakamura, H.; Fang, J. The EPR effect for macro-molecular drug delivery to solid tumors: Improvement of tumor uptake, lowering of systemic toxicity, and distinct tumor imaging in vivo. Adv. Drug Deliv. Rev. 2013, 65, 71–79.
Golombek, S. K.; May, J. N.; Theek, B.; Appold, L.; Drude, N.; Kiessling, F.; Lammers, T. Tumor targeting via EPR: Strategies to enhance patient responses. Adv. Drug Deliv. Rev. 2018, 130, 17–38.
Esmaeili, F.; Dinarvand, R.; Ghahremani, M. H.; Amini, M.; Rouhani, H.; Sepehri, N.; Ostad, S. N.; Atyabi, F. Docetaxel-albumin conjugates: Preparation, in vitro evaluation and biodistribution studies. J. Pharm. Sci. 2009, 98, 2718–2730.
Immordino, M. L.; Brusa, P.; Arpicco, S.; Stella, B.; Dosio, F.; Cattel, L. Preparation, characterization, cytotoxicity and pharmacokinetics of liposomes containing docetaxel. J. Control. Release 2003, 91, 417–429.
Chan, J. M.; Zhang, L. F.; Yuet, K. P.; Liao, G.; Rhee, J. W.; Langer, R.; Farokhzad, O. C. PLGA-lecithin-PEG core-shell nanoparticles for controlled drug delivery. Biomaterials 2009, 30, 1627–1634.
Hwang, H. Y.; Kim, I. S.; Kwon, I. C.; Kim, Y. H. Tumor targetability and antitumor effect of docetaxel-loaded hydrophobically modified glycol chitosan nanoparticles. J. Control. Release 2008, 128, 23–31.
Tan, L. W.; Peng, J. R.; Zhao, Q.; Zhang, L.; Tang, X. C.; Chen, L. J.; Lei, M. Y.; Qian, Z. Y. A novel MPEG-PDLLA-PLL copolymer for docetaxel delivery in breast cancer therapy. Theranostics 2017, 7, 2652–2672.
Gaucher, G.; Marchessault, R. H.; Leroux, J. C. Polyester-based micelles and nanoparticles for the parenteral delivery of taxanes. J. Control. Release 2010, 143, 2–12.
Huynh, L.; Leroux, J. C.; Allen, C. Enhancement of docetaxel solubility via conjugation of formulation-compatible moieties. Org. Biomol. Chem. 2009, 7, 3437–3446.
Sun, B. Y.; Straubinger, R. M.; Lovell, J. F. Current taxane formulations and emerging cabazitaxel delivery systems. Nano Res. 2018, 11, 5193–5218.
Pillai, G. Nanomedicines for cancer therapy: An update of FDA approved and those under various stages of development. SOJ Pharm. Pharm. Sci. 2014, 1, 13.
Hawkins, M. J.; Soon-Shiong, P.; Desai, N. Protein nanoparticles as drug carriers in clinical medicine. Adv. Drug Deliv. Rev. 2008, 60, 876–885.
Ernsting, M. J.; Murakami, M.; Undzys, E.; Aman, A.; Press, B.; Li, S. D. A docetaxel-carboxymethylcellulose nanoparticle outperforms the approved taxane nanoformulation, Abraxane, in mouse tumor models with significant control of metastases. J. Control. Release 2012, 162, 575–581.
Bowerman, C. J.; Byrne, J. D.; Chu, K. S.; Schorzman, A. N.; Keeler, A. W.; Sherwood, C. A.; Perry, J. L.; Luft, J. C.; Darr, D. B.; Deal, A. M. et al. Docetaxel-loaded PLGA nanoparticles improve efficacy in taxane-resistant triple-negative breast cancer. Nano Lett. 2017, 17, 242–248.
Contreras-Cáceres, R.; Leiva, M. C.; Ortiz, R.; Díaz, A.; Perazzoli, G.; Casado-Rodríguez, M. A.; Melguizo, C.; Baeyens, J. M.; López-Romero, J. M.; Prados, J. Paclitaxel-loaded hollow-poly (4-vinylpyridine) nanoparticles enhance drug chemotherapeutic efficacy in lung and breast cancer cell lines. Nano Res. 2017, 10, 856–875.
Huang, J. B.; Zhang, H.; Yu, Y.; Chen, Y.; Wang, D.; Zhang, G. Q.; Zhou, G. C.; Liu, J. J.; Sun, Z. G.; Sun, D. X. et al. Biodegradable self-assembled nanoparticles of poly (D, L-lactide-co-glycolide)/hyaluronic acid block copolymers for target delivery of docetaxel to breast cancer. Biomaterials 2014, 35, 550–566.
Liang, D. S.; Zhang, W. J.; Wang, A. T.; Su, H. T.; Zhong, H. J.; Qi, X. R. Treating metastatic triple negative breast cancer with CD44/neuropilin dual molecular targets of multifunctional nanoparticles. Biomaterials 2017, 137, 23–36.
Li, S. H.; Goins, B.; Hrycushko, B. A.; Phillips, W. T.; Bao, A. Feasibility of eradication of breast cancer cells remaining in postlumpectomy cavity and draining lymph nodes following intracavitary injection of radioactive immunoliposomes. Mol. Pharmaceutics 2012, 9, 2513–2522.
Wilhelm, S.; Tavares, A. J.; Dai, Q.; Ohta, S.; Audet, J.; Dvorak, H. F.; Chan, W. C. W. Analysis of nanoparticle delivery to tumours. Nat. Rev. Mater. 2016, 1, 16014.
Petersen, A. L.; Hansen, A. E.; Gabizon, A.; Andresen, T. L. Liposome imaging agents in personalized medicine. Adv. Drug Deliv. Rev. 2012, 64, 1417–1435.
Moss, J. I.; Barjat, H.; Emmas, S. A.; Strittmatter, N.; Maynard, J.; Goodwin, R. J. A.; Storm, G.; Lammers, T.; Puri, S.; Ashford, M. B. et al. High-resolution 3D visualization of nanomedicine distribution in tumors. Theranostics 2020, 10, 880–897.
Hauert, S.; Berman, S.; Nagpal, R.; Bhatia, S. N. A computational framework for identifying design guidelines to increase the penetration of targeted nanoparticles into tumors. Nano Today 2013, 8, 566–576.
Palange, A. L.; Palomba, R.; Rizzuti, I. F.; Ferreira, M.; Decuzzi, P. Deformable discoidal polymeric nanoconstructs for the precise delivery of therapeutic and imaging agents. Mol. Ther. 2017, 25, 1514–1521.
Kolhar, P.; Anselmo, A. C.; Gupta, V.; Pant, K.; Prabhakarpandian, B.; Ruoslahti, E.; Mitragotri, S. Using shape effects to target antibody-coated nanoparticles to lung and brain endothelium. Proc. Natl. Acad. Sci. USA 2013, 110, 10753–10758.
Myerson, J. W.; Anselmo, A. C.; Liu, Y. L.; Mitragotri, S.; Eckmann, D. M.; Muzykantov, V. R. Non-affinity factors modulating vascular targeting of nano- and microcarriers. Adv. Drug. Deliv. Rev. 2016, 99, 97–112.
Key, J.; Palange, A. L.; Gentile, F.; Aryal, S.; Stigliano, C.; Di Mascolo, D.; De Rosa, E.; Cho, M.; Lee, Y.; Singh, J. et al. Soft discoidal polymeric nanoconstructs resist macrophage uptake and enhance vascular targeting in tumors. ACS Nano 2015, 9, 11628–11641.
Decuzzi, P.; Godin, B.; Tanaka, T.; Lee, S. Y.; Chiappini, C.; Liu, X.; Ferrari, M. Size and shape effects in the biodistribution of intravascularly injected particles. J. Control. Release 2010, 141, 320–327.
van de Ven, A. L.; Kim, P.; Haley, O.; Fakhoury, J. R.; Adriani, G.; Schmulen, J.; Moloney, P.; Hussain, F.; Ferrari, M.; Liu, X. W. et al. Rapid tumoritropic accumulation of systemically injected plateloid particles and their biodistribution. J. Control. Release 2012, 158, 148–155.
Adriani, G.; de Tullio, M. D.; Ferrari, M’; Hussain, F.; Pascazio, G.; Liu, X. W.; Decuzzi, P. The preferential targeting of the diseased microvasculature by disk-like particles. Biomaterials 2012, 33, 5504–5513.
Valcourt, D. M.; Harris, J.; Riley, R. S.; Dang, M. G.; Wang, J. X.; Day, E. S. Advances in targeted nanotherapeutics: From bioconjugation to biomimicry. Nano Res. 2018, 11, 4999–5016.
Palomba, R.; Palange, A. L.; Rizzuti, I. F.; Ferreira, M.; Cervadoro, A.; Barbato, M. G.; Canale, C.; Decuzzi, P. Modulating phagocytic cell sequestration by tailoring nanoconstruct softness. ACS Nano 2018, 12, 1433–1444.
Ferreira, M.; Rizzuti, I. F.; Palange, A. L.; Barbato, M. G.; Di Francesco, V.; Di Francesco, M.; Decuzzi, P. Optimizing the pharmacological properties of discoidal polymeric nanoconstructs against triple-negative breast cancer cells. Front. Bioeng. Biotechnol. 2020, 8, 5.
Colasuonno, M.; Palange, A. L.; Aid, R.; Ferreira, M.; Mollica, H.; Palomba, R.; Emdin, M.; Del Sette, M.; Chauvierre, C.; Letourneur, D. et al. Erythrocyte-inspired discoidal polymeric nanoconstructs carrying tissue plasminogen activator for the enhanced lysis of blood clots. ACS Nano 2018, 12, 12224–12237.
Key, J.; Aryal, S.; Gentile, F.; Ananta, J. S.; Zhong M.; Landis, M. D.; Decuzzi, P. Engineering discoidal polymeric nanoconstructs with enhanced magneto-optical properties for tumor imaging. Biomaterials 2013, 34, 5402–5410.
Kutscher, H. L.; Chao, P.; Deshmukh, M.; Singh, Y.; Hu, P. D.; Joseph, L. B.; Reimer, D. C.; Stein, S.; Laskin, D. L.; Sinko, P. J. Threshold size for optimal passive pulmonary targeting and retention of rigid microparticles in rats. J. Control. Release 2010, 143, 31–37.
Anselmo, A. C.; Modery-Pawlowski, C. L.; Menegatti, S.; Kumar, S.; Vogus, D. R.; Tian, L. L.; Chen, M.; Squires, T. M.; Sen Gupta, A.; Mitragotri, S. Platelet-like nanoparticles: Mimicking shape, flexibility, and surface biology of platelets to target vascular injuries. ACS Nano 2014, 8, 11243–11253.
Mosallaei, N.; Jaafari, M. R.; Hanafi-Bojd, M. Y.; Golmohammadzadeh, S.; Malaekeh-Nikouei, B. Docetaxel-loaded solid lipid nanoparticles: Preparation, characterization, in vitro, and in vivo evaluations. J. Pharm. Sci. 2013, 102, 1994–2004.
Acknowledgements
The authors wish to thank the reviewers for their valuable comments and suggestions to improve the quality of the paper. This project was partially supported by the European Research Council, under the European Union’s Seventh Framework Programme (FP7/2007-2013)/ERC grant agreement No. 616695, by the Italian Association for Cancer Research (AIRC) under the individual investigator grant No. 17664, and by the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No. 754490. The authors acknowledge the precious support provided by the Nikon Center, the Material Characterization Facility, the electron microscopy and nanofabrication facilities at the Italian Institute of Technology, and the work of Luca Caseracciu for the mechanical characterization of DPN.
Funding
Funding note: Open access funding provided by Università degli Studi di Padova.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors have declared that no competing interest exists.
Electronic Supplementary Material
12274_2021_3507_MOESM1_ESM.pdf
Vascular-confined multi-passage discoidal nanoconstructs for the low-dose docetaxel inhibition of triple-negative breast cancer growth
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Felici, A., Di Mascolo, D., Ferreira, M. et al. Vascular-confined multi-passage discoidal nanoconstructs for the low-dose docetaxel inhibition of triple-negative breast cancer growth. Nano Res. 15, 482–491 (2022). https://doi.org/10.1007/s12274-021-3507-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12274-021-3507-8