Abstract
Crossing of interspecies barriers by microorganisms is observed. In recent years, Staphylococcus pseudintermedius—a species formerly thought to be animal—has also been isolated from human clinical materials. Many virulence factors are responsible for the colonization, which is the first step an infection, of the new host organism. We analyzed the factors influencing this colonization as well as susceptibility to antibiotics in fourteen S. pseudintermedius strains isolated from clinical cases from humans and animals. The occurrence of genes responsible for binding elastin, fibronectin, and fibrinogen and some phenotypic features, although different between strains, is comparable in both groups. However, the animal isolates had more genes coding for virulence factors. All isolates tested had the exfoliating toxin gene and the leukotoxin determining genes, but only the human strains had enterotoxin genes. The assessment of antibiotic resistance of strains of both groups indicates their broad resistance to antibiotics commonly used in veterinary medicine. Antibiotic resistance was more common among animal isolates. The multilocus sequence typing analysis of the studied strains was performed. The results indicated a large diversity of the S. pseudintermedius population in both studied groups of strains. Equipped with important virulence factors, they showed the ability to infect animals and humans. The clonal differentiation of the methicillin-susceptible strains and the multidrug resistance of the strains of both studied groups should be emphasized. The considerable genetic diversity of strains from a limited geographical area indicates the processes of change taking place within this species. Thus, careful observation of the ongoing process of variation is necessary, as they may lead to the selection of S. pseudintermedius, which will pose a significant threat to humans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, viruses and bacteria have been crossing interspecies barriers more and more often. Adaptation to different hosts allows them to spread effectively (Gortazar et al. 2014). Pathogens that until recently were considered to be typically animal, causing only diseases in animals or constituting their microbiota, can now also cause human infections, including life-threatening ones (Van Hoovels et al. 2006; Chrobak-Chmiel et al. 2018; Gonzalez-Martin et al. 2020).
Staphylococcus pseudintermedius is a coagulase-positive species of staphylococci, commonly colonizing the skin and mucous membranes of animals, most often dogs and cats (Bardiau et al. 2013; Pitchenin et al. 2017; Chrobak-Chmiel et al. 2018). It has also been proven that these bacteria are transmitted to humans in contact with animals (Phumthanakorn et al. 2017). In animals, S. pseudintermedius is often isolated from wounds, ears, bones, or postoperative abscesses (Abouelkhair et al. 2018; Maali et al. 2018). S. pseudintermedius is also found in human infections. The most common are wound infections, mainly after a dog bite, soft tissue infections, otitis externa, and sinusitis. Severe infections such as septic arthritis, nosocomial pneumonia, endocarditis, and bacteremia have also been reported. Contact between an infected animal and person is indicated as crucial in these infections (Van Hoovels et al. 2006; Chrobak et al. 2011; Bannoehr and Guardabassi 2012; Viau et al. 2015; Kmieciak and Szewczyk 2018; Maali et al. 2018; Phumthanakorn et al. 2018). Therapeutic management of S. pseudintermedius infections has become challenging due to the emergence of methicillin-resistant strains (Carroll et al. 2021).
The pathogenesis of S. pseudintermedius infections follows the stages typical of staphylococci. Adhesion begins the colonization of an organism. The virulence factors responsible for this process are surface adhesins, which recognize host extracellular matrix adhesives (MSCRAMM) (Crawford et al. 2016; Phumthanakorn et al. 2017). Their presence supports the invasion and active colonization of host epithelial cells and thus develops infection (Zuniga et al. 2015; Maali et al. 2018). The production of many enzymes, including coagulase, and the ability to form biofilms determine the multiplication of bacteria and, consequently, the development of infection. It has been shown that some strains can also produce toxins (Garbacz et al. 2013; Pitchenin et al. 2017). The presence of these characteristics in strains isolated from human clinical material indicates a risk that should be considered. The spread of clones and their resistance requires constant monitoring.
We studied S. pseudintermedius strains isolated in municipal laboratories from swabs and pus from humans and companion animals. They were the etiological cause of existing infections. Potential factors influencing colonization and spread in the infected organism and susceptibility to antibiotics were investigated. Clonal relationships between the strains were analyzed by comparing the seven housekeeping gene sequences (MLST, multilocus sequence typing analysis) to evaluate the diversity of the isolated strain populations.
Materials and methods
Growth conditions of the tested strains
Fourteen S. pseudintermedius strains isolated from wounds, ears, and abdominal cavity in the hospital laboratories (seven human strains) and veterinary laboratories (seven strains from accompanying animals) in Lodz city, Poland, were used.
Strains selected for this study were initially identified as S. pseudintermedius and S. intermedius by MALDI-TOF MS. However, genetic identification based on the sequence of the nuc gene showed that all tested strains belonged to the S. pseudintermedius species (Sasaki et al. 2010). The strains were isolated and propagated on Columbia Agar and for antibiotic susceptibility testing on Mueller–Hinton media. DNA isolation was performed after an overnight cultivation of the isolates in the Brain Heart Infusion broth.
Phenotypic features
The ability to produce coagulase, lipase, lecithinase, caseinase, and gelatinase CF aggregating factor (clumping factor) test was determined according to the methods described earlier (Freney et al. 1999; Chakraborty et al. 2011; Haddad et al. 2018). Staphylococcus aureus ATCC 25923 was used as the control.
Susceptibility to antibiotics was tested by the disc diffusion method according to European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines for human strains and to Clinical and Laboratory Standards Institute (CLSI) guidelines for animal strains (CLSI 2015; EUCAST 2019). In the study, 14 antibiotics recommended in the treatment of staphylococcal human and animal infections were used: penicillins (oxacillin, benzylpenicillin), fluoroquinolones group (ciprofloxacin, norfloxacin), aminoglycosides (gentamicin), lincosamides and macrolides group (clindamycin, erythromycin), tetracyclines group (tetracycline, tigecycline), quinupristin/dalfopristin, trimethoprim/sulfamethoxazole, linezolid, fusidic acid, and rifampicin. Due to the lack of antibiotic breakpoints in CLSI VET01S other than clindamycin and tetracyclines for staphylococcal strains isolated from animals, human clinical values with EUCAST were used in this study.
The sensitivity to oxacillin was determined to detect methicillin-resistant phenotype (MRSP). Staphylococcus aureus ATCC 29213 was used as a quality control strain. For oxacillin-resistant strains, the MIC values (minimum inhibitory concentration) for vancomycin and daptomycin were determined. Results were interpreted according to EUCAST (EUCAST 2019).
Genotypic features
Bacterial DNA isolation was performed according to the Genomic Mini AX Staphylococcus Gravity protocol (A&ABiotechnology 2020).
Detection of genes responsible for the colonization and development of infections
Table 1 shows the genes searched in this study. Genes with sequences similar or identical to those found in S. aureus are found in various species of Staphylococcus. This homology allows their detection using primers designed for this species. These sequences were also used in this study. Table 1 presents the origin of the searched sequences and the size of the amplicons. The bacterial species for which the presence of the genes was tested based on the proposed sequence were also listed.
Detection of the mecA and blaZ genes
The mecA and blaZ genes were detected to confirm methicillin and penicillin resistance. The genes were detected using the primers and reaction conditions previously described (Kang et al. 2014).
PCR reactions were performed on a Professional Basic Gradient Thermal Cycler (Biometra). The reaction products were separated by electrophoresis on a 1% agarose gel stained with Midori Green DNA stain (NIPPON Genetics EUROPE, Germany) in TAE buffer for 60 min at 70 V and visualized under ultraviolet light.
Multilocus sequence typing (MLST) analysis
The genetic diversity of the investigated S. pseudintermedius isolates was determined by the MLST method using seven loci (ack, cpn60, fdh, purA, pta, sar, tuf) (Solyman et al. 2013). PCR products were sequenced (Genomed, Poland).
The sequences were analyzed and compared with known sequences in the PubMLST database (http://pubmlst.org/). The identified alleles of the seven genes of each strain were used to assign a specific sequence type (ST). All isolates were tested for association with the European sequence types reported in the MLST database. For this purpose, the geoBURST 1.2.1 program was used.
The DNA sequences generated in this study were deposited in GenBank, accession no. for the ack gene, OL378202–OL378215; for the cpn60 gene, OL378216–OL378229; for the fdh gene, OL378230–OL378243; for the purA gene, OL378258–OL378271; for the pta gene, OL378244–OL378257; for the sar gene, OL378272–OL378285; and for the tuf gene, OL372245–OL372258.
The sequences of the primers used in the genetic research are posted in Online Resource 1 in Table S1 (file ESM_1).
Results
All the tested strains were coagulase positive, but the clumping factor (CF) tests were positive only in four human isolates. Proteases were found in both human and animal strains. Only one animal strain produced lecithinase. It was the one with the highest resistance and collected the most significant number of sought genes (Table 2).
Antibiotic resistance was more common among animal isolates. Both methicillin-resistant and methicillin-susceptible isolates were resistant to many classes of antibiotics. In addition to penicillin resistance, among the strains tested, the most common was resistance to erythromycin and clindamycin.
Only two of the 14 isolates tested were phenotypically resistant to methicillin. Genetic studies confirmed the presence of the mecA gene only for these strains. Only methicillin-resistant isolates (MRSP) showed resistance to sulfamethoxazole with trimethoprim. The blaZ gene was detected in 11 strains, consistent with the penicillin resistance phenotype. There was no resistance to the following antibiotics: rifampicin, linezolid and tigecycline, quinupristin/dalfopristin, and fusidic acid, used in severe infections. All strains were susceptible to vancomycin and daptomycin. The results of susceptibility testing of human and animal strains to antibiotics are presented in Table 2.
All tested isolates had essential genes allowing for efficient attachment to host tissues by binding elastin, fibronectin, and fibrinogen (ebpS, spsL, spsE, coa). Some of them had accumulated additional genes conditioning the nonspecific binding of immunoglobulins (spsP, spsO) and of fibronectin (fnbA). The presence of the highest number of genes necessary for adhesion to the cell matrix was accompanied by an antibiotic resistance phenotype (SPZ2, SPZ3, SPZ4, SPL6 isolates). All tested strains possessed the icaD gene, one of the three sought genes related to the biofilm production capacity. Only in human isolates enterotoxin genes (sed, sec) were detected. All tested isolates had the siet gene encoding the exfoliating toxin and the genes determining the production of leukotoxin and lipase (LukS, LukF, lip). However, none of the tested strains carried the pvl gene.
The following genes were not found in the studied isolates: pvl responsible for the production of Panton-Valentine leukotoxin; enterotoxins (sea, seb, see), accountable for the formation of biofilm (icaC and bap) and spsD, whose protein binds fibrinogen, fibronectin, and elastin, as well as genes that specifically bind fibrinogen (fib), fibronectin (fnbB), collagen (cna), and sialoprotein (bbp).
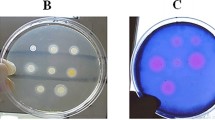
In the isolates used in this study, the ack gene sequences had four alleles and four polymorphic sites. Ten polymorphic sites were detected in the cpn60 gene, resulting in seven alleles. Sequence analysis of the fdh gene revealed three alleles with four polymorphic sites. The sar gene sequences had two alleles with one polymorphic site. Six polymorphic sites were detected in the pta gene, resulting in five alleles. Eight alleles with six polymorphic sites were obtained in the purA gene. Sequence analysis of the tuf gene showed one allele. MLST analysis of sequence variation at seven loci showed 12 STs. Two MRSP isolates from animals were classified as the most frequently identified in the database MRSP clone—ST71. None of the STs found in the group of strains isolated from humans occurred in the group of strains isolated from animals. The results of the MLST analysis are shown in Table 3. Figure 1 shows the relationship between the sequence types of the tested isolates and those of European origin reported in the database. The genetic association of the seven obtained STs with the STs reported in Europe was confirmed.
Connection diagram of the S. pseudintermedius sequence types found in Europe. Sequence types (STs) identified in this study are signed in gray dot spot areas. STs of methicillin-resistant S. pseudintermedius strains are signed in dark gray circles. All remain STs are classified as STs of methicillin-susceptible S. pseudintermedius strains
Discussion
The widespread colonization of the mucous membranes and skin of animals by S. pseudintermedius means that the transfer of this coagulase-positive species to humans is inevitable (Garbacz et al. 2013; Phumthanakorn et al. 2017; Maali et al. 2018; Malisova et al. 2019). The carrier state of these staphylococci in humans has already been demonstrated (Chrobak et al. 2011; Phumthanakorn et al. 2017). Studies have shown that the pangenome of this species is very wide and includes many invasive factors, which means that the pathogenic potential of these bacteria is high (Garbacz et al. 2013). This observation was confirmed by our studies showing the large variety of isolates obtained in a short period only in laboratories of one hospital and veterinary clinic.
In animals, S. pseudintermedius strains most often cause pyoderma and ear infections but are also responsible for systemic diseases (Phumthanakorn et al. 2017; Chrobak-Chmiel et al. 2018). In humans, these staphylococci caused wound infections, sinusitis, soft tissue infections, and endocarditis (Maali et al. 2018; Phumthanakorn et al. 2018). Human infections are not frequently reported, but Maali et al. reported hospital epidemics related to S. pseudintermedius (Maali et al. 2018). This information shows that human infections may appear despite the fact that there was no contact with animals. The animal isolates we studied constituted the etiological factor of ear and skin infections. Human strains originated from severe skin lesions and wound infections, and one was isolated from inflammatory lesions in the abdominal cavity (SPL5).
The invasiveness of S. pseudintermedius strains described so far concerns mainly the skin. MSCRAMM adhesins are essential in such infections (Phumthanakorn et al. 2017; Maali et al. 2018). These adhesins interact with receptors on keratinocytes, corneocytes, and proteins of the skin’s extracellular matrix (Chrobak-Chmiel et al. 2018). The sps genes play an important role in adhesion to the host extracellular matrix (ECM) proteins (Phumthanakorn et al. 2017).
The surface proteins of staphylococcal SpsP and SpsQ, whose genes were present in the strains we studied, are crucial in the adhesion process. These proteins show high homology with S. aureus protein A, which binds IgG and inactivates the complement system. These genes were proven to be expressed in S. pseudintermedius (Phumthanakorn et al. 2017; Balachandran et al. 2018; Gonzalez-Martin et al. 2020). Our results indicate a tandem arrangement of spsP and spsQ genes. Phumthanakorn et al. (Phumthanakorn et al. 2017) linked the presence of these genes with the development of skin infections. Genes determining proteins binding the extracellular matrix (ECM), including fibronectin, fibrinogen, and cytokeratin, also present in our strains, may support further invasion of the pathogen (Phumthanakorn et al. 2017; Chrobak-Chmiel et al. 2018; Richards et al. 2018).
Canine keratinocyte invasion is particularly favored by products of the spsD, spsL, and spsO genes (Gonzalez-Martin et al. 2020). The two latter ones were present in the strains we studied. The production of elastin-binding protein promotes the colonization of the host tissue. The gene coding for this protein, ebpS, was present in all strains we tested. Most strains also had the eno gene, which encodes the enolase, which is a plasminogen receptor, and also determines adherence to laminin, the main component of the basal membrane of the vessels, which allows the spread of infection (Zuniga et al. 2015; Kot et al. 2018).
Adhesion precedes colonization of the infected site and biofilm formation. All the isolates we tested had the icaD gene belonging to the icaADCB operon responsible for biofilm formation (Crawford et al. 2016). Admittedly, a biofilm may arise independently of the expression of icaA and icaD genes. These genes, however, stimulate PIA—the intercellular adhesion polysaccharide—an essential component of the biofilm (Casagrande Proietti et al. 2015; Meroni et al. 2019).
In staphylococci, proteases and lipases are considered important virulence factors (da Cunha et al. 2006; Krzyminska et al. 2015; Haddad et al. 2018). These factors determine the breakdown of sebum, the skin’s protective layer, and promote the spread of bacteria (Kmieciak and Szewczyk 2018). The ability to proteolyze and the gene responsible for lipase production were found in all the isolates we studied.
Coagulase is undoubtedly a vital enzyme in the pathogenicity of S. pseudintermedius. It enables bacteria to escape phagocytosis (Chrobak-Chmiel et al. 2018; Sewid et al. 2018). Coagulase was produced by all the isolates we tested. However, only in the strains isolated from humans the clumping factor (CF) was present. In addition to promoting tissue adhesion, this factor causes platelet aggregation and bacterial clumping in the plasma. This protects bacteria against phagocytosis by neutrophils. Its presence is important in cases of septic arthritis and infective endocarditis (Geoghegan et al. 2009; Lacey et al. 2016, 2019).
In S. aureus, Panton-Valentine leukocidin (PVL) was associated with severe skin infections (Hoppe et al. 2019). The equivalent of PVL in the S. pseudintermedius is the binary leukotoxin Luk-I consisting of the secreted proteins LukF-I and LukS-I (Garbacz et al. 2013; Chrobak-Chmiel et al. 2018). In the tested strains, we found both genes coding these proteins. All isolates also had the siet gene encoding the exfoliating toxin. This gene is common in S. pseudintermedius (Ruscher et al. 2010; Garbacz et al. 2013; Gharsa et al. 2015; Melter et al. 2017). This toxin is essential in pyoderma and chronic otitis in animals (Bannoehr and Guardabassi 2012; Garbacz et al. 2013; Banovic et al. 2017; Gonzalez-Martin et al. 2020). In the genomes of the tested strains isolated from humans, we also found other genes that determine the presence of exfoliative toxins: exiA and exiB. These toxins are responsible for the intra-epidermal cleavage caused by the degradation of desmoglein (Bannoehr and Guardabassi 2012; Richards et al. 2018; Gonzalez-Martin et al. 2020).
In some strains isolated from humans, we detected enterotoxin genes. Of the most important enterotoxins A-E (SEA-SEE) sought, these strains encoded SEC or SED toxin, one of them both. These superantigens bind T lymphocytes to MHC molecules and overstimulate them, leading to acute clinical symptoms (Yoon et al. 2010). These toxins are mainly responsible for food poisoning (Piechota et al. 2014). Chrobak-Chmiel et al. (Chrobak-Chmiel et al. 2018) indicated, however, that simultaneous production of exfoliating toxins and enterotoxins may significantly affect the course of pyoderma.
The assessment of antibiotic resistance of the studied strains indicates their broad resistance regarding the antibiotics used in therapy, including in veterinary medicine. Resistance to β-lactam antibiotics reached 79%. Other authors also noted S. pseudintermedius resistance to this class of antibiotics (Carroll et al. 2021). This resistance may be due to modified penicillin-binding proteins (mecA gene), production of β-lactamases (blaZ gene), or tolerance phenomena. Enzymatic resistance of staphylococci to penicillins is widespread (Silva et al. 2021), and our strains often present this resistance. Both methicillin-resistant strains (MRSP) also had the blaZ gene and, in addition, proved to be resistant to the greatest number of tested antibiotics—they were isolates from dogs.
The MLST method allowed us to assess the population structure of the strains we collected. Although the isolates collection came from one small region, it was very diverse. Twelve types of ST sequences were obtained, nine of which had previously been registered in Europe. None of the MSSP STs shown by us has been previously reported in Poland. Strains isolated from humans turned out to be different from those from animals, which contradicts the common belief about the animal nature of S. pseudintermedius infection. These data show a high level of recombination within the species and, in consequence, its poor clonality. Our animal MRSP isolates belong to the ST71 sequence dominant in Northern Europe. To date, only three such human isolates have been reported. The relationship between the ST71 sequence and other MRSP sequence types ST680 and ST551 present in Poland has already been shown (Bannoehr et al. 2007; Black et al. 2009).
Conclusion
The animal and human isolates we studied have essential features that allow them to infect both hosts. There are similarities between the groups, but at the same time, the strains that compose them are very diverse, confirming the data on the extent of the pangenome of this species. Important features such as being members of different ST groups, the presence of specific genes, or antibiotic resistance features contradict the often-presented view of the exclusively zoonotic nature of S. pseudintermedius infections in humans. The presence of genes determining the severe course of infections makes us recognize the importance of this species and the need for better monitoring of its occurrence.
References
A&ABiotechnology (2020) Genomic Micro AX Staphylococcus Gravity. Gravity flow kit for genomic DNA purification from Staphylococcus bacteria, ver. 1220. https://www.aabiot.com/en/dna-purification/genomic-dna-purification/genomic-micro-ax-staphylococcus-gravity, A&A Biotechnology
Abouelkhair MA, Bemis DA, Giannone RJ, Frank LA, Kania SA (2018) Characterization of a leukocidin identified in Staphylococcus pseudintermedius. Plos One 13(9): e0204450. https://doi.org/10.1371/journal.pone.0204450
Balachandran M, Bemis DA, Kania SA (2018) Expression and function of protein A in Staphylococcus pseudintermedius. Virulence 9(1): 390–401. https://doi.org/10.1080/21505594.2017.1403710
Bannoehr J, Ben Zakour NL, Waller AS, Guardabassi L, Thoday KL, van den Broek AHM, Fitzgerald JR (2007) Population genetic structure of the Staphylococcus intermedius group: insights into agr diversification and the emergence of methicillin-resistant strains. J Bacteriol 189:8685–8692. https://doi.org/10.1128/JB.01150-07
Bannoehr J, Guardabassi L (2012) Staphylococcus pseudintermedius in the dog: taxonomy, diagnostics, ecology, epidemiology and pathogenicity. Vet Dermatol 23: 253–266, e51–2. https://doi.org/10.1111/j.1365-3164.2012.01046.x
Banovic F, Linder K, Olivry T (2017) Clinical, microscopic and microbial characterization of exfoliative superficial pyoderma-associated epidermal collarettes in dogs. Vet Dermatol 28:107-e23. https://doi.org/10.1111/vde.12352
Bardiau M, Yamazaki K, Ote I, Misawa N, Mainil JG (2013) Characterization of methicillin-resistant Staphylococcus pseudintermedius isolated from dogs and cats. Microbiol Immunol 57:496–501. https://doi.org/10.1111/1348-0421.12059
Becker K, Keller B, von Eiff C, Bruck M, Lubritz G, Etienne J, Peters G (2001) Enterotoxigenic potential of Staphylococcus intermedius. Appl Environ Microbiol 67:5551–5557. https://doi.org/10.1128/AEM.67.12.5551-5557.2001
Bergot M, Martins-Simoes P, Kilian H, Chatre P, Worthing KA, Norris JM, Madec JY, Laurent F, Haenni M (2018) Evolution of the population structure of Staphylococcus pseudintermedius in France. Front Microbiol 9: 3055. https://doi.org/10.3389/fmicb.2018.03055
Black CC, Solyman SM, Eberlein LC, Bemis DA, Woron AM, Kania SA (2009) Identification of a predominant multilocus sequence type, pulsed-field gel electrophoresis cluster, and novel staphylococcal chromosomal cassette in clinical isolates of mecA-containing, methicillin-resistant Staphylococcus pseudintermedius. Vet Microbiol 139:333–338. https://doi.org/10.1016/j.vetmic.2009.06.029
Carroll KC, Burnham CAD, Westblade LF (2021) From canines to humans: clinical importance of Staphylococcus pseudintermedius. Plos Pathogens 17: e1009961. https://doi.org/10.1371/journal.ppat.1009961
Casagrande Proietti P, Stefanetti V, Hyatt DR, Marenzoni ML, Capomaccio S, Coletti M, Bietta A, Franciosini MP, Passamonti F (2015) Phenotypic and genotypic characterization of canine pyoderma isolates of Staphylococcus pseudintermedius for biofilm formation. J Vet Med Sci 77:945–951. https://doi.org/10.1292/jvms.15-0043
Cavalcante FS, Saintive S, Ferreira DC, Silva ABR, Guimaraes LC, Braga BS, Abad ED, Ribeiro M, dos Santos KRN (2021) Methicillin-resistant Staphylococcus aureus from infected skin lesions present several virulence genes and are associated with the CC30 in Brazilian children with atopic dermatitis. Virulence 12:260–269. https://doi.org/10.1080/21505594.2020.1869484
Çetin H, Tuncer Y (2016) Investigation of enterotoxin genes in coagulase-negative Staphylococcus and Micrococcus caseolyticus strains from Turkish dry fermented sausage (sucuk). GIDA - J Food 41:163–170
Chakraborty SP, Mahapatra SK, Roy S (2011) Biochemical characters and antibiotic susceptibility of Staphylococcus aureus isolates. Asian Pac J Trop Biomed 1:212–216. https://doi.org/10.1016/S2221-1691(11)60029-4
Chrobak D, Kizerwetter-Swida M, Rzewuska M, Moodley A, Guardabassi L, Binek M (2011) Molecular characterization of Staphylococcus pseudintermedius strains isolated from clinical samples of animal origin. Folia Microbiol 56:415–422. https://doi.org/10.1007/s12223-011-0064-7
Chrobak-Chmiel D, Golke A, Dembele K, Cwiek K, Kizerwetter-Swida M, Rzewuska M, Binek M (2018) Staphylococcus pseudintermedius, both commensal and pathogen. Medycyna Weterynaryjna-Veterinary Medicine-Science and Practice 74:362–370
CLSI (2015) VET01S: performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals. (VET01S Cs, ed.).
Crawford EC, Singh A, Gibson TWG, Weese JS (2016) Biofilm-associated gene expression in Staphylococcus pseudintermedius on a variety of implant materials. Vet Surg 45:499–506. https://doi.org/10.1111/vsu.12471
Cucarella C, Solano C, Valle J, Amorena B, Lasa I, Penades JR (2001) Bap, a Staphylococcus aureus surface protein involved in biofilm formation. J Bacteriol 183:2888–2896. https://doi.org/10.1128/JB.183.9.2888-2896.2001
da Cunha M, Rugolo L, Lopes CAD (2006) Study of virulence factors in coagulase-negative staphylococci isolated from newborns. Mem Inst Oswaldo Cruz 101:661–668. https://doi.org/10.1590/s0074-02762006000600014
European Committee on Antimicrobial Susceptibility Testing EUCAST (2019) Breakpoint tables for interpretation of MICs and zone diameters, version 9.0. (9.0) Cb-bv, ed.). http://www.eucast.org/clinical_breakpoints/
Firoozeh F, Omidi M, Saffari M, Sedaghat H, Zibaei M (2020) Molecular analysis of methicillin-resistant Staphylococcus aureus isolates from four teaching hospitals in Iran: the emergence of novel MRSA clones. Antimicrob Resist Infect Control 9: 112. https://doi.org/10.1186/s13756-020-00777-8
Freney J, Kloos WE, Hajek V, Webster JA, Bes M, Brun Y, Vernozy-Rozand C, Subcommittee Taxonomy S (1999) Recommended minimal standards for description of new staphylococcal species. Int J Syst Bacteriol 49:489–502. https://doi.org/10.1099/00207713-49-2-489
Garbacz K, Zarnowska S, Piechowicz L, Haras K (2013) Pathogenicity potential of Staphylococcus pseudintermedius strains isolated from canine carriers and from dogs with infection signs. Virulence 4:255–259. https://doi.org/10.4161/viru.23526
Geoghegan JA, Smith EJ, Speziale P, Foster TJ (2009) Staphylococcus pseudintermedius expresses surface proteins that closely resemble those from Staphylococcus aureus. Vet Microbiol 138:345–352. https://doi.org/10.1016/j.vetmic.2009.03.030
Gharsa H, Ben Slama K, Gomez-Sanz E, Gomez P, Klibi N, Zarazaga M, Boudabous A, Torres C (2015) Characterisation of nasal Staphylococcus delphini and Staphylococcus pseudintermedius isolates from healthy donkeys in Tunisia. Equine Vet J 47:463–466. https://doi.org/10.1111/evj.12305
Ghasemian A, Najar-Peerayeh S, Bakhshi B, Mirzaee M (2015) High prevalence of icaABCD genes responsible for biofilm formation in clinical isolates of Staphylococcus aureus from hospitalized children. Arch Pediatr Infect Dis 3: e20703. https://doi.org/10.5812/pedinfect.20703v2
Gonzalez-Martin M, Corbera JA, Suarez-Bonnet A, Tejedor-Junco MT (2020) Virulence factors in coagulase-positive staphylococci of veterinary interest other than Staphylococcus aureus. Vet Q 40:118–131. https://doi.org/10.1080/01652176.2020.1748253
Gortazar C, Reperant LA, Kuiken T, de la Fuente J, Boadella M, Martinez-Lopez B, Ruiz-Fons F, Estrada-Pena A, Drosten C, Medley G, Ostfeld R, Peterson T, VerCauteren KC, Menge C, Artois M, Schultsz C, Delahay R, Serra-Cobo J, Poulin R, Keck F, Aguirre AA, Henttonen H, Dobson AP, Kutz S, Lubroth J, Mysterud A (2014) Crossing the interspecies barrier: opening the door to zoonotic pathogens. Plos Pathogens 10: e1004129. https://doi.org/10.1371/journal.ppat.1004129
Haddad O, Merghni A, Elargoubi A, Rhim H, Kadri Y, Mastouri M (2018) Comparative study of virulence factors among methicillin resistant Staphylococcus aureus clinical isolates. Bmc Infect Dis 18: 560. https://doi.org/10.1186/s12879-018-3457-2
Hoppe PA, Holzhauer S, Lala B, Buhrer C, Gratopp A, Hanitsch LG, Humme D, Kieslich M, Kallinich T, Lau S, Leistner R, Niebank M, Pokrywka A, Ringe H, Schaper AS, Schroder JT, Schwarz C, Staab D, Stegemann MS, Thee S, Varnholt V, von Bernuth H, Weber-Carstens S, Wendt A, Kruger R (2019) Severe infections of Panton-Valentine leukocidin positive Staphylococcus aureus in children. Medicine 98: e17185. https://doi.org/10.1097/MD.0000000000017185
Hritcu OM, Schmidt VM, Salem SE, Maciuca IE, Moraru RF, Lipovan I, Mares M, Solcan G, Timofte D (2020) Geographical variations in virulence factors and antimicrobial resistance amongst staphylococci isolated from dogs from the United Kingdom and Romania. Front Vet Scie 7: 414. https://doi.org/10.3389/fvets.2020.00414
Ishihara K, Shimokubo N, Sakagami A, Ueno H, Muramatsu Y, Kadosawa T, Yanagisawa C, Hanaki H, Nakajima C, Suzuki Y, Tamura Y (2010) Occurrence and molecular characteristics of methicillin-resistant Staphylococcus aureus and methicillin-resistant Staphylococcus pseudintermedius in an academic veterinary hospital. Appl Environ Microbiol 76:5165–5174. https://doi.org/10.1128/AEM.02780-09
Kang MH, Chae MJ, Yoon JW, Kim SG, Lee SY, Yoo JH, Park HM (2014) Antibiotic resistance and molecular characterization of ophthalmic Staphylococcus pseudintermedius isolates from dogs. J Vet Sci 15:409–415. https://doi.org/10.4142/jvs.2014.15.3.409
Kmieciak W, Szewczyk EM (2018) Are zoonotic Staphylococcus pseudintermedius strains a growing threat for humans? Folia Microbiol 63:743–747. https://doi.org/10.1007/s12223-018-0615-2
Kot B, Sytykiewicz H, Sprawka I (2018) Expression of the biofilm-associated genes in methicillin-resistant Staphylococcus aureus in biofilm and planktonic conditions. Int J Mol Sci 19: 3487. https://doi.org/10.3390/ijms19113487
Krzyminska S, Szczuka E, Dudzinska K, Kaznowski A (2015) Virulence and the presence of aminoglycoside resistance genes of Staphylococcus haemolyticus strains isolated from clinical specimens. Antonie Van Leeuwenhoek Int J Gen Mol Microbiol 107:857–868. https://doi.org/10.1007/s10482-015-0378-6
Lacey KA, Geoghegan JA, McLoughlin RM (2016) The role of Staphylococcus aureus Virulence factors in skin infection and their potential as vaccine antigens. Pathogens 5: 22. https://doi.org/10.3390/pathogens5010022
Lacey KA, Mulcahy ME, Towell AM, Geoghegan JA, McLoughlin RM (2019) Clumping factor B is an important virulence factor during Staphylococcus aureus skin infection and a promising vaccine target. Plos Pathogens 15: e1007713. https://doi.org/10.1371/journal.ppat.1007713
Lange J, Heidenreich K, Higelin K, Dyck K, Marx V, Reichel C, van Wamel W, den Reijer M, Gorlich D, Kahl BC (2020) Staphylococcus aureus pathogenicity in cystic fibrosis patients-results from an observational prospective multicenter study concerning virulence genes, phylogeny, and gene plasticity. Toxins 12: 279. https://doi.org/10.3390/toxins12050279
Lautz S, Kanbar T, Alber J, Lammler C, Weiss R, Prenger-Berningho E, Zschock M (2006) Dissemination of the gene encoding exfoliative toxin of Staphylococcus intermedius among strains isolated from dogs during routine microbiological diagnostics. J Vet Med Series B-Infect Dis Vet Public Health 53:434–438. https://doi.org/10.1111/j.1439-0450.2006.00999.x
Maali Y, Badiou C, Martins-Simoes P, Hodille E, Bes M, Vandenesch F, Lina G, Diot A, Laurent F, Trouillet-Assant S (2018) Understanding the virulence of Staphylococcus pseudintermedius: a major role of pore-forming toxins. Front Cell Infect Microbiol 8: 221. https://doi.org/10.3389/fcimb.2018.00221
Malisova L, Safrankova R, Keklakova J, Petras P, Zemlickova H, Jakubu V (2019) Correct species identification (reclassification in CNCTC) of strains of Staphylococcus intermedius-group can improve an insight into their evolutionary history. Folia Microbiol 64:231–236. https://doi.org/10.1007/s12223-018-0647-7
Mello PL, Moraes Riboli DF, Pinheiro L, Martins LD, Brito M, da Cunha M (2016) Detection of enterotoxigenic potential and determination of clonal profile in staphylococcus aureus and coagulase-negative staphylococci isolated from bovine subclinical mastitis in different brazilian states. Toxins 8: 104. https://doi.org/10.3390/toxins8040104
Melter O, Svec P, Tkadlec J, Doskar J, Kinska H, Pantucek R (2017) Characterisation of methicillin-susceptible Staphylococcus pseudintermedius isolates from canine infections and determination of virulence factors using multiplex PCR. Vet Med 62:81–89. https://doi.org/10.17221/105/2016-VETMED
Meroni G, Filipe JFS, Drago L, Martino PA (2019) Investigation on antibiotic-resistance, biofilm formation and virulence factors in multi drug resistant and non multi drug resistant Staphylococcus pseudintermedius. Microorganisms 7: 702. https://doi.org/10.3390/microorganisms7120702
Nasaj M, Saeidi Z, Tahmasebi H, Dehbashi S, Arabestani MR (2020) Prevalence and distribution of resistance and enterotoxins/enterotoxin-like genes in different clinical isolates of coagulase-negativeStaphylococcus. Eur J Med Res 25: 48. https://doi.org/10.1186/s40001-020-00447-w
Parastan R, Kargar M, Solhjoo K, Kafilzadeh F (2020) A synergistic association between adhesion-related genes and multidrug resistance patterns of Staphylococcus aureus isolates from different patients and healthy individuals. J Glob Antimicrob Resist 22:379–385. https://doi.org/10.1016/j.jgar.2020.02.025
Park JY, Fox LK, Seo KS, McGuire MA, Park YH, Rurangirwa FR, Sischo WM, Bohach GA (2011) Detection of classical and newly described staphylococcal superantigen genes in coagulase-negative staphylococci isolated from bovine intramammary infections. Vet Microbiol 147:149–154. https://doi.org/10.1016/j.vetmic.2010.06.021
Phumthanakorn N, Chanchaithong P, Prapasarakul N (2017) Development of a set of multiplex PCRs for detection of genes encoding cell wall-associated proteins in Staphylococcus pseudintermedius isolates from dogs, humans and the environment. J Microbiol Methods 142:90–95. https://doi.org/10.1016/j.mimet.2017.09.003
Phumthanakorn N, Fungwithaya P, Chanchaithong P, Prapasarakul N (2018) Enterotoxin gene profile of methicillin-resistant Staphylococcus pseudintermedius isolates from dogs, humans and the environment. J Med Microbiol 67:866–873. https://doi.org/10.1099/jmm.0.000748
Piechota M, Kot B, Frankowska-Maciejewska A, Gruzewska A, Wozniak-Kosek A (2018) Biofilm formation by methicillin-resistant and methicillin-sensitive Staphylococcus aureus strains from hospitalized patients in Poland. Biomed Res Int 2018: 4657396. https://doi.org/10.1155/2018/4657396
Piechota M, Kot B, Zdunek E, Mitrus J, Wicha J, Wolska MK, Sachanowicz K (2014) Distribution of classical enterotoxin genes in staphylococci from milk of cows with- and without mastitis and the cowshed environment. Pol J Vet Sci 17:407–411. https://doi.org/10.2478/pjvs-2014-0058
Pitchenin LC, Brandao LNS, Rosa JMA, Kagueyama FC, Alves AD, Rocha ISM, Nakazato L, Dutra V (2017) Occurrence of toxin genes in Staphylococcus pseudintermedius from diseased dogs and other domestic and wild species. J Infect Dev Ctries 11:957–961. https://doi.org/10.3855/jidc.8261
Rall VLM, Miranda ES, Castilho IG, Camargo CH, Langoni H, Guimaraes FF, Araujo JP, Fernandes A (2014) Diversity of Staphylococcus species and prevalence of enterotoxin genes isolated from milk of healthy cows and cows with subclinical mastitis. J Dairy Sci 97:829–837. https://doi.org/10.3168/jds.2013-7226
Richards AC, O’Shea M, Beard PM, Goncheva MI, Tuffs SW, Fitzgerald JR, Lengeling A (2018) Staphylococcus pseudintermedius surface protein L (SpsL) is required for abscess formation in a murine model of cutaneous infection. Infect Immun 86:e00631-18. https://doi.org/10.1128/IAI.00631-18
Ruscher C, Lubke-Becker A, Semmler T, Wleklinski CG, Paasch A, Soba A, Stamm I, Kopp P, Wieler LH, Walther B (2010) Widespread rapid emergence of a distinct methicillin- and multidrug-resistant Staphylococcus pseudintermedius (MRSP) genetic lineage in Europe. Vet Microbiol 144:340–346. https://doi.org/10.1016/j.vetmic.2010.01.008
Ruzauskas M, Couto N, Pavilonis A, Klimiene I, Siugzdiniene R, Virgailis M, Vaskeviciute L, Anskiene L, Pomba C (2016) Characterization of Staphylococcus pseudintermedius isolated from diseased dogs in Lithuania. Pol J Vet Sci 19:7–14. https://doi.org/10.1515/pjvs-2016-0002
Saad MS, Hassan MA, Abou El-Roos-Nahla A, Gaafar MH (2017) Staphylococcal contamination of cattle carcasses with particular reference to Staph. aureus enterotoxins. Benha Vet Med J 32: 94–98. https://doi.org/10.21608/BVMJ.2017.31121
Salaberry SRS, Saidenberg ABS, Zuniga E, Melville PA, Santos FGB, Guimaraes EC, Gregori F, Benites NR (2015) Virulence factors genes of Staphylococcus spp. isolated from caprine subclinical mastitis. Microb Pathog 85: 35–39. https://doi.org/10.1016/j.micpath.2015.05.007
Sasaki T, Tsubakishita S, Tanaka Y, Sakusabe A, Ohtsuka M, Hirotaki S, Kawakami T, Fukata T, Hiramatsu K (2010) Multiplex-PCR method for species identification of coagulase-positive staphylococci. J Clin Microbiol 48:765–769. https://doi.org/10.1128/JCM.01232-09
Sewid AH, Hassan MN, Ammar AM, Bemis DA, Kania SA (2018) Identification, cloning, and characterization of Staphylococcus pseudintermedius coagulase. Infect Immun 86:e00027-18. https://doi.org/10.1128/IAI.00027-18
Silva V, Oliveira A, Manageiro V, Canica M, Contente D, Capita R, Alonso-Calleja C, Carvalho I, Capelo JL, Igrejas G, Poeta P (2021) Clonal diversity and antimicrobial resistance of methicillin-resistant Staphylococcus pseudintermedius isolated from canine pyoderma. Microorganisms 9: 482. https://doi.org/10.3390/microorganisms9030482
Solyman SM, Black CC, Duim B, Perreten V, van Duijkeren E, Wagenaar JA, Eberlein LC, Sadeghi LN, Videla R, Bemis DA, Kania SA (2013) Multilocus sequence typing for characterization of Staphylococcus pseudintermedius. J Clin Microbiol 51:306–310. https://doi.org/10.1128/JCM.02421-12
Szemraj M, Grazul M, Balcerczak E, Szewczyk EM (2020) Staphylococcal species less frequently isolated from human clinical specimens - are they a threat for hospital patients? Bmc Infect Dis 20: 128. https://doi.org/10.1186/s12879-020-4841-2
Tanabe T, Toyoguchi M, Hirano F, Chiba M, Onuma K, Sato H (2013) Prevalence of staphylococcal enterotoxins in Staphylococcus pseudintermedius isolates from dogs with pyoderma and healthy dogs. Microbiol Immunol 57:651–654. https://doi.org/10.1111/1348-0421.12069
Thompson TA, Brown PD (2017) Association between the agr locus and the presence of virulence genes and pathogenesis in Staphylococcus aureus using a Caenorhabditis elegans model. Int J Infect Dis 54:72–76. https://doi.org/10.1016/j.ijid.2016.11.411
Tristan A, Ying L, Bes M, Etienne J, Vandenesch F, Lina G (2003) Use of multiplex PCR to identify Staphylococcus aureus adhesins involved in human hematogenous infections. J Clin Microbiol 41:4465–4467. https://doi.org/10.1128/JCM.41.9.4465-4467.2003
Van Hoovels L, Vankeerberghen A, Boel A, Van Vaerenbergh K, De Beenhouwer H (2006) First case of Staphylococcus pseudintermedius infection in a human. J Clin Microbiol 44:4609–4612. https://doi.org/10.1128/JCM.01308-06
Vancraeynest D, Hermans K, Haesebrouck F (2004) Genotypic and phenotypic screening of high and low virulence Staphylococcus aureus isolates from rabbits for biofilm formation and MSCRAMMs. Vet Microbiol 103:241–247. https://doi.org/10.1016/j.vetmic.2004.09.002
Viau R, Hujer AM, Hujer KM, Bonomo RA, Jump RLP (2015) Are Staphylococcus intermedius infections in humans cases of mistaken identity? A case series and literature review. Open Forum Infect Dis 2: ofv110. https://doi.org/10.1093/ofid/ofv110
Wisniewska K, Piorkowska A, Kasprzyk J, Bronk M, Swiec K (2014) Clonal distribution of bone sialoprotein-binding protein gene among Staphylococcus aureus isolates associated with bloodstream infections. Folia Microbiol 59:465–471. https://doi.org/10.1007/s12223-014-0321-7
Yoon JW, Lee GJ, Lee SY, Park C, Yoo JH, Park HM (2010) Prevalence of genes for enterotoxins, toxic shock syndrome toxin 1 and exfoliative toxin among clinical isolates of Staphylococcus pseudintermedius from canine origin. Vet Dermatol 21:484–489. https://doi.org/10.1111/j.1365-3164.2009.00874.x
Ziasistani M, Shakibaie MR, Kalantar-Neyestanaki D (2019) Genetic characterization of two vancomycin-resistant Staphylococcus aureus isolates in Kerman Iran. Infect Drug Resist 12:1869–1875. https://doi.org/10.2147/IDR.S205596
Zuniga E, Melville PA, Saidenberg ABS, Laes MA, Gonsales FF, Salaberry SRS, Gregori F, Brandao PE, dos Santos FGB, Lincopan NE, Benites NR (2015) Occurrence of genes coding for MSCRAMM and biofilm-associated protein Bap in Staphylococcus spp. isolated from bovine subclinical mastitis and relationship with somatic cell counts. Microb Pathog 89: 1–6. https://doi.org/10.1016/j.micpath.2015.08.014
Funding
This study was supported by the statutory research funds (502–03/3–012-03/503–31-011) of the Medical University of Lodz.
Author information
Authors and Affiliations
Contributions
All authors designed the experiments. Paulina Glajzner and Magdalena Szemraj performed the experiments. Magdalena Szemraj and Eligia Szewczyk analyzed the data. Paulina Glajzner, Eligia Szewczyk, and Magdalena Szemraj wrote the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Glajzner, P., Szewczyk, E.M. & Szemraj, M. Pathogenic potential and antimicrobial resistance of Staphylococcus pseudintermedius isolated from human and animals. Folia Microbiol 68, 231–243 (2023). https://doi.org/10.1007/s12223-022-01007-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12223-022-01007-x