Abstract
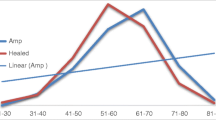
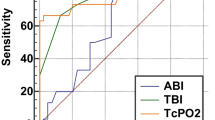
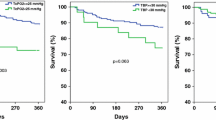
Foot ulcer is a common complication of diabetes mellitus. The co-existence of peripheral arterial disease (PAD) increases the risk of non-healing of the ulcer. Ankle brachial index (ABI) and transcutaneous partial pressure of oxygen (TcPO2) are two tests used to assess the vascularity of the foot, using two different parameters. This study was done to compare the sensitivity, specificity and diagnostic accuracy of ABI and TcPO2 and to find out which of these is a better predictor of healing in diabetic foot ulcers in patients without palpable foot pulses. The hospital-based longitudinal study was done from March 2016 to March 2018 among 121 adult patients diagnosed with diabetic foot ulcer without palpable peripheral pulses who fit the inclusion and exclusion criteria. Vascularity of the foot in these patients was assessed using ABI and TcPO2. The participants were followed up for 3 months, and the healing status was recorded. The mean (SD) age of patients was 64.99 (10.03) years. Out of 121 patients, 89 were men and 32 were women. The mean ABI in healed and non-healed group were significantly different (P value < 0.001). TcPO2 also showed significant difference in healed and non-healed groups (P value < 0.001). The values of 0.65 in receiver operating characteristic (ROC) curve showed optimal sensitivity (86.1%) and specificity (75.5%) for ABI. ROC curve with a TcPO2 cut-off value of 27.5 mmHg had optimal sensitivity (84.7%) and specificity (81.6%). Although sensitivity of TcPO2 and ABI is comparable (84.7% v 86.1%), specificity and diagnostic accuracy are better for TcPO2.


Similar content being viewed by others
References
Fard AS, Esmaelzadeh M, Larinjani B (2007) Assessment and treatment of diabetic foot ulcer. Int J Clin Pract 61(11):1931–1938
Armstrong EJ, Walternerger J, Rogers JH (2014) Percutaneous coronary intervention in patients with diabetes: current concepts and future directions. J Diabetes Sci Technol 8(3):581–589
Wild SH, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030: response to Rathman and Giani. Diabetes Care 27(10):2569–2570
Saad N, Elhadedy K, Ramadan N, Mohmady O, Farid M (2013) The prevalence and risk categorisation of diabetic foot complications in cohort group in Beni Suif, Egypt. Life Sci J 3:10
Jain AKC (2012) A new classification of diabetic foot complications: a simple and effective teaching tool. J Diabetic Foot Complicat 4:1–5
Amogne W, Reja A, Amare A (2011) Diabetic foot disease in Ethiopian patients: a hospital based study. Ethiop J Health Sci 25(1):17–21
Abbot CA, Carrington AL, Ashe H, Bath S, Every LC, Griffiths J et al (2002) The north-west diabetes foot care study: incidence of, and risk factors for, new diabetic foot ulceration in a community-based patient cohort. Diabet Med 19(5):377–384
Kumhar M, Dara N, Saini T (2014) Foot wear and footcare knowledge—an independent risk factor for diabetic foot in Indian diabetics. Indian Med Gazette 148(1):25–28
Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K, Edmonds M, Holstein P, Jirkovska A, Mauricio D, Ragnarson Tennvall G, Reike H, Spraul M, Uccioli L, Urbancic V, van Acker K, van Baal J, van Merode F, Schaper N (2007) High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia. 50(1):18–25
Nyamu PN, Otieno CF, Amayo EO, McLigeyo SO (2003) Risk factors and prevalence of diabetic foot ulcers at Kenyatta National Hospital, Nairobi. East Afr Med J 80(1):36–43
Prompers L, Schaper N, Apelqvist J, Edmonds M, Jude E, Mauricio D, Uccioli L, Urbancic V, Bakker K, Holstein P, Jirkovska A, Piaggesi A, Ragnarson-Tennvall G, Reike H, Spraul M, van Acker K, van Baal J, van Merode F, Ferreira I, Huijberts M (2008) Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia 51(5):747–755
Siersma V, Thorsen H, Holstein PE, Kars M, Apelqvist J, Jude EB, Piaggesi A, Bakker K, Edmonds M, Jirkovska A, Mauricio D, Ragnarson Tennvall G, Reike H, Spraul M, Uccioli L, Urbancic V, van Acker K, van Baal J, Schaper NC (2013) Importance of factors determining the low health-related quality of life in people presenting with a diabetic foot ulcer: the Eurodiale study. Diabet Med 30(11):1382–1387
Lazarides MK, Giannoukas AD (2007) The role of hemodynamic measurements in the management of venous and ischemic ulcers. Int J Low Extrem Wounds 6(4):254–261
Renner R, Simon JC (2008) Current therapeutic options of chronic leg ulcers. JDDG 6(5):389–401
Pecoraro RE, Reiber GE, Burgess EM (1990) Pathways to diabetic limb amputation: basis for prevention. Diabetes Care 13(5):513–521
Beckert S, Pietsch AM, Küper M, Wicke C, Witte M, Königsrainer A, Coerper S (2009) MAID: a prognostic score estimating probability of healing in chronic lower extremity wounds. Ann Surg 249(4):677–681
Beckert S, Witte M, Wicke C, Königsrainer A, Coerper S (2006) A new wound-based severity score for diabetic foot ulcers: a prospective analysis of 1,000 patients. Diabetes Care 29(5):988–992
Lalithambika CV, Nisha B, Saraswathy L, Varma AK, Jose A, Sundaram KR (2014) Ankle brachial index and transcutaneous partial pressure of oxygen as predictors of wound healing in diabetic foot ulcers. J Diabetic Foot Complicat 6(2):54–59
Veves A, Murray HJ, Young MJ, Boulton AJ (1992) The risk of foot ulceration in diabetic patients with high foot pressure: a prospective study. Diabetologia. 35(7):660–663
Yang C, Weng H, Chen L, Yang H, Luo G, Mai L, Jin G, Yan L (2013) Transcutaneous oxygen pressure measurement in diabetic foot ulcers: mean values and cut-point for wound healing. J Wound Ostomy Continence Nurs 40(6):585–589
Kalani M, Brismar K, Fagrell B, Ostergren J, Jörneskog G (1999) Transcutaneous oxygen tension and toe blood pressure as predictors for outcome of diabetic foot ulcers. Diabetes Care 22(1):147–151
Park SC, Choi CY, Ha YI, Yang HE (2012) Utility of toe-brachial index for diagnosis of peripheral artery disease. Arch Plast Surg 39(3):227–231
Ix JH, Miller RG, Criqui MH, Orchard TJ (2012) Test characteristics of the ankle-brachial index and ankle-brachial difference for medial arterial calcification on X-ray in type 1 diabetes. J Vasc Surg 56(3):721–727
Aubert CE, Cluzel P, Kemel S, Michel PL, Lajat-Kiss F, Dadon M, Hartemann A, Bourron O (2014) Influence of peripheral vascular calcification on efficiency of screening tests for peripheral arterial occlusive disease in diabetes—a cross-sectional study. Diabet Med 31(2):192–199
Bacharach JM, Rooke TW, Osmundson PJ, Gloviczki P (1992 Mar) Predictive value of transcutaneous oxygen pressure and amputation success by use of supine and elevation measurements. J Vasc Surg 15(3):558–563
Author information
Authors and Affiliations
Contributions
All authors were involved in the clinical care of the patient. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
The study was approved by the Institute Ethical Committee (IEC) of Malabar Institute of Medical Sciences Limited, Kozhikode.
Conflict of Interest
The authors declare no potential conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thottiyen, S., Kuruvilla, R., George, A. et al. Ankle Brachial Index vs Transcutaneous Partial Pressure of Oxygen for Predicting Healing of Diabetic Foot Ulcers with Peripheral Arterial Disease: a Comparative Study. Indian J Surg 85 (Suppl 1), 183–188 (2023). https://doi.org/10.1007/s12262-020-02587-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02587-z