Abstract
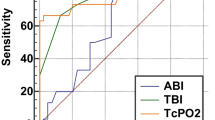
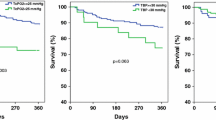
Diabetic foot ulcer (DFU) is the commonest condition for hospital admission and usually the starting point of most diabetic related lower limb amputations. Considering the significant role played by vascularity in the outcome of ulcer healing, we undertook this study to find out the comparative utility of commonly used vascular assessment methods. This study was a single center prospective non-randomized observational study, conducted for a period of 6 months, in diabetic patients presenting with foot ulcers of Wagner Grade II and III. The aim of our study was to compare the performances of ankle-brachial index (ABI) and transcutaneous partial pressure of oxygen (tcPO2) measurement in predicting wound healing in diabetic ulcers and to define the optimal cut-off value for Indian patients. Five hundred sixty-four patients were included in this study, with the mean age of 58 years. Eighty-seven patients (15%) had peripheral arterial occlusive disease. Four hundred seventy ulcers (83%) healed with the mean healing days of 42.6 days. Age, duration of diabetes, serum creatinine level, and presence of infection were the factors with negative impact in wound healing. In our study, ABI value of 0.6 was found to have 100% sensitivity and 70% specificity, and tcPO2 value of 22.5 was found to have 75% sensitivity and 100% specificity in predicting wound healing. Both ABI and tcPO2 are complementary, but tcPO2 is a better predictor for amputation while ABI is a better predictor for ulcer healing. While assessing the ischemic status of foot ulcer, the cut-off values should be higher in diabetics than non-diabetics.


Similar content being viewed by others
References
Viswanathan V, Thomas N, Tandon N, Asirvatham A, Rajasekar S, Ramachandran A, et al. Profile of diabetic foot complications and its associated complications—a multicentric study from India. J Assoc Phys India. 2005;53:933–6.
Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293:217–28.
Loslin EP. The menace of diabetic gangrene. N Engl J Med. 1934;211:16–20.
Potier L, Abi Khalil C, Mohammedi K, Roussel R. Use and utility of ankle brachial index in patients with diabetes. Eur J Vasc Endovasc Surg. 2011;41:110–6.
Chang CH, Peng YS, Chang CC, Chen MY. Useful screening tools for preventing foot problems of diabetics in rural areas: a cross-sectional study. BMC Public Health. 2013;13:612.
Aerden D, Massaad D, von Kemp K, van Tussenbroek F, Debing E, Keymeulen B, et al. The ankle-brachial index and the diabetic foot: a troublesome marriage. Ann Vasc Surg. 2011;25:770–7.
de Meijer VE, Van’t Sant HP, Spronk S, Kusters FJ, den Hoed PT. Reference value of transcutaneous oxygen measurement in diabetic patients compared with nondiabetic patients. J Vasc Surg. 2008;48:382–8.
Barnikol WK, Pötzschke H. A novel, non-invasive diagnostic clinical procedure for the determination of an oxygenation status of chronic lower leg ulcers using peri-ulceral transcutaneous oxygen partial pressure measurements: results of its application in chronic venous insufficiency (CVI). Ger Med Sci. 2012;10:Doc11.
Hutchison DC, Rocca G, Honeybourne D. Estimation of arterial oxygen tension in adult subjects using a transcutaneous electrode. Thorax. 1981;36:473–7.
Lalka SG, Malone JM, Anderson GG, Hagaman RM, McIntyre KE, Bernhard VM. Transcutaneous oxygen and carbon dioxide pressure monitoring to determine severity of limb ischemia and to predict surgical outcome. J Vasc Surg. 1988;7:507–14.
Arora NK, Pillai R, Dasgupta R, Garg PR. Whole-of-society monitoring framework for sugar, salt, and fat consumption and noncommunicable diseases in India. Ann N Y Acad Sci. 2014;1331:157–73.
Zimny S, Schatz H, Pfohl M. Determinants and estimation of healing times in diabetic foot ulcers. J Diabetes Complicat. 2002;16:327–32.
Wang C, Mai L, Yang C, Liu D, Sun K, Song W, et al. Reducing major lower extremity amputations after the introduction of a multidisciplinary team in patient with diabetes foot ulcer. BMC Endocr Disord. 2016;16:38.
Marston WA. Risk factors associated with healing chronic diabetic foot ulcers: the importance of hyperglycemia. Ostomy Wound Manage. 2006;52:26–8.
Markuson M, Hanson D, Anderson J, Langemo D, Hunter S, Thompson P, et al. The relationship between hemoglobin A(1c) values and healing time for lower extremity ulcers in individuals with diabetes. Adv Skin Wound Care. 2009;22:365–72.
Lee KM, Kim WH, Choi MSS. Risk factors of treatment failure in diabetic foot ulcer patients. Arch Plast Surg. 2013;40:123–8.
Akini B, Yesil S, Eraslan S. The effect of creatinine clearance on the short-term outcome of neuropathic diabetic foot ulcers. J Prim Care Diabetes. 2010;4:181–5.
Sohn MW, Budiman-Mak E, Lee TA, Oh E, Stuck RM. Significant J-shaped association between body mass index and diabetic foot ulcers. Diabetes Metab Res Rev. 2011;27:402–9.
Margolis DJ, Allen Taylor L, Hoffstad O, Berlin JA. Diabetic neuropathic foot ulcers: predicting which ones will not heal. Am J Med. 2003;115:627–31.
Margolis DJ, Kantor J, Santanna J, Strom BL, Berlin JA. Risk factors for delayed healing of neuropathic diabetic foot ulcers: a pooled analysis. Arch Dermatol. 2000;136:1531–5.
Mohan V, Premlatha G, Shastry NG. Peripheral vascular disease in non-insulin-dependent diabetes mellitus in south India. Diab Res Clin Pract. 1995;27:235–40.
Pendsey SP. Peripheral vascular disease: an Indian scenario. Diabtol Croat. 1998;27:153–6.
Jayaprakash P, Bhansali A, Dutta P, Ananthraman R. Magnitude of foot problems in diabetes in the developing world: a study of 1044 patients. Diab Med. 2009;26:939–42.
Parvez N, Dutta P, Ray P, Shah VN, Prakash M, Khandelwal M, et al. Microbial profile and utility of soft tissue, pus and bone cultures in diagnosing diabetic foot infections. Diabetes Technol Ther. 2012;14:669–74.
Sinahary K, Paul UK, Bhattacharyya AK, Pal SK. Prevalence of diabetic foot ulcers in newly diagnosed diabetes mellitus patients. J Indian Med Assoc. 2012;110:608–11.
Walters DP, Gatling W, Mullee MA, Hill RD. The prevalence, detection and epidemiological correlates of peripheral vascular disease: a comparison of diabetic and non-diabetic subjects in an English community. Diabet Med. 1992;9:710–5.
Al-Rubeaan K, Al Derwish M, Quizi S, Youssef AM, Subhani SM, Ibrahim HM, et al. Diabetic foot complications and their risk factors from a large retrospective cohort study. PLoS One. 2015;10:e0124446.
Bowling FL, Rashid TS, Boulton JM. Preventing and treating foot complications associated with diabetes mellitus. Nat Rev Endocrinol. 2015;11:606–16.
Lalithambika CV, Nisha B, Saraswathy L, Varma AK, Jose A, Sundaram KR. Ankle brachial index and transcutaneous partial pressure of oxygen as predictors of wound healing in diabetic foot ulcers. J Diabet Foot Complications. 2014;6:54–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Rajagopalan, C., Viswanathan, V., Rajsekar, S. et al. Diabetic foot ulcers—comparison of performance of ankle-brachial index and transcutaneous partial oxygen pressure in predicting outcome. Int J Diabetes Dev Ctries 38, 179–184 (2018). https://doi.org/10.1007/s13410-017-0580-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-017-0580-3