Abstract
Background and object
The risk of occult HBV infection (OBI) in children whose mothers are HBV carriers has received more widespread attention, but there were few reports to focus on the children with HBsAg-positive parents. In this study, we aimed to investigate the prevalence of OBI in immunized children with HBsAg-positive parents.
Methods
HBV-vaccinated Chinese hospitalized children with HBsAg-positive parents were analyzed in our investigation. Eligible subjects were tested using a standard nested PCR for all HBV genes, and analyzed by direct sequencing.
Results
There were 327 HBsAg-negative children included in the study out of about 9800 involved HBV-vaccinated hospitalized children. The positive rate of OBI was 3.1% (10/327) in the eligible children and 14.1% (46/327) with HBV DNA detectable. No significant differences were found between one and at least two regions positive groups (p > 0.05). The proportions of HBV DNA detectable in children with HBV father-carriers and mother-carriers were similar. The risk factors for HBV DNA-positive children could be male, anti-HBs levels, and anti-HBc positive.
Conclusion
There are 3.1% of OBIs and 14.1% of suspected OBI in vaccinated children with HBsAg-positive parents. The potential risk of suspected OBI in children with HBsAg-positive father should not be ignored. Anti-HBc positivity may be a useful seromarker for suspected OBI screening in vaccinated children. To prevent HBV breakthrough infection, accurate and convenient method is needed to detect OBI timely and exhaustively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic hepatitis B virus (HBV) infection is a major global health concern. Occult HBV infection (OBI) is regarded as the fifth phase of the natural history of chronic HBV infection [1], which is defined as the presence of HBV DNA in the liver (either with or without detectable HBV DNA in the serum) of people who test negative for hepatitis B surface antigen (HBsAg). On the basis of the HBV antibody profile, OBI distinguished as: seropositive-OBI, (hepatitis B core antigen antibodies [anti-HBc] and/or hepatitis B surface antigen antibodies [anti-HBs] positive) and seronegative-OBI (anti-HBc and anti-HBs negative) [2]. The amount of HBV DNA in serum is usually very low (< 200 IU/ml). Nowadays, the available assays for occult HBV testing is the analysis of DNA extracts from liver as well as blood, and samples amplify in two subsequent rounds of PCR (“nested” PCR) or by a “real-time PCR” technique.
Different clinical conditions have been involved in occult HBV infection: some studies suggest that OBI has the potential to reactivate and cause severe acute disease under immune suppression; transmission of the infection by blood transfusion or organ transplantation; and contribute to the development of cirrhosis, HCC [1, 3]. The majority of HBV infections in children are contracted either during perinatal period or early childhood, and individuals from HBV hyper-endemic areas may be more likely with occult HBV infections [4].
In China, hepatitis B routine immunization began in 1992 and is free for all newborn babies since 2002. The national serosurvey (carried out in 2006) showed that the prevalence of HBsAg fell from 9.8 to 7.2% for people aged 1–59 years between 1992 and 2006, and the infection in children under 5 years of age is only 1.0% [5]. Currently the first vaccine dose was administered within 24 h of birth and subsequent doses at 1 and 6 months, and newborns with HBsAg-positive mothers were recommended to receive hepatitis B immunoglobulin (HBIG) within 24 h.
In recent years, occult HBV infection was presented worldwide despite immunization against HBV, and varying proportions of infants born to HBsAg-positive mothers have been reported with OBI [6,7,8]. Data are scanty on the risk of OBI in children with HBV-positive father. In this study, we aimed at exploring the prevalence of OBI in hepatitis B-vaccinated children with HBV-positive mothers and/or fathers, trying to identify the risk factors of OBI.
Patients and methods
Study population
We had taken about 2.5 years to ask hospitalized children and their parents one by one, from April 2013 to November 2015. The inclusion criteria: (1) negative for HBsAg, (2) from HBsAg-positive parents (mother and/or father), (3) 3-dose hepatitis B vaccination immunized after birth, (4) other factors that may get infections such as blood transfusions, (5)with other pathogen infections, e.g., hepatitis C virus (HCV) and human immunodeficiency virus (HIV).
Hepatitis virus markers
Serological markers (HBsAg, anti-HBs, hepatitis B e antigen [HBeAg], hepatitis B e antibody [anti-HBe], and anti-HBc) were detected using commercial Chemiluminescence Microparticle Immuno Assay (CMIA) kits (Abbott GmbH & Co. KG, Wiesbaden, Germany). Subjects were considered HBsAg-positive at values > 0.05 IU/mL, anti-HBs-positive or seroprotected at values ≥ 10 mIU/ml, HBeAg-positive at values ≥ 1 S/CO (sample rate/cut off rate), anti-HBe-positive at values ≤ 1 S/CO, and anti-HBc-positive at values ≥ 1 S/CO.
DNA extraction and nested PCR
Viral DNA was extracted from 200 µl of serum using the QIAamp DNA Blood Mini Kit (QIAGEN Inc., Germany), according to the manufacturer’s instructions. All DNA samples were aliquoted and kept at − 20 °C prior to amplification and sequencing. Specific primers were designed to target the X and C regions of the HBV genome using Primer Premier 5. Primers targeting the S and Pre-S regions were designed by Shahmoradi et al. [9]. All primers (Supplement Table 1) were synthesized by Sangon Biotech Co., Ltd (Shanghai, China). The sensitivity of the PCR assay was determined by serial dilutions of serum samples containing known concentrations of the HBV genome: 1 × 107, 1 × 106, 1 × 105, 1 × 104, 1 × 103, 1 × 102, 1 × 101, IU/mL. The limit of detection for the nested PCR assay was approximately 10 IU/mL. The PCR mix was the same for all reactions and comprised 12.5 µl of 2 × Taq PCR Master Mix (Tiagen, Beijing, China), and the first and the second-round primers (10 pM). Five microliters of HBV DNA were used in the first round PCR, and 5 µl of the first round PCR product was used as the template for the second round. Amplification was performed for 35 cycles of denaturation at 94 ℃ for 30 s, annealing at 55 ℃ for 30 s, and elongation at 72 ℃ for 1 min, followed by a final extension at 72 ℃ for 5 min. Finally, 5 µl of PCR product was analyzed by electrophoresis in 1% agarose gel. Precautions were taken to avoid cross-contamination during sample collection, DNA extraction, PCR, and gel electrophoresis. To avoid the effect of cross-contamination on the results, negative and blank controls were included in each assay. Only reproducible data from assays with “clean” negative controls were analyzed. The positive test result was repeated three times.
DNA sequencing
PCR products were directly sequenced in an automated DNA Sequencer (ABI 3730) and the data were analyzed using Chromas 2.4.1 software (Technelysium Pty Ltd., South Brisbane, Australia).
Nucleotide sequence analysis
Sequences were analyzed by the BLAST tool of NCBI and Molecular Evolutionary Genetics Analysis (MEGA, Version 6.0). HBV sequences from OBI children were aligned and compared with GenBank reference sequences (genotypes A–H). Phylogenetic analysis was performed using the neighbor-joining method based on the nucleotide sequence of the amplified S, C, and Pre-S region. Bootstrap resampling and reconstruction were performed 1000 times to confirm the reliability of the phylogenetic analysis. Genetic distances were evaluated using Kimura 2-parameter corrections. The accession numbers for the reference sequences are as follows: AF090842, D00330, AB033556, X65259, X75657, X69798, AF160501, AY090454.
Ethical considerations
All experiments were performed in accordance with relevant guidelines and regulations. Two forms of informed consent were prepared, one was for parents when the child is less than 8 years, and another was to obtain both the children's and parents' informed information when the child is older than 8 years. The parents of the patients with OBI were informed when their children’s results were positive.
Statistical analysis
Statistical analyses were performed using the Statistical Package for Social Science (SPSS) for Windows, Version 20.0 (SPSS Inc., Chicago, USA). Anti-HBs values ≥ 1000 mIU/ml were calculated as 1000 mIU/ml. Non-normal variables were expressed as median (interquartile range, IQR) and analyzed using Mann–Whitney U test. Categorical variables were analyzed using the Chi-squared (χ2) test or Fisher’s exact test when the expected count in one cell was less than 5; Yates correction was applied when appropriate. Candidate variables with a p value < 0.25 on univariate analysis were included in multivariate logistic regression model. All statistical tests were two-tailed. A value of p < 0.05 was considered statistically significant.
Results
Basic characteristic of demographics
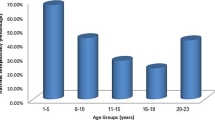
The sample selection and diagnostic workflow of tests in hepatitis B-vaccinated children were shown in Fig. 1. From April 2013 to November 2015, 9800 hospitalized children were given HBV seromarker test, and 400 HBV-vaccinated children whose mother, father, or both were HBsAg-positive met. There are 21 children with blood transfusion were excluded, and 49 children could not involve in the research due to the rejection of their parents. Finally, a total of 327 HBsAg-negative children were involved in the study. Within the 327 samples, there were 52.60% of children with HBsAg-positive mothers, 44.95% with HBsAg-positive fathers, and 2.45% with parents-carriers. All of these children received three doses of hepatitis B vaccine as planned and most (70.03%) received full prophylactic coverage (vaccine plus HBIG). HBV seromarkers were identified in the children, and positive rate was 74.62% (244/351) in anti-HBs (≥ 10 mIU/ml), 7.12% (25/351) in anti-HBc (s/co ≥ 1), and 0.85% (7/351) in anti-HBe (s/co ≤ 1), respectively.
The nested PCR results and sequence analysis
All 327 samples were analyzed to determine the existence of HBV DNA by nested PCR, and HBV DNA was detected in 46 [14.1%; 95% confidence interval (CI) 10.3–17.9%] children (Fig. 1, Table 1); using nested PCR, 20 (43.5%; 95% CI: 28.6–58.4%), 23 (50.0%; 95% CI 35.0–65.0%), and 16 (34.8%; 95% CI 20.5–49.1%) children were found positive for surface, core/pre-core, and pre-S regions (Supplement Fig. 1), none of sample amplified positive for HBV complete genome and X region. Overall, three (6.5%) samples were positive for three regions, seven (15.2%) samples were positive for two regions, 36 (78.3%) were positive for one region (Table 2).
The nested PCR amplification products of HBV S, and C, pre-S gene fragments in the 46 serum samples were successfully sequenced. All sequence information had been retrieved on National Center for Biotechnology Information (NCBI), and accession numbers were from MG738731 to MG738789. Different fragments of sequence information were used to construct the phylogenetic tree separately, and compared with standard sequences of HBV genotypes A-H (Supplement Fig. 2). There were 22 (47.8%) genotype B and 24 (52.2%) genotype C. Samples with sufficient blood were quantified for HBV-DNA using commercially real-time PCR-based detection kit, and mutation analysis at amino acid levels with the S, C, pre-S gene sequencing information was done. One ‘a’ determinant (amino acids 124–147) variant M133L was detected in isolate P77, which was associated with vaccine escape. P77 harbored an ‘a’ determinant variant and with a high level of HBV DNA (11,800 mIU/ml) was categorized as “false” OBI.
Comparison within one region and ≥ two regions positive samples
Demographic, epidemiological data, serological markers, and parent-carrier status identification within the 46 children were shown in Table 2, 87.0% (40/46) in anti-HBs positive, 13.0% (6/46) in anti-HBc positive, and no children were anti-HBc positive alone. Comparison was done between one region positive group (n = 10) and ≥ two regions positive group (n = 36) detected by nested PCR, and no significant differences were found including age, gender, HBIG usage, anti-HBs titer, positive rate of ALT, AST and anti-HBc, maternal and paternal factors in those children (Table 3. Potential risk factors for suspected OBI in immunized children with multivariable analysisOR* (95% CI)p valueAge (m) > 0.05 1–361.00 36–145–Gender < 0.05 Female1.00 Male4.24 (1.62–11.04)Anti-HBs (mIU/ml) < 0.05 < 101.00 ≥ 103.67 (1.45–9.315)Anti-HBc (s/co) < 0.05 < 11.00 ≥ 14.81(1.40–16.6)*Odds ratio3).
Analysis of HBV DNA detectable children with HBsAg-positive parents
Forty-six [14.10% (95% CI 10.3–17.9%)] HBsAg-negative children were detected HBV DNA positive by nested PCR, which were confirmed through sequencing analysis. There were 5 (5/9, 55.6%), 15 (15/35, 42.9%), and 20 (20/44, 45.5%) children with HBV carrier fathers detected ≥ two regions positive, one region positive, and ≥ one region positive by nested PCR, respectively (Fig. 2). The proportions of HBV DNA detectable in children with HBV father-carriers and mother-carriers were similar, and no statistical difference were found (p > 0.05). For HBV DNA detectable children, 20 (13.6%, 95% CI 8.0–19.2%), 24 (14.0%, 95% CI 8.7–19.2%) were found with HBV father-carriers, mother-carriers.
The risk factors associated with HBV DNA-positive children
Univariate statistical analysis was done between the HBV DNA detectable and undetectable children, and no statistically significant difference was found in the basic characteristics (gender, age, HBIG usage, serum anti-HBc, AST, ALT, maternal and paternal factors) (p > 0.05), except for anti-HBs titer. (Supplement Table 2).
To identify the risk factors that may affect HBV DNA-positive children, variables were explored with multivariate logistic regression model, and the dependent variable being the weighted in the HBV DNA detectable children. Independent variables included age, gender, anti-HBs, anti-HBc (variables for inclusion were carefully chosen, to ensure parsimony of the final model). Results showed that male [Odds Ratio (OR) 4.24], anti-HBs titer (OR 3.67), and anti-HBc-positive (OR 4.81) had higher risk with HBV DNA detectable than females (p < 0.05) (Table 4).
Discussion
Firstly, identified in the 1970s, more and more evidence has suggested that the clinical significance of OBI, which has become a major health issue attracting much attention. In recent years, variable proportions of OBI had been reported in immunized children with HBV-positive mothers. To our acknowledgement, this is the first study to explore the prevalence of OBI among hepatitis B vaccinated children with HBsAg-positive parents lived in HBV highly endemic areas.
In this study, results of nested PCR amplification show 14.10% (46/327; 95% CI 10.3–17.9%) of HBsAg-negative children with ≥ one gene fragment positive. Detection ≥ two regions of HBV genome by nested PCR is considered as the standard for HBV infection, only ten children (3.1%) would be considered as having OBI if definition is followed. Recently, the results of the quantitative RT-PCR for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) nucleic acid show that 87.5% of patients were finally defined as SARS-CoV-2 positive, in whom originally had only one positive target [10]. Thus, to examine the possibility of whether one HBV gene fragment detectable could indicate the existing occult HBV infection, we did the following analysis. First, there were 36 (11.0%; 95% CI 7.6–14.4%) and 10 (3.10%; 95% CI 1.2–4.9%) patients tested positive for one and ≥ two HBV gene fragments with strict quality control during the experiment, and no statistical differences were found between the two groups. Second, results of previous studies had found that one hepatitis B fragment positive also could indicate occult HBV infection: Jazayeri et al. detected HBV DNA in 28% (21/75) children by real-time PCR quantitatively, while some of the samples only amplified one segment [9]; for other researches amplified one HBV fragment with the samples, and the positive amplicons were confirmed from HBV genome by sequencing analysis [11, 12]. The sensitivity of nested-PCR assays may not be consistent, and thus there could be 14.1% of suspected OBIs in children with HBsAg-positive parents.
The risk of suspected OBI in children with HBsAg-positive parents should not be ignored. Considering the significant reservoir of HBV infections, the status of HBV infection in many countries is still not optimistic. Relatively high prevalence of OBI was found previously, range from 7.7 to 28% [6, 9, 13]. In China, HBV infection is still a severe public health burden with 97 million HBV carriers, and 14.1% of suspected OBI may exist in immunized children with HBsAg-positive parents. OBI may be involved in different clinical contexts, the development of cirrhosis and hepatocellular carcinoma [1]. Therefore, it could be important to have long term follow-up in children after uncovering OBI despite vaccination to prevent chronic complication in adulthood.
There is an equal potential risk of occult HBV infection in children with the HBsAg-positive father and mother. The positive rate of suspected OBI in father carriers was equal to mother carriers (13.6% vs. 14.0%), and 25% in both parents were HBV carriers. In China, it has been reported that 23.2% of HBsAg-positive families contained more than two HBV carriers [14]. The pattern of father-to-child transmission may not be ignored [15,16,17,18]. It is not uncommon that HBV integration was detected in PBMCs and cellular genes in HCC cases [19, 20]. HBV DNA integrates into the paternal DNA and causes the neonatal be infected through the sperm is possible.
Many independent factors had been analyzed between the suspected OBI positive and negative children in the study. Similar to HBV highly endemic areas, OBI in children living in HBV low prevalence regions are also more common than “overt” HBV infection, and the risk of OBI could be closely related to the parents' infection status [21, 22]. Results in previous study conducted in HBV low prevalence regions have shown that the risk factors for OBI could include whether to get hepatitis B vaccine, the genotype of HBV, while none of those found significant difference in this study [21]. The titer of anti-HBs was higher in the suspected OBI-positive than OBI-negative (p < 0.05). The escape mutations in HBV S gene needs to take attention [7, 9, 13, 23].
HBcAg is the most immunogenic HBV component during infection [24]. In recent years, some researches have suggested that anti-HBc was a very useful marker for OBI screening in HBsAg-negative subjects [25,26,27]. The risk of suspected OBI in anti-HBc-positive children may need to pay more attention, while it has to be stressed that not all anti-HBc positive individuals are found to be HBV DNA positive (anti-HBc negative also does not exclude OBI), and that anti-HBc tests may provide false-positive results.
There are some limitations exist in the study. First, this study is related to the hospital-based study design and children who are hospitalized may not represent children in the general population. Anyway, we had tried to avoid other factors that might get infections such as blood transfusions. Second, exploring the risk of OBI with one region positive and sequence analysis may be insufficient in this study, while it may be the more convenient and accurate method for suspected OBI detection. Three, in this study, although the transmission of HBV was mainly from parental carriers, the influence of other persons could not exclude, e.g., family members other than parents. Nevertheless, most Chinese children live with their parents and vertical transmission is the main way in Asian areas [28]. Thus, the children in this study with occult HBV infection were more likely from parent-to-child transmission.
In conclusion, a relatively high prevalence of suspected OBI may exist in hepatitis B-vaccinated Chinese children with HBsAg-positive parents, and the importance of monitoring OBI should be taken into account, especially for HBV hypo-endemic areas. Paternal factors should not be ignored with an equal potential risk of suspected OBI in children with HBsAg-positive father and (or) mother. Anti-HBc seropositivity may be a useful marker for suspected OBI screening in vaccinated children. Diagnosis of OBI with one HBV region amplifying positive using nested PCR may be reliable. To prevent HBV breakthrough infection, accurate and convenient method is needed to detect OBI timely and exhaustively.
References
Squadrito G, Spinella R, Raimondo G. The clinical significance of occult HBV infection. Ann Gastroenterol. 2014;27(1):15–19.
Raimondo G, Allain JP, Brunetto MR, et al. Statements from the Taormina expert meeting on occult hepatitis B virus infection. J Hepatol. 2008;49(4):652–657.
Shi Y, Wu Y, Wu W, et al. Association between occult hepatitis B infection and the risk of hepatocellular carcinoma: A meta-analysis. Liver Int. 2012;32:231–240.
Torbenson M, Thomas D. Occult hepatitis B. Lancet Infect Dis. 2002;2:479–486.
Liang X, Bi S, Yang W, et al. Epidemiological serosurvey of hepatitis B in China- declining HBV prevalence due to hepatitis B vaccination. Vaccine. 2009;27(47):6550–6557.
Lu Y, Liu YL, Nie JJ, et al. Occult HBV infection in immunized neonates born to HBsAg-positive mothers: a prospective and follow-up study. PLoS ONE. 2016;11(11):e0166317.
Su H, Zhang Y, Xu D, et al. Occult hepatitis B virus infection in Anti-HBs-positive infants born to HBsAg-positive mothers in China. PLoS ONE. 2013;8:8.
Foaud H, Maklad S, Mahmoud F, et al. Occult hepatitis B virus infection in children born to HBsAg-positive mothers after neonatal passive-active immunoprophylaxis. Infection. 2015;43(3):307–314.
Shahmoradi S, Yahyapour Y, Mahmoodi M, et al. High prevalence of occult hepatitis B virus infection in children born to HBsAg-positive mothers despite prophylaxis with hepatitis B vaccination and HBIG. J Hepatol. 2012;57(3):515–521.
Yang Y, Lu Q, Liu M, et al. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China. medRxiv. 2020. https://doi.org/10.1101/2020.02.10.20021675:2020.02.10.20021675.
Mandour M, Nemr N, Shehata A, et al. Occult HBV infection status among chronic hepatitis C and hemodialysis patients in Northeastern Egypt: regional and national overview. Rev Soc Bras Med Trop. 2015;48(3):258–264.
Gachara G, Magoro T, Mavhandu L, et al. Characterization of occult hepatitis B virus infection among HIV positive patients in Cameroon. AIDS Res Ther. 2017;14(1):11.
Mu SC, Lin YM, Jow GM, et al. Occult hepatitis B virus infection in hepatitis B vaccinated children in Taiwan. J Hepatol. 2009;50(2):264–272.
Wang FS, Fan JG, Zhang Z, et al. The global burden of liver disease: the major impact of China. Hepatology. 2014;60(6):2099–2108.
Franks AL, Berg CJ, Kane MA, et al. Hepatitis B virus infection among children born in the United States to Southeast Asian refugees. N Engl J Med. 1989;321(19):1301–1305.
Wang SS, Li WL, Peng GF, et al. The analysis of S gene phylogenetic tree of HBV in transmission from father to infant. Zhonghua Yi Xue Za Zhi. 2003;83(6):451–454.
Tajiri H, Tanaka Y, Kagimoto S, et al. Molecular evidence of father-to-child transmission of hepatitis B virus. J Med Virol. 2007;79(7):922–926.
Takegoshi K, Zhang W. Hepatitis B virus infections in families in which the mothers are negative but the fathers are positive for HBsAg. Hepatol Res. 2006;36(2):75–77.
Laskus T, Radkowski M, Wang LF, et al. Detection and sequence analysis of hepatitis B virus integration in peripheral blood mononuclear cells. J Virol. 1999;73(2):1235–1238.
Murakami Y, Saigo K, Takashima H, et al. Large scaled analysis of hepatitis B virus (HBV) DNA integration in HBV related hepatocellular carcinomas. Gut. 2005;54(8):1162–1168.
Escobedo-Melendez G, Panduro A, Fierro NA, et al. High prevalence of occult hepatitis B virus genotype H infection among children with clinical hepatitis in west Mexico. Mem Inst Oswaldo Cruz. 2014;109(6):728–737.
Escobedo-Melendez G, Panduro A, Celis A, et al. Risk factors associated with horizontal transmission of hepatitis B viral infection from parents to children in Mexico. J Infect Dev Ctries. 2019;13(1):44–49.
El Chaar M, Candotti D, Crowther RA, et al. Impact of hepatitis B virus surface protein mutations on the diagnosis of occult hepatitis B virus infection. Hepatology. 2010;52(5):1600–1610.
Milich DR, McLachlan A. The nucleocapsid of hepatitis B virus is both a T-cell-independent and a T-cell-dependent antigen. Science. 1986;234(4782):1398–1401.
Hsu H, Chang M, Ni Y, et al. Universal infant immunization and occult hepatitis B virus infection in children and adolescents: a population-based study. Hepatol Res. 2014;61(4):1183–1191.
Dickson R, Everhart J, Lake J, et al. Transmission of hepatitis B by transplantation of livers from donors positive for antibody to hepatitis B core antigen. Gastroenterology. 1997;113(5):1668–1674.
Seto W, Chan T, Hwang Y, et al. Hepatitis B reactivation in occult viral carriers undergoing hematopoietic stem cell transplantation: a prospective study. Hepatology. 2017;65(5):1451–1461.
Hadziyannis SJ. Natural history of chronic hepatitis B in Euro-Mediterranean and African countries. J Hepatol. 2011;55(1):183–191.
Acknowledgements
We wish to thank Yu Shi for sample collection and Junjie Tan for assisting with the quantification of HBV. We also thank Professor Xiaodong Zhao for helpful discussion.
Funding
This study was supported by the National Clinical Research Center for Child Health and Disorders General Project (No. NCRCCHD-2019-GP-04), Central Government Guides Local Science and Technology Development Projects-demonstration of Science and Technology Innovation projects, National Natural Science Foundation of China (No. 81371876), Outstanding Youth Foundation of Children's Hospital of Chongqing Medical University.
Author information
Authors and Affiliations
Contributions
Study concept and design: YZ, YC, AH. Sample collection: SZ, CG, YC, XY, ZZ, HX. Performing experiments: SZ, CG, YY. Statistical analysis: SZ, YY. Drafting the manuscript: SZ, YY, YZ. Critical revision of the manuscript: SZ, CG, YC, AH, YZ.
Corresponding author
Ethics declarations
Conflict of interest
Shurui Zhuge, Congcong Ge, Yuting Yang, Yuxia Cui, Xiaomei Yue, Zhenzhen Zhang, Hongmei Xu, Ailong Huang, Yao Zhao declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All included subjects gave informed consent for their participation in the study, and we checked HBV infection of the mothers and/or fathers again. The study was approved by the Ethics Committee of the Children’s Hospital of Chongqing Medical University.
Informed consent
Informed consent was obtained from all individual participants included in the study. All authors reviewed and approved the final version of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhuge, S., Ge, C., Yang, Y. et al. The prevalence of occult HBV infection in immunized children with HBsAg-positive parents: a hospital-based analysis. Hepatol Int 14, 503–512 (2020). https://doi.org/10.1007/s12072-020-10055-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-020-10055-9