Abstract
Purpose
The purpose of the current study is to identify the predictors of planned and unplanned admission to intensive care units (ICU) after colorectal cancer (CRC) surgery.
Methods
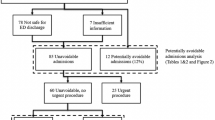
We retrospectively collected CRC patients’ information from January 2016 to June 2021 in a single clinical center. The predictors of planned and unplanned admission to ICU after CRC surgery were analyzed.
Results
A total of 4263 patients were included in this study and there were 349 (8.2%) CRC patients who were admitted to ICU. There were 34 (9.7%) CRC patients in unplanned ICU admission group and 315 (90.3%) CRC patients in planned ICU admission group. Older age (p < 0.01, OR = 1.093, 95% CI = 1.079–1.108), male (p = 0.013, OR = 0.721, 95% CI = 0.557–0.933), lower body mass index (BMI) (p = 0.001, OR = 0.932, 95% CI = 0.896–0.971), type 2 diabetes mellitus (T2DM) (p = 0.035, OR = 1.422, 95% CI = 1.024–1.975), coronary heart disease (CHD) (p = 0.036, OR = 1.579, 95% CI = 1.031–2.420), colon cancer (p = 0.002, OR = 1.475, 95% CI = 1.149–1.894), advanced tumor stage (p = 0.003, OR = 1.265, 95% CI = 1.082–1.478), longer operation time (p = 0.005, OR = 1.002, 95% CI = 1.001–1.003), and larger blood loss (p < 0.01, OR = 1.002, 95% CI = 1.001–1.002) were independent predictors of planned ICU admission. Older age (p < 0.01, OR = 1.062, 95% CI = 1.029–1.097) and longer operation time (p = 0.003, OR = 1.004, 95% CI = 1.001–1.007) were independent predictors of unplanned ICU admission.
Conclusion
Cautions should be paid for CRC patients with predictive factors to avoid unnecessary ICU admission.

Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Cheng YX, Tao W, Zhang H et al (2021) Does liver cirrhosis affect the surgical outcome of primary colorectal cancer surgery? A meta-analysis. World J Surg Oncol 19(1):167. https://doi.org/10.1186/s12957-021-02267-6
X Stachtea MB Loughrey M Salvucci et al 2021 Stratification of chemotherapy-treated stage III colorectal cancer patients using multiplexed imaging and single-cell analysis of T-cell populations Mod Patholhttps://doi.org/10.1038/s41379-021-00953-0
Segal NH, Cercek A, Ku G et al (2021) Phase II single-arm study of durvalumab and tremelimumab with concurrent radiotherapy in patients with mismatch repair-proficient metastatic colorectal cancer. Clin Cancer Res 27(8):2200–2208. https://doi.org/10.1158/1078-0432.CCR-20-2474
Kanani A, Veen T, Søreide K. 2021 Neoadjuvant immunotherapy in primary and metastatic colorectal cancer. Br J Surg. 2021 Oct 25: znab342. https://doi.org/10.1093/bjs/znab342.
Peng D, Liu XY, Cheng YX, Tao W et al (2021) Improvement of diabetes mellitus after colorectal cancer surgery: a retrospective study of predictive factors for type 2 diabetes mellitus remission and overall survival. Front Oncol 6(11):694997. https://doi.org/10.3389/fonc.2021.694997
Puxty K, McLoone P, Quasim T et al (2015) Risk of critical illness among patients with solid cancers: a population-based observational study. JAMA Oncol 1(8):1078–1085. https://doi.org/10.1001/jamaoncol.2015.2855
Soares M, Bozza FA, Azevedo LC et al (2016) Effects of organizational characteristics on outcomes and resource use in patients with cancer admitted to intensive care units. J Clin Oncol 34(27):3315–3324. https://doi.org/10.1200/JCO.2016.66.9549
Azoulay E, Schellongowski P, Darmon M et al (2017) The intensive care medicine research agenda on critically ill oncology and hematology patients. Intensive Care Med 43(9):1366–1382. https://doi.org/10.1007/s00134-017-4884-z
Zampieri FG, Romano TG, Salluh JIF et al (2021) Trends in clinical profiles, organ support use and outcomes of patients with cancer requiring unplanned ICU admission: a multicenter cohort study. Intensive Care Med 47(2):170–179. https://doi.org/10.1007/s00134-020-06184-2
Shimabukuro-Vornhagen A, Böll B, Kochanek M, Azoulay É et al (2016) Critical care of patients with cancer. CA Cancer J Clin 66(6):496–517. https://doi.org/10.3322/caac.21351
DR Rice JM Hyer D Tsilimigras et al 2021 Implications of intensive care unit admissions among medicare beneficiaries following resection of pancreatic cancer J SurgOncol https://doi.org/10.1002/jso.26710
Camus MF, Ameye L, Berghmans T et al (2015) Rate and patterns of ICU admission among colorectal cancer patients: a single-center experience. Support Care Cancer 23(6):1779–1785. https://doi.org/10.1007/s00520-014-2524-5
Weiser MR (2018) AJCC 8th edition: colorectal cancer. Ann Surg Oncol 25(6):1454–1455. https://doi.org/10.1245/s10434-018-6462-1
Cha JK, Oh TK, Song IA (2019) Impacts of financial coverage on long-term outcome of intensive care unit survivors in South Korea. Yonsei Med J 60(10):976–983. https://doi.org/10.3349/ymj.2019.60.10.976
Ponzoni CR, Corrêa TD, Filho RR, et al. 2017 Readmission to the intensive care unit: incidence, risk factors, resource use, and outcomes. A Retrospective Cohort Study. Ann Am Thorac Soc. 2017 Aug; 14(8): 1312–1319. https://doi.org/10.1513/AnnalsATS.201611-851OC.
Sculier JP (1995) Intensive care and oncology. Support Care Cancer 3(2):93–105. https://doi.org/10.1007/BF00365848
K Tsuboi J Ninagawa N Tsuboi et al 2021 Unplanned admission to pediatric intensive care after general anesthesia: a seven-year retrospective cohort study in a tertiary children’s hospital PaediatrAnaesth https://doi.org/10.1111/pan.14313
Kostakou E, Rovina N, Kyriakopoulou M et al (2014) Critically ill cancer patient in intensive care unit: issues that arise. J Crit Care 29(5):817–822. https://doi.org/10.1016/j.jcrc.2014.04.007
Thiéry G, Azoulay E, Darmon M et al (2005) Outcome of cancer patients considered for intensive care unit admission: a hospital-wide prospective study. J Clin Oncol 23(19):4406–4413. https://doi.org/10.1200/JCO.2005.01.487
Huang H, Han Z, Liang X, et al. 2021 Nomogram for predicting mandatory ICU admission after gastrectomy for gastric cancer. Ann Palliat Med. 2021 Jun; 10(6): 6208–6219. https://doi.org/10.21037/apm-21-178.
Tong C, Cao H, Xu Y et al (2021) Causes, risk factors and outcomes of patients readmitted to the intensive care unit after esophageal cancer surgery: a retrospective cohort study. World J Surg 45(7):2167–2175. https://doi.org/10.1007/s00268-021-06081-9
Salvini R, Frey B (2021) Iatrogenic events contributing to paediatric intensive care unit admission. Swiss Med Wkly 15(151):w20414. https://doi.org/10.4414/smw.2021.20414
Allen DZ, Worobetz N, Lukens J et al (2020) Outcomes intensive care unit placement following pediatric adenotonsillectomy. Int J Pediatr Otorhinolaryngol 129:109736. https://doi.org/10.1016/j.ijporl.2019.109736
Rubano JA, Vosswinkel JA, McCormack JE et al (2016) Unplanned intensive care unit admission following trauma. J Crit Care 33:174–179. https://doi.org/10.1016/j.jcrc.2016.02.012
Acknowledgements
We acknowledge all the authors whose publications are referred in our article.
Funding
This study was supported by Chongqing Key Diseases Research and Application Demonstration Program (Colorectal Cancer Prevention and Treatment Technology Research and Application Demonstration [No. 2019ZX003]).
Author information
Authors and Affiliations
Contributions
All the authors contributed to the data collection and analysis, drafting or revising the manuscript, have agreed on the journal to which the manuscript will be submitted, gave final approval of the version to be published, and agreed to be accountable for all the aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and informed consent
The study was approved by the ethics committee of our institution (The First Affiliated Hospital of Chongqing Medical University, 2021–517), and all the patients signed informed consent.
Consent for publication
All the figures and tables in this study were original; all were made by our authors.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiao-Yu Liu and Chao Yuan are co-first authors.
Rights and permissions
About this article
Cite this article
Liu, XY., Yuan, C., Kang, B. et al. Predictors associated with planned and unplanned admission to intensive care units after colorectal cancer surgery: a retrospective study. Support Care Cancer 30, 5099–5105 (2022). https://doi.org/10.1007/s00520-022-06939-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-06939-1