Abstract
Aims
Ankle–brachial index (ABI) is the most commonly used test when diagnosing peripheral vascular disease and is considered a marker for cardiovascular risk. Transcutaneous oxygen pressure (TcPO2), a test associated with microvascular function, has in several studies shown better correlation with diabetic foot ulcer (DFU) healing. Whether a low TcPO2 could be a marker for mortality in the high-risk population of DFU patients has not been evaluated before. The aim of this study was to evaluate the predictive value of TcPO2 in comparison with ABI and toe blood pressure (TBP) on 1-year mortality in type 2 diabetes patients with DFU.
Methods
Type 2 diabetes patients aged ≤ 90 years, with one DFU who attended our multidisciplinary DFU-unit during year 2013–2015 and were screened with TcPO2, ABI and TBP were retrospectively evaluated. One-year mortality was assessed from the national death register in Sweden.
Results
A total of 236 patients (30% women) with a median age of 76 (69–82) years were evaluated in this study. Within 1 year, 14.8% of the patients died. TcPO2 < 25 mmHg was associated with a higher 1-year mortality compared with TcPO2 ≥ 25 mmHg (27.7 vs. 11.6%, p = 0.003). TBP and ABI did not significantly influence 1-year mortality. In a Cox regression analysis adjusted for confounders, TcPO2 was independently predicting 1-year mortality with a hazard ratio for TcPO2 < 25 mmHg of 2.8 (95% CI 1.34–5.91, p = 0.006).
Conclusions
This study indicates that a low TcPO2 is an independent prognostic marker for 1-year mortality among patients with type 2 diabetes and DFU.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic foot ulcers (DFU) are a common complication of diabetes mellitus, associated with both an increased risk of amputations in the lower limb and a higher risk of cardiovascular disease and death [1,2,3]. Peripheral vascular disease (PVD) is frequently contributing, together with peripheral neuropathy in the development of a DFU, and the presence of PVD is considered a predictor of worse outcome both for ulcer healing and survival [4, 5]. Ankle–brachial index (ABI) is the most commonly used test for the diagnosis of PVD and has also been associated with increased cardiovascular risk in the general population [6]. However, in patients with diabetes, both the diagnostic and the predictive value of ABI may be limited due to a high prevalence of false-negative values as a result of medial artery calcification [7,8,9]. Further, ABI does not reflect microvascular dysfunction, a condition often seen in patients with DFU. Transcutaneous oxygen pressure (TcPO2) is a non-invasive method measuring tissue perfusion and is considered to better reflect the microvascular status in the skin. The International Working Group on the Diabetic Foot (IWGDF) recommend in their guideline document, urgent vascular imaging and if feasible revascularisation when TBP < 30 mmHg or TcPO2 < 25 mmHg, as patients with higher levels are more likely to heal their ulcers [10]. It has previously been demonstrated a plausible association between TcPO2 and mortality in patients with diabetes, but without significant PVD, or ongoing DFUs [11]. Also, in a study by Gazzaruso et al. [12], a low TcPO2 has been considered a risk factor for major cardiovascular events (MACEs) in patients with type 2 diabetes, but without a history of foot ulcer, or previous cardiovascular disease. Whether a low TcPO2 could be a marker for mortality in the high-risk population of DFU patients has not been evaluated before. The aim of this study was to evaluate the predictive value of TcPO2, in comparison with ABI and TBP, on 1-year all-cause mortality in patients with type 2 diabetes and DFU.
Methods
For this study, we retrospectively enrolled patients with type 2 diabetes, aged ≤ 90 years, with at least one DFU who visited our DFU-unit between year 2013–2015. All patients were examined with TcPO2, ABI and TBP, measured with Periflux System 5000 diagnostic instrument (Perimed AB, Stockholm Sweden). These non-invasive assessments are routine in all referrals at our DFU unit.
TcPO2-measurements were performed at the dorsum of both feet, while patient was breathing ambient air, in a resting supine position at room temperature, between 21 °C and 24 °C. The site on the foot was carefully cleaned before the transducer was applied to the skin, using adhesive rings and contact liquid, supplied by the manufacturer. The measurement was performed after calibration and preheating of the transducer to approximate 44 °C. Patients were stratified according to TcPO2 < and ≥ 25 mmHg, and to evaluate mortality related to different TcPO2 levels, patients were also grouped according to TcPO2 quartiles.
The systolic ankle pressure and TBP were also evaluated during resting, in a supine position. Three measurements were performed on each foot and averaged. ABI was calculated by dividing the systolic ankle pressure with the systolic arm pressure, and ABI 0.9–1.3 was considered normal [13]. TBP was measured at the great toe, and TBP < 30, as well as < 50 mmHg, was used in the analyses. The lowest value (of ABI, TBP and TcPO2) of the two legs was used in mortality analysis, while the value of the affected foot was used when analysing ulcer healing.
Baseline characteristics were assessed from patient’s medical records and included age, gender, diabetes duration, as well as co-morbidities, such as history of hypertension, hyperlipidaemia, cardiovascular disease (CVD), as well as concomitant medication, and laboratory data (HbA1c, LDL-cholesterol and creatinine). CVD was defined as verified myocardial infarction, angina pectoris, heart failure or cerebral vascular disease. Hypertension was defined as blood pressure ≥ 140/90, or ongoing treatment with antihypertensive drugs. Hyperlipidaemia was defined as LDL > 2.5 mmol/l, or the ongoing treatment with cholesterol-lowering drugs. Glomerular filtration rate (eGFR) was estimated from plasma creatinine, using the modification of diet in renal disease (MDRD) equation [14].
All patients were treated according to international guidelines, at our multidisciplinary diabetic foot clinic, and were evaluated for vascular intervention when indicated. Ulcer healing, defined as complete epithelialisation within 12 weeks, and above-ankle amputation during follow-up were assessed from patients’ charts. Mortality data were obtained from the National Death Registry of Sweden. Approval of the study was given by the Ethics Committee in Lund, Sweden.
Statistical analysis
Continuous data are expressed as median and interquartile ranges (IQR; 25–75 percentile), and to assess differences Mann–Whitney U tests were performed. Categorical data are expressed as percentages, and Fisher’s exact test was used to compare differences. Survival analyses were performed with Kaplan–Meier estimates, and significances calculated with log-rank tests. A Cox regression analysis was performed, to adjust for confounding factors. Those factors with a significant (p < 0.05), or nearly significant (p < 0.1) difference between groups at baseline, as well as those with a significant association with mortality in the univariate analysis, were stepwise entered in a multivariate Cox model. Only those variables that changed the p value of our variables of interest, or significantly predicted mortality, were kept in the final model. The results of the Cox analysis are given as Hazard ratios (HRs) with 95% confidence interval (CI). All statistical analyses were performed using SPSS program (IBM, version 22). A two-sided p value < 0.05 was taken as statistical significant.
Results
We enrolled 236 type 2 diabetes patients with DFU, with a median age of 76 years (69–82), visiting our multidisciplinary diabetic foot clinic between year 2013 and 2015. A total number of 47 patients had a baseline TcPO2 < 25 mmHg, and among them, the probability for healing was low and only 8.8% successfully healed their ulcers after 12 weeks. Further, these patients suffered an increased risk of above-ankle amputations (23.4 vs. 4.2%, in TcPO2 ≥ 25 mmHg, p = 0.001). Minor amputation or auto-amputation was performed in 17 (9.0%) patients during follow-up in the group with TcPO2 ≥ 25 mmHg, compared to 6 (12.8%) in the TcPO2 < 25 mmHg group (n.s). Baseline characteristics, as well as healing, and major amputation rates of the study population, and of patients stratified by TcPO2 < and ≥ 25 mmHg, are given in Table 1. ABI < 0.9 or > 1.3 was significantly associated with worse ulcer outcome (12-week healing rate of 15.7 vs. 32.7%, in patients with normal ABI, p = 0.004), but no significant association between ulcer healing and TBP was found (both < 30 mmHg and < 50 mmHg analysed). Within the population of patients with TcPO2 < 25 mmHg, the revascularisation rate during follow-up was 25.5%. Additional 21.3% were vascular assessed, but intervention was not manageable, a decision made by a vascular surgeon. The remaining 53.2% (n = 25) of patients in TcPO2 < 25 mmHg were separately evaluated concerning plausible explanations why vascular diagnostics or revascularisation was not performed (Table 2).
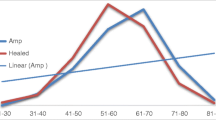
After 1 year of follow-up, 35 patients were deceased (14.8%). Patients who died within 1 year were significantly older [81 (75–84) vs. 75 (68–82) years old, p = 0.005] and had worse renal function, compared to survivors [eGFR 50 (26–66) vs. 63 (46–83) ml min−1 1.73 m2, p = 0.002]. TcPO2 < 25 mmHg was significantly associated with a higher 1-year mortality rate (27.7 vs. 11.6%, p = 0.003), as demonstrated in Fig. 1a. The impact of different TcPO2 levels on mortality is illustrated in Fig. 2. There was a not significant trend (p = 0.061) in the Kaplan–Meier analysis of worse survival rates in patients with TBP < 30 mmHg (Fig. 1b). ABI < 0.9 or > 1.3 was not linked to a higher mortality rate (Fig. 1c). There was a trend towards better 1-year survival among patients with TcPO2 < 25 mmHg who underwent a revascularisation procedure (91.7 vs. 65.7%, in patients not re-vascularised, p = 0.094). To adjust for confounders, a Cox proportional analysis was performed. The following factors (age, gender, eGFR, 3 months ulcer healing, revascularisation and above-ankle amputation), that either differed, or nearly differed, between groups at baseline, or was significantly associated with mortality in a univariate analysis were entered stepwise into a multivariate Cox model, together with our variables of interest. Of these plausible confounding factors, only age and renal function (eGFR) were significantly predicting mortality, and thus kept in the final model together with TcPO2 and TBP. ABI, revascularisation and ulcer healing at 3 months did not predict mortality or were significant confounders, and consequently, not entered in the final Cox analysis. There were a few cases of missing data, and these were consequently censored in the Cox analysis (n = 2 in ulcer healing at 3 months and n = 2 in eGFR). The result of the final multivariate Cox analysis is given in Table 3, and as shown, a TcPO2 < 25 mmHg was an independent predictor for 1-year mortality with a HR of 2.8 (95% CI 1.34–5.91, p = 0.006). Also, when analysing TcPO2 as a continuous variable, a significant association between increased survival with each mmHg increasing TcPO2 level was found. TBP was not an independent predictor for mortality.
One-year mortality (%) in patients divided into different quartiles of TcPO2 and HR calculated for each quartile. Q1 (reference group): ≥ 52 mmHg, Q2: 41–51 mmHg, Q3: 29–40 mmHg, Q4: ≤ 28 mmHg. Pooled comparison (log rank) p = 0.032. For separate comparisons in a univariate Cox regression model: Q1 versus Q4: HR 3.4 (1.2–9.4), p = 0.018. Q1 versus Q3: HR 2.0 (0.67–5.9), ns. Q1 versus Q2: HR 1.2 (0.4–4.0), ns
Discussion
TcPO2 has in several studies been associated with ulcer healing and has in previously published studies been associated with cardiovascular events and mortality in patients with type 2 diabetes, but without DFU and/or a history of previous CVD [11, 12, 15,16,17]. Our study is the first to demonstrate that TcPO2 also may be a predictor for mortality in the high-risk population of patients with DFUs, with a 2.8-folded increase in 1-year mortality among patients with TcPO2 < 25 mmHg. We demonstrated a continuous relation between TcPO2 levels and survival, with increasing survival for each mmHg higher TcPO2. Today, the current consensus among experts is that ulcer healing more likely occurs when TcPO2 ≥ 25 mmHg and TBP ≥ 45 mmHg, and urgent vascular imaging should be considered when TcPO2 < 25 mmHg or TBP < 30 mmHg [10]. In our study, 91.8% of our patients with baseline TcPO2 < 25 mm Hg failed to heal their ulcers in 3 months, a result similar with others. In the study by Pecoraro et al. [18], there was a 39-fold increase in healing failure if TcPO2 was < 20 mmHg. Kalani et al. [15], evaluated the threshold of TcPO2 < 25 mmHg, and found impaired healing in 31 out of 34 ulcers (91.2%), compared to improvement in ulcer area in 34 of 37 patients with TcPO2 ≥ 25 mmHg. In the Kalani study, ulcer improvement seemed to be more prevalent, compared with our results, but as they evaluated improvement (defined as a decrease in ulcer area of 25%) after 12 months, instead of complete epithelisation after 3 months, as we did, it is difficult to compare these results with ours [15]. In another study, evaluating hyperbaric oxygen therapy and wound healing, no ulcer healed when TcPO2 was < 25 mmHg [16].
We observed a high rate of above-ankle amputations (23.4%) in the group of people with TcPO2 < 25 mmHg (median TcPO2 11 (5–22) mmHg). Faglia et al. [17] reported major amputation rates of 9.8% in their entire cohort, consisting of patients with PVD (defined as ankle pressure < 70 mmHg, TcPO2 < 50 mmHg or obstruction identified at duplex scanning). In their study, the prediction probability of above-the-ankle amputation correlated to the level of TcPO2 (after revascularisation), with a probability of 2.6, 6.1, 22.5, 44.0 and 68.0% when TcPO2 was 40–49, 30–39, 20–29, 10–19 and < 10 mmHg, respectively. We did only report baseline TcPO2, which is a limitation, and reported a total amputation rate of 8.1% in our entire cohort, with a median TcPO2 of 41 (28–52). In a separate analysis of patients with TcPO2 < 50 mmHg (n = 174), the rate increased to 9.8%, similar to the result by Faglia et al. Patients who undergo major amputations are considered to even higher mortality rates, but neither above-ankle amputations nor healing failure was associated with 1-year mortality or was confounding the predictive value of TcPO2 on mortality, in our study [19,20,21]. TBP or ABI were not significantly associated with mortality in our study, which is in contrast to previous results. In a study by Zobel et al. [22], a significant association between toe–brachial index (TBI), ABI and mortality was found. Our cohorts differed, however, in baseline criteria as they included patients with type 2 diabetes and microalbuminuria, but no clinical signs of CVD, compared to our unselected high-risk population of DFU patients. Further, follow-up time was 6 years in the study by Zobel, compared to 1 year in our study. Therefore, one can speculate on whether the trend towards worse outcome seen among patients with TBP < 30 mmHg, would have significantly affect mortality in a longer perspective. Another study, including 81 type 2 diabetes with a history of myocardial infarctions, evaluated the risk of recurrent MACE when TBP < 50 mmHg and reported a HR of 3.83 (1.45–10.1) [23]. Further, in the Hoorn study, a population-based cohort study, including 155 patients with, and 469 patients without type 2 diabetes, Hanssen et al. [24] demonstrated a significant association between ABI < 0.9 and all-cause mortality in both patients with and without diabetes, after a median follow-up time of 17.2 years. Our present study, evaluating 1-year mortality in the high-risk population of patients with type 2 diabetes and DFU indicates that TcPO2 might be a useful tool for risk assessment, with a prognostic value in the short-term perspective, superior compared to ABI and TBP.
Concerning revascularisation, the observed rate of 25.5% among patients with TcPO2 < 25 mmHg is considerably low. Additional 21.3% performed diagnostic imaging and were assessed by a vascular surgeon, but were not amenable for revascularisation. More than half of the patients with TcPO2 < 25 mmHg did not, however, perform a complete diagnostic assessment, which is inconsistent with the recommendation by IWGDF. When evaluating those cases separately, we found cases with prompt ulcer improvement, as well as patients with severe comorbidity, including renal failure, among these individuals, but also a few cases with unknown reasons were limb ischaemia with possibility for revascularisation might have been under-diagnosed. Patients with TcPO2 < 25 mmHg who underwent revascularisation procedures had a trend towards better survival, but in the 1-year perspective this finding did not reach significance, or was confounding our results. In a study by Faglia et al. [21], patients with identified critical limb ischaemia had higher survival rates after successful intervention, during 6 years of follow-up. However, when the authors adjusted for confounders in a Cox model, only age turned out to predict mortality in that study [21]. Our low revascularisation rate is, however, an important observation, but not unique in our setting. In a German study by Malyar et al. [25], only 18% of the patients were re-vascularised, and another 25% were evaluated with angiography. Also, in the EURODIALE study, vascular imaging was only performed in 56% of patients with severe limb ischaemia, and of them, only 43% were re-vascularised [26]. This might reflect the complexity of patients with DFUs, where several factors, and often severe comorbidity need to be considered before intervention. Nevertheless, further optimising the multidisciplinary approach, when managing DFU patients, is desirable.
We can only speculate about the mechanisms behind the increase in all-cause mortality, among our patients with low TcPO2. Traditionally cardiovascular risk factors, such as smoking, hypertension and previous CVD, did not significantly relate to either TcPO2 or mortality, in our study. One possible explanation could be that a low TcPO2 on the foot might serve as a marker for impaired microcirculation in general, with a higher burden of microvascular complications. It has previously been shown by Huang et al. [27], a significant negative association between TcPO2 and microvascular events (albuminuria and distal polyneuropathy) in type 2 diabetes patients, with a tenfold risk of microvascular complications when TcPO2 was < 50 mmHg. Similar, our study demonstrated a significant association between a low TcPO2 and renal impairment, and a low eGFR did also independently associated with mortality, results previously shown by many [28,29,30]. eGFR did not, however, confound the impact of TcPO2 on mortality in the Cox analysis. Another possible mechanism contributing to the increased mortality rate among patients with low TcPO2, could be a higher prevalence of neuropathy [31]. In a study by Arora et al. [32], a lower TcPO2 in the forearm and foot was found in patients with diabetic neuropathy, compared to non-neuropathic patients, as well as healthy subjects. Another study by Pfutzner et al. [33] indicated a relation between microvascular disturbance and small fibre neuropathy. As small fibre neurons are involved both in peripheral neuropathy, and in the serious diabetes complication cardiac autonomic neuropathy, the latter could be a plausible mechanism contributing to increased mortality in patients with microvascular impairment [34]. In our study, we lack quantitative data on neuropathy, and thus, we can only speculate on a causality.
Our study has some strengths and limitations that need to be stated. The study design as a retrospective cohort study might be afflicted with bias, and the findings might only serve as hypothesis generating for future prospective studies. However, one strength is our relatively large cohort size, which is representative of the DFU-population as most patients with DFUs in our region are transferred to our multidisciplinary DFU-unit. Further, the vast majority of our patients are routinely screened with TcPO2, TBP and ABI and are seen at a regularly basis at our department, until ulcer healing. Mortality data are accurate since all deaths in Sweden are registered in our National Death Register. We only report all-cause mortality, due to the low frequency of autopsies in Sweden, and thus, we can thus only speculate on underlying cause of death. The lack of quantitative data on neuropathy and albuminuria is a limitation, and the association between TcPO2 and cardiac autonomic neuropathy needs further studies. Several factors, besides microvascular function, might contribute to a low TcPO2 that we did not correct for, such as advanced pulmonary diseases or heart failure with chronic hypoxia, as well as local factors such as tissue oedema and inflammation. Only one patient in the TcPO2 < 25 mmHg group was suffering from chronic obstructive pulmonary disease, but since we did not measure oxygen saturation, undiagnosed hypoxia could have affected our results.
Besides limitations, our novel findings indicate an independent association between a low TcPO2 and increased 1-year mortality in patients with type 2 diabetes and DFU. This suggests that screening with TcPO2 might improve identification of DFU patients with urgent need for both vascular intervention and intensive cardiovascular risk factor assessment.
Abbreviations
- ABI:
-
Ankle–brachial index
- CVD:
-
Cardiovascular disease
- DFU:
-
Diabetic foot ulcer
- eGFR:
-
Estimated glomerular filtration rate
- HR:
-
Hazard ratio
- IWGDF:
-
The International Working Group on the Diabetic Foot
- IQR:
-
Interquartile range
- MACEs:
-
Major cardiovascular events
- MDRD:
-
Modification of diet in renal disease
- PVD:
-
Peripheral vascular disease
- TcPO2 :
-
Transcutaneous oxygen pressure
- TBP:
-
Toe blood pressure
References
Brownrigg JR, Davey J, Holt PJ et al (2012) The association of ulceration of the foot with cardiovascular and all-cause mortality in patients with diabetes: a meta-analysis. Diabetologia 55:2906–2912
Moulik PK, Mtonga R, Gill GV (2003) Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabetes Care 26:491–494
Abbott CA, Carrington AL, Ashe H et al (2002) The North-West Diabetes Foot Care Study: incidence of, and risk factors for, new diabetic foot ulceration in a community-based patient cohort. Diabet Med 19:377–384
Criqui MH, Langer RD, Fronek A et al (1992) Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med 326:381–386
Prompers L, Huijberts M, Apelqvist J et al (2007) High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia 50:18–25
Resnick HE, Carter EA, Lindsay R et al (2004) Relation of lower-extremity amputation to all-cause and cardiovascular disease mortality in American Indians: the Strong Heart Study. Diabetes Care 27:1286–1293
Potier L, Abi Khalil C, Mohammedi K, Roussel R (2011) Use and utility of ankle brachial index in patients with diabetes. Eur J Vasc Endovasc Surg 41:110–116
Nam SC, Han SH, Lim SH et al (2010) Factors affecting the validity of ankle–brachial index in the diagnosis of peripheral arterial obstructive disease. Angiology 61:392–396
Potier L, Halbron M, Bouilloud F et al (2009) Ankle-to-brachial ratio index underestimates the prevalence of peripheral occlusive disease in diabetic patients at high risk for arterial disease. Diabetes Care 32:e44
Bakker K, Apelqvist J, Lipsky BA, Van Netten JJ, Schaper NC (2016) The 2015 IWGDF guidance on the prevention and management of foot problems in diabetes. Int Wound J 13:1072
Carrington AL, Shaw JE, Van Schie CH, Abbott CA, Vileikyte L, Boulton AJ (2002) Can motor nerve conduction velocity predict foot problems in diabetic subjects over a 6-year outcome period? Diabetes Care 25:2010–2015
Gazzaruso C, Coppola A, Falcone C et al (2013) Transcutaneous oxygen tension as a potential predictor of cardiovascular events in type 2 diabetes: comparison with ankle–brachial index. Diabetes Care 36:1720–1725
Hinchliffe RJ, Brownrigg JR, Apelqvist J et al (2016) IWGDF guidance on the diagnosis, prognosis and management of peripheral artery disease in patients with foot ulcers in diabetes. Diabetes Metab Res Rev 32(Suppl 1):37–44
Levey AS, Coresh J, Greene T et al (2006) Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 145:247–254
Kalani M, Brismar K, Fagrell B, Ostergren J, Jorneskog G (1999) Transcutaneous oxygen tension and toe blood pressure as predictors for outcome of diabetic foot ulcers. Diabetes Care 22:147–151
Londahl M, Katzman P, Hammarlund C, Nilsson A, Landin-Olsson M (2011) Relationship between ulcer healing after hyperbaric oxygen therapy and transcutaneous oximetry, toe blood pressure and ankle–brachial index in patients with diabetes and chronic foot ulcers. Diabetologia 54:65–68
Faglia E, Clerici G, Caminiti M, Quarantiello A, Curci V, Morabito A (2007) Predictive values of transcutaneous oxygen tension for above-the-ankle amputation in diabetic patients with critical limb ischemia. Eur J Vasc Endovasc Surg 33:731–736
Pecoraro RE, Ahroni JH, Boyko EJ, Stensel VL (1991) Chronology and determinants of tissue repair in diabetic lower-extremity ulcers. Diabetes 40:1305–1313
Fagher K, Nilsson A, Londahl M (2015) Heart rate-corrected QT interval prolongation as a prognostic marker for 3-year survival in people with type 2 diabetes undergoing above-ankle amputation. Diabet Med 32:679–685
Tentolouris N, Al-Sabbagh S, Walker MG, Boulton AJ, Jude EB (2004) Mortality in diabetic and nondiabetic patients after amputations performed from 1990 to 1995: a 5-year follow-up study. Diabetes Care 27:1598–1604
Faglia E, Clerici G, Caminiti M et al (2010) Mortality after major amputation in diabetic patients with critical limb ischemia who did and did not undergo previous peripheral revascularization: data of a cohort study of 564 consecutive diabetic patients. J Diabetes Complications 24:265–269
Zobel EH, von Scholten BJ, Reinhard H et al (2017) Toe–brachial index as a predictor of cardiovascular disease and all-cause mortality in people with type 2 diabetes and microalbuminuria. Diabetologia 60:1883–1891
Martin-Fuentes M, Herranz L, Saez-de-Ibarra L, Pallardo LF (2015) Low toe–brachial pressure index predicts increased risk of recurrent cardiovascular disease in type 2 diabetes. Diabetes Care 38:e53–e54
Hanssen NM, Huijberts MS, Schalkwijk CG, Nijpels G, Dekker JM, Stehouwer CD (2012) Associations between the ankle–brachial index and cardiovascular and all-cause mortality are similar in individuals without and with type 2 diabetes: 19-year follow-up of a population-based cohort study. Diabetes Care 35:1731–1735
Malyar NM, Freisinger E, Meyborg M et al (2016) Amputations and mortality in in-hospital treated patients with peripheral artery disease and diabetic foot syndrome. J Diabetes Complications 30:1117–1122
Prompers L, Huijberts M, Apelqvist J et al (2008) Delivery of care to diabetic patients with foot ulcers in daily practice: results of the Eurodiale Study, a prospective cohort study. Diabet Med 25:700–707
Huang K, Ma Y, Wang J et al (2017) The correlation between transcutaneous oxygen tension and microvascular complications in type 2 diabetic patients. J Diabetes Complications 31:886–890
Afkarian M, Sachs MC, Kestenbaum B et al (2013) Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol 24:302–308
de Boer IH, Katz R, Cao JJ et al (2009) Cystatin C, albuminuria, and mortality among older adults with diabetes. Diabetes Care 32:1833–1838
Ninomiya T, Perkovic V, de Galan BE et al (2009) Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol 20:1813–1821
Malik RA, Newrick PG, Sharma AK et al (1989) Microangiopathy in human diabetic neuropathy: relationship between capillary abnormalities and the severity of neuropathy. Diabetologia 32:92–102
Arora S, Smakowski P, Frykberg RG et al (1998) Differences in foot and forearm skin microcirculation in diabetic patients with and without neuropathy. Diabetes Care 21:1339–1344
Pfutzner A, Forst T, Engelbach M et al (2001) The influence of isolated small nerve fibre dysfunction on microvascular control in patients with diabetes mellitus. Diabet Med 18:489–494
Festa A, D’Agostino R Jr, Rautaharju P, Mykkanen L, Haffner SM (2000) Relation of systemic blood pressure, left ventricular mass, insulin sensitivity, and coronary artery disease to QT interval duration in nondiabetic and type 2 diabetic subjects. Am J Cardiol 86:1117–1122
Funding
This study was supported by the Swedish Diabetes Foundation, Sydvästra Skånes Diabetesförening, Krapperup Foundation, Skåne county council’s research and development foundation and Faculty of Medicine (ALF), Lund University, Sweden. This study was supported by the Swedish Diabetes Foundation, Sydvästra Skånes Diabetesförening, Krapperup Foundation, Skåne county council’s research and development foundation and Faculty of Medicine (ALF), Lund University, Sweden.
Author information
Authors and Affiliations
Contributions
KF, PK and ML contributed to the design of the study. KF and ML performed data and statistical analysis. KF wrote, and all authors reviewed the article. ML is the guarantor of this work and is responsible for integrity and accuracy of data.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of Ethics Committee in Lund, Sweden and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Approval of the study was given by the Ethics Committee in Lund, Sweden.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Managed by Massimo Porta.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Fagher, K., Katzman, P. & Löndahl, M. Transcutaneous oxygen pressure as a predictor for short-term survival in patients with type 2 diabetes and foot ulcers: a comparison with ankle–brachial index and toe blood pressure. Acta Diabetol 55, 781–788 (2018). https://doi.org/10.1007/s00592-018-1145-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1145-8