Abstract
It has been shown that a reciprocal relationship between cancer patients and their family caregivers positively decreases distress in both. In this context we tried to explore the role of relationship reciprocity in the dyad members’ symptoms of fatigue and distress (anxiety and depression). Specifically, we aimed to assess the implications of relationship reciprocity testing the link between the various measurements of patient Quality of Life (QoL) and caregiver burden and the other measures of fatigue, distress, and relationship reciprocity. Moreover we aimed to examine the inter-relatedness of patients’ and caregivers’ relationship reciprocity with their own as well as fatigue and distress of the dyads. A convenience sample of 545 adult cancer patients and their caregivers from 15 cancer centers were examined using a cross-sectional design. Participants were administered dyadic measures (fatigue, distress, relationship reciprocity) and individual measures (patients’ QoL and caregivers’ burden). Patients’ QoL and caregivers’ Burden were associated with fatigue, distress and relationship reciprocity. The Actor-Partner Interdependence Model (APIM) revealed that each person’s relationship reciprocity was associated with their own distress and fatigue (actor effects); only caregivers’ relationship reciprocity was associated with patients’ fatigue and distress (partner effects). These findings suggest that the implication of the caregiving relationship for fatigue symptoms in both - patients and caregivers - appears worth of investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer diagnosis and treatment are highly stressful events for patients (Grassi et al., 2013; Holland, 2013), bearing practical and emotional repercussions for the entire family, the majority of the care and assistance patients require is given at home by a family caregiver. In addition or similarly to emotional distress, fatigue certainly plays a role in significant consequence of cancer and its treatment which may still affect the Quality of Life (QoL) years after the end of treatment (Berger et al., 2012; Minton et al., 2013). However, as Smith and collaborators affirm (Smith et al., 2019), it is often underrecognized and undertreated. The National Comprehensive Cancer Network defines cancer-associated fatigue as an unpleasant continuous feeling of tiredness or exhaustion that is related to cancer, is not related to recent activity, and interferes with daily functioning (NCCN, Berger et al., 2018). It involves the dysregulation of several interrelated physiological, biochemical, and psychological systems, with inflammation as a key biological pathway (Bower & Lamkin, 2013; O’Higgins et al., 2018). Cancer patients typically experience fatigue, anxiety, and depression symptoms together, which has led to conjecture about shared underlying processes (Bower et al., 2011; Brown & Kroenke, 2009).
Observing a loved one undergo cancer treatment and worrying about the result causes caregivers to experience considerable feelings of fatigue, a general word that encompasses both physical and mental depletion (Langenberg et al., 2019; Peters et al., 2015). Interestingly, research has shown significant levels of fatigue often related to depressive symptoms and existential burden for caregivers as well (Clark et al., 2014; Gaston-Johansson et al., 2004).
Studies suggest that patients’ and caregivers’ reactions to the stress of facing cancer are often interdependent. Hagedoorn et al. (2008) conducted a meta-analysis and discovered a moderate association between the suffering of patients and that of their partners, indicating that they experience cancer as an emotional system rather than as an individual. Family researchers have highlighted the importance of a dyadic paradigm that considers the role of individual factors as well as how each partner affects the other (Badr et al., 2014; Camara et al., 2019; Karlstedt et al., 2017; Kayser & Acquati, 2019). Several studies have focused on the interdependence between patients and caregivers regarding the symptoms of emotional distress (Jacobs et al., 2017; Kershaw et al., 2015).
Although many studies have explored the patient-caregiver interdependence in regard to distress, the implications of the patient-caregiver relationship has not been addressed in regard to fatigue. However, as reported by some authors (Bower, 2019; Mustian et al., 2017), there is considerable variability in the experience of fatigue that is not explained by disease- or treatment-related characteristics, suggesting that other factors may play an important role in the development and persistence of fatigue symptoms. Thus, the implication of the caregiving relationship for fatigue symptoms both in patients and in caregivers appears worth the investigation. Furthermore, the negative consequences of fatigue and distress on both patient QoL (Bower, 2014) and caregiver burden (Langenberg et al., 2019) are well known; therefore, both patient Qol and caregiver burden deserve consideration, when exploring the association of the patient-caregiver relationship with symptoms of distress and fatigue.
Many studies have primarily addressed the impact of cancer on the couple relationship (Hagedoorn et al., 2008; Regan et al., 2015). However, it may be difficult to differentiate caregiving vs couple relationship when they overlap. Illness progression inevitably creates an imbalance in the patient-caregiver relationship, by making patients more dependent while limiting caregivers’ options for work and social life. Support only has favorable psychological and health-related effects when the support recipient perceives reciprocity from the support provider, as some scholars have noticed, because the relationship’s sense of dependence is diminished (Buunk & Schaufeli, 1999). Additionally, there is data that suggests reciprocity may lessen caregiver stress (McPherson et al., 2010; Reid et al., 2005; Ybema et al., 2002).
Numerous research (Gaston-Johansson et al., 2004; Milbury et al., 2013; Tan et al., 2018) have investigated the connections between caregivers and cancer patient outcomes. Patients’ psychological functions were significantly correlated with caregiver load among cancer patients. In this context, it is crucial to remember that healthcare professionals must prepare for the frequently unpleasant experiences of caregivers and start assessing their psychological distress, exhaustion, caregiving load, and quality of life. Since related health issues might have long-term implications like increased distress, as we already discussed, this experience may be problematic for both patients and caregivers.
According to contextual theory (Boszormenyi-Nagy & Krasner, 1986; Boszormenyi-Nagy, 2013) the investment of family members to achieve a reciprocal give-and-take, in terms of commitment to the well-being of the other, is what shapes relational mutuality over time. In this perspective, cancer is a threatening challenge because reciprocity can be achieved only by acknowledging that the patient-caregiver relationship is naturally asymmetric; this is defined equitable asymmetry in contextual terms (Gurman & Kniskern, 1991). Actually, the research review on reciprocity in caregiving relationships has evidenced how a good reciprocity of the relationship is partially determined by the dyad members’ acceptance of the contribution that each can give to the other according to one’s own terms and possibilities (McPherson et al., 2010). In fact, there is evidence that interpersonal exchanges, such as love and concern for the caregiver, may still occur and be important for his or her QoL even when a family member is seriously ill and unable to reciprocate with material tangible support (Curci & Rimé, 2012; McPherson et al., 2011; Reid et al., 2005). According to Gleason and colleagues’ findings from 2003, offering assistance in a relationship characterized by reciprocal caring improved mood.
Consequently, from the theoretical and empirical considerations formerly enunciated and for the purpose of this study, reciprocity was identified as the characteristic pertaining to the reciprocity of the patient-caregiver relationship. Within the frame of the contextual theory, reciprocity cannot be equal to a mere evaluation of give-and take in terms of quid-pro-quo between partners. Rather, each dyad member evaluate their relationship in terms of ‘emotional support received by the other’, ‘freedom to share oneself with the other’ and ‘giving acknowledgement for caring to the other’ and that will represent their effort to achieve reciprocity within an asymmetrical relationship.
According to the literature review and the above considerations, the aim of this multicenter study was to explore the implications of relationship reciprocity for the dyad members’ symptoms of fatigue and distress (to simplify, fatigue will be used, hereafter, to refer to both patients’ and caregivers’ fatigue symptoms). In particular (1) we, firstly, assessed the implications of relationship reciprocity testing the association between the different measures of patient Quality of Life (QoL) and caregiver burden and the other measures of fatigue, distress, and relationship reciprocity. Finally (2) we addressed our main aim by examining the inter-relatedness of patients’ and caregivers’ relationship reciprocity with their own as well as the other dyad members’ fatigue and distress, through the Actor-Partner Interdependence Model (APIM) (Cook & Kenny, 2005). The APIM was run to test the inter-relatedness of Relationship Reciprocity, fatigue and distress in dyads by taking both patient and caregiver contributions in a single regression model where illness severity was considered as covariate since it is a clinical determinant that may affect the degree of distress and fatigue experienced.
Methods
Design
A cohort of cancer patients and their informal caregivers who were receiving treatment at fifteen Italian out-patient cancer centers representative of different regions of ItalyFootnote 1 were examined using a cross-sectional design.
Participants
Adult outpatients with a cancer diagnosis (or cancer recurrence) who were undergoing outpatient cancer-related operations made up the sample, consecutively admitted to the Day Hospitals of the Medical Oncology Units of fifteen Italian Healthcare Institutions. Participation took place with free access, research measures were administered while they waited their turn to be subjected to cancer-related procedures and under examiner supervision. Inclusion criteria were: Patients with solid cancer (regardless of type of diagnosis and stage of disease) who had caregivers willing to participate in the study. Patients named their primary source of emotional and/or physical care as their caregivers. Significant cognitive deficits, major psychiatric disorders, significant sensory impairment, and a lack of education sufficient to meet exam requirements were among the exclusion factors. All patients and their caregivers were simultaneously recruited during a four-week period (May through June 2018). When either a patient or a caregiver or both returned incomplete questionnaires, the whole dyad was excluded from the study (6 patients and 3 caregivers refused to fill in the questionnaires, after their initial enrollment; 23 patients and 9 caregivers returned incomplete questionnaires). A total of 545 patient-caregiver dyads submitted accurate data for the research variables out of the 586 dyads that agreed to participate in the current study (enrollment rate = 93%).
Measures
Demographic and clinical data
Socio-demographic and clinical data were collected from participants and through the review of patients’ medical charts and physician consultation (Table 1).
Fatigue
The Italian version of the European Organization for Research and Treatment of Cancer – fatigue 12 Phase IV module (EORTC-FA 12), (Weis et al., 2017), was used to assess fatigue in both patients (PT) and caregivers (CG); the same assessment instrument was preferred for comparable measures between the two groups. The scale includes ten unidirectional items and two criteria variables ranged from 1 to 4, with higher values indicating higher levels. The two criteria variables measure Interference with daily life (item 11) and Social sequelae (item 12). The ten items load the three subscales: Physical (items 1–5; αPT = .88; αCG = .88), Emotional (items 6–8;αPT = .83; αCG = .87), and Cognitive fatigue (items 9–10; αPT = .84; αCG = .87). Following the scoring procedure of the EORTC QLQ-C30, all subscales were standardized and transformed in 0–100 scales. For the purpose of the current study, only the three subscales were considered.
Distress
The Italian version of the Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, 1983) was used to measure distress in both patients (PT) and caregivers (CG). In cancer care, the HADS is commonly used as a tool for screening for psychological distress because it has been validated with cancer patients (Annunziata et al., 2020). It consists of fourteen 4-point items, ranging 0–3. Items were averaged into two dimensions: a) HADS-anxiety (αPT = .84; αCG = .83), b) HADS-depression (αPT = .83; αCG = .79), with higher values indicating higher levels of distress.
Relationship reciprocity
The perceived quality of the patient-caregiver relationship was assessed by asking both patients (PT) and caregivers (CG) to rate each other using three 7-point items (1 = never, 7 = always): 1) ‘I receive the emotional support and help that I need from the other’, 2) ‘I feel free to express my emotions to the other’, 3) ‘The other gives me acknowledgement for what I do for him/her’. To authors’ knowledge, only the Mutuality Scale has been translated into Italian and adapted for both patients and caregivers, although in a stroke population (Pucciarelli et al., 2016). For the purpose of the current study, in particular to best approach the concept of the contextual theory, and in accordance with the concept of relationship reciprocity conveyed in the Introduction, we choose three items derived from the Reciprocity Subscale of the Mutuality Scale that best matched with contextual theory and adapted accordingly (e.g., “How often does he or she express feelings of appreciation for you and the things you do?” was replaced by “The other gives me acknowledgement for what I do for him/her”). The three items showed satisfactory reliability (αPT = .80; αCG = .81) and high intra-correlations (for patients: ritem1-item2 = .55, ritem1-item3 = .61, ritem2-item3 = .60; for caregivers: ritem1-item2 = .64, ritem1-item3 = .59, ritem2-item3 = .52; ps < .001). The three scores were summed to get the total relationship reciprocity Index with higher scores indicating a better quality of relationship reciprocity (αPT = .80; αCG = .81).
Patients’ quality of life
The Italian version of the Short-Form-36 Health Survey (SF-36) was used to assess patients’ health status (Ware, 2003). SF-36 has been widely used in cancer patients and it comprises eight health sub-scales: Physical functioning (α = .92), Limitations physical health (α = .87), Limitations emotional problems (α = .80), Energy fatigue (α = .82), Emotional well-being (α = .84), Social functioning (α = .83), Pain (α = .88), and General health (α = .70). SF-36 indicates strengths and weaknesses of patient functioning.
Caregivers’ burden
Caregivers were evaluated for burden of care using the Italian version of the Caregiver Burden Inventory (CBI), widely used to evaluate caregivers’ burden of chronically ill patients, including cancer (Novak & Guest, 1989). The scale consists of twenty-four 5-point items (0 = not at all disruptive; 4 = very disruptive) and provides five dimensions: Time Dependence (α = .88), Developmental (α = .83), Physical (α = .85), Social (α = .75), and Emotional (α = .77), with higher values indicating higher levels of burden.
Procedure
Ethical approval was obtained by the Ethical Committees of participating institutions. Detailed procedures were shared among all participating centers to ensure uniformity in the research setting. A research psychologist personally offered the study to patients and caregivers at the time of admission to the unitFootnote 2 in order to enroll participants. They were all assured that declining to participate would not affect their medical care, and their informed consent was obtained after discussing any study ramifications. Patients and carers completed their self-administered questionnaires independently, without consulting one another, in the presence of a research staff member.
Information regarding socio-demographics and health features was collected from participants, patient charts and physician consultation. Each dyad was assigned a code number to be reported on their completed questionnaires followed by ‘PT’ (patient) or ‘CG’ (caregiver) accordingly. In this way it was possible to keep track of the dyadic information, while preserving anonymity.
Data analyses
Socio-demographics and clinical characteristics of patient and caregiver samples were calculated and results were expressed as mean ± sd for continuous and ordinal variables and as frequencies and percentages for categorical variables (Tables 1). To assess Aim (1), Pearson’s correlation analyses were also conducted to assess the associations between fatigue, distress, relationship reciprocity, patients’ QoL and caregivers’ burden (Table 2). Mentioned analyses were performed with SPSS Statistics 21 (IBM Corp. Released, 2012).
The APIM was run to assess our principal Aim (2) and test the inter-relatedness of relationship reciprocity, fatigue and distress in dyads by taking both patient and caregiver contributions into account in a single regression model. To date, APIM represents the most adopted conceptual and statistical framework for dyadic data analysis (Cook & Kenny, 2005; Ledermann & Kenny, 2015). The strength of using APIM consists in concurrently test the effect of one’s own predictor on one’s own outcome and on the outcome of the other dyad member. Because it tackles the dyad’s interdependence, or how dyad members impact and contribute to shaping their relationship, it is a crucial tool for researching dyadic interpersonal dynamics (Kenny et al., 2020). The APIM specifically tested the ‘actor effect’—a person’s own characteristics, such as relationship reciprocity, on their own outcomes, such as fatigue and distress—and the ‘partner effect’—a person’s own characteristics, such as relationship reciprocity, on the other dyad member’s outcomes, such as fatigue and distress. In the distinguishable standard dyadic design, there are two actor effects and two partner effects. A distinguishable standard dyadic design in which each person of the dyad has one and only partner was estimated, and the factor role clearly differentiated the two members: patients vs. caregivers. Illness severity was included in the APIM analysis as priori covariate and it has been examined in terms of association with the variables of interest. The illness severity is given by the extent of the disease Local versus Metastatic. The APIM analyses were conducted using the user-friendly web application developed by Stas et al. (2018) “[…] which automatically performs the statistical analyses associated with the APIM, using lavaan. Because structural equation model (SEM) techniques are used to fit the APIM, the app is called APIM_SEM. […] The program is written in shiny (Chang et al., 2015), a web application framework for R (R Core Team, 2016) by RStudio (RStudio Team, 2015), and has an appealing point-and-click interface.” (Stas et al., 2018).
Results
Socio-demographics and clinical characteristics of the sample
Participants were predominantly advanced middle-aged and married, with caregivers (CG) slightly younger than patients (PT) (MCG = 53.47; MPT = 60.53), moreover CG had higher educational level (high schoolCG ≥ 63.1% vs. high schoolPT ≥ 36.2%) and active life in terms of occupation (CG = 47.7% vs. PT = 28.6%) as meaning that the PT were more often pensioners or housewives. In both groups, the gender distribution was somewhat skewed toward a female component; in the caregiver subgroup, females (299) were slightly prevalent than males (245). About half caregivers (52.11%) were the patient’s spouse/partner (174 men vs 110 women) and about a quarter (25.87) were adult children (40 men vs 101 women).
Most patients had been diagnosed within five years (about 86%) with almost half of them diagnosed within one year. Breast (33.9%) and gastrointestinal (26.1%) cancer were the most representative in terms of diagnosis. On the average, patients’ Karnowsky Performance Status (KPS) demonstrated capability to carry normal activity with effort, with some signs of disease (M = 82.35). At the time of the study, more than half patients presented metastasis, 85% were involved in treatment (prevalently chemotherapy), while about half patient sub-sample had also been treated previously and about three quarters had had surgery. Among concomitant symptoms, sleep disorders were predominant (27.3%), followed by pain (19.3%), cognitive disorders (16.1%), and anemia (10.3%). Table 1 provides demographic and clinical characteristics of both patients and caregivers.
Correlations between fatigue, distress, relationship reciprocity, QoL and burden
Pearson’s correlations were conducted to examine the associations between fatigue, distress, relationship reciprocity, patients’ QoL and caregivers’ Burden, in patient and caregiver sub-samples (see Table 2). There were positive correlations between fatigue and distress (anxiety and depression) for both patients and caregivers. Relationship reciprocity appeared negatively associated with all dimensions of fatigue and distress for both sub-samples. As presumable, patient QoL and caregiver burden were negatively and positively, respectively, correlated with all fatigue and distress dimensions. In addition, correlation analyses supported the role of relationship reciprocity on fatigue and distress symptoms.
The dyadic association of relationship reciprocity with fatigue and distress in patients and caregivers
To address our principal aim (2) of the study, five APIMs were conducted for three EORTC-12 (Physical, Emotional, and Cognitive fatigue) and for two distress (Anxiety and Depression) outcomes. Given the sample heterogeneity with respect to the illness trajectory, time from diagnosis and stages of disease, the patient’s Illness severity was included as covariate. Table 3 summarizes the Actor and the Partner effects of relationship reciprocity on fatigue and distress.
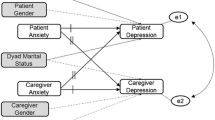
The APIM findings revealed a statistically significant actor influence of one’s own relationship reciprocity on all outcomes of one’s own fatigue (Physical, Emotional, and Cognitive) and distress (Anxiety and Depression), for both patients and caregivers (ps < .001). According to these findings, patients or caregivers who expressed greater connection reciprocity experienced less weariness and anxiety. Furthermore, there were statistically significant partner effects of caregivers’ relationship reciprocity on patients’ Emotional fatigue (β = −.54, p = .03, effect size = −.1), Cognitive fatigue (β = −.54, p = .03, effect size = −.1), Anxiety (β = −.13, p = .003, effect size = −.13), and Depression (β = −.09, p = .04, effect size = −.11). These results indicated that when the caregiver reported high levels of relationship reciprocity the other dyad member - i.e., the patient - exhibited less fatigue and distress. In contrast, there were no statistically significant partner effects of patients’ relationship reciprocity on caregivers’ fatigue and distress. Testing Illness severity as covariate did not change the actor and partner effects of the model. Table 3 reports the APIM results (Fig. 1).
Shows the standard models with covariate estimated. Standard APIM for (a) Physical, (b) Emotional, (c) Cognitive Fatigue and for Distress – (d) Anxiety and (e) Depression. The double-headed arrows between ‘Reciprocity of Relationship Caregiver’ and ‘Reciprocity of Relationship Patient’ represent their covariance. The double-headed arrows between ‘Fatigue/Distress Patient’ and ‘Fatigue/Distress Caregiver’ are the residual nonindependence in these outcome scores, which are represented by the covariance between their corresponding two error terms. Unstandardized parameter estimates, standard error and level of significance are reported. *p < .05; **p < .01; ***p < .001
Discussion
This multicenter cross-sectional study examined the associations among fatigue, distress, patient QoL, caregiver burden and relationship reciprocity in patient-caregiver dyads in a cohort of Italian outpatients undergoing oncological procedures. The following findings deserve discussion. In regard to the first aim of the study, correlation analyses have shown negative association of patient QoL and positive association of caregiver burden with all fatigue and distress dimensions. Last but not least, the APIM demonstrated that each individual’s relationship reciprocity was related to their own distress and fatigue (actor effects); only caregivers’ relationship reciprocity was related to patients’ distress and fatigue.
As far as the first aim, as previously mentioned, we have found that patient QoL was negativetely associated with all fatigue and distress dimensions while caregiver burden was positivitely associted with the same domensions; this is consistent with other studies that found that patients’ and caregivers’ emotional symptoms were related to their own QoL (Milbury et al., 2013). Relationship reciprocity was negatively associated with all dimensions of fatigue and distress for both sub-samples; consequently, relationship reciprocity has implications for both patient QoL and caregiver burden, where both patients and relatives are likely to benefit from increased quality of relationship reciprocity that reduce fatigue and distress. The significant correlation among all these aspects confirms what reported in the literature (Reid et al., 2005; Ybema et al., 2002) regarding the role of reciprocity in the patient-caregiver relationship and suggests that relationship reciprocity must be taken into consideration when evaluating the QoL of both patients and caregivers.
The distinct contribute of the current study was to examine the reciprocal relationships between the symptoms of fatigue and distress experienced by patients and their caregivers (Aim 2). The results showed that there were significant actor effects on each person’s level of discomfort and exhaustion, indicating that those who had insufficient or poor relationship reciprocity were at risk of experiencing an increase in these symptoms.
Regarding the role played by one’s own perceived marital satisfaction in reducing own distress, this finding is consistent with the findings of previous studies conducted among cancer patients (Hagedoorn et al., 2008) as well as studies conducted among patients with other chronic illnesses such as diabetes (Trief et al., 2006) and acute coronary syndrome (Dekel et al., 2014).
The generalization of results to other pathologies may be due to the fact that relationship reciprocity is a construct that is based on the role played by the actors acting in the dyad and not by the type of pathology. Previous research about the patient-caregiver relationship has primarily focused on the effect of perceived reciprocity/mutuality on patient’s depression/QoL or on caregiver’s burden (Buunk & Schaufeli, 1999; Gleason et al., 2003; McPherson et al., 2011; Reid et al., 2005). The patient-caregiver dyad has not been extensively studied as a unit of care (Badr et al., 2014; Kershaw et al., 2015); none in regard to the interdependence between relationship reciprocity and fatigue and distress. In a recent review of the literature on interdependent physical and psychological morbidity in patients with cancer and family caregivers, Streck et al. (2020) found that the studies demonstrated a stronger relationship between patients’ and caregivers’ psychological morbidity than between their physical morbidity. However, the studies used a range of techniques and cancer types, and the results were discordant, indicating variable interdependence.
In the current study, dyadic analyses revealed important partner effects only on the side of caregivers’ relationship reciprocity on all patients’ fatigue and distress symptoms. The transmission of the effect from the partner to the patient is consistent with research on interdependence in psychological QoL, study showed indications of long-term dyadic interdependence for psychological QOL, especially from partners to patients, in dyads adjusting to breast cancer and prostate cancer (Segrin et al., 2006, 2007, 2012).
The current study seemingly is the first one to perform a dyadic approach to the analysis of fatigue and cancer patients’ and their caregivers’ distress signs in relation to the reciprocity of their relationships. The assumption deriving from contestual teory is that reciprocity in the patient-caregiver relationship would have an effect on symptoms of distress and fatigue for both patients and caregivers. While this is confirmed by the actor effect of the model, the fact that the only partner’s effect is from caregivers to patients and non viceversa leads to some speculations. According to contextual theory, one hypothesis might be that caregivers may feel a lack of entitlemnet to receive, as if they perform the role of a “giver” only. On the other hand, it may also suggest that patients may be particularly vulnerable to caregivers’ perception of their relationship, whereas caregivers are not. In both instances, these findings go into the direction indicated by Bower (2019) and Mustian et al. (2017) that there must be other factors, besides cancer and its treatment, that contribute to the development and persistence of fatigue. Although aware of the weekness of a cross-sectional study, still current findings encourage to further investigate the interdependence between relationship reciprocity and the psychophysical health of both patients and caregivers.
Limitations
The study has several limitations. The cross-sectional design meant that directionality or causality between the variables could not be determined. Future studies might benefit from looking at the evolution of relationships between caregivers and care recipients as they adjust to the changes brought on by cancer. Advanced cancer frequently results in a continuous decline in functioning, necessitating adaptation on the part of both the patient and caregiver that is different from what is required during early disease. The study only looked at an Italian population; patients and caregivers may interact and have different expectations in families from other cultures. Therefore, it is important to examine actor and partner impacts in various settings and cultural/ethnic groupings. The convenience sampling methodology further raises concerns about the representativeness of the current findings. Another limitation is the absence of a standardized, specific instrument to measure relationship reciprocity. Despite these limitations, the study bears some strengths. The concomitant evaluation of fatigue and distress symptoms within a real life, controlled situation, across a variety of dyads (in terms of cancer diagnosis and severity and caregiver role) and across the country, is an asset of this study. Even though the analyses were based on cross-sectional data, which restricted the conclusions about the directionality, temporality of the relationships, and sensitivity to change over time, they nevertheless enabled us to increase our understanding of the psychological effects that cancer has on families in various cancer cases and caregiving relationships. Replication of this research in different cultural and ethnic contexts and through sample randomization is needed to generalize results.
Conclusions
In terms of research and clinical implications, this study contributes to bring attention to the analysis of those mechanisms by which patient-caregiver relationship plays a role in fatigue and distress for both dyadic members. According to contextual theory, the investment of family members to achieve a reciprocal give-and-take, in terms of commitment to the well-being of the other, is what shapes relational mutuality over time, so our study demostate that relationship reciprocity could help the dyad to increase QoL of patient and decrease caregiver burden in the way of less levels of distress and fatigue. This study may also help informing the development of dyadic interventions that will enhance patient and caregiver outcomes in the context of a rapidly progressing and life-threatening disease by assessing a potential intervention that could maximize the benefits of relationship reciprocity and reciprocal give-and-take.
Data availability
There is no public access to the datasets created for and/or used in this study due their containing information that could compromise the privacy of patients involved in the study but are available from the corresponding author [TL] on reasonable request.
Notes
Four centers were from Northern Italy (Milan, Piacenza, Novara, Aviano), two from Central Italy (Rome, Pescara), seven from Southern Italy (Naples, Rionero in Vulture, Foggia, Bari-4 centers), and two from Sicily (Siracusa, Catania).
The majority of patients going for a visit or for therapy to Italian cancer centers are accompanied by a family member, usually their caregiver.
References
Annunziata, M. A., Muzzatti, B., Bidoli, E., Flaiban, C., Bomben, F., Piccinin, M., Gipponi, K. M., Mariutti, G., Busato, S., & Mella, S. (2020). Hospital anxiety and depression scale (HADS) accuracy in cancer patients. Supportive Care in Cancer, 28(8), 3921–3926. https://doi.org/10.1007/s00520-019-05244-8
Badr, H., Gupta, V., Sikora, A., & Posner, M. (2014). Psychological distress in patients and caregivers over the course of radiotherapy for head and neck Cancer. Oral Oncology, 50(10), 1005–1011. https://doi.org/10.1016/j.oraloncology.2014.07.003
Berger, A. M., Gerber, L. H., & Mayer, D. K. (2012). Cancer-related fatigue: Implications for breast cancer survivors. Cancer, 118(S8), 2261–2269. https://doi.org/10.1002/cncr.27475
Berger, A. M., Fernandez-Robles, C., & Murphy, B. A. (2018). NCCN Guidelines Index Table of Contents Discussion. 64.
Boszormenyi-Nagy, I. K. (2013). Between Give And Take (0 ed.). Routledge. https://doi.org/10.4324/9780203776315
Boszormenyi-Nagy, I., & Krasner, B. R. (1986). Between give and take: A clinical guide to contextual therapy. Psychology Press.
Bower, J. E. (2014). Cancer-related fatigue—Mechanisms, risk factors, and treatments. Nature Reviews Clinical Oncology, 11(10), 597–609. https://doi.org/10.1038/nrclinonc.2014.127
Bower, J. E. (2019). The role of neuro-immune interactions in cancer-related fatigue: Biobehavioral risk factors and mechanisms. Cancer, 125(3), 353–364. https://doi.org/10.1002/cncr.31790
Bower, J. E., & Lamkin, D. M. (2013). Inflammation and cancer-related fatigue: Mechanisms, contributing factors, and treatment implications. Brain, Behavior, and Immunity, 30, S48–S57. https://doi.org/10.1016/j.bbi.2012.06.011
Bower, J. E., Ganz, P. A., Irwin, M. R., Kwan, L., Breen, E. C., & Cole, S. W. (2011). Inflammation and behavioral symptoms after breast Cancer treatment: Do fatigue, depression, and sleep disturbance share a common underlying mechanism? Journal of Clinical Oncology, 29(26), 3517–3522. https://doi.org/10.1200/JCO.2011.36.1154
Brown, L. F., & Kroenke, K. (2009). Cancer-related fatigue and its associations with depression and anxiety: A systematic review. Psychosomatics, 50(5), 440–447. https://doi.org/10.1016/S0033-3182(09)70835-7
Buunk, B. P., & Schaufeli, W. B. (1999). Reciprocity in interpersonal relationships: An evolutionary perspective on its importance for health and well-being. European Review of Social Psychology, 10(1), 259–291. https://doi.org/10.1080/14792779943000080
Camara, C., Caroline Vos, M., de Rooij, B. H., Pijnenborg, J. M. A., Boll, D., van de Poll-Franse, L. V., & Ezendam, N. P. M. (2019). The role of positive psychological changes in anxiety and depression of patients with ovarian tumors and their partners: An observational study from the population-based PROFILES registry. Supportive Care in Cancer, 27(2), 423–431. https://doi.org/10.1007/s00520-018-4327-6
Chang, W., Cheng, J., Allaire, J. J., Xie, Y., & McPherson, J. (2015). Shiny: Web application framework for R. R package version 0.12.1. https://CRAN.R-project.org/package=shiny
Clark, M. M., Atherton, P. J., Lapid, M. I., Rausch, S. M., Frost, M. H., Cheville, A. L., Hanson, J. M., Garces, Y. I., Brown, P. D., Sloan, J. A., Richardson, J. W., Piderman, K. M., & Rummans, T. A. (2014). Caregivers of patients with Cancer fatigue: A high level of symptom burden. American Journal of Hospice and Palliative Medicine®, 31(2), 121–125. https://doi.org/10.1177/1049909113479153
Cook, W. L., & Kenny, D. A. (2005). The actor–partner interdependence model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development, 29(2), 101–109. https://doi.org/10.1080/01650250444000405
Curci, A., & Rimé, B. (2012). The temporal evolution of social sharing of emotions and its consequences on emotional recovery: A longitudinal study. Emotion, 12(6), 1404–1414. https://doi.org/10.1037/a0028651
Dekel, R., Vilchinsky, N., Liberman, G., Leibowitz, M., Khaskia, A., & Mosseri, M. (2014). Marital satisfaction and depression among couples following men’s acute coronary syndrome: Testing dyadic dynamics in a longitudinal design. British Journal of Health Psychology, 19(2), 347–362. https://doi.org/10.1111/bjhp.12042
Gaston-Johansson, F., Lachica, E. M., Fall-Dickson, J. M., & John Kennedy, M. (2004). Psychological distress, fatigue, burden of care, and quality of life in primary caregivers of patients with breast Cancer undergoing autologous bone marrow transplantation. Oncology Nursing Forum, 31(6), 1161–1169. https://doi.org/10.1188/04.ONF.1161-1169
Gleason, M. E. J., Iida, M., Bolger, N., & Shrout, P. E. (2003). Daily supportive equity in close relationships. Personality and Social Psychology Bulletin, 29(8), 1036–1045. https://doi.org/10.1177/0146167203253473
Grassi, L., Johansen, C., Annunziata, M. A., Capovilla, E., Costantini, A., Gritti, P., Torta, R., Bellani, M., & on behalf of the Italian Society of Psycho-Oncology Distress Thermometer Study Group. (2013). Screening for distress in cancer patients: A multicenter, nationwide study in Italy. Cancer, 119(9), 1714–1721. https://doi.org/10.1002/cncr.27902
Gurman, A. S., & Kniskern, D. P. (1991). Handbook of family therapy (2nd ed.).
Hagedoorn, M., Sanderman, R., Bolks, H. N., Tuinstra, J., & Coyne, J. C. (2008). Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychological Bulletin, 134(1), 1–30. https://doi.org/10.1037/0033-2909.134.1.1
Holland, J. C. (2013). Distress screening and the integration of psychosocial care into routine oncologic care. Journal of the National Comprehensive Cancer Network, 11(5S), 687–689. https://doi.org/10.6004/jnccn.2013.0202
IBM Corp. Released. (2012). IBM SPSS statistics for windows (21.0). IBM Corp.
Jacobs, J. M., Shaffer, K. M., Nipp, R. D., Fishbein, J. N., MacDonald, J., El-Jawahri, A., Pirl, W. F., Jackson, V. A., Park, E. R., Temel, J. S., & Greer, J. A. (2017). Distress is interdependent in patients and caregivers with newly diagnosed incurable cancers. Annals of Behavioral Medicine, 51(4), 519–531. https://doi.org/10.1007/s12160-017-9875-3
Karlstedt, M., Fereshtehnejad, S.-M., Aarsland, D., & Lökk, J. (2017). Determinants of dyadic relationship and its psychosocial impact in patients with Parkinson’s disease and their spouses. Parkinson’s Disease, 2017, 1–9. https://doi.org/10.1155/2017/4697052
Kayser, K., & Acquati, C. (2019). The influence of relational mutuality on dyadic coping among couples facing breast cancer. Journal of Psychosocial Oncology, 37(2), 194–212. https://doi.org/10.1080/07347332.2019.1566809
Kenny, D. A., Kashy, D. A., & Cook, W. L. (2020). Dyadic data analysis. Guilford Publications.
Kershaw, T., Ellis, K. R., Yoon, H., Schafenacker, A., Katapodi, M., & Northouse, L. (2015). The interdependence of advanced Cancer patients’ and their family caregivers’ mental health, physical health, and self-efficacy over time. Annals of Behavioral Medicine, 49(6), 901–911. https://doi.org/10.1007/s12160-015-9743-y
Langenberg, S. M. C. H., van Herpen, C. M. L., van Opstal, C. C. M., Wymenga, A. N. M., van der Graaf, W. T. A., & Prins, J. B. (2019). Caregivers’ burden and fatigue during and after patients’ treatment with concomitant chemoradiotherapy for locally advanced head and neck cancer: A prospective, observational pilot study. Supportive Care in Cancer, 27(11), 4145–4154. https://doi.org/10.1007/s00520-019-04700-9
Ledermann, T., & Kenny, D. A. (2015). A toolbox with programs to restructure and describe dyadic data. Journal of Social and Personal Relationships, 32(8), 997–1011. https://doi.org/10.1177/0265407514555273
McPherson, C. J., Wilson, K. G., Chyurlia, L., & Leclerc, C. (2010). The balance of give and take in caregiver–partner relationships: An examination of self-perceived burden, relationship equity, and quality of life from the perspective of care recipients following stroke. Rehabilitation Psychology, 55(2), 194–203. https://doi.org/10.1037/a0019359
McPherson, C. J., Wilson, K. G., Chyurlia, L., & Leclerc, C. (2011). The caregiving relationship and quality of life among partners of stroke survivors: A cross-sectional study. Health and Quality of Life Outcomes, 9(1), 29. https://doi.org/10.1186/1477-7525-9-29
Milbury, K., Badr, H., Fossella, F., Pisters, K. M., & Carmack, C. L. (2013). Longitudinal associations between caregiver burden and patient and spouse distress in couples coping with lung cancer. Supportive Care in Cancer, 21(9), 2371–2379. https://doi.org/10.1007/s00520-013-1795-6
Minton, O., Berger, A., Barsevick, A., Cramp, F., Goedendorp, M., Mitchell, S. A., & Stone, P. C. (2013). Cancer-related fatigue and its impact on functioning: Cancer-related fatigue. Cancer, 119, 2124–2130. https://doi.org/10.1002/cncr.28058
Mustian, K. M., Alfano, C. M., Heckler, C., Kleckner, A. S., Kleckner, I. R., Leach, C. R., Mohr, D., Palesh, O. G., Peppone, L. J., Piper, B. F., Scarpato, J., Smith, T., Sprod, L. K., & Miller, S. M. (2017). Comparison of pharmaceutical, psychological, and exercise treatments for Cancer-related fatigue: A Meta-analysis. JAMA Oncology, 3(7), 961. https://doi.org/10.1001/jamaoncol.2016.6914
Novak, M., & Guest, G. (1989). Caregiver burden inventory (CBI). Gerontologist, 29, 798–803.
O’Higgins, C. M., Brady, B., O’Connor, B., Walsh, D., & Reilly, R. B. (2018). The pathophysiology of cancer-related fatigue: Current controversies. Supportive Care in Cancer, 26(10), 3353–3364. https://doi.org/10.1007/s00520-018-4318-7
Peters, M. E. W. J., Goedendorp, M. M., Verhagen, S. A. H. H. V. M., Smilde, T. J., Bleijenberg, G., & van der Graaf, W. T. A. (2015). A prospective analysis on fatigue and experienced burden in informal caregivers of cancer patients during cancer treatment in the palliative phase. Acta Oncologica, 54(4), 500–506. https://doi.org/10.3109/0284186X.2014.953254
Pucciarelli, G., Buck, H. G., Barbaranelli, C., Savini, S., Simeone, S., Juarez-Vela, R., Alvaro, R., & Vellone, E. (2016). Psychometric characteristics of the mutuality scale in stroke patients and caregivers. The Gerontologist, 56(5), e89–e98. https://doi.org/10.1093/geront/gnw083
R Core Team (2016). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. https://www.R-project.org/
Regan, T. W., Lambert, S. D., Kelly, B., Falconier, M., Kissane, D., & Levesque, J. V. (2015). Couples coping with cancer: Exploration of theoretical frameworks from dyadic studies: Couples and cancer: Dyadic theoretical frameworks. Psycho-Oncology, 24(12), 1605–1617. https://doi.org/10.1002/pon.3854
Reid, C. E., Moss, S., & Hyman, G. (2005). Caregiver reciprocity: The effect of reciprocity, carer self-esteem and motivation on the experience of caregiver burden. Australian Journal of Psychology, 57(3), 186–196. https://doi.org/10.1080/00049530500141022
RStudio Team (2015). RStudio: Integrated Development for R. RStudio, Inc., Boston, MA (Computer Software v0.98.1074). http://www.rstudio.com/
Segrin, C., Badger, T., Sieger, A., Meek, P., & Lopez, A. M. (2006). Interpersonal well-being and mental health among male partners of woman with breast cancer. Issues in Mental Health Nursing, 27(4), 371–389. https://doi.org/10.1080/01612840600569641
Segrin, C., Badger, T., Dorros, S. M., Meek, P., & Lopez, A. M. (2007). Interdependent anxiety and psychological distress in women with breast cancer and their partners. Psycho-Oncology, 16(7), 634–643. https://doi.org/10.1002/pon.1111
Segrin, C., Badger, T. A., & Harrington, J. (2012). Interdependent psychological quality of life in dyads adjusting to prostate cancer. Health Psychology, 31(1), 70–79. https://doi.org/10.1037/a0025394
Smith, T. G., Troeschel, A. N., Castro, K. M., Arora, N. K., Stein, K., Lipscomb, J., Brawley, O. W., McCabe, R. M., Clauser, S. B., & Ward, E. (2019). Perceptions of patients with breast and Colon Cancer of the Management of Cancer-Related Pain, fatigue, and emotional distress in community oncology. Journal of Clinical Oncology, 37(19), 1666–1676. https://doi.org/10.1200/JCO.18.01579
Stas, L., Kenny, D. A., Mayer, A., & Loeys, T. (2018). Giving dyadic data analysis away: A user-friendly app for actor–partner interdependence models. Personal Relationships, 25(1), 103–119. https://doi.org/10.1111/pere.12230
Streck, B. P., Wardell, D. W., LoBiondo-Wood, G., & Beauchamp, J. E. S. (2020). Interdependence of physical and psychological morbidity among patients with cancer and family caregivers: Review of the literature. Psycho-Oncology, 29(6), 974–989. https://doi.org/10.1002/pon.5382
Tan, J. Y., Molassiotis, A., Lloyd-Williams, M., & Yorke, J. (2018). Burden, emotional distress and quality of life among informal caregivers of lung cancer patients: An exploratory study. European Journal of Cancer Care, 27(1), 1–11. https://doi.org/10.1111/ecc.12691
Trief, P. M., Morin, P. C., Izquierdo, R., Teresi, J., Starren, J., Shea, S., & Weinstock, R. S. (2006). Marital quality and diabetes outcomes: The IDEATel project. Families, Systems & Health, 24(3), 318–331. https://doi.org/10.1037/1091-7527.24.3.318
Ware, J. E. J. (2003). SF-36 health survey: Manual and interpretation guide.
Weis, J., Tomaszewski, K. A., Hammerlid, E., Ignacio Arraras, J., Conroy, T., Lanceley, A., Schmidt, H., Wirtz, M., Singer, S., Pinto, M., Alm El-Din, M., Compter, I., Holzner, B., Hofmeister, D., Chie, W.-C., Czeladzki, M., Harle, A., Jones, L., Ritter, S., … on Behalf of the EORTC Quality of Life Group. (2017). International psychometric validation of an EORTC quality of life module measuring Cancer related fatigue (EORTC QLQ-FA12). JNCI: Journal of the National Cancer Institute, 109(5). https://doi.org/10.1093/jnci/djw273
Ybema, J. F., Kuijer, R. G., Hagedoorn, M., & Buunk, B. P. (2002). Caregiver burnout among intimate partners of patients with a severe illness: An equity perspective. Personal Relationships, 9(1), 73–88. https://doi.org/10.1111/1475-6811.00005
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Acknowledgments
Other contributing investigators: Valentina Abate, Chiara Abbatantuono, Maria Acquafresca, Daniela Barberio, Francesco Cappuccio, Chiara Citterio, Camilla Di Nunzo, Mariachiara Foresio, Cira Antonietta Forte, Giorgia Gintili, Maria Lombardi, Vittoria Losurdo, Enrica Maggio, Sebastiana Roccaro, Licia Santamaria, Florian Stratica, Veronica Verri, Veronica Villani. Grateful acknowledgements to all institutional staff members for their help with recruitment and to all participant patients and caregivers for their contribution.
Funding
Open access funding provided by Università degli Studi di Bari Aldo Moro within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The corresponding author declares that there are no competing interests on behalf of the other writers.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Taurisano, P., De Feudis, R.L., Graziano, G. et al. Patient-caregiver relationship in cancer fatigue and distress. A dyadic approach. Curr Psychol 42, 28167–28179 (2023). https://doi.org/10.1007/s12144-022-03860-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-03860-y