Abstract
The increasing number of long-term survivors of pediatric brain tumors requires us to incorporate the most recent knowledge derived from cognitive neuroscience into their oncological treatment. As the lesion itself, as well as each treatment, can cause specific neural damage, the long-term neurocognitive outcomes are highly complex and challenging to assess. The number of neurocognitive studies in this population grows exponentially worldwide, motivating modern neuroscience to provide guidance in follow-up before, during and after treatment. In this review, we provide an overview of structural and functional brain connectomes and their role in the neuropsychological outcomes of specific brain tumor types. Based on this information, we propose a theoretical neuroscientific framework to apply appropriate neuropsychological and imaging follow-up for future clinical care and rehabilitation trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Given that the survival rates of pediatric brain tumor patients have increased over time, the quality of daily life increasingly requires attention. As the lesion itself, as well as each treatment constituent can induce neurotoxicity [1], these survivors are at risk of long-term educational or work-related difficulties. Problems in attention, school results, and social functioning can already be observed before or shortly after diagnosis. In addition to these initial symptoms, treatment can lead to additional neural damage. First, neurosurgery causes direct brain tissue damage with related degenerative cascade effects. Since functional brain imaging or direct electrical stimulation during awake surgery is implemented less often in pediatrics, sparing of eloquent areas is highly challenging in this population. Second, cranial radiation can additionally lead to a decline in IQ, with younger patients being more at risk [2]. Even though more precision radiotherapy (RT) techniques, including proton beam irradiation (PBT), yield less scatter radiation and theoretically could be beneficial for cognitive sparing [3], IQ scores and attention [4] can still decline in younger irradiated patients [5]. The beneficial neurological effects of replacing RT with high-dose chemotherapy (CT) in younger patients are still to be elucidated [6]. In addition, how these treatments interact with the developing brain network, or the so-called connectome, needs to be investigated further. In the case of pediatric brain tumors, connectome reorganization primarily depends on the location, size, and histological type of the primary tumor. To understand the functional impact of neural damage on specific brain areas, we provide an overview of the structural and functional brain connectomes involved in cognitive outcomes, which can be translated into the findings of long-term cognitive outcomes for each pediatric brain tumor type. In addition, we propose a new scheme for brain network-informed neurocognitive evaluations and potential rehabilitation strategies in the future.
Developing Neural Networks with a Neurocognitive Role
Multiple functional brain subnetworks are involved in daily life neurocognitive functioning (Fig. 1). There is growing evidence that such networks emerge in the first postnatal year, with increasing network integration as well as segregation, referring to the functional specialization of brain subnetworks [7]. The sensorimotor and visual networks, responsible for sensorimotor perception and the processing of visual information, develop first [8]. Networks associated with language, attention, and executive function develop later on. Although the specialized roles of attention-related networks have yet to be elucidated, a useful heuristic has been to envisage the salience, frontoparietal, and dorsal attentional networks as related to external processing while the default mode network is primarily related to internal processing and representations of one's self and past. All of these networks are well-integrated to produce complex human behavior and cognitive outcomes related to attention, learning, memory, and executive function. They have been defined mainly using functional neuroimaging, which is based on the activity of single regions. The correlated activity of two different regions is often referred to as "functional connectivity". While functional connectivity does not necessarily always imply a structural connection (in the form of white matter tracts or fiber bundles), there is evidence that the functionally-defined networks are underpinned by white matter connections (Fig. 2). Crucially, though, there is more to the network than the inter-regional tracts. Connectivity rather seems to obey a "small-world" principle, whereby some regions act as “railway stations” or so-called hubs, showing both local connections to neighboring regions and more distant connections to other hubs. With a growing understanding of these principles and the particular critical structural and functional hubs, it is becoming increasingly realistic to link impaired cognitive function in children with brain tumors, to the structural disturbances caused by these tumors (and their treatment). In turn, this promises a greater capacity to predict longer-term outcomes and, potentially, to implement targeted neurorehabilitation interventions exploiting the great potential for neuroplasticity.
Functional brain areas showing coherent activity associated with certain cognitive or functional tasks. ACC, anterior cingulate cortex; FEF, frontal eye fields; IFG, inferior frontal gyrus (Broca’s area); IPS, intraparietal sulcus; LP, lateral parietal; LPFC, lateral prefrontal cortex; PCC, posterior cingulate cortex; PFC, prefrontal cortex; PPC, posterior parietal cortex; pSTG, posterior superior temporal gyrus (Wernicke’s area); SMG, supramarginal gyrus; Superior, superior section of the S1/M1 areas; Lateral, lateral section of the S1/M1 areas.
Single delineated white matter tracts. The most well-acknowledged single white matter tracts, being part of the whole-brain tractogram, are depicted in the center of the figure. Example tracts were derived from the HCP tractography atlas and created using DSI studio [119]. AF, Arcuate Fasciculus, CC, Corpus Callosum, CST, Corticospinal Tract, ICP, Inferior Cerebellar Peduncle, IFOF, Inferior Fronto-Occipital Fasciculus ILF, Inferior Longitudinal Fasciculus, MCP, Middle Cerebellar Peduncle, SCP, Superior Cerebellar Peduncle, SLF, Superior Longitudinal Fasciculus, UC, Uncinate Fasciculus.
Modern Imaging in Assessing Neural Networks in Pediatrics
Regarding conventional neuroradiological approaches, standard anatomical imaging includes contrast-enhanced imaging to detect primary tumors or metastases. However, these imaging techniques do not allow us to estimate brain networks or behavioral outcomes. Hence, to improve the sparing of daily life functional outcomes, we need to move towards the implementation of functional assessments and more advanced imaging techniques. Nowadays, advanced neuroimaging allows us to estimate not only the local micro- and macrostructure of the brain (e.g. cortical thickness, tissue density, gyrification, sulcification) but also estimate the topology of the structural networks and functional coherence or time-dependency (Fig. 3). More specifically, diffusion-weighted MRI allows us to estimate tractograms and consequently structural connectomes. On the other hand, resting-state functional MRI (rs-fMRI) provides an estimate of simultaneous or dynamic oxygen supply, resulting in estimations of functional connectomes. Connectomics is increasingly receiving attention, as cognitive outcomes are not considered to be explained as one-region-specific anymore, but rather as being network-dependent, with the possible importance of hub areas [9]. Connectomics research based on tractography and rs-fMRI can assist in identifying the involved hub areas. In the following sections, specific tumors and associated cognitive outcomes are discussed, with a specific translation to their involved hub areas (Table 1). Histology-specific tumor locations are depicted in Figure 4.
Connectome graph demonstrating the complexity of the existing functional and structural brain networks. A connectome consists of nodes (i.e. regions, depicted as circles) and edges (i.e. representation of a connectivity measure between two regions, depicted as grey lines). In this graph, both the whole-brain tractogram (i.e. estimated streamlines) and regional activity patterns are depicted, which determine connectivity measures of structural and functional connectivity, respectively. For the streamlines in the background, blue indicates tracts along the axial axis (superior-inferior), green indicates tracts along the sagittal axis (anterior-posterior), and red indicates tracts along the coronal axis (left-right). Different nodes are indicated in different colors, presenting different activity patterns. The colored mini-graphs show average activity patterns for different nodes. Based on such a connectome, graph theoretical metrics can be calculated to determine the brain topology. This figure was constructed based on the Human Connectome Project tractography atlas Yeh et al. [119], which was complemented with an illustrative functional connectome, using DSI studio. For both the tract atlas and the functional connectome, cortical parcellation was applied according to the AAL-atlas.
Histology-specific pediatric brain tumor locations and their position in the developing connectome. In the upper figure, the different types of pediatric brain tumors are demonstrated. On the left panel below, these locations of brain tumors are mapped on the whole-brain functional connectome, where different signaling of different regions is demonstrated. On the right panel below, the tumor types are mapped on the whole-brain tractogram, showing which tracts are involved for each subtype.
Site-and Tumor-specific Neurocognitive Dysfunction and Imaging Findings
Infratentorial Tumors
The infratentorial area is the most common location of pediatric brain tumors, with pilocytic astrocytoma (PiA), medulloblastoma (MB), and ependymoma occurring most frequently. PiA is usually treated with surgery only, while treatment of ependymomas and MB can include radiation. Ependymomas are treated with focal treatments (surgery and RT), whereas craniospinal RT is the standard of care for children aged three years or more with MB. These tumors located in or neighboring the cerebellum can infiltrate and induce pressure in this region, affecting mainly motor functions (Figure 1 and Table 1). In this regard, the most well-known acute neurological complication is the so-called cerebellar mutism syndrome (CMS), which is characterized by short-term mutism, reduced speech, hypotonia, and oropharyngeal dysfunction/dysphagia shortly after cerebellar surgery. This often co-occurs with the cerebellar cognitive affective syndrome, including cognitive regulation of affect symptoms as well [10, 11]. These syndromes occur when surgery affects the efferent cerebellar tracts (specifically the dento-thalamo-cortical tracts [10]) but they are also associated with altered supratentorial perfusion [12]. In addition to surgery, cranial RT and systemic CT can also amplify cognitive decline [13].
While PiA presenting as cystic cerebellar lesions are associated with a low risk of neurocognitive dysfunction, an intrinsic lesion or exophytic brainstem or cerebellar peduncle lesion can still cause significant sequelae, similar to more infiltrative tumors. Such symptoms range from difficulties in executive functioning to lower attention and processing speed problems due to front-cerebellar connectivity [14]. Also, patients’ spatial orientation can be affected after surgery [15] as they can suffer from ataxia. Still, the fine motor skills of patients with PiA are better at the group level than patients with an MB [16].
Neuroimaging studies have indicated that the amount of brain tissue resected during surgery is associated with verbal or working memory outcomes [17], which could be associated with secondary demyelination along cerebellar-cortical tracts [18]. Regarding functional brain changes, decreased activity [19] and decreased N-acetylaspartate metabolite levels [20] in cerebellar areas could explain the encountered behavioral outcomes.
Literature is lacking on neurocognitive effects in infratentorial ependymoma, probably due to small sample sizes. Still, sequelae can be expected, given the possible involvement of the cranial nerves and the brainstem.
Craniospinal RT in MBs is known to increase the risk of neurocognitive decline, with the most evidence for decreases in intelligence throughout their development [21], with a loss of ~ 2.5 estimated IQ points per year [22]. Early findings of decreases in IQ and executive scores (i.e. within 1 year) can be associated with acute CMS [23], while in the longer run, the negative effects of younger age at treatment and treatment intensity become increasingly apparent [24]. Studies have shown that a higher RT dose to the temporal lobe and hippocampus is associated with lower IQ scale scores [25]. Although replacing RT with high-dose chemotherapy might result in fewer cognitive problems [26], certainly in infants, high-dose chemotherapy is still associated with declines in cognitive scores [27] and with leukomalacia [28] as well.
Besides intellectual decline, executive functioning [29] and fine motor skills [16] are also more severely affected in MB patients than PiA patients, as their craniospinal RT plan involves more brain areas, of which some are eloquent.
Not surprisingly, in neuroimaging studies, atrophic processes in MB can occur across the entire brain. Cerebellar atrophy in MB patients is specifically associated with information processing, attention [30], executive functioning [31], and working memory [19]. These outcomes can also be explained by decreased cerebellar-cerebral connectivity [29, 32]. In addition, hippocampal atrophy [33] can occur post-treatment, and this is associated with decreased memory performance. Other imaging features that are associated with the intelligence outcomes of MB patients consist of white matter volume [34], white matter lesions (e.g. 16% after 8 months [35]), and microstructural alterations [18], of which each can be affected by systemic treatment and irradiation. It is hypothesized that RT can induce accelerated cerebrovascular damage in long-term survivors of pediatric brain tumors [36]. The strongest effects of neural changes are found in the case of higher RT doses [37] and intrathecal methotrexate [28], mostly when treated at a younger age [38]. Also, hydrocephalus [39] and ventricular shunt [38], female gender, and seizures [40] are additional risk factors for normal brain tissue development.
In comparison to PiA, MB patients show decreased cerebral blood flow [18], more evident leukoencephalopathy [30], and less cortical thinning throughout development [41].
Supratentorial Tumors
Supratentorial tumors have different histological subtypes and can be located either centrally (pituitary/pineal gland, basal ganglia) or in the lobe-specific supratentorial cortices. For each supratentorial brain area involved, other functional outcomes can arise (Figure 1 and Table 1). In the following section, we summarize the literature for each specific tumor.
First, germ cell tumors are located at suprasellar, pineal, or basal ganglia sites. Although the IQ scores can be stable and within the normal range throughout treatment [42, 43], the scores can be somewhat lower than the norm [43]. More specifically, if the tumor involves the basal ganglia, a lower IQ has been found compared to the pineal or suprasellar regions [43, 44]. This can partly be explained by microstructural changes in the white matter [45]. Furthermore, in the case of oculomotor or visual problems, the visuospatial and fine motor skills can be affected [42], which can affect visual memory, processing speed [46], and the performance scale of IQ assessments [47]. Such symptoms are more present at baseline when the mass is located in the pineal than the suprasellar area [42], while the cognitive decline is stronger in the latter subgroup [46]. In addition, RT of these tumors can potentially lead to cavernous malformations, which can affect brain development as well [48].
Craniopharyngiomas and pituitary adenomas are specifically located in the suprasellar area, which is not only close to the hypothalamus but also the hippocampal area. They are generally treated with surgery, with or without focal RT. These tumors are generally reported to have more significant morbidities compared with other suprasellar tumors due to the inherent invasive growth pattern (involving the hypothalamus, for example), which leads to an interruption in neuroendocrine networks. Long-term sequelae include cognitive deterioration, socio-emotional symptoms, sleep dysfunction, and neuroendocrine problems [49]. Furthermore, due to the location close to the hippocampus (Table 1), episodic memory problems are most often reported in craniopharyngioma [50]. Acute post-surgical difficulties can arise in encoding and memory recall, both for visual [51] and verbal information [52]. Such problems are most prevalent in craniopharyngioma involving the hypothalamus [53] (being proximal to the hippocampal areas and more invasive than pituitary tumors). These problems appear worse in the case of hydrocephalus, shunt insertion [54], or growth into the third ventricle [55]. Due to disruptions of thalamocortical and supratentorial tracts (Table 1 and Figure 2), but also to functional and endocrine changes [56], executive functioning can be altered as well as processing speed [57] or impulsivity [58] and working memory problems [59] in particular. An important underlying mechanism could be the hypothalamic-hippocampal circuitry involvement in impulsivity [60], although such deficits are less frequently reported than memory.
Besides surgery, cranial RT can exacerbate cognitive decline, with the most evidence for memory problems after higher temporal lobe RT doses [61], but also a lower IQ when RT doses exceed > 30–45 Gy in the supratentorial region (specifically in left hippocampal/temporal areas) [62].
Based on imaging findings, memory recall is associated with the functional coupling between the medial prefrontal cortex and the thalamus [50], the grey matter volume of the posterior cingulate cortex [63], and treatment-related microstructural changes in the cingulum [64]. Functional imaging has also demonstrated higher amygdala reactivity when emotional faces are presented to craniopharyngioma patients [65], and this is altered after intranasal oxytocin administration [66].
Pituitary adenomas can be functioning (producing excess hormone) or non-functioning. Given the heterogeneity in endocrine sequelae of these tumors, heterogeneous findings exist regarding their neuropsychological profile. Patients with non-functioning adenomas (NFAs) show decreased verbal memory and processing speed compared to the norm before surgery [67]. These findings can be attributed to locations close to the hippocampus and crossing tracts. Such scores remain stable after surgery, also in the case of suprasellar extension [67, 68]. Postsurgical hypothyroidism can lead to further deterioration [67] due to increased fatigue, hyponatremia, and seizures. Furthermore, decreased cognitive scores can still be detected in 41% of long-term survivors, years after treatment [69], while their intelligence assessments remain within the normal range [70]. In the case of macroadenomas, NFAs can grow upward, compressing the optic chiasma and resulting in vision loss (blurry vision). Limited research on specific cognitive outcomes has been performed in these patients. In patients receiving additional RT (because of a tumor remnant or regrowth), working memory and verbal memory can either decline further [71] or stabilize years after treatment [69]. Gamma-knife radiosurgery is specifically not associated with decreased performance in this population [72].
Patients with functioning pituitary adenomas (FPAs), express more cognitive problems before surgery compared to NFA patients [73]. These patients suffer from hyperpituitarism, of which the most well-known conditions are prolactinomas, acromegaly, and Cushing’s disease. This pre-treatment hormonal overproduction appears to be more important for cognitive outcomes than tumor size. More specifically, negative correlations have been found between adrenocorticotropic hormone (ACTH) levels and arithmetic scores [74], prolactin levels, and memory scores [75], and positive correlations between thyroxine and processing speed, working memory [76], and visual recall [74]. In other words, the relationships between endocrine fluctuations and cognitive performance are hormone-specific in FPA patients. Endocrine changes can lead to difficulties in concentration, learning, planning, and complex attention [77], in addition to problems in memory recall [70], while overall IQ scores are stable. Furthermore, long-term hypercortisolism (i.e. endogenous cortisol) as well as cortisol replacement (e.g. exogenous cortisol) can potentially lead to decreased memory performance [78].
Grey matter volume loss has also been noted in patients with pituitary adenomas. More specifically, Cushing’s disease in FPA is associated with decreased grey matter volume in the anterior cingulate cortex [79] and cerebellum [80], which can be associated with the activity of the disease (i.e. ACTH and serum cortisol levels) [81]. Although NFA patients can demonstrate leukoencephalopathy after treatment (certainly in cases with high blood pressure), such lesions are not associated with cognitive outcomes [82]. With regard to functional imaging, decreased working and verbal memory scores are associated with altered perfusion in the temporal areas [71]. Furthermore, electroencephalographic studies have suggested alterations in conflict monitoring [83].
Finally, visual impairment can occur in case of altered connectivity between visual and higher-order areas [84]. Patients with supratentorial tumors who are even more at risk for visual disturbance have hypothalamic gliomas involving the optic pathway and chiasma [85]. However, this population remains to be underinvestigated to date.
Finally, for lobe-specific supratentorial ependymomas/astrocytomas in pediatrics, no studies have focused on the cognitive outcomes of these specific histological subtypes. Depending on the tumor locations, specific subnetworks can be affected, and result in certain behavioral sequelae in daily life (Table 1).
Challenges of Assessing Neurocognitive Dysfunction After Treatment for Pediatric Brain Tumors
Even though the amount of literature on cognition in pediatric brain tumors is growing exponentially, concerns exist regarding current approaches. More specifically, the existing literature is highly heterogeneous due to the variability of this population, with many confounding factors. These factors include histological tumor types, multimodal treatments with differential surgical approaches and therapeutic doses, wide age ranges, hemisphere dominance, and institution-specific findings due to the lack of multicenter studies.
Not only irradiation and younger age are significant risk factors [5], but also histological tumor type, location, and size [31], relapse [86], epilepsy, endocrine problems [74], hydrocephalus [39] or ventricular shunt [38], cerebellar mutism/cognitive-affective syndrome [23], anesthesia exposure [87], female gender, and seizures [88] can play a major role in daily life neurobehavioral outcomes. In addition, hearing loss, which can be induced by chemotherapy (e.g. platinum-based agents) [89] and RT, can negatively affect neurocognitive outcomes [90]. Hence, intensity-modulated RT [91] and PBT [92] can be beneficial for cognitive measures by sparing healthy brain tissue and decreasing ototoxicity. In addition, multiple single nucleotide polymorphisms have been associated with neurocognitive outcomes [93]. In pediatric brain tumors specifically, most studies evidenced the catechol-O-methyltransferase (COMT) gene involved in neurotransmission [94] and antioxidant enzyme genes (e.g. glutathione S-transferase Theta 1 (GSTT1) and glutathione S-transferase Mu 1 (GSTM1) [95] to be possibly involved. The question for future research remains how these risk factors in addition to a brain tumor interact with the development of the human brain connectome. In this review, we provide a framework for future studies (see below).
Appraisal of Clinical Tools for Assessing Pediatric Neurocognitive Function
Given the heterogeneity in assessment tools, guidelines have been constructed to homogenize test materials and timing. In Europe, the SIOPe Quality of Life Group has proposed that patients below the age of 5 be screened [96] using at least measurements of the developmental quotient (<4 years), and (>4 years) receptive and expressive language, matrices, processing speed, number recall, fine motor, visual motor, semantic memory, and long-term memory. Above the age of 5 years, tests can additionally include the fine motor pegboard and sustained attention and processing speed [97]. These cognitive screenings are suggested to take place at baseline (within the first 6 weeks after diagnosis), 2 years, 5 years post-diagnosis, and 18 years old. This procedure was mainly proposed to standardize assessments across studies, and thus to apply in trials across the pediatric brain population. By contrast, some clinicians might prefer to define time points at the individual level, e.g. to look at specific treatment effects.
While this is a proposed core battery of tests to assess neurocognitive dysfunction, these measures should additionally be associated with neuroimaging parameters, including morphological features of the tumors and non-lesion brain volumes, to improve our knowledge of which areas are crucial to spare from toxicity in the future. This can be a challenge in routine clinical practice. Hence, automated methods of image segmentation and parcellation need to be developed, e.g. for the segmentation of tumoral tissues, as well as regions to be spared (i.e. “organs at risk”). Even more, such optimizations will need to take anatomical deformations into account, using normative templates or healthy tissue as a reference. In order to take the involved networks into account, the selection of cognitive tests could be informed by the tumor-, treatment- and location-based information (Table 1). More specifically, initial “key” tests can be selected and prioritized based on the functional hub (i.e. region) that is involved. In addition, we propose to expand the assessment measuring related or “connected” functions as well (e.g. verbal comprehension as well as speech).
For instance, given that more eloquent areas can be affected by craniospinal or whole-brain RT compared to focal treatment, patients with infratentorial tumors should receive more elaborate testing post-CSI (e.g. IQ, executive function, and visuomotor skills). Similarly, supratentorial tumors close to the medial temporal lobe, such as craniopharyngiomas, can cause more working, verbal, and visual memory problems. Hence, the involved functional hubs should be considered.
Proposal for a Unified Approach to Measure Neurocognition in Combination with Its Neural Correlates
Regarding functional brain imaging, the acquisition of valid active fMRIs can be challenging in a pediatric population (due to anxiety, excessive movement, boredom, and little understanding of a complicated task). The same limitations count for awake electrical stimulation during neurosurgery as well. Therefore, most of the functional imaging studies outlined above in children applied resting-state fMRI to estimate functional brain networks. However, since functional connectivity in the resting state is a state-dependent correlative measure, it does not provide sufficient information about the causal role of brain regions in functional outcomes, nor about underlying structural connectivity. Furthermore, it cannot be interpreted without taking the state of mind of the individual into account [98]. What complicates the interpretation of resting-state fMRI even more, is when children are too young and sedation is needed; this can affect brain signaling [99]. Future research is therefore needed to determine which functional brain areas apply as hub regions for which behavioral outcomes in healthy children. In addition to these challenges in pediatrics, the definition of a “hub” in brain networks depends on which graph metric is used; this is mostly related to the centrality of a node. These metrics often include nodal degree, nodal efficiency, or betweenness centrality. However, such individual metrics can provide different results on what brain areas are assumed to be the hub regions. Hence, hubness can alternatively be defined based on a combination of graph metrics. Van den Heuvel et al. [100] proposed such a combination of nodal metrics (nodal strength, betweenness centrality, clustering coefficient, and characteristic path length), leading to a nodal hub score on a scale of 0–4. More specifically, each nodal metric increased by 1 point if the nodal value was within the 20% highest values. Such an approach could be a more reliable method to estimate hubs within a functional or structural connectome.
In addition, how brain networks reorganize throughout the child’s brain development (and thus the changing microstructural brain environment), up to adulthood, incorporating resting state fMRI and validation against active fMRI is required. Current studies are very limited in acquiring longitudinal data in both pediatric brain tumor patients and controls [32, 101] due to practical challenges. In this context, recent international large-cohort databases have allowed us to use better estimates of normative brain development, including anatomical cortical development as well as network changes [102] and their relationships [103], from the neonatal stage [104] to adulthood [105]. Regarding analyses, it would therefore be advisable to use age- and modality-specific normative templates and parcellations that have been developed for T1-weighted MRI [106], susceptibility mapping [107], perfusion [108], functional networks [109], and diffusion-weighted MRI [110, 111]. Given that functional networks have been generally defined based on the adult population [112], more research on functional pediatric atlases is needed. To handle deformations in the case of pediatric brain tumors, new techniques to artificially correct deformations or lesions are being developed [113] and should be further validated.
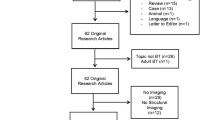
As neuroimaging findings are scarcer than neurocognitive studies, we recommend that centers obtain uniform prospective imaging data of sufficient quality to perform statistical analyses. This includes high-resolution anatomical scanning (e.g. T1-weighted or T2-weighted MR scanning, < 1 mm isotropic resolution) as well as future imaging studies with sufficiently large samples, including yearly functional and structural connectomics data acquisition [e.g. resting state fMRI and diffusion MRI (including b = 1000)]. Once centers have acquired these data in a standardized way, pre-and post-surgical neural development, as well as RT dosimetry plans, can be investigated more in-depth regarding their neural sequelae and associations with cognitive measurements. Ideally, advanced imaging acquisition (including connectomics data) would take place as close as possible to the time points of the standardized neuropsychological assessments. In other words, this would at least take place at baseline (within the first 6 weeks after diagnosis) and at 2-year follow-up (Fig. 5). Trials can then be performed comparing hub information and functional outcomes in targeted neurocognitive rehabilitation arms and control arms with the standard of care.
Flowchart for neuroimaging-informed neuropsychological assessment. This figure explains the selection procedure of tests in clinical practice based on tumor location and network information. First, the brain tumor location is used as prior information, to estimate which functional hub is certainly affected. This core network is neuropsychologically assessed in the first place. For example, speech can be assessed in case of damage to Broca’s area. Second, related functions are assessed. For speech, this could be verbal comprehension as an example. Third, functions that can be secondarily affected by changes in the brain network are assessed in addition. For the speech example, this could be auditory sustained attention, which is “connected” to speech function via the arcuate fasciculus and superior longitudinal fasciculus.
Finally, throughout the procedures of neuropsychological and advanced imaging follow-up, it is important to incorporate shared decision-making with parents as much as possible. Although this can be challenging in pediatric oncology [114], examples of prognostic communication have recently been proposed for pediatric patients with neurological conditions [115].
Current Conclusions Towards Treatment Optimization
Regarding neurosurgery, subtotal resection is intrinsically associated with less brain injury. However, the disease process itself might result in secondary damaging effects, and thus the aggressiveness of the tumor, as well as shared decision-making with parents, are important to keep in mind for such decisions. Awake surgery can additionally be recommended in adolescents with tumors located in eloquent areas. Regarding infratentorial tumors, proximal efferent cerebellar pathways are to be spared in modern neurosurgery as much as possible, without interfering with the superior cerebellar peduncles, to limit the risk of cerebellar mutism/cognitive-affective syndrome. Finally, FPA surgery can improve neurocognitive outcomes when stabilizing the hormonal status.
Second, RT planning can be modified in order to spare the eloquent areas as much as possible, of which the hippocampal area has been proposed as a potentially important hub [62]. However, hub analyses could yield new findings and novel information on tract-based or function-based sparing. In addition, (hyper-)fractionation of RT or PBT [4, 116] could also reduce the cognitive sequelae compared to conventional photon beam therapy.
Finally, interventional studies including pharmacological studies have only recently shown some preliminary positive evidence for metformin [117]. Furthermore, behavioral interventions such as physical exercise can improve neural sparing [118]. In conclusion, efficient sparing of hub areas associated with specific cognitive functions from atrophy or any treatment-induced toxic mechanisms will require large-scale imaging-neurobehavioral research in this population in the near future.
References
Mulhern RK, Merchant TE, Gajjar A, Reddick WE, Kun LE. Late neurocognitive sequelae in survivors of brain tumours in childhood. Lancet Oncol 2004, 5: 399–408.
Raghubar KP, Lamba M, Cecil KM, Yeates KO, Mahone EM, Limke C. Dose-volume metrics and their relation to memory performance in pediatric brain tumor patients: A preliminary study. Pediatr Blood Cancer 2018, 65: e27245.
Pulsifer MB, Sethi RV, Kuhlthau KA, MacDonald SM, Tarbell NJ, Yock TI. Early cognitive outcomes following proton radiation in pediatric patients with brain and central nervous system tumors. Int J Radiat Oncol 2015, 93: 400–407.
Kahalley LS, Peterson R, Douglas Ris M, Janzen L, Okcu MF, Grosshans DR, et al. Superior intellectual outcomes after proton radiotherapy compared with photon radiotherapy for pediatric medulloblastoma. J Clin Oncol 2020, 38: 454–461.
Pulsifer MB, Duncanson H, Grieco J, Evans C, Delgado Tseretopoulos I, MacDonald S, et al. Cognitive and adaptive outcomes after proton radiation for pediatric patients with brain tumors. Int J Radiat Oncol 2018, 102: 391–398.
O’Neil SH, Whitaker AM, Kayser K, Nelson MB, Finlay JL, Dhall G, et al. Neuropsychological outcomes on Head Start III: A prospective, multi-institutional clinical trial for young children diagnosed with malignant brain tumors. Neurooncol Pract 2020, 7: 329–337.
Wen X, Zhang H, Li G, Liu M, Yin W, Lin W, et al. First-year development of modules and hubs in infant brain functional networks. NeuroImage 2019, 185: 222–235.
Grayson DS, Fair DA. Development of large-scale functional networks from birth to adulthood: A guide to the neuroimaging literature. NeuroImage 2017, 160: 15–31.
Stam CJ. Modern network science of neurological disorders. Nat Rev Neurosci 2014, 15: 683–695.
Avula S. Radiology of post-operative paediatric cerebellar mutism syndrome. Child’s Nerv Syst 2020, 36: 1187–1195.
Schmahmann JD. Pediatric post-operative cerebellar mutism syndrome, cerebellar cognitive affective syndrome, and posterior fossa syndrome: Historical review and proposed resolution to guide future study. Childs Nerv Syst 2020, 36: 1205–1214.
Toescu SM, Hales PW, Aquilina K, Clark CA. Quantitative MRI in post-operative paediatric cerebellar mutism syndrome. Eur J Radiol 2018, 108: 43–51.
Merchant TE, Sharma S, Xiong X, Wu S, Conklin H. Effect of cerebellum radiation dosimetry on cognitive outcomes in children with infratentorial ependymoma. Int J Radiat Oncol 2014, 90: 547–553.
Aarsen FK, Paquier PF, Arts WF, Van Veelen ML, Michiels E, Lequin M, et al. Cognitive deficits and predictors 3 years after diagnosis of a pilocytic astrocytoma in childhood. J Clin Oncol 2009, 27: 3526–3532.
Quintero-Gallego EA, Gómez CM, Morales M, Márquez J. Spatial orientation deficit in children due to cerebellum astrocytoma pediatric tumor obtained by means of the Attentional Network Test. Neurosci Lett 2011, 504: 232–236.
Rueckriegel SM, Blankenburg F, Henze G, Baqué H, Driever PH. Loss of fine motor function correlates with ataxia and decline of cognition in cerebellar tumor survivors. Pediatr Blood Cancer 2009, 53: 424–431.
Benavides-Varela S, Lorusso R, Baro V, Denaro L, Estévez-Pérez N, Lucangeli D, et al. Mathematical skills in children with pilocytic astrocytoma. Acta Neurochir (Wien) 2019, 161: 161–169.
Li MD, Forkert ND, Kundu P, Ambler C, Lober RM, Burns TC, et al. Brain perfusion and diffusion abnormalities in children treated for posterior Fossa brain tumors. J Pediatr 2017, 185: 173-180.e3.
Hoang DH, Pagnier A, Cousin E, Guichardet K, Schiff I, Icher C, et al. Anatomo-functional study of the cerebellum in working memory in children treated for medulloblastoma. J Neuroradiol 2019, 46: 207–213.
Rueckriegel SM, Driever PH, Bruhn H. Supratentorial neurometabolic alterations in pediatric survivors of posterior Fossa tumors. Int J Radiat Oncol 2012, 82: 1135–1141.
Di Rocco C, Chieffo D, Pettorini BL, Massimi L, Caldarelli M, Tamburrini G. Preoperative and postoperative neurological, neuropsychological and behavioral impairment in children with posterior cranial fossa astrocytomas and medulloblastomas: The role of the tumor and the impact of the surgical treatment. Childs Nerv Syst 2010, 26: 1173–1188.
Palmer SL, Goloubeva O, Reddick WE, Glass JO, Gajjar A, Kun L, et al. Patterns of intellectual development among survivors of pediatric medulloblastoma: A longitudinal analysis. J Clin Oncol 2001, 19: 2302–2308.
Schreiber JE, Palmer SL, Conklin HM, Mabbott DJ, Swain MA, Bonner MJ, et al. Posterior fossa syndrome and long-term neuropsychological outcomes among children treated for medulloblastoma on a multi-institutional, prospective study. Neuro-oncology 2017, 19: 1673–1682.
Palmer SL, Armstrong C, Onar-Thomas A, Wu S, Wallace D, Bonner MJ, et al. Processing speed, attention, and working memory after treatment for medulloblastoma: An international, prospective, and longitudinal study. J Clin Oncol 2013, 31: 3494–3500.
Merchant TE, Schreiber JE, Wu S, Lukose R, Xiong X, Gajjar A. Critical combinations of radiation dose and volume predict intelligence quotient and academic achievement scores after craniospinal irradiation in children with medulloblastoma. Int J Radiat Oncol 2014, 90: 554–561.
Lafay-Cousin L, Bouffet E, Hawkins C, Amid A, Huang A, Mabbott DJ. Impact of radiation avoidance on survival and neurocognitive outcome in infant medulloblastoma. Curr Oncol 2009, 16: 21–28.
Fay-McClymont TB, Ploetz DM, Mabbott D, Walsh K, Smith A, Chi SN, et al. Long-term neuropsychological follow-up of young children with medulloblastoma treated with sequential high-dose chemotherapy and irradiation sparing approach. J Neurooncol 2017, 133: 119–128.
Riva D, Giorgi C, Nichelli F, Bulgheroni S, Massimino M, Cefalo G, et al. Intrathecal methotrexate affects cognitive function in children with medulloblastoma. Neurology 2002, 59: 48–53.
Law N, Smith ML, Greenberg M, Bouffet E, Taylor MD, Laughlin S, et al. Executive function in paediatric medulloblastoma: The role of cerebrocerebellar connections. J Neuropsychol 2017, 11: 174–200.
Khajuria RK, Blankenburg F, Wuithschick I, Rueckriegel S, Thomale UW, Mansour M, et al. Morphological brain lesions of pediatric cerebellar tumor survivors correlate with inferior neurocognitive function but do not affect health-related quality of life. Childs Nerv Syst 2015, 31: 569–580.
Vaquero E, Gómez CM, Quintero EA, González-Rosa JJ, Márquez J. Differential prefrontal-like deficit in children after cerebellar astrocytoma and medulloblastoma tumor. Behav Brain Funct 2008, 4: 1–16.
Glass JO, Ogg RJ, Hyun JW, Harreld JH, Schreiber JE, Palmer SL, et al. Disrupted development and integrity of frontal white matter in patients treated for pediatric medulloblastoma. Neuro-oncology 2017, 19: 1408–1418.
Decker AL, Szulc KU, Bouffet E, Laughlin S, Chakravarty MM, Skocic J, et al. Smaller hippocampal subfield volumes predict verbal associative memory in pediatric brain tumor survivors. Hippocampus 2017, 27: 1140–1154.
Reddick WE, Russell JM, Glass JO, Xiong X, Mulhern RK, Langston JW, et al. Subtle white matter volume differences in children treated for medulloblastoma with conventional or reduced dose craniospinal irradiation. Magn Reson Imaging 2000, 18: 787–793.
Fouladi M, Chintagumpala M, Laningham FH, Ashley D, Kellie SJ, Langston JW, et al. White matter lesions detected by magnetic resonance imaging after radiotherapy and high-dose chemotherapy in children with medulloblastoma or primitive neuroectodermal tumor. J Clin Oncol 2004, 22: 4551–4560.
Remes TM, Suo-Palosaari MH, Koskenkorva PKT, Sutela AK, Toiviainen-Salo SM, Arikoski PM, et al. Radiation-induced accelerated aging of the brain vasculature in young adult survivors of childhood brain tumors. Neurooncol Pract 2020, 7: 415–427.
Khong PL, Leung LHT, Chan GCF, Kwong DLW, Wong WHS, Cao G, et al. White matter anisotropy in childhood medulloblastoma survivors: Association with neurotoxicity risk factors. Radiology 2005, 236: 647–652.
Reddick WE, Glass JO, Palmer SL, Wu S, Gajjar A, Langston JW, et al. Atypical white matter volume development in children following craniospinal irradiation. Neuro-oncology 2005, 7: 12–19.
Stadskleiv K, Stensvold E, Stokka K, Bechensteen AG, Brandal P. Neuropsychological functioning in survivors of childhood medulloblastoma/CNS-PNET: The role of secondary medical complications. Clin Neuropsychol 2022, 36: 600–625.
Nagel BJ, Palmer SL, Reddick WE, Glass JO, Helton KJ, Wu S, et al. Abnormal hippocampal development in children with medulloblastoma treated with risk-adapted irradiation. AJNR Am J Neuroradiol 2004, 25: 1575–1582.
Kundu P, Li MD, Durkee BY, Hiniker SM, Bush K, von Eyben R, et al. Chemoradiation impairs normal developmental cortical thinning in medulloblastoma. J Neurooncol 2017, 133: 429–434.
Coutinho V, Dellatolas G, Castaignede-Lalande C, Longaud-Vales A, Kieffer V, Guerrini-Rousseau L, et al. Cognitive profile of children with intracranial germ cell tumor according to tumor location. J Pediatr Hematol 2018, 40: e424–e428.
Park Y, Yu ES, Ha B, Park HJ, Kim JH, Kim JY. Neurocognitive and psychological functioning of children with an intracranial germ cell tumor. Cancer Res Treat 2017, 49: 960–969.
Liang SY, Yang TF, Chen YW, Liang ML, Chen HH, Chang KP, et al. Neuropsychological functions and quality of life in survived patients with intracranial germ cell tumors after treatment. Neuro-oncology 2013, 15: 1543–1551.
Tso WWY, Hui ESK, Lee TMC, Liu APY, Ip P, Vardhanabhuti V, et al. Brain microstructural changes associated with neurocognitive outcome in intracranial germ cell tumor survivors. Front Oncol 2021, 11: 573798.
Mabbott DJ, Monsalves E, Spiegler BJ, Bartels U, Janzen L, Guger S, et al. Longitudinal evaluation of neurocognitive function after treatment for central nervous system germ cell tumors in childhood. Cancer 2011, 117: 5402–5411.
Sands SA, Kellie SJ, Davidow AL, Diez B, Villablanca J, Weiner HL, et al. Long-term quality of life and neuropsychologic functioning for patients with CNS germ-cell tumors: From the First International CNS Germ-Cell Tumor Study. Neuro-oncology 2001, 3: 174–183.
Li L, Mugikura S, Kumabe T, Murata T, Mori E, Takase K, et al. A comparative study of the extent of cerebral microvascular injury following whole-brain irradiation versus reduced-field irradiation in long-term survivors of intracranial germ cell tumors. Radiother Oncol 2015, 117: 302–307.
Daubenbüchel AMM, Müller HL. Neuroendocrine disorders in pediatric craniopharyngioma patients. J Clin Med 2015, 4: 389–413.
Özyurt J, Müller HL, Thiel CM. A systematic review of cognitive performance in patients with childhood craniopharyngioma. J Neurooncol 2015, 125: 9–21.
Ondruch A, Maryniak A, Kropiwnicki T, Roszkowski M, Daszkiewicz P. Cognitive and social functioning in children and adolescents after the removal of craniopharyngioma. Childs Nerv Syst 2011, 27: 391–397.
Carpentieri SC, Waber DP, Scott RM, Goumnerova LC, Kieran MW, Cohen LE, et al. Memory deficits among children with craniopharyngiomas. Neurosurgery 2001, 49: 1053–1057; discussion 1057–1058.
Fournier-Goodnight AS, Ashford JM, Merchant TE, Boop FA, Indelicato DJ, Wang L, et al. Neurocognitive functioning in pediatric craniopharyngioma: Performance before treatment with proton therapy. J Neurooncol 2017, 134: 97–105.
Di Pinto M, Conklin HM, Li C, Merchant TE. Learning and memory following conformal radiation therapy for pediatric craniopharyngioma and low-grade glioma. Int J Radiat Oncol 2012, 84: e363–e369.
Fjalldal S, Holmer H, Rylander L, Elfving M, Ekman B, Österberg K, et al. Hypothalamic involvement predicts cognitive performance and psychosocial health in long-term survivors of childhood craniopharyngioma. J Clin Endocrinol Metab 2013, 98: 3253–3262.
Bawden HN, Salisbury S, Eskes G, Morehouse R. Neuropsychological functioning following craniopharyngioma removal. J Clin Exp Neuropsychol 2009, 31: 140–144.
Özyurt J, Thiel CM, Lorenzen A, Gebhardt U, Calaminus G, Warmuth-Metz M, et al. Neuropsychological outcome in patients with childhood craniopharyngioma and hypothalamic involvement. J Pediatr 2014, 164: 876-881.e4.
Kiehna EN, Mulhern RK, Li C, Xiong X, Merchant TE. Changes in attentional performance of children and young adults with localized primary brain tumors after conformal radiation therapy. J Clin Oncol 2006, 24: 5283–5290.
Waber DP, Pomeroy SL, Chiverton AM, Kieran MW, Scott RM, Goumnerova LC, et al. Everyday cognitive function after craniopharyngioma in childhood. Pediatr Neurol 2006, 34: 13–19.
Noble EE, Wang Z, Liu CM, Davis EA, Suarez AN, Stein LM, et al. Hypothalamus-hippocampus circuitry regulates impulsivity via melanin-concentrating hormone. Nat Commun 2019, 10: 4923.
Toussaint L, Indelicato DJ, Muren LP, Li Z, Lassen-Ramshad Y, Kirby K, et al. Temporal lobe sparing radiotherapy with photons or protons for cognitive function preservation in paediatric craniopharyngioma. Radiother Oncol 2020, 142: 140–146.
Goda JS, Dutta D, Krishna U, Goswami S, Kothavade V, Kannan S, et al. Hippocampal radiotherapy dose constraints for predicting long-term neurocognitive outcomes: Mature data from a prospective trial in young patients with brain tumors. Neuro-oncology 2020, 22: 1677–1685.
Özyurt J, Müller HL, Warmuth-Metz M, Thiel CM. Hypothalamic tumors impact gray and white matter volumes in fronto-limbic brain areas. Cortex 2017, 89: 98–110.
Fjalldal S, Follin C, Svärd D, Rylander L, Gabery S, Petersén Å, et al. Microstructural white matter alterations and hippocampal volumes are associated with cognitive deficits in craniopharyngioma. Eur J Endocrinol 2018, 178: 577–587.
Ozyurt J, Lorenzen A, Gebhardt U, Warmuth-Metz M, Müller HL, Thiel CM. Remote effects of hypothalamic lesions in the prefrontal cortex of craniopharygioma patients. Neurobiol Learn Mem 2014, 111: 71–80.
Hoffmann A, Özyurt J, Lohle K, Reichel J, Thiel CM, Müller HL. First experiences with neuropsychological effects of oxytocin administration in childhood-onset craniopharyngioma. Endocrine 2017, 56: 175–185.
Butterbrod E, Gehring K, Voormolen EH, Depauw PRAM, Nieuwlaat WA, Rutten GJ M, et al. Cognitive functioning in patients with nonfunctioning pituitary adenoma before and after endoscopic endonasal transsphenoidal surgery. J Neurosurg 2019: 709–716.
Hendrix P, Griessenauer CJ, Hans E, Simgen A, Oertel J, Karbach J. Cognitive function surrounding resection of nonfunctioning pituitary adenomas with suprasellar extension: A prospective matched-control study. J Clin Neurosci 2017, 40: 109–114.
Crouzeix G, Morello R, Thariat J, Morera J, Joubert M, Reznik Y. Quality of Life but not Cognition is Impacted by Radiotherapy in Patients with Non-Functioning Pituitary Adenoma. Horm Metab Res 2019, 51: 178–185.
Alana Tooze. Neurocognitive changes in pituitary adenoma patients after gamma knife radiosurgery: A preliminary study. World Neurosurg 2012, 78: 122–128.
Lecumberri B, Estrada J, García-Uría J, Millán I, Pallardo LF, Caballero L, et al. Neurocognitive long-term impact of two-field conventional radiotherapy in adult patients with operated pituitary adenomas. Pituitary 2015, 18: 782–795.
Alibas H, Uluc K, Uygur MM, Tuncer N, Tanridag T, et al. Evaluation of depressive mood and cognitive functions in patients with acromegaly under somatostatin analogue therapy. J Endocrinol Invest 2017, 40: 1365–1372.
Wang X, Tong X, Zou Y, Tian X, Mao Z, Sun Z. The impact on cognitive functions of patients with pituitary adenoma before and after surgery. Neurol Sci 2017, 38: 1315–1321.
Kan W, Wang R, Yang K, Liu H, Zou Y, Liu Y, et al. Effect of hormone levels and aging on cognitive function of patients with pituitary adenomas prior to medical treatment. World Neurosurg 2019, 128: e252–e260.
Bala A, Łojek E, Marchel A. Cognitive functioning of patients with a PRL-secreting pituitary adenoma: A preliminary report. Neurology 2016, 86: 731–734.
Müssig K, Besemer B, Saur R, Klingberg S, Häring HU, Gallwitz B, et al. Deteriorated executive functions in patients with successful surgery for pituitary adenomas compared with other chronically ill patients. J Int Neuropsychol Soc 2011, 17: 369–375.
Yedinak CG, Fleseriu M. Self-perception of cognitive function among patients with active acromegaly, controlled acromegaly, and non-functional pituitary adenoma: A pilot study. Endocrine 2014, 46: 585–593.
Tiemensma J, Kokshoorn NE, Biermasz NR, Keijser BJSA, Wassenaar MJE, Middelkoop HAM, et al. Subtle cognitive impairments in patients with long-term cure of cushing’s disease. J Clin Endocrinol Metab 2010, 95: 2699–2714.
Andela CD, van der Werff SJA, Pannekoek JN, van den Berg SM, Meijer OC, van Buchem MA, et al. Smaller grey matter volumes in the anterior cingulate cortex and greater cerebellar volumes in patients with long-term remission of Cushing’s disease: A case-control study. Eur J Endocrinol 2013, 169: 811–819.
Santos A, Resmini E, Crespo I, Pires P, Vives-Gilabert Y, Granell E, et al. Small cerebellar cortex volume in patients with active Cushing’s syndrome. Eur J Endocrinol 2014, 171: 461–469.
Hou B, Gao L, Shi L, Luo Y, Guo X, Young GS, et al. Reversibility of impaired brain structures after transsphenoidal surgery in Cushing’s disease: A longitudinal study based on an artificial intelligence-assisted tool. J Neurosurg 2020: 512–521.
Brummelman P, Sattler MGA, Meiners LC, van den Berg G, van der Klauw MM, Elderson MF, et al. Cognition and brain abnormalities on MRI in pituitary patients. Eur J Radiol 2015, 84: 295–300.
Cao C, Song J, Lin P, Yan D, Yao S, Yue J, et al. A longitudinal, prospective study to evaluate the effects of treatment on the inhibitory control function after transsphenoidal surgery for pituitary adenomas. Clin EEG Neurosci 2021, 52: 444–454.
Song G, Qiu J, Li C, Li J, Gui S, Zhu H, et al. Alterations of regional homogeneity and functional connectivity in pituitary adenoma patients with visual impairment. Sci Rep 2017, 7: 13074.
Riva D, Massimino M, Giorgi C, Nichelli F, Erbetta A, Usilla A, et al. Cognition before and after chemotherapy alone in children with chiasmatic-hypothalamic tumors. J Neurooncol 2009, 92: 49–56.
Morrall MCHJ, Reed-Berendt R, Moss K, Stocks H, Houston AL, Siddell P, et al. Neurocognitive, academic and functional outcomes in survivors of infant ependymoma (UKCCSG CNS 9204). Childs Nerv Syst 2019, 35: 411–420.
Jacola LM, Anghelescu DL, Hall L, Russell K, Zhang H, Wang F, et al. Anesthesia exposure during therapy predicts neurocognitive outcomes in survivors of childhood medulloblastoma. J Pediatr 2020, 223: 141-147.e4.
Stensvold E, Stadskleiv K, Myklebust TÅ, Wesenberg F, Helseth E, Bechensteen AG, et al. Unmet rehabilitation needs in 86% of Norwegian paediatric embryonal brain tumour survivors. Acta Paediatr 2020, 109: 1875–1886.
Orgel E, Jain S, Ji L, Pollick L, Si S, Finlay J, et al. Hearing loss among survivors of childhood brain tumors treated with an irradiation-sparing approach. Pediatr Blood Cancer 2012, 58: 953–958.
Heitzer AM, Villagran AM, Raghubar K, Brown AL, Camet ML, Ris MD, et al. Effect of sensorineural hearing loss on neurocognitive and adaptive functioning in survivors of pediatric embryonal brain tumor. J Neurooncol 2020, 146: 147–156.
Jain N, Krull KR, Brouwers P, Chintagumpala MM, Woo SY. Neuropsychological outcome following intensity-modulated radiation therapy for pediatric medulloblastoma. Pediatr Blood Cancer 2008, 51: 275–279.
Moeller BJ, Chintagumpala M, Philip JJ, Grosshans DR, McAleer MF, Woo SY, et al. Low early ototoxicity rates for pediatric medulloblastoma patients treated with proton radiotherapy. Radiat Oncol 2011, 6: 58.
Wefel JS, Noll KR, Scheurer ME. Neurocognitive functioning and genetic variation in patients with primary brain tumours. Lancet Oncol 2016, 17: e97–e108.
Howarth RA, Adamson AM, Ashford JM, Merchant TE, Ogg RJ, Schulenberg SE, et al. Investigating the relationship between COMT polymorphisms and working memory performance among childhood brain tumor survivors. Pediatr Blood Cancer 2014, 61: 40–45.
Kautiainen RJ, Dwivedi B, MacDonald TJ, King TZ. GSTP1 polymorphisms sex-specific association with verbal intelligence in survivors of pediatric medulloblastoma tumors. Child Neuropsychol 2020, 26: 739–753.
Limond J, Thomas S, Bull KS, Calaminus G, Lemiere J, Traunwieser T, et al. Quality of survival assessment in European childhood brain tumour trials, for children below the age of 5 years. Eur J Paediatr Neurol 2020, 25: 59–67.
Limond JA, Bull KS, Calaminus G, Kennedy CR, Spoudeas HA, Chevignard MP. Quality of survival assessment in European childhood brain tumour trials, for children aged 5 years and over. Eur J Paediatr Neurol 2015, 19: 202–210.
Gonzalez-Castillo J, Kam JWY, Hoy CW, Bandettini PA. How to interpret resting-state fMRI: Ask your participants. J Neurosci 2021, 41: 1130–1141.
Liu X, Lauer KK, Douglas Ward B, Roberts C, Liu S, Gollapudy S, et al. Propofol attenuates low-frequency fluctuations of resting-state fMRI BOLD signal in the anterior frontal cortex upon loss of consciousness. Neuroimage 2017, 147: 295–301.
van den Heuvel MP, Mandl RCW, Stam CJ, Kahn RS, Hulshoff Pol HE. Aberrant frontal and temporal complex network structure in schizophrenia: A graph theoretical analysis. J Neurosci 2010, 30: 15915–15926.
Calmon R, Puget S, Varlet P, Dangouloff-Ros V, Blauwblomme T, Beccaria K, et al. Cerebral blood flow changes after radiation therapy identifies pseudoprogression in diffuse intrinsic pontine gliomas. Neuro-oncology 2018, 20: 994–1002.
Khundrakpam BS, Lewis JD, Zhao L, Chouinard-Decorte F, Evans AC. Brain connectivity in normally developing children and adolescents. Neuroimage 2016, 134: 192–203.
Reardon PK, Seidlitz J, Vandekar S, Liu S, Patel R, Park MTM, et al. Normative brain size variation and brain shape diversity in humans. Science 2018, 360: 1222–1227.
Fenchel D, Dimitrova R, Robinson EC, Batalle D, Chew A, Falconer S, et al. Neonatal multi-modal cortical profiles predict 18-month developmental outcomes. Dev Cogn Neurosci 2022, 54: 101103.
Van Essen DC, Ugurbil K, Auerbach E, Barch D, Behrens TJ, Bucholz R, et al. The Human Connectome Project: A data acquisition perspective. NeuroImage 2012, 62: 2222–2231.
Sanchez CE, Richards JE, Almli CR. Age-specific MRI templates for pediatric neuroimaging. Dev Neuropsychol 2012, 37: 379–399.
Zhang Y, Wei H, Cronin MJ, He N, Yan F, Liu C. Longitudinal atlas for normative human brain development and aging over the lifespan using quantitative susceptibility mapping. Neuroimage 2018, 171: 176–189.
Avants BB, Duda JT, Kilroy E, Krasileva K, Jann K, Kandel BT, et al. The pediatric template of brain perfusion. Sci Data 2015, 2: 150003.
Zhu J, Zhang H, Chong YS, Shek LP, Gluckman PD, Meaney MJ, et al. Integrated structural and functional atlases of Asian children from infancy to childhood. Neuroimage 2021, 245: 118716.
Bobba PS, Weber CF, Mak A, Mozayan A, Malhotra A, Sheth KN, et al. Age-related topographic map of magnetic resonance diffusion metrics in neonatal brains. Hum Brain Mapp 2022, 43: 4326–4334.
Chu C, Guan H, Xie S, Wang Y, Luo J, Zhao G, et al. The SACT template: A human brain diffusion tensor template for school-age children. Neurosci Bull 2022, 38: 607–621.
Whitfield-Gabrieli S, Nieto-Castanon A. Conn: A functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connect 2012, 2: 125–141.
Radwan AM, Emsell L, Blommaert J, Zhylka A, Kovacs S, Theys T, et al. Virtual brain grafting: Enabling whole brain parcellation in the presence of large lesions. Neuroimage 2021, 229: 117731.
Olson RA, Bobinski MA, Ho A, Goddard KJ. Oncologists’ view of informed consent and shared decision making in paediatric radiation oncology. Radiother Oncol 2012, 102: 210–213.
Lemmon ME, Barks MC, Bansal S, Bernstein S, Kaye EC, Glass HC, et al. The ALIGN Framework: A Parent-Informed Approach to Prognostic Communication for Infants With Neurologic Conditions. Neurology. 2023, 100(8): e800–e807. https://doi.org/10.1212/WNL.0000000000201600.
Ajithkumar T, Price S, Horan G, Burke A, Jefferies S. Prevention of radiotherapy-induced neurocognitive dysfunction in survivors of paediatric brain tumours: The potential role of modern imaging and radiotherapy techniques. Lancet Oncol 2017, 18: e91–e100.
Ayoub R, Ruddy RM, Cox E, Oyefiade A, Derkach D, Laughlin S, et al. Assessment of cognitive and neural recovery in survivors of pediatric brain tumors in a pilot clinical trial using metformin. Nat Med 2020, 26: 1285–1294.
Szulc-Lerch KU, Timmons BW, Bouffet E, Laughlin S, de Medeiros CB, Skocic J, et al. Repairing the brain with physical exercise: Cortical thickness and brain volume increases in long-term pediatric brain tumor survivors in response to a structured exercise intervention. Neuroimage Clin 2018, 18: 972–985.
Yeh FC, Panesar S, Fernandes D, Meola A, Yoshino M, Fernandez-Miranda JC, et al. Population-averaged atlas of the macroscale human structural connectome and its network topology. Neuroimage 2018, 178: 57–68.
Acknowledgements
During the literature review phase, C.S. was funded by the Fonds voor Wetenschappelijk Onderzoek for a senior post-doctoral fellowship. PCF is supported by funding from the Bernard Wolfe Health Neuroscience Fund (206368/Z/17/Z). His research is also supported by the NIHR Cambridge Biomedical Research Centre (BRC-1215-20014).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to declare.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sleurs, C., Fletcher, P., Mallucci, C. et al. Neurocognitive Dysfunction After Treatment for Pediatric Brain Tumors: Subtype-Specific Findings and Proposal for Brain Network-Informed Evaluations. Neurosci. Bull. 39, 1873–1886 (2023). https://doi.org/10.1007/s12264-023-01096-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12264-023-01096-9