Abstract
Object
Disease progression is an important factor affecting the long-term survival in hepatocellular carcinoma (HCC). The progression-free survival (PFS) has been used as a surrogate endpoint for overall survival (OS) in many solid tumors. However, there were few models to predict the PFS in HCC patients. This study aimed to explore the prognostic factors that affect the PFS in HCC and establish an individualized prediction model.
Methods
We included 2890 patients with hepatitis B-related HCC hospitalized at Beijing Ditan Hospital, Capital Medical University and randomly divided into training and validation cohort. Cox multivariate regression was used to analyze independent risk factors affecting the 1-year PFS of HCC, and an artificial neural networks (ANNs) model was constructed. C-index, calibration curve, and decision curve analysis were used to evaluate the performance of the model.
Results
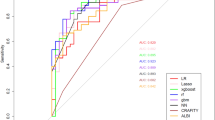
The median survival time was 26.2 m (95% CI: 24.08–28.32) and the 1-year PFS rate was 52.3% in whole study population. Cox multivariate regression showed smoking history, tumor number ≥ 2, tumor size ≥ 5 cm, portal vein tumor thrombus, WBC, NLR, γ-GGT, ALP, and AFP ≥ 400 ng/mL were risk factors for 1-year progression-free survival, while albumin and CD4 T cell counts were protective factors in HCC patients. A prediction model for 1-year PFS was constructed (https://lixuan.me/annmodel/myg-v3/). The ANNs model’s ability to predict 1-year PFS had an area under the receiver operating characteristic curve (AUROC) of 0.866 (95% CI 0.848–0.884) in HCC patients, which was higher than predicted by TNM, BCLC, Okuda, CLIP, CUPI, JIS, and ALBI scores (p < 0.0001). In addition, the ANNs model could also estimate the probability of 1-year OS and presented a higher AUROC value, 0.877 (95% CI 0.858–0.895), than those other models. All patients were divided into high-, medium-, and low-risk groups, according to the ANNs model scores. Compared with the hazard ratios (HRs) of PFS and OS in low-risk group, those in the high-risk group were 26.42 (95% CI 18.74–37.25; p < 0.0001) and 11.26 (95% CI 9.11–13.93; p < 0.0001), respectively.
Conclusion
The ANNs model has good individualized prediction performance and may be helpful to evaluate the probability of progression-free survival in HCC during clinical practice.



Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Foreman KJ, Marquez N, Dolgert A, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet. 2018;392(10159):2052–2090.
Sapisochin G, Bruix J. Liver transplantation for hepatocellular carcinoma: outcomes and novel surgical approaches. Nat Rev Gastroenterol Hepatol. 2017;14(4):203–217.
He LL, Liu XL, Zhang S, et al. Independent risk factors for disease recurrence after surgery in patients with hepatitis B virus-related hepatocellular carcinoma≤ 3 cm in diameter. Gastroenterol Rep. 2019;7(4):250–257.
Marasco G, Colecchia A, Colli A, et al. Role of liver and spleen stiffness in predicting the recurrence of hepatocellular carcinoma after resection. J Hepatol. 2019;70(3):440–448.
Shiina S, Tateishi R, Arano T, et al. Radiofrequency ablation for hepatocellular carcinoma: 10-year outcome and prognostic factors. Am J Gastroenterol. 2012;107(4):569–577.
Shim JH, Jun MJ, Han S, et al. Prognostic nomograms for prediction of recurrence and survival after curative liver resection for hepatocellular carcinoma. Ann Surg. 2015;261(5):939–946.
Mehta N, Heimbach J, Harnois DM, et al. Validation of a risk estimation of tumor recurrence after transplant (RETREAT) score for hepatocellular carcinoma recurrence after liver transplant. JAMA Oncol. 2017;3(4):493–500.
Han K, Ren M, Wick W, et al. Progression-free survival as a surrogate endpoint for overall survival in glioblastoma: a literature-based meta-analysis from 91 trials. Neuro-Oncology. 2013;16(5):696–706.
Llovet JM, Montal R, Villanueva A. Randomized trials and endpoints in advanced HCC: role of PFS as a surrogate of survival. J Hepatol. 2019;70(6):1262–1277.
Saad ED, Buyse M. Statistical controversies in clinical research: end points other than overall survival are vital for regulatory approval of anticancer agents. Ann Oncol. 2015;27(3):373–378.
Bishop CM. Neural networks for pattern recognition. Oxford: Oxford University Press; 1995.
Amato F, López A, Peña-Méndez EM, et al. Artificial neural networks in medical diagnosis. J Appl Biomed. 2013;11(2):47–58.
Liu X, Li M, Wang X, et al. PD-1+ TIGIT+ CD8+ T cells are associated with pathogenesis and progression of patients with hepatitis B virus-related hepatocellular carcinoma. Cancer Immunol Immunother. 2019;68(12):2041–2054.
Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30(01):052–060.
Minagawa M, Ikai I, Matsuyama Y, et al. Staging of hepatocellular carcinoma: assessment of the Japanese TNM and AJCC/UICC TNM systems in a cohort of 13,772 patients in Japan. Ann Surg. 2007;245(6):909.
Forner A, Reig ME, de Lope CR, et al. Current strategy for staging and treatment: the BCLC update and future prospects. Semin Liver Dis. 2010;30(01):061–074.
Okuda K, Obata H, Nakajima Y, et al. Prognosis of primary hepatocellular carcinoma. Hepatology. 1984;4(S1):3S–6S.
Cancer of the Liver Italian Program (CLIP) Investigators. A new prognostic system for hepatocellular carcinoma: a retrospective study of 435 patients. Hepatology. 1998;28(3):751–755.
Leung TWT, Tang AMY, Zee B, et al. Construction of the Chinese University Prognostic Index for hepatocellular carcinoma and comparison with the TNM staging system, the Okuda staging system, and the Cancer of the Liver Italian Program staging system: a study based on 926 patients. Cancer. 2002;94(6):1760–1769.
Kudo M, Chung H, Osaki Y. Prognostic staging system for hepatocellular carcinoma (CLIP score): its value and limitations, and a proposal for a new staging system, the Japan Integrated Staging Score (JIS score). J Gastroenterol. 2003;38(3):207–215.
Pinato DJ, Sharma R, Allara E, et al. The ALBI grade provides objective hepatic reserve estimation across each BCLC stage of hepatocellular carcinoma. J Hepatol. 2017;66(2):338–346.
Agatonovic-Kustrin S, Beresford R. Basic concepts of artificial neural network (ANN) modeling and its application in pharmaceutical research. J Pharm Biomed Anal. 2000;22(5):717–727.
Huitzil-Melendez FD, Capanu M, O'Reilly EM, et al. Advanced hepatocellular carcinoma: which staging systems best predict prognosis? J Clin Oncol. 2010;28(17):2889.
Chen ZH, Hong YF, Lin J, et al. Validation and ranking of seven staging systems of hepatocellular carcinoma. Oncology letters. 2017;14(1):705–714.
Liu PH, Hsu CY, Hsia CY, et al. Prognosis of hepatocellular carcinoma: assessment of eleven staging systems. J Hepatol. 2016;64(3):601–608.
Fridman WH, Pagès F, Sautès-Fridman C, et al. The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer. 2012;12(4):298.
Gabrielson A, Wu Y, Wang H, et al. Intratumoral CD3 and CD8 T-cell densities associated with relapse-free survival in HCC. Cancer Immunol Res. 2016;4(5):419–430.
Martens A, Wistuba-Hamprecht K, Yuan J, et al. Increases in absolute lymphocytes and circulating CD4+ and CD8+ T cells are associated with positive clinical outcome of melanoma patients treated with ipilimumab. Clin Cancer Res. 2016;22(19):4848–4858.
Phares TW, Stohlman SA, Hwang M, et al. CD4 T cells promote CD8 T cell immunity at the priming and effector site during viral encephalitis. J Virol. 2012;86(5):2416–2427.
Kim HJ, Cantor H. CD4 T-cell subsets and tumor immunity: the helpful and the not-so-helpful. Cancer Immunol Res. 2014;2(2):91–98.
Perez-Diez A, Joncker NT, Choi K, et al. CD4 cells can be more efficient at tumor rejection than CD8 cells. Blood. 2007;109(12):5346–5354.
Funding
This work was supported by the National Science Foundation of China (No. 81874435), Application of Clinical Features of Capital City of Science and Technology commission (No. Z171100001017082), Dengfeng Talent Support Program of Beijing Municipal Administration of Hospitals (No. DFL20191803).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors confirm that there are no known conflicts of interest associated with this study.
Ethical approval
The study was approved by the Ethics Committee of Beijing Ditan Hospital, Capital Medical University. Written informed consent was obtained from each patient. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, X., Hou, Y., Wang, X. et al. Machine learning-based development and validation of a scoring system for progression-free survival in liver cancer. Hepatol Int 14, 567–576 (2020). https://doi.org/10.1007/s12072-020-10046-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-020-10046-w