Abstract
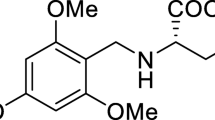
Microglia-induced neuroinflammation is a contributing factor to neurodegenerative diseases. Jatrorrhizine (JAT), an alkaloid isolated from Huanglian, has been shown to have neuroprotective effects against various neurodegenerative diseases, but its impact on microglia-induced neuroinflammation remains unclear. In this study, we investigated the role of JAT in MAPK/NF-κB/NLRP3 signaling pathway in an H2O2-induced oxidative stress model using microglia (N9 cells). We divided cells into six groups, including control, JAT, H2O2, H2O2 + 5 μmol/L JAT, H2O2 + 10 μmol/L JAT, and H2O2 + 20 μmol/L minocycline groups. Cell viability was measured using MTT assay and TNF-α levels were detected with an ELISA Kit. Western blot was used to detect NLRP3, HMGB1, NF-κB, p-NF-κB, ERK, p-ERK, p38, p-p38, p-JNK, JNK, IL-1β, and IL-18 expressions. Our results showed that JAT intervention improved H2O2-induced cytotoxicity in N9 cells and reduced the elevated expression of TNF-α, IL-1β, IL-18, p-ERK/ERK, p-p38/p38, p-JNK/JNK, p-p65/p65, NLRP3, and HMGB1 in H2O2 group. Furthermore, treatment with ERK inhibitor SCH772984 specifically blocked ERK phosphorylation, resulting in decreased protein levels of p-NF-κB, NLRP3, IL-1β, and IL-18 in H2O2 group. These results suggest that the MAPK/NF-κB signaling pathway may regulate the protein levels of NLRP3. Overall, our study indicates that JAT may have a protective effect on H2O2-treated microglia via inhibition the MAPK/NF-κB/NLRP3 pathway and could be a potential therapeutic approach for neurodegenerative diseases.








Similar content being viewed by others
Data Availability
The datasets supporting the conclusions of this article are included within the article.
References
Liddelow SA, Guttenplan KA, Clarke LE et al (2017) Neurotoxic reactive astrocytes are induced by activated microglia. Nature 541(7638):481–487
Hansen DV, Hanson JE, Sheng M (2018) Microglia in Alzheimer’s disease. J Cell Biol 217(2):459–472
Mecca C, Giambanco I, Donato R et al (2018) Microglia and Aging: The Role of the TREM2-DAP12 and CX3CL1-CX3CR1 Axes. Int J Mol Sci 19(1):318
Zhang WB, Yang F, Wang Y et al (2019) Inhibition of HDAC6 attenuates LPS-induced inflammation in macrophages by regulating oxidative stress and suppressing the TLR4-MAPK/NF-κB pathways. Biomed Pharmacother 117:109166–109166
Gee MS, Son SH, Jeon SH et al (2020) A selective p38α/β MAPK inhibitor alleviates neuropathology and cognitive impairment, and modulates microglia function in 5XFAD mouse. Alzheimers Res Ther 12(1):45
Sho T, Xu J (2019) Role and mechanism of ROS scavengers in alleviating NLRP3-mediated inflammation. Biotechnol Appl Biochem 66:4–13
Yang Q, Liu Q, Lv H et al (2020) Effect of pulegone on the NLPR3 inflammasome during inflammatory activation of THP-1 cells. Exp Ther Med 19(2):1304–1312
Lai M, Yao H, Shah SZA et al (2018) The NLRP3-caspase 1 inflammasome negatively regulates autophagy via TLR4-TRIF in prion peptide-infected microglia. Front Aging Neurosci 10:116
Sun S, Zhou S, Lei S et al (2019) Jatrorrhizine reduces 5-HT and NE uptake via inhibition of uptake-2 transporters and produces antidepressant-like action in mice. Xenobiotica 49(10):1237–1243
Yu H, Wang Y, Wang X et al (2019) Jatrorrhizine suppresses the antimicrobial resistance of methicillin-resistant Staphylococcus aureus. Exp Ther Med 18:3715–3722
Wang P, Gao XY, Yang SQ et al (2019) Jatrorrhizine inhibits colorectal carcinoma proliferation and metastasis through Wnt/beta-catenin signaling pathway and epithelial-mesenchymal transition. Drug Des Devel Ther 13:2235–2247
Luo T, Shen XY, Li S et al (2017) The protective effect of jatrorrhizine against oxidative stress in primary rat cortical neurons. CNS Neurol Disord Drug Targets 16:617–623
Wang S, Jiang W, Ouyang T et al (2019) Jatrorrhizine balances the gut microbiota and reverses learning and memory deficits in APP/PS1 transgenic mice. Sci Rep. 9(1):19575
Yuan Z, Chen X, Yang W et al (2019) The anti-inflammatory effect of minocycline on endotoxin-induced uveitis and retinal inflammation in rats. Mol Vis 25:359–372
Akhtar A, Sah SP (2020) Insulin signaling pathway and related molecules: Role in neurodegeneration and Alzheimer’s disease. Neurochem Int 135:104707
Matarin M, Salih DA, Yasvoina M et al (2015) A genome-wide gene-expression analysis and database in transgenic mice during development of amyloid or tau pathology. Cell Rep 10(4):633–644
Kaur D, Sharma V, Deshmukh R (2019) Activation of microglia and astrocytes: a roadway to neuroinflammation and Alzheimer’s disease. Inflammopharmacology 27(4):663–677
Sevenich L (2018) Brain-resident microglia and blood-borne macrophages orchestrate central nervous system inflammation in neurodegenerative disorders and brain cancer. Front Immunol 9:697
Choi YH (2019) Catalpol attenuates lipopolysaccharide-induced inflammatory responses in BV2 microglia through inhibiting the TLR4-mediated NF-kappaB pathway. Gen Physiol Biophys 38(2):111–122
Birla H, Minocha T, Kumar G et al (2020) Role of oxidative stress and metal toxicity in the progression of Alzheimer’s disease. Curr Neuropharmacol 18(7):552–562
Martinez Leo EE, Segura Campos MR (2019) Systemic oxidative stress: a key point in neurodegeneration -A review. J Nutr Health Aging 23(8):694–699
Qiu H, Sun S, Ma X et al (2018) Jatrorrhizine hydrochloride suppresses proliferation, migration, and secretion of synoviocytes in vitro and ameliorates rat models of rheumatoid arthritis in vivo. Int J Mol Sci 19(5):1514
Rolle J, Asante DO, Kok-Fong LL et al (2021) Jatrorrhizine: a review of its pharmacological effects. J Pharm Pharmacol 73(6):709–719
Duan W, Chen X (2021) Jatrorrhizine can improve nerve cell injury induced by Aβ 25–35, acting through miR-223-3p/HDAC4 axis. Am J transl Res 13(5):4644–4655
Liu B, Piao X, Niu W et al (2020) Kuijieyuan decoction improved intestinal barrier injury of ulcerative colitis by affecting TLR4-dependent PI3K/AKT/NF-κB oxidative and inflammatory signaling and gut microbiota. Front Pharmacol 11:1036
Niu S, Jing M, Wen J et al (2022) Jatrorrhizine alleviates DSS-induced ulcerative colitis by regulating the intestinal barrier function and inhibiting TLR4/MyD88/NF-κB signaling pathway. Evidence-based complementary and alternative medicine : eCAM. 3498310
Wu H, He K, Wang Y et al (2014) The antihypercholesterolemic effect of jatrorrhizine isolated from Rhizoma Coptidis. Phytomedicine : Int J Phytother Phytopharmacol 21(11):1373–1381
Li H, Wang J, Sun Q et al (2018) Jatrorrhizine hydrochloride suppresses RANKL-induced osteoclastogenesis and protects against wear particle-induced osteolysis. Int J Mol Sci 19(11):3698
Amani M, Shokouhi G, Salari A-A (2019) Minocycline prevents the development of depression-like behavior and hippocampal inflammation in a rat model of Alzheimer’s disease. Psychopharmacology 236(4):1281–1292
Li J, Chen J, Mo H et al (2016) Minocycline protects against NLRP3 inflammasome-induced inflammation and P53-Associated apoptosis in early brain injury after subarachnoid hemorrhage. Mol Neurobiol 53:2668–2678
Garcez ML, Mina F, Bellettini-Santos T et al (2017) Minocycline reduces inflammatory parameters in the brain structures and serum and reverses memory impairment caused by the administration of amyloid beta (1–42) in mice. Prog Neuropsychopharmacol Biol Psychiatry 77:23–31
Tang J, Chen Q, Guo J et al (2016) Minocycline attenuates neonatal germinal-matrix-hemorrhage-induced neuroinflammation and brain edema by activating cannabinoid receptor 2. Mol Neurobiol 53:1935–1948
Mehrabian Z, Guo Y, Weinreich D et al (2017) Oligodendrocyte death, neuroinflammation, and the effects of minocycline in a rodent model of nonarteritic anterior ischemic optic neuropathy (rNAION). Mol Vis 23:963–976
Song X, Xu A, Pan W et al (2008) Minocycline protects melanocytes against H2O2-induced cell death via JNK and p38 MAPK pathways. Int J Mol Med 22:9–16
O’Neil JD, Ammit AJ, Clark AR (2018) MAPK p38 regulates inflammatory gene expression via tristetraprolin: doing good by stealth. Int J Biochem Cell Biol 94:6–9
Mulero MC, Huxford T, Ghosh G (2019) NF-κB, IκB, and IKK: Integral components of immune system signaling. Adv Exp Med Biol 1172:207–226
Vermeulen L, De Wilde G, Van Damme P et al (2003) Transcriptional activation of the NF-kappaB p65 subunit by mitogen- and stress-activated protein kinase-1 (MSK1). EMBO J 22(6):1313–1324
He LX, Tong X, Zeng J et al (2016) Paeonol suppresses neuroinflammatory responses in LPS-activated microglia cells. Inflammation 39:1904–1917
Chen HB, Luo CD, Liang JL et al (2017) Anti-inflammatory activity of coptisine free base in mice through inhibition of NF-κB and MAPK signaling pathways. Eur J Pharmacol 811:222–231
Xia T, Liang X, Liu CS et al (2022) network pharmacology integrated with transcriptomics analysis reveals Ermiao Wan alleviates atopic dermatitis via suppressing MAPK and activating the EGFR/AKT signaling. Drug Des Dev Ther 16:4325–4341
Ran QS, Mu J, Li T et al (2022) Research of preparation quality markers of Yulian Tang with anti-inflammatory activity. Zhongguo Zhong Yao Za Zhi 47(11):2947–2954
Sharma K (2019) Cholinesterase inhibitors as Alzheimer’s therapeutics (Review). Mol Med Rep 20(2):1479–1487
Tripathi PN, Srivastava P, Sharma P et al (2019) Biphenyl-3-oxo-1,2,4-triazine linked piperazine derivatives as potential cholinesterase inhibitors with anti-oxidant property to improve the learning and memory. Bioorg Chem 85:82–96
Srivastava P, Tripathi PN, Sharma P et al (2019) Design and development of some phenyl benzoxazole derivatives as a potent acetylcholinesterase inhibitor with antioxidant property to enhance learning and memory. Eur J Med Chem 163:116–135
Hassan NA, Alshamari AK, Hassan AA et al (2022) Advances on therapeutic strategies for Alzheimer’s disease: from medicinal plant to nanotechnology. Molecules 27(15):4839
Tan JL, Xu YL, Fei YQ et al (2022) Simultaneous screening, identification, quantitation, and activity evaluation of six acetylcholinesterase (AChE) inhibitors in Coptidis Rhizoma by online UPLC-DAD coupled with AChE biochemical detection. J Pharm Biomed Anal 219:114897
An Y, Zhang H, Wang C et al (2019) Activation of ROS/MAPKs/NF-kappaB/NLRP3 and inhibition of efferocytosis in osteoclast-mediated diabetic osteoporosis. FASEB J 33(11):12515–12527
Liu Y, He H, Fan L et al (2020) Compound C attenuates NLRP3 inflammasome despite AMPK knockdown in LPS plus palmitate-induced THP-1 cells. Naunyn-Schmiedeberg’s Arch Pharmacol 393(1):67–76
Nakahira K, Haspel JA, Rathinam VA et al (2011) Autophagy proteins regulate innate immune responses by inhibiting the release of mitochondrial DNA mediated by the NALP3 inflammasome. Nat Immunol 12:222–230
Kim SW, Lee JK (2020) Role of HMGB1 in the Interplay between NETosis and Thrombosis in Ischemic Stroke: A Review. Cells 9(8):1794
Mangan MSJ, Olhava EJ, Roush WR et al (2018) Targeting the NLRP3 inflammasome in inflammatory diseases. Nat Rev Drug Discovery 17(9):688
Zhang H, Ding L, Shen T et al (2019) HMGB1 involved in stress-induced depression and its neuroinflammatory priming role: a systematic review. Gen Psychiat 32(4):e100084
Paudel YN, Angelopoulou E, Semple B et al (2020) Potential neuroprotective effect of the HMGB1 inhibitor glycyrrhizin in neurological disorders. ACS Che Neurosci 11(4):485–500
Su J, Pan YW, Wang SQ et al (2020) Saikosaponin-d attenuated lipopolysaccharide-induced depressive-like behaviors via inhibiting microglia activation and neuroinflammation. Int Immunopharmacol 80:106181
Bai H, Zhang Q (2021) Activation of NLRP3 inflammasome and onset of Alzheimer’s disease. Front Immunol 12:701282
Qiu WQ, Pan R, Tang Y et al (2020) Lychee seed polyphenol inhibits abeta- induced activation of NLRP3 inflammasome via the LRP1/AMPK Mediated autophagy induction. BioMed Pharmacother 130:110575
Wang CY, Xu Y, Wang X et al (2019) Dl-3-N-butylphthalide inhibits NLRP3 inflammasome and mitigates Alzheimer’s-like pathology via Nrf2-TXNIP -TrX axis. Antioxid Redox Signal 30(11):1411–1431
Kim N, Do J, Ju IG et al (2020) Picrorhiza Kurroa prevents memory deficits by inhibiting NLRP3 inflammasome activation and BACE1 expression in 5xfad mice. Neurotherapeutics 17(1):189–199
Cattaneo A, Cattane N, Galluzzi S et al (2017) Association of brain amyloidosis with pro-inflammatory gut bacterial taxa and peripheral inflammation markers in cognitively impaired elderly. Neurobiol Aging 49:60–68
Thawkar BS, Kaur G (2019) Inhibitors of NF-kappaB and P2X7/NLRP3/Caspase 1 pathway in microglia: novel therapeutic opportunities in neuroinflammation induced early-stage Alzheimer’s disease. J Neuroimmunol 326:62–74
Che H, Li Q, Zhang T et al (2018) Effects of astaxanthin and docosahexaenoic-acid-acylated astaxanthin on Alzheimer’s disease in APP/PS1 double-transgenic mice. J Agricultural Food Chem 66(19):4948–4957
Lan Z, Xie G, Wei M et al (2017) The protective effect of Epimedii Folium and Curculiginis Rhizoma on Alzheimer’s disease by the inhibitions of NF-kappaB/MAPK pathway and NLRP3 inflammasome. Oncotarget 8(27):43709–43720
Wei X, Zhang B, Wei F et al (2022) Gegen Qinlian pills alleviate carrageenan-induced thrombosis in mice model by regulating the HMGB1/NF-κB/NLRP3 signaling. Phytomedicine: Intl J Phytother Phytopharmacol 100:154083
Li R, Chen Y, Shi M et al (2016) Gegen Qinlian decoction alleviates experimental colitis via suppressing TLR4/NF-κB signaling and enhancing antioxidant effect. Phytomedicine: Intl J Phytother Phytopharmacol 23(10):1012–1020
Funding
This work was supported by Natural Science Foundation of Guangdong Province (No.2020A1515010580, 2021A1515011516, 2015A030313066), Science and Technology Planning Project of Guangzhou (No. 202102080239), National Natural Science Foundation of China (No. 81501093), Science and Technology Planning Project of Guangdong Province (No. 2014A020212622).
Author information
Authors and Affiliations
Contributions
Conceptualization: Sheng Wang, Tao Luo, and Hua-Qiao Wang; data curation: Sheng Wang and Cai-Li Xu; formal analysis: Sheng Wang, Cai-Li Xu; funding acquisition: Tao Luo and Hua-Qiao Wang; investigation: Sheng Wang; methodology: Sheng Wang; supervision: Tao Luo and Hua-Qiao Wang; writing–original draft: Sheng Wang; writing – review & editing: Tao Luo. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics Approval
Not applicable.
Consent for Publication
This article has not been published in part or in full elsewhere and has not been considered by other journals. All the authors read and approved the final manuscript. The authors gave consent for publication in Molecular Neurobiology.
Consent to Participate
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, S., Xu, CL., Luo, T. et al. Effects of Jatrorrhizine on inflammatory response induced by H2O2 in microglia by regulating the MAPK/NF-κB/NLRP3 signaling pathway. Mol Neurobiol 60, 5725–5737 (2023). https://doi.org/10.1007/s12035-023-03385-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-023-03385-w