Summary
Peripheral T‑cell lymphomas (PTCL) are a heterogeneous group of rare lymphoid malignancies. Brentuximab vedotin plus cyclophosphamide, doxorubicin, and prednisone (BV+CHP, anti-CD30) is indicated as first-line treatment in the subgroup anaplastic large cell lymphoma (ALCL). Romidepsin plus cyclophosphamide, doxorubicin, vincristine, and prednisone (Ro-CHOP) is inferior to CHOP in PTCL; however, the subtype angioimmunoblastic T‑cell lymphoma (AITL) might favor Ro-CHOP. An increase of survival after consolidation with autologous stem cell transplantation (ASCT) in first line was found in a retrospective analysis. New antibody (anti-CD47 or anti-KIR3DL2) and CAR T/NK treatments are emerging and entering clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
When we speak of peripheral T‑cell lymphomas, we encounter a heterogenous group of rare lymphomas of over 29 different subdiagnoses according to the latest revised version from the World Health Organization (WHO) [1]. Despite this heterogeneity, the traditional treatment for most of the subtypes is still the anthracycline-based regiment CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone). After CHOP, approximately 60–70% of the patients achieve complete remission; however, 5‑year overall survival (OS) is only 32–45% due to the high rate of relapse or disease progression [2]. The median OS after relapse is 5.1 months [3].
New treatment options have been emerging over the last few years, though the low incidence (< 1 of 100,000 in Europe, and slightly higher in Asia [1]) and the strong heterogeneity is challenging in designing clinical trials with sufficient patient numbers and reasonable patient stratification.
Overview of PTCL subtypes
New characteristics and markers regarding prognosis within subtypes can be found in Table 1.
PTCL, NOS
The “waste basket” category is the largest category in PTCL, in which cases are assigned to if characteristics do not fit with specific subtypes.
AITL
The immune-rich subtype has typical mutations in TET2, RHOA, IDH2 und DNMT3A. These genes encode for epigenetic modifiers.
ALCL
The ALCL subtype is CD30 positive. The ALK+ group shows a chromosomal translocation of the ALK gene and occurs in patients < 30 years old. In the ALK group, this translocation is missing and occurs in the elderly.
New treatments beside CHOP
A retrospective study analyzed 224 patients from 1992–2019 and compared OS between conventional chemotherapy and new targeted treatment. New targeted treatment and improved genetic, epigenetic, and transcriptional characterization of distinct subtypes showed significantly longer OS over the past three decades [4].
One of the most promising emerging drugs against peripheral T cell lymphomas is brentuximab vedotin (BV). BV is an immune conjugate combining a CD30-antibody and the toxic mono-methyl-auristatin E (MME). In 2012, BV was approved by the US Food and Drug Administration (FDA) for the characteristically CD30-positive PTCL subtype, anaplastic large T cell lymphoma (ALCL).
In the ECHELON-2 study from Horwitz et al. in 2019, the global, double-blind, randomized, phase 3 trial showed frontline treatment with BV+CHP was superior to CHOP for 452 patients with CD30-positive peripheral T‑cell lymphomas [5]. The impressive results of CR responses of 68% for BV+CHP and 56% for CHOP and a significantly improved progression-free survival (PFS) of 48.8 months for BV+CHP compared to 20.8 months for CHOP prompted FDA-approval of BV+CHP as first-line treatment for CD30+ PTCL (Fig. 1). European Medicines Agency (EMA) guidelines are more restrictive and BV+CHP is indicated only in ALCL (characteristically CD30 positive) as first-line treatment.
ECHELON‑2 study. BV brentuximab-vedotin, C cyclophosphamide, H doxorubicin, P prednisone, O Vincristin (modified from [5])
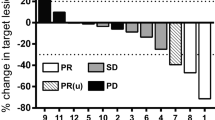
In the setting of relapsed or refractory PTCL, histone deacytelase inhibitors, such as belinostat and romidepsin showed responses of 13–17 months and achieved FDA approval in 2011 (but not EMA approval). These promising results lead to several combinational studies with HDAC inhibitors as the Ro-CHOP trial. The well-designed Ro-CHOP trial conducted by Bachy et al. from Lyon randomized 421 patients into a Ro-CHOP vs. a CHOP group. Unfortunately, the final results were disappointing and showed no significant improvement in OS and PFS for the Ro-CHOP group, but higher toxicities compared to the standard treatment of CHOP ([6]; Fig. 2a) These disillusioning results were repeated in an additional study, which had to be stopped due to insufficient responses and PFS (48% of the patients achieved PFS of 18 months) [7].
Ro-CHOP phase III study (from [6]) a Overall survival (OS). b Hazard ratio (HR), progression-free survival (PFS) according to specific subgroups. Ro Romidepsin, C cyclophosphamide, H doxorubicin, O Vincristin, P prednisone, 95% CI 95% confidence interval, IPI internatinal prognostic index, PIT prognostic index for T-cell lymphoma, HR hazard ratio
However, the response of the PTCL subgroup of AITL (angioimmunoblastic T‑cell lymphoma) to Ro-CHOP showed encouraging results. This observation aligns with previously found insights into the epigenetic deregulation in AITL due to mutations in the TET2 or DNMT3A genes, which are responsible for epigenetic modulation in T cells. These subgrouping results give promising insights into the effectiveness of Ro-CHOP in AITL, although further studies are still needed ([1, 6]; Fig. 2b).
The high mutational burden in the epigenetic modulator genes TET2 and DNMTR3 in AITL also provided the basis for further clinical studies testing the hypomethylating agent azacytidine. O’Connor et al. tested a combination of azacytidine with romidepsin and showed an ORR in a phase 1 trial of 73% and complete remissions in 55% in the setting of relapsed/refractory (r/r) AITL. In the next step, a randomized study compares orally applied azacytidine against romidepsin, gemcitabine or bendamustine monotherapy in r/r AITL (NCT03593018; 86 participants, recruiting closed).
Studies evaluating the role of autologous stem cell transplantation (SCT) are unfortunately discordant. Randomized clinical trials are still missing and retrospective evidence is “for” and “against”. There are a few prospective clinical trials, but because of diverse subtype inclusion comparisons are difficult.
Recently, Brink et al. analyzed 1427 patients < 65 years divided in two cohorts retrospectively and consolidation with ASCT in first-line setting significantly increased 5‑year OS (78% vs 45% without ASCT) in ALK-negative ALCL, AITL, and PTCL NOS [8].
To assess the clear role of autoSCT in PTCL a randomized clinical trial has been launched recently (TRANSCRIPT – NCT05444712, planned patients: 204, ECOG 0–2, including PTCL-NOS, TFH-TCL, ALCL-ALK neg).
Promising new treatment candidates
Peripheral T cell lymphoma, especially the angioimmunoblastic T‑cell lymphoma subtype, show histologically a rich environment of infiltrating immune cells. Malignant T cells cleverly escape these checkpoints. Unfortunately, conducted studies with PD‑1 inhibitors showed even contrary results in PTCL and disease progression was experienced.
Another approach is to block the CD47 glycoprotein, the “do-not-eat me” marker for macrophages, on PTCL cells, which is found to be overexpressed in some PTCL cases [9].
Furthermore, blocking the killer-cell immunoglobulin-like receptor KIR3DL2, which is found to be overexpressed in PTCL, showed efficacy in cutaneous T cell lymphoma. KIR3DL2 is also found on some nodal PTCL cases. The TELLOMAK phase II study is therefore testing the KIR3DL2-antibody IPH4102 in PTCL (NCT03902184) [10].
Targeting the SYK/JAK-signaling pathway, as cerdalutinib inhibits SYK, JAK1, JAK3 and Tyk2, and showed responses especially in TFH/AITL and ALCL subtypes. The SYK-signaling pathway is important for the malign transformation in T cells and is overactivated in 90% of ALCL, AITL and PTCL, NOS [11].
CAR T/NK
The emerging field of CAR‑T and NK (natural killer cells) treatment is also entering the field of T cell lymphoma. So far CAR-T/NK studies are still in a preclinical phase, but larger clinical studies are recruiting or underway. One of the major challenges in CAR‑T cells engineered for T cell lymphoma are fratricide effects—CAR‑T cells recognizing T‑cell antigens and targeting other CAR‑T cells. However, genetic modification of CAR-Ts might resolve this issue [12]. Another problem occurs regarding T cell aplasia: As the human immune system can compensate for a complete B‑cell deprivation, pan T‑cell aplasia leads to severe immunodeficiency.
An alternative approach targeting only malignant T cells is to focus on the exclusive expression of the T‑cell receptor β‑chain 1 or 2. Targeting only the malignant clone expressing one of the two T‑cell receptor β‑chains provides a substantial fraction of physiological T‑cells with the contrary T‑cell receptor β‑chain in the mouse model [13].
Other CAR-engineered T or NK cells target CD3, CD4, CD5, CD7, CD30 or CCR4 [14].
CAR-NK cells have the advantage of circumventing the HLA-matching restriction. The abundant source makes it potentially available to be an off-the-shelf product that could be readily available for immediate clinical use [15].
Functional in vitro drug screening of patient-derived real-time tumor biopsies is another approach to test the plethora of clinically available anticancer drugs for patients with rare diseases like T cell lymphoma directly. In the prospective clinical EXALT trial, functional drug screening was applied to test 136 small molecule drugs on primary patient tumor cells. The most effective in vitro hits were integrated in clinical drug selection for each individual patient. Especially the heterogeneous subgroup of patients with T cell lymphomas demonstrated a benefit in median PFS compared to B‑cell malignancies [16].
Precise genetic and epigenetic patient stratification in the heterogenous diagnosis of peripheral T cell lymphoma will help guide treatment selection in the future.
Key points
-
Brentuximab vedotin + CHP (anti-CD30) is recommended for the PTCL (peripheral T‑cell lymphoma) subgroup ALCL (anaplastic large T cell lymphoma) as first-line treatment (European Medicines Agency).
-
New characteristics of subgroups show new vulnerabilities, e.g., HDAC inhibitors (romidepsin) or azacytidine in AITL (angioimmunoblastic T‑cell lymphoma).
References
Swerdlow SH, et al. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. International agency for research on Cancer (IARC); 2017. IARC WHO Classification of Tumours, Volume 2.
Chihara D, et al. The survival outcome of patients with relapsed/refractory peripheral T‑cell lymphoma-not otherwise specified and angioimmunoblastic T‑cell lymphoma. Br J Haematol. 2017;176:750–8.
Mak V, et al. Survival of patients with peripheral T‑cell lymphoma after first relapse or progression: spectrum of disease and rare long-term survivors. J Clin Oncol. 2013;31:1970–6.
Ma H, et al. Survival benefit in patients with peripheral T‑cell lymphomas after treatments with novel therapies and clinical trials. Hematol Oncol. 2019; https://doi.org/10.1002/hon.2705.
Horwitz S, et al. Brentuximab vedotin with chemotherapy for CD30-positive peripheral T‑cell lymphoma (ECHELON-2): a global, double-blind, randomised, phase 3 trial. Lancet. 2019;393:229–40.
Bachy E, et al. Romidepsin plus CHOP versus CHOP in patients with previously untreated peripheral T‑cell lymphoma: results of the Ro-CHOP phase III study (conducted by LYSA). J Clin Oncol. 2022;40:242–51.
Chiappella A, Carniti C, Re A, Castellino C, Evangelista A, Tabanelli V, Ciancia R, Orsucci L, Pinto A, Usai SV, Arcari A, Ilariucci F, Rossi FG, Ben FPC. Adding romidepsin to CHOEP in first line treatment of peripheral T‑cell lymphomas does not improve the response rate: final analysis of phase II PTCL13 study. Blood. 2021;138:134.
Brink M, et al. Impact of etoposide and ASCT on survival among patients aged 〈65 years with stage II to IV PTCL: a population-based cohort study. Blood. 2022;140:1009–19.
Johnson LDS, et al. Targeting CD47 in Sézary syndrome with SIRPaFc. Blood Adv. 2019;3:1145–53.
Bagot M, et al. IPH4102, a first-in-class anti-KIR3DL2 monoclonal antibody, in patients with relapsed or refractory cutaneous T‑cell lymphoma: an international, first-in-human, open-label, phase 1 trial. Lancet Oncol. 2019;20:1160–70.
Horwitz SM, et al. Tolerability and response of the novel SYK/JAK inhibitor cerdulatinib in a phase 2a study in relapsed/refractory peripheral t cell lymphoma (PTCL). J Clin Oncol. 2018;36:e19532.
Cooper ML, et al. An “off-the-shelf” fratricide-resistant CAR‑T for the treatment of T cell hematologic malignancies. Leukemia. 2018;32:9–32.
Maciocia PM, et al. Targeting the T cell receptor β‑chain constant region for immunotherapy of T cell malignancies. Nat Med. 2017;23:1416–23.
Fiore D, et al. Peripheral T cell lymphomas: from the bench to the clinic. Nat Rev Cancer. 2020;20:6–20.
Lu H, Zhao X, Li Z, Hu Y, Wang H. From CAR‑T cells to CAR-NK cells: a developing immunotherapy method for hematological malignancies. Front Oncol. 2021;11:1–13.
Kornauth C, et al. Functional precision medicine provides clinical benefit in advanced aggressive hematologic cancers and identifies exceptional responders. Cancer Discov. 2022;12:372–87.
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Pichler reports grants from the Austrian Society of Hematology and Medical Oncology and received honoraria from Takeda.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pichler, A. News on Peripheral T-cell lymphoma. memo 16, 17–20 (2023). https://doi.org/10.1007/s12254-022-00864-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12254-022-00864-z