Abstract
Purpose
The aim of this study is to investigate whether previous abdominal surgery (PAS) affected stage I-III colorectal cancer (CRC) patients who underwent radical resection.
Methods
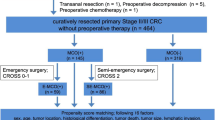
Stage I-III CRC patients who received surgery at a single clinical center from Jan 2014 to Dec 2022 were retrospectively included in this study. Baseline characteristics and short-term outcomes were compared between the PAS group and the non-PAS group. Univariate and multivariate logistic regression analyses were used to find risk factors for overall complications and major complications. A 1:1 ratio propensity score matching (PSM) was used to minimize the selection bias between the two groups. Statistical analysis was performed using SPSS (version 22.0) software.
Results
A total of 5895 stage I-III CRC patients were included according to the inclusion and exclusion criteria. The PAS group had 1336 (22.7%) patients, and the non-PAS group had 4559 (77.3%) patients. After the PSM, there were 1335 patients in each group, and no significant difference was found in all baseline characteristics between the two groups (P > 0.05). After comparing the short-term outcomes, the PAS group had a longer operation time (before PSM, P < 0.01; after PSM, P < 0.01) and more overall complications (before PSM, P = 0.027; after PSM, P = 0.022) whether before or after PSM. In univariate and multivariate logistic regression analyses, PAS was an independent risk factor for overall complications (univariate analysis, P = 0.022; multivariate analysis, P = 0.029) but not for major complications (univariate analysis, P = 0.688).
Conclusion
Stage I-III CRC patients with PAS might experience longer operation time and have a higher risk of postoperative overall complications. However, it did not appear to significantly affect the major complications. Surgeons should take steps to improve surgical outcomes for patients with PAS.

Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Adeleke S, Haslam A, Choy A, Diaz-Cano S, Galante JR, Mikropoulos C, et al. Microsatellite instability testing in colorectal patients with lynch syndrome: lessons learned from a case report and how to avoid such pitfalls. Per Med. 2022;19(4):277–86. https://doi.org/10.2217/pme-2021-0128.
Akagi T, Nakajima K, Hirano Y, Abe T, Inada R, Kono Y, et al. Laparoscopic versus open resection for stage II/III rectal cancer in obese patients: a multicenter propensity score-based analysis of short- and long-term outcomes. Ann Gastroenterol Surg. 2022;7(1):71–80. https://doi.org/10.1002/ags3.12599.
Tang J, Liu J, Du B, Zhang J, Zheng L, Wang X, et al. Short- and long-term outcomes of laparoscopic versus open pelvic exenteration for locally advanced rectal cancer: a single-center propensity score matching analysis. Tech Coloproctol. 2023;27(1):43–52. https://doi.org/10.1007/s10151-022-02691-0.
Samalavicius NE, Kuliesius Z, Samalavičius RS, Tikuisis R, Smolskas E, Gricius Z, et al. Hand assisted laparoscopic surgery for colorectal cancer: surgical and oncological outcomes from a single tertiary referral centre. J Clin Med. 2022;11(13):3781. https://doi.org/10.3390/jcm11133781.
Safiejko K, Tarkowski R, Koselak M, Juchimiuk M, Tarasik A, Pruc M, et al. Robotic-assisted vs. Standard laparoscopic surgery for rectal cancer resection: a systematic review and meta-analysis of 19,731 patients. Cancers (Basel). 2021;14(1):180. https://doi.org/10.3390/cancers14010180.
Watanabe M. Current status of and outlook for the latest minimally invasive surgery for colorectal diseases. Nihon Geka Gakkai Zasshi. 2015;116(5):297–301.
Morneau M, Boulanger J, Charlebois P, Latulippe JF, Lougnarath R, Thibault C, et al. Laparoscopic versus open surgery for the treatment of colorectal cancer: a literature review and recommendations from the Comité de l’évolution des pratiques en oncologie. Can J Surg. 2013;56(5):297–310. https://doi.org/10.1503/cjs.005512.
Kronberg U, Kiran RP, Soliman MS, Hammel JP, Galway U, Coffey JC, et al. A characterization of factors determining postoperative ileus after laparoscopic colectomy enables the generation of a novel predictive score. Ann Surg. 2011;253(1):78–81. https://doi.org/10.1097/SLA.0b013e3181fcb83e.
Franko J, O’Connell BG, Mehall JR, Harper SG, Nejman JH, Zebley DM, et al. The influence of prior abdominal operations on conversion and complication rates in laparoscopic colorectal surgery. JSLS. 2006;10(2):169–75.
Offodile AC 2nd, Lee SW, Yoo J, Whelan RL, Moradi D, Baxter R, et al. Does prior abdominal surgery influence conversion rates and outcomes of laparoscopic right colectomy in patients with neoplasia? Dis Colon Rectum. 2008;51(11):1669–74. https://doi.org/10.1007/s10350-008-9278-4.
Siegel R, Cuesta MA, Targarona E, Bader FG, Morino M, Corcelles R, et al. Laparoscopic extraperitoneal rectal cancer surgery: the clinical practice guidelines of the European association for endoscopic surgery (EAES). Surg Endosc. 2011;25(8):2423–40. https://doi.org/10.1007/s00464-011-1805-z.
Gilshtein H, Yellinek S, Setton I, Wexner SD. What are the results of laparoscopic re-operative rectal surgery? Am J Surg. 2020;219(6):896–9. https://doi.org/10.1016/j.amjsurg.2019.12.003.
Weiser MR. AJCC 8th edition: colorectal cancer. Ann Surg Oncol. 2018;25(6):1454–5. https://doi.org/10.1245/s10434-018-6462-1.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96. https://doi.org/10.1097/SLA.0b013e3181b13ca2.
Kane LT, Fang T, Galetta MS, Goyal DKC, Nicholson KJ, Kepler CK, et al. Propensity score matching: a statistical method. Clin Spine Surg. 2020;33(3):120–2. https://doi.org/10.1097/BSD.0000000000000932.
Tam MS, Kaoutzanis C, Mullard AJ, Regenbogen SE, Franz MG, Hendren S, et al. A population-based study comparing laparoscopic and robotic outcomes in colorectal surgery. Surg Endosc. 2016;30(2):455–63. https://doi.org/10.1007/s00464-015-4218-6.
Greco F, Cindolo L, Autorino R, Micali S, Stein RJ, Bianchi G, et al. Laparoendoscopic single-site upper urinary tract surgery: assessment of postoperative complications and analysis of risk factors. Eur Urol. 2012;61(3):510–6. https://doi.org/10.1016/j.eururo.2011.08.032.
Li J, Guo H, Guan XD, Cai CN, Yang LK, Li YC, et al. The impact of laparoscopic converted to open colectomy on short-term and oncologic outcomes for colon cancer. J Gastrointest Surg. 2015;19(2):335–43. https://doi.org/10.1007/s11605-014-2685-z.
Patel CB, Ragupathi M, Ramos-Valadez DI, Haas EM. A three-arm (laparoscopic, hand-assisted, and robotic) matched-case analysis of intraoperative and postoperative outcomes in minimally invasive colorectal surgery. Dis Colon Rectum. 2011;54(2):144–50. https://doi.org/10.1007/DCR.0b013e3181fec377.
Liu XY, Yuan C, Kang B, Cheng YX, Tao W, Zhang B, et al. Predictors associated with planned and unplanned admission to intensive care units after colorectal cancer surgery: a retrospective study. Support Care Cancer. 2022;30(6):5099–105. https://doi.org/10.1007/s00520-022-06939-1.
Cheng YX, Tao W, Zhang H, Peng D, Wei ZQ. Does liver cirrhosis affect the surgical outcome of primary colorectal cancer surgery? A meta-analysis. World J Surg Oncol. 2021;19(1):167. https://doi.org/10.1186/s12957-021-02267-6.
Hoek VT, Edomskis PP, Menon AG, Dwarkasing RS, Kleinrensink GJ, Jeekel J, et al. Calcification of the aorta-iliac trajectory as a risk factor for anastomotic leakage in colorectal surgery: individual patient data meta-analysis and systematic review. Surg Technol Int. 2021;20(39):155–65. https://doi.org/10.52198/21.STI.39.CR1479.
Liu XY, Kang B, Cheng YX, Yuan C, Tao W, Zhang B, et al. Higher body mass index was associated with better prognosis in diabetic patients with stage II colorectal cancer. BMC Cancer. 2022;22(1):596. https://doi.org/10.1186/s12885-022-09691-1.
Wang WJ, Li HT, Yu JP, Su L, Guo CA, Chen P, et al. Severity and incidence of complications assessed by the Clavien-Dindo classification following robotic and laparoscopic gastrectomy for advanced gastric cancer: a retrospective and propensity score-matched study. Surg Endosc. 2019;33(10):3341–54. https://doi.org/10.1007/s00464-018-06624-7.
Cheng YX, Liu XY, Kang B, Tao W, Wei ZQ, Peng D. Comparison of surgical and oncologic outcomes in very elderly patients (≥ 80 years old) and elderly (65–79 years old) colorectal cancer patients: a propensity score matching. BMC Gastroenterol. 2022;22(1):205. https://doi.org/10.1186/s12876-022-02277-y.
Ouaïssi M, Gaujoux S, Veyrie N, Denève E, Brigand C, Castel B, et al. Post-operative adhesions after digestive surgery: their incidence and prevention: review of the literature. J Visc Surg. 2012;149(2):e104–14. https://doi.org/10.1016/j.jviscsurg.2011.11.006.
van der Wal JB, Iordens GI, Vrijland WW, van Veen RN, Lange J, Jeekel J. Adhesion prevention during laparotomy: long-term follow-up of a randomized clinical trial. Ann Surg. 2011;253(6):1118–21. https://doi.org/10.1097/SLA.0b013e318217e99c.
Toneman M, Groenveld T, Krielen P, Hooker A, de Wilde R, Torres-de la Roche LA, et al. Risk factors for adhesion-related readmission and abdominal reoperation after gynecological surgery: a nationwide cohort study. J Clin Med. 2023;12(4):1351. https://doi.org/10.3390/jcm12041351.
Zeng WG, Liu MJ, Zhou ZX, Hou HR, Liang JW, Wang Z, et al. Impact of previous abdominal surgery on the outcome of laparoscopic resection for colorectal cancer: a case-control study in 756 patients. J Surg Res. 2015;199(2):345–50. https://doi.org/10.1016/j.jss.2015.05.022.
Karaman K, Çakıroğlu H, Nogay FB, Şekeroğlu MR, Yilmaz F. The preventive effect of omega-3 fish oil on peritoneal adhesion formation. Pol Przegl Chir. 2023;95(4):1–5. https://doi.org/10.5604/01.3001.0016.2730.
Kim IK, Kang J, Baik SH, Lee KY, Kim NK, Sohn SK. Impact of prior abdominal surgery on postoperative prolonged ileus after ileostomy repair. Asian J Surg. 2018;41(1):86–91. https://doi.org/10.1016/j.asjsur.2016.07.006.
Kim IY, Kim BR, Kim YW. Impact of prior abdominal surgery on rates of conversion to open surgery and short-term outcomes after laparoscopic surgery for colorectal cancer. PLoS One. 2015;10(7): e0134058. https://doi.org/10.1371/journal.pone.0134058.
Stommel MW, de Wilt JH, ten Broek RP, Strik C, Rovers MM, van Goor H. Prior abdominal surgery jeopardizes quality of resection in colorectal cancer. World J Surg. 2016;40(5):1246–54. https://doi.org/10.1007/s00268-015-3390-0.
Kim IY, Kim BR, Kim YW. Impact of timing of conversion to open surgery on short-term and oncologic outcomes in patients undergoing minimally invasive surgery for colorectal cancer. Am Surg. 2017;83(1):71–7.
Ushigome H, Nishimura J, Takahashi Y, Yasui M, Ohue M, Yamada D, et al. Colorectal surgery in patients with prior pancreaticoduodenectomy. J Anus Rectum Colon. 2019;3(3):121–7. https://doi.org/10.23922/jarc.2019-005.
Park S, Kang J, Park EJ, Baik SH, Lee KY. Laparoscopic and robotic surgeries for patients with colorectal cancer who have had a previous abdominal surgery. Ann Coloproctol. 2017;33(5):184–91. https://doi.org/10.3393/ac.2017.33.5.184.
Ishida H, Ishiguro T, Ishibashi K, Ohsawa T, Kuwabara K, Okada N, et al. Impact of prior abdominal surgery on curative resection of colon cancer via minilaparotomy. Surg Today. 2011;41(3):369–76. https://doi.org/10.1007/s00595-010-4281-5.
Huang CW, Su WC, Chang TK, Ma CJ, Yin TC, Tsai HL, et al. Impact of previous abdominal surgery on robotic-assisted rectal surgery in patients with locally advanced rectal adenocarcinoma: a propensity score matching study. World J Surg Oncol. 2020;18(1):308. https://doi.org/10.1186/s12957-020-02086-1.
Sueda T, Tei M, Nishida K, Yoshikawa Y, Matsumura T, Koga C, et al. Impact of prior abdominal surgery on short-term outcomes following laparoscopic colorectal cancer surgery: a propensity score-matched analysis. Surg Endosc. 2022;36(6):4429–41. https://doi.org/10.1007/s00464-021-08794-3.
Liakakos T, Thomakos N, Fine PM, Dervenis C, Young RL. Peritoneal adhesions: etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Dig Surg. 2001;18(4):260–73. https://doi.org/10.1159/000050149.
Boussios S, Ozturk MA, Moschetta M, Karathanasi A, Zakynthinakis-Kyriakou N, Katsanos KH, et al. The developing story of predictive biomarkers colorectal cancer. J Pers Med. 2019;9(1):12. https://doi.org/10.3390/jpm9010012.
Acknowledgements
We acknowledge all the authors whose publications are referred to in our article.
Funding
Not appliance.
Author information
Authors and Affiliations
Contributions
DP contributed to the conception and design and administrative support; X-RL and DP contributed to the provision of study materials or patients; X-YL, FL, and Z-WL collected and assembled the data; X-RL and DP analyzed and interpreted the data; X-RL contributed to first manuscript writing; all authors finally approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Drs. Xu-Rui Liu, Dong Peng, Xiao-Yu Liu, Fei Liu, and Zi-Wei Li declare that they have no conflict of interest or financial ties to disclose.
Ethical approval and consent to participate
This study was conducted in accordance with the World Medical Association Declaration of Helsinki and was approved by the ethics committee (2022-k206). All patients signed informed consent.
Consent for publication
Not appliance.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, XR., Liu, F., Li, ZW. et al. The risk of postoperative complications is higher in stage I-III colorectal cancer patients with previous abdominal surgery: a propensity score matching analysis. Clin Transl Oncol 25, 3471–3478 (2023). https://doi.org/10.1007/s12094-023-03210-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03210-9