Abstract
Examination of post-mortem brain tissues has previously revealed a strong association between Parkinson’s disease (PD) pathophysiology and endoplasmic reticulum (ER) stress. Evidence in the literature regarding the circulation of ER stress-regulated factors released from neurons provides a rationale for investigating ER stress biomarkers in the blood to aid diagnosis of PD. The levels of ER stress-regulated proteins in serum collected from 29 PD patients and 24 non-PD controls were measured using enzyme-linked immunosorbent assays. A panel of four biomarkers, protein disulfide-isomerase A1, protein disulfide-isomerase A3, mesencephalic astrocyte-derived neurotrophic factor, and clusterin, together with age and gender had higher ability (area under the curve 0.64, sensitivity 66%, specificity 57%) and net benefit to discriminate PD patients from the non-PD group compared with other analyzed models. Addition of oligomeric and total α-synuclein to the model did not improve the diagnostic power of the biomarker panel. We provide evidence that ER stress-regulated proteins merit further investigation for their potential as diagnostic biomarkers of PD.
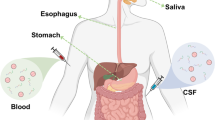
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disorder of the central nervous system. It is characterized by a progressive loss of dopaminergic neurons in the substantia nigra pars compacta and the accumulation of misfolded α-synuclein fibrils in glial and neuronal inclusions called Lewy bodies [1]. Making an accurate diagnosis of PD is difficult, time-consuming and is based on the clinical assessment of symptoms, medical history, physical and neurological examination, and responsiveness to the drug Levodopa. Imaging methods, such as magnetic resonance imaging (MRI), photon emission tomography (PET), and single-photon emission computed tomography (SPECT) are used to exclude conditions not associated with dopamine deficiency [1, 2]. Unfortunately, these methods are costly and some involve the exposure of patients to radiation. Thus, there is an urgent need for a non-invasive and rapid diagnostic test for PD [3]. Blood-based biomarker(s) monitoring pathological processes associated with the disease are economic, minimally invasive, and easily accessible methods that are readily used by clinicians for the diagnosis of various other diseases.
Neuropathological examination of post-mortem brain tissues from PD patients has revealed a strong association between PD pathophysiology and endoplasmic reticulum (ER) stress [4,5,6,7,8,9]. Studies using animal and cellular models of PD, including patient-derived induced pluripotent stem cells, indicate that ER dysfunction is an early event in PD pathogenesis contributing to neurodegeneration [6, 10, 11]. The ER plays a central role in the secretory pathway and it houses several resident chaperone proteins, which mediate the folding of transmembrane and secreted proteins [12]. These proteins contain Lys-Asp-Glu-Leu (KDEL)-like ER retention sequences and, while they are normally localized to the ER, they can be released from cells upon ER stress [13,14,15,16]. ER stress is induced by the accumulation of misfolded and unfolded proteins in the ER and it triggers the unfolded protein response (UPR). The UPR leads to the upregulation of ER-resident chaperone proteins, which restore proteostasis by facilitating proper folding and post-translational modifications of transmembrane and secretory proteins [17].
Systemic communication of stress signals between neurons and distal tissues has been recognized to affect non-cell autonomous control of homeostasis [18,19,20]. Indeed, stress proteins from neurons have been detected in the bloodstream [21, 22]. This offers an opportunity to uncover blood-based biomarkers of neurodegeneration that are related to ER stress. We hypothesized that ER stress-regulated chaperones that have been previously reported to (1) be upregulated in brain tissues of PD patients, (2) exhibit altered secretion from cells upon ER stress, and (3) have been detected in blood/cerebrospinal fluid (CSF) may have potential as blood-based biomarkers for PD. In this pilot study, we assessed levels of several ER stress-regulated chaperones in serum from PD patients and non-PD controls. We show that, while none of the analyzed proteins could independently discriminate between PD and non-PD groups, multiple logistic regression analysis and generation of a mathematical model comprising PDIA1, PDIA3, MANF, clusterin, and two confounding factors, age and gender, allowed for discrimination between the two diagnostic groups. These findings suggest that this panel of ER stress-regulated chaperones may have the potential as a diagnostic tool for PD, albeit with moderate sensitivity and specificity.
Results
Comparison of Serum Levels of Candidate Biomarker Proteins Between Non-PD and PD Groups
Based on our review of the literature to find proteins which met the selection criteria, chaperones PDIA1, PDIA3, MANF, GRP78, calreticulin, and clusterin were selected for validation as potential PD serum-based biomarkers. All of these proteins have been reported to be upregulated in PD [7, 9, 11, 23,24,25,26,27,28]. With the exception of clusterin, they are all KDEL-containing proteins that are residents in the ER [29, 30]. Clusterin is normally secreted through the ER-Golgi secretory pathway, but under conditions of ER stress it is redirected to the cytosol where it may be involved in the trafficking of misfolded proteins for degradation by the proteasome and/or autophagy [31, 32]. All of these proteins have been found in blood/CSF, which demonstrates their potential to be detected in serum [33,34,35,36].
We performed enzyme-linked immunosorbent assay (ELISA) analysis to determine the concentrations of these proteins in serum taken from PD patients and non-PD controls. This revealed higher levels of PDIA1 (p = 0.096) (Fig. 1a), MANF (p = 0.17) (Fig. 1b), and clusterin (p = 0.31) (Fig. 1c), and reduced levels of PDIA3 (p = 0.27) (Fig. 1d) in PD patients, while GRP78 (p = 0.63) (Fig. 1e) and calreticulin (p = 0.56) (Fig. 1f) levels were similar in both groups. We noted that one of the PD values for clusterin (333.71 µg/ml) deviated very far from the mean value, and that if this sample was omitted from the calculation the mean changed from 54.69 to 42.56 µg/ml, which was similar to the mean for non-PD group (Table 1). We also examined levels of the oligomeric form of α-synuclein and total α-synuclein, since both have been previously flagged as promising biomarkers of PD. Levels of oligomeric α-synuclein were higher in serum from PD patients (p = 0.40) (Fig. 1g), while total α-synuclein levels were not different between diagnostic groups (p = 0.51) (Fig. 1h). However, the levels of examined proteins considerably overlapped between diagnostic groups, and the observed differences in mean protein levels between diagnostic groups did not reach the statistical significance, indicating that none of the tested proteins were able to distinguish between PD and non-PD groups as single biomarkers (Table 1).
Serum concentrations of a PDIA1, b MANF, c clusterin, d PDIA3, e GRP78, f calreticulin, g oligomeric α-synuclein, and h total α-synuclein plotted as individual values in indicated diagnostic groups. The line through the middle of the boxes in box-and-whiskers plots corresponds to the median and the lower and the upper lines to the 25th and 75th percentiles, respectively. The whiskers extend from the minimum value at the bottom to the maximum value at the top
A Panel of Biomarkers Discriminates PD Patients from Control Group
Levels of single biomarkers often show considerable overlap between diagnostic groups [37, 38]. In such circumstances, a combination of multiple biomarkers is a better strategy for obtaining a more accurate diagnosis [39, 40]. We performed multiple logistic regression analysis and identified a panel of four proteins PDIA1, PDIA3, MANF, and clusterin, which together with two confounders age and gender, provided the greatest discrimination of PD patients from the non-PD control group, with an accuracy measured by an area under the curve (AUC) of 0.64, calculated from the receiver operating characteristic (ROC) curve (sensitivity 66%, specificity 57%) (Fig. 2a). Decision curve analysis of this model including significant variables and the two confounders consistently demonstrated higher net benefit value in disease detection compared to “diagnose all,” “diagnose none,” and “diagnose based on age and gender” models (Fig. 2b).
Conversion of monomeric α-synuclein into oligomers and fibrils is a major neuropathological hallmark of PD and oligomeric α-synuclein has gained attention as a promising diagnostic biomarker [40,41,42]. We measured levels of oligomeric and total α-synuclein in serum (Table 1) and performed logistic regression analysis to test if α-synuclein can contribute to the performance of our biomarker panel. A combined assessment revealed that neither total α-synuclein (Fig. 3a, b), oligomeric α-synuclein (Fig. 3c, d) nor both combined together with the biomarker panel (Fig. 3e, f) improved the diagnostic discriminatory power and benefit of this biomarker panel.
Discussion
This exploratory study is the first to report on the performance of a panel of ER stress-regulated chaperone proteins, analyzed in serum, in discriminating between PD patients and non-PD controls. We tested ER stress-related proteins that met our criteria of being increased in PD, displaying altered secretion upon ER stress and reported to be found in blood/CSF. We were able to detect each of the six proteins in serum from PD patients and non-PD controls, although none of the proteins tested were able to distinguish between PD and non-PD groups when used individually. However, multiple logistic regression analysis identified a panel containing PDIA1, PDIA3, MANF, and clusterin that could discriminate between PD and non-PD groups, with PDIA1 and MANF contributing most to the discriminatory power. This study underscores the value of combining multiple biomarkers and the potential of ER stress-regulated proteins as serum-based biomarkers for PD.
A recent systematic review provided evidence that biomarker panels increase diagnostic accuracy and outperform single biomarkers in the detection of Alzheimer’s disease [39]. Similar findings were described in a review focused on biomarkers for PD [2]. For example, a combination of oligomeric/total α-synuclein, phosphorylated α-synuclein, and phosphorylated tau in CSF discriminates PD from healthy controls significantly better than each biomarker individually [40]. Similarly, CSF neurofilament contributes to a panel of CSF α‐synuclein species in distinguishing PD from non-PD groups, even though neurofilament levels largely overlapped between the two groups [37]. In agreement with these studies, we found that a panel of ER stress-regulated biomarkers could discriminate PD and non-PD groups, while each protein individually could not.
Our findings show for the first time that ER stress-regulated proteins are worthy of investigation as serum biomarkers for PD. Indeed, higher levels of MANF and clusterin have already been reported in serum samples of PD patients [35, 43]. Increased concentrations of clusterin in CSF were reported to be predictive of PD [27]. Clusterin is an extracellular chaperone secreted through the ER-Golgi secretory pathway but its localization can be altered upon ER stress, with clusterin trafficking to the cytosol [31]. ERdj3 is another ER-resident protein whose secretion is elevated upon ER stress [44]. Unfortunately, we were unable to include ERdj3 in our analysis due to a lack of suitable ELISA. However, it would be very interesting to include this in the model.
Proteins, such as MANF, PDIA1, PDIA3, GRP78, and calreticulin are normally ER resident chaperones due to the presence of ER-localizing C-terminal KDEL-like sequence [30]. KDEL proteins are recognized by KDEL receptors in the Golgi and recycled back to the ER [45]. Upon ER stress, the increased expression of KDEL-containing ER resident proteins can overwhelm the KDEL-dependent retrieval system which results in their secretion from cells [30]. Moreover, imperfect KDEL sequences, such as the C-terminal RTDL sequence in MANF, can lead to poorer ER retention and easier diversion of the protein. KDEL-like sequences have been found in more than 70 human proteins [29, 30]. Given that biomarker panels exhibit improved performance over single biomarkers, it is worth considering whether other KDEL proteins could contribute to the enhanced performance of the panel.
The diagnostic accuracy of the ER stress-regulated biomarker panel was moderate at best, with an AUC of 0.64. This indicates a need for further panel evaluation to better understand the dynamics and confounders that affect its performance. For example, age-related changes in chaperone expression might occur due to a decline in proteostasis in neurons [46]. Biological sex is also an important factor contributing to the clinical features of PD [47]. Indeed, we observed that age and gender contributed to the performance of the biomarker panel and therefore, they were included in the analysis. By incorporating sex into the model, the unbalanced male/female ratio in the samples collected was also taken into account. It is possible that other factors, for example, disease duration and severity, may influence chaperone levels in the serum of PD patients. For example, it has been reported that MANF levels in serum are higher in PD patients classified as depressed based on Beck Depression Inventory scoring [35]. A better understanding of confounding factors could help to explain why some patients had significantly higher values for specific biomarkers, like clusterin, than the group mean values. This needs to be investigated further in a larger cohort study.
Furthermore, combining biomarkers reflecting the multiple neuropathological processes that are associated with PD may improve the diagnostic accuracy of the biomarker panel. Apart from ER stress, inflammation, lysosomal dysfunction, metabolic impairment, aberrant autophagy, amyloid pathology, tauopathy, and synucleinopathy have also been implicated in PD [2]. Interestingly, ER stress impacts most of those processes [48, 49]. For example, ER stress has been reported to induce α-synuclein oligomerization [50, 51]. Previously, it has been suggested that oligomeric α-synuclein in serum might be a potential biomarker for the diagnosis of PD [41, 52]. The reports on total α-synuclein levels in the blood of PD patients and non-PD controls are conflicting [53,54,55]. We did not observe significant differences in levels of total and oligomeric forms of α-synuclein between diagnostic groups. The inclusion of total and oligomeric α-synuclein in our model did not improve the performance of the biomarker panel in discriminating between PD and non-PD groups.
In conclusion, the data presented here show for the first time a panel of PDIA1, PDIA2, MANF, and clusterin that could be useful in the diagnosis of PD. This pilot study provides a rationale for further validation of ER stress-regulated chaperone proteins in a larger cohort study as well as longitudinal studies to assess the dynamics of changes as a function of PD stage and duration. It will be important to evaluate the model in cohorts of patients representing a spectrum of neurodegenerative diseases and ER stress-related disorders. The results also underscore the potential added benefit of including other biomarkers in the panel in order to improve its diagnostic performance.
Methods
Participant Recruitment and Assessment
This cross-sectional pilot study was approved by the University Hospital Galway Research Ethics Committee and written informed consent was obtained from the subjects. Blood samples were collected from 29 idiopathic PD patients and 24 non-PD controls. Patients diagnosed with PD before the onset of the study were recruited from a tertiary referral movement disorders clinic and all patients were diagnosed with idiopathic Parkinson’s disease by a movement disorder specialist in accordance with current Movement Disorder Society (MDS) clinical diagnostic criteria [56]. Hoehn & Yahr (H&Y) staging and Mini-Mental State Examination (MMSE) score assessments were completed for the enrolled patient on the day of blood collection. Patients were eligible for inclusion if they were diagnosed with idiopathic PD by a movement disorders specialist, with no signs of dementia (MMSE score ≥ 24), and moderate disease severity (H&Y stages 2 and 3). Clinical data, such as disease duration and medication, were obtained. Unrelated non-PD subjects or spouses of patients were enrolled from the local community. Volunteers with neurological disorders on cytotoxic drugs or a family history of neurodegenerative diseases were excluded. The demographic and clinical characteristics of the enrolled subjects listed in Table 2 show the distribution of age and sex between the diagnostic groups.
Collection and Processing of Human Serum Samples
Venous blood was collected by a trained phlebotomist into BD Vacutainer serum tubes (Becton, Dickinson, NJ, USA; #367,895) containing silica for clot activation. Samples were left to coagulate in a dark at room temperature for 1 h. Tubes were centrifuged at 1300 × g for 10 min. Serum was collected, aliquoted into polypropylene 0.5 ml tubes, and stored at − 80 °C within 50 min from centrifugation. Serum samples were validated for hemolysis.
The Biomarker Selection Process
PubMed was used to search English language publications. The initial database search used the following search terms: (endoplasmic reticulum stress OR the unfolded protein response) AND (protein secretion OR secretory proteins). The literature search identified two sets of proteins whose secretion is under the control of ER stress: (1) proteins that are normally resident in the ER, due to the presence of a C-terminus KDEL-like retention sequence but have been demonstrated to be released from cells upon ER stress; and (2) secretory proteins that are folded in the ER and whose secretion is altered upon ER stress. We searched through the list of proteins to identify chaperones. From the list of proteins with KDEL-like motif [29, 30], we selected chaperones PDIA1, PDIA3, GRP78, calreticulin, MANF, and CDNF, because they were previously reported to (1) be upregulated in brain tissues of PD patients [7, 9, 11, 23,24,25,26,27,28], (2) exhibit altered secretion from cells upon ER stress [13, 57,58,59], and (3) have been detected in blood/CSF [33,34,35,36, 60, 61]. From the list of secreted chaperones, only the localization of clusterin and ERdj3 have been reported to be altered upon ER stress [32, 44]. We tested clusterin, for which higher levels have been reported in serum and CSF samples of PD patients [27, 43]. We did not analyze CDNF or ERdj3 due to the lack of a suitable ELISA that would enable us to measure protein levels in serum without a matrix effect.
Enzyme‐Linked Immunosorbent Assay (ELISA)
Protein concentrations in serum were measured by enzyme‐linked immunosorbent assays: PDIA1 (Abbexa, Cambridge, UK; abx152685), MANF (Abcam, Cambridge, UK; ab215417), PDIA3 (Abbexa; abx252930), GRP78 (Enzo, NY, USA; ADI-900–214), Calreticulin (Abbexa; abx250954), Clusterin (BioVendor, Heidelberg, Germany; RD194034200R), α-synuclein (Invitrogen, CA, USA; KHB0061), and oligomeric α-synuclein (Analytic-Jena, Jena, Germany; BM-847–0,104,000,108) according to the manufacturer’s protocols. Protein standard dilutions and blank (1 × dilution buffer) were prepared and 100 μl of each were added in duplicate to a pre-coated plate. The serum samples were either undiluted (for detection of PDIA1, PDIA3, calreticulin, oligomeric α-synuclein) or diluted in a sample diluent buffer (1:25 for GRP78, 1:8 for MANF, 1:2 for α-synuclein, 1:3,000 for clusterin) and 100 μl were added in duplicate into wells. For the GRP78 ELISA, 50 μl of antibody were added into each well, except the blank wells. The plates were incubated at room temperature for 1 h with shaking. The wells were washed 5 times with 300 μl 1 × wash solution except for the GRP78 ELISA. After the final wash, any remaining solution was removed. A secondary antibody solution was added into each well (100 μl for detection of MANF, clusterin, calreticulin, PDIA1, and PDIA3 or 50 μl for detection of GRP78). The plates were incubated for 1 h at room temperature on a shaker. The wells were washed 5 times. Substrate solution (100 μl or 200 μl for GRP78 detection) was added and plates were incubated for up to 30 min at room temperature with shaking. The plates were sealed at every incubation step. The stop solution (100 μl or 50 μl for GRP78 detection) was pipetted into each well. The absorbance at 450 nm was measured using a VICTOR3™ Multilabel Plate Reader (Perkin Elmer, MA, USA). For the calculation of protein concentration, the mean absorbance of the blank was subtracted from all readings. The protein concentrations were interpolated from the standard curve and multiplied by the respective dilution factor. The standard curve was generated by plotting the mean absorbance of the standards against the known concentration of the standards in a logarithmic scale, using the four-parameter algorithm.
Statistical Analysis
Quantitative variables were compared using an unpaired two-tailed t-test with Welch’s correction. P-values were considered significant if p < 0.05. Patient information including serum levels of ER stress-regulated chaperones were used to build a statistical model to predict PD. Biomarker concentrations were adjusted between plates for the biomarkers that showed a significant difference between the plate means.
For oligomerized α-synuclein, 31% of the values were below the detection limit of the analytical procedure. These values called censored were different from missing values as they lie between zero and the detection limit. Cohen’s method was used for the imputation of data below the detection limit considering the sample size and the percentage of censoring [62]. The data were imputed using the inverse cumulative normal distribution with the adjusted sample mean and standard deviation using the maximum likelihood estimation.
The stepwise variable selection technique was used to identify a combination of biomarkers which could distinguish Parkinson’s disease patients from the control group [63]. The effects of selected biomarkers were modelled using logistic regression [64]. Ten-fold cross validation was used for internal validation of the models to confirm that no patient was used to both develop and test the model [65]. Ten-fold cross validation involves randomly dividing the data into ten evenly sized subgroups (fold). The data from the first nine folds were used for modelling and applied to the tenth fold as the validation set. The model building and validation process was repeated ten times with each fold of patients used once as the validation set. The accuracy of the models was determined using the area under the curve (AUC) calculated from the receiver operator characteristic (ROC) by plotting the sensitivity and specificity at each of its risk thresholds [66]. The closer the AUC value to 1, the better the panel of biomarkers can distinguish PD patients from the control group. Decision-curve analysis was also undertaken to examine the potential net benefit of the application of each model where a higher net benefit value shows improvement in disease detection [67].
Data Availability
Anonymized data that support the findings of this study are available on request from the corresponding author for purposes of replicating procedures and results. The data are not publicly available due to containing information that could compromise research participant consent.
References
Bloem BR, Okun MS, Klein C (2021) Parkinson’s disease. Lancet 397:2284–2303. https://doi.org/10.1016/S0140-6736(21)00218-X
Parnetti L, Gaetani L, Eusebi P et al (2019) CSF and blood biomarkers for Parkinson’s disease. Lancet Neurol 18:573–586. https://doi.org/10.1016/S1474-4422(19)300
Tönges L, Buhmann C, Klebe S et al (2022) Blood-based biomarker in Parkinson’s disease: potential for future applications in clinical research and practice. J Neural Transm 129:1201–1217. https://doi.org/10.1007/S00702-022-02498-1
Hoozemans JJM, van Haastert ES, Eikelenboom P et al (2007) Activation of the unfolded protein response in Parkinson’s disease. Biochem Biophys Res Commun 354:707–711. https://doi.org/10.1016/J.BBRC.2007.01.043
Selvaraj S, Sun Y, Watt JA et al (2012) Neurotoxin-induced ER stress in mouse dopaminergic neurons involves downregulation of TRPC1 and inhibition of AKT/mTOR signaling. J Clin Invest 122:1354–1367. https://doi.org/10.1172/JCI61332
Heman-Ackah SM, Manzano R, Hoozemans JJM et al (2017) Alpha-synuclein induces the unfolded protein response in Parkinson’s disease SNCA triplication iPSC-derived neurons. Hum Mol Genet 26:4441–4450. https://doi.org/10.1093/hmg/ddx331
Conn KJ, Gao W, McKee A et al (2004) Identification of the protein disulfide isomerase family member PDIp in experimental Parkinson’s disease and Lewy body pathology. Brain Res 1022:164–172. https://doi.org/10.1016/j.brainres.2004.07.026
Esteves AR, Cardoso SM (2020) Differential protein expression in diverse brain areas of Parkinson’s and Alzheimer’s disease patients. Sci Rep 10:13149. https://doi.org/10.1038/S41598-020-70174-Z
Baek JH, Mamula D, Tingstam B et al (2019) GRP78 Level is altered in the brain, but not in plasma or cerebrospinal fluid in Parkinson’s disease patients. Front Neurosci 13:697. https://doi.org/10.3389/fnins.2019.00697
Mercado G, Castillo V, Soto P et al (2018) Targeting PERK signaling with the small molecule GSK2606414 prevents neurodegeneration in a model of Parkinson’s disease. Neurobiol Dis 112:136–148. https://doi.org/10.1016/j.nbd.2018.01.004
Colla E, Coune P, Liu Y et al (2012) Endoplasmic reticulum stress is important for the manifestations of α-synucleinopathy in vivo. J Neurosci 32:3306–3320. https://doi.org/10.1523/jneurosci.5367-11.2012
Plate L, Wiseman RL (2017) Regulating secretory proteostasis through the unfolded protein response: from function to therapy. Trends Cell Biol 27:722–737. https://doi.org/10.1016/j.tcb.2017.05.006
Gold LI, Eggleton P, Sweetwyne MT et al (2010) Calreticulin: non-endoplasmic reticulum functions in physiology and disease. FASEB J 24:665–683. https://doi.org/10.1096/fj.09-145482
Turano C, Coppari S, Altieri F, Ferraro A (2002) Proteins of the PDI family: unpredicted non-ER locations and functions. J Cell Physiol 193:154–163. https://doi.org/10.1002/jcp.10172
Ni M, Zhang Y, Lee AS (2011) Beyond the endoplasmic reticulum: atypical GRP78 in cell viability, signalling and therapeutic targeting. Biochem J 434:181–188. https://doi.org/10.1042/BJ20101569
Voutilainen MH, Arumäe U, Airavaara M, Saarma M (2015) Therapeutic potential of the endoplasmic reticulum located and secreted CDNF/MANF family of neurotrophic factors in Parkinson’s disease. FEBS Lett 589:3739–3748. https://doi.org/10.1016/j.febslet.2015.09.03
da Costa CA, El MW, Duplan E, Checler F (2020) The endoplasmic reticulum stress/unfolded protein response and their contributions to Parkinson’s disease physiopathology. Cells 9:2495. https://doi.org/10.3390/cells9112495
Taylor RC, Dillin A (2013) XBP-1 is a cell-nonautonomous regulator of stress resistance and longevity. Cell 153:1435–1447. https://doi.org/10.1016/j.cell.2013.05.042
Sprenkle NT, Lahiri A, Simpkins JW, Meares GP (2019) Endoplasmic reticulum stress is transmissible in vitro between cells of the central nervous system. J Neurochem 148:516–530. https://doi.org/10.1111/JNC.14642
Williams KW, Liu T, Kong X et al (2014) Xbp1s in Pomc neurons connects ER stress with energy balance and glucose homeostasis. Cell Metab 20:471–482. https://doi.org/10.1016/J.CMET.2014.06.002
Sui Y-T, Bullock KM, Erickson MA et al (2014) Alpha synuclein is transported into and out of the brain by the blood–brain barrier. Peptides 62:197–202. https://doi.org/10.1016/J.PEPTIDES.2014.09.018
Kluge A, Bunk J, Schaeffer E et al (2022) Detection of neuron-derived pathological α-synuclein in blood. Brain 145:3058–3071. https://doi.org/10.1093/BRAIN/AWAC115
Lee YM, Park SH, Chung KC, Oh YJ (2003) Proteomic analysis reveals upregulation of calreticulin in murine dopaminergic neuronal cells after treatment with 6-hydroxydopamine. Neurosci Lett 352:17–20. https://doi.org/10.1016/j.neulet.2003.08.018
Andreu CI, Woehlbier U, Torres M, Hetz C (2012) Protein disulfide isomerases in neurodegeneration: from disease mechanisms to biomedical applications. FEBS Letters 586(18):2826–34. https://doi.org/10.1016/j.febslet.2012.07.02
Kim-Han JS, O’Malley KL (2007) Cell stress induced by the parkinsonian mimetic, 6-hydroxydopamine, is concurrent with oxidation of the chaperone, ERp57, and aggresome formation. Antioxid Redox Signal 9:2255–2264. https://doi.org/10.1089/ARS.2007.1791
Holtz WA, O’Malley KL (2003) Parkinsonian mimetics induce aspects of unfolded protein response in death of dopaminergic neurons. J Biol Chem 278:19367–19377. https://doi.org/10.1074/jbc.M211821200
Přikrylová Vranová H, Mareš J, Nevrlý M et al (2010) CSF markers of neurodegeneration in Parkinson’s disease. J Neural Transm 117:1177–1181. https://doi.org/10.1007/S00702-010-0462-Z
Fernandes HJR, Patikas N, Foskolou S et al (2020) Single-cell transcriptomics of Parkinson’s disease human in vitro models reveals dopamine neuron-specific stress responses. Cell Rep 33:108263. https://doi.org/10.1016/j.celrep.2020.108263
Raykhel I, Alanen H, Salo K et al (2007) A molecular specificity code for the three mammalian KDEL receptors. J Cell Biol 179:1193–1204. https://doi.org/10.1083/jcb.200705180
Trychta KA, Bäck S, Henderson MJ et al (2018) KDEL receptors are differentially regulated to maintain the ER proteome under calcium deficiency. Cell Rep 25:1829-1840.e6. https://doi.org/10.1016/j.celrep.2018.10.055
Nizard P, Tetley S, Le Dréan Y et al (2007) Stress-induced retrotranslocation of clusterin/ApoJ into the cytosol. Traffic 8:554–565. https://doi.org/10.1111/j.1600-0854.2007.00549.x
Satapathy S, Wilson MR (2021) The dual roles of clusterin in extracellular and intracellular proteostasis. Trends Biochem Sci 46:652–660. https://doi.org/10.1016/J.TIBS.2021.01.005
Ní Fhlathartaigh M, McMahon J, Reynolds R et al (2013) Calreticulin and other components of endoplasmic reticulum stress in rat and human inflammatory demyelination. Acta Neuropathol Commun 1:37. https://doi.org/10.1186/2051-5960-1-37
Ma X, Guo W, Yang S et al (2015) Serum GRP78 as a tumor marker and its prognostic significance in non-small cell lung cancers: a retrospective study. Dis Markers 2015:814670. https://doi.org/10.1155/2015/814670
Galli E, Planken A, Kadastik-Eerme L et al (2019) Increased serum levels of mesencephalic astrocyte-derived neurotrophic factor in subjects with Parkinson’s disease. Front Neurosci 13:929. https://doi.org/10.3389/fnins.2019.00929
Ladd JJ, Busald T, Johnson MM et al (2012) Increased plasma levels of the APC-interacting protein MAPRE1, LRG1, and IGFBP2 preceding a diagnosis of colorectal cancer in women. Cancer Prev Res 5:655–664. https://doi.org/10.1158/1940-6207.CAPR-11-0412
Oosterveld LP, Verberk IMW, Majbour NK et al (2020) CSF or serum neurofilament light added to α-Synuclein panel discriminates Parkinson’s from controls. Mov Disord 35:288–295. https://doi.org/10.1002/mds.27897
Parnetti L, Farotti L, Eusebi P et al (2014) Differential role of CSF alpha-synuclein species, tau, and Aβ42 in Parkinson’s Disease. Front Aging Neurosci 6:53. https://doi.org/10.3389/fnagi.2014.00053
Hardy-Sosa A, León-Arcia K, Llibre-Guerra JJ et al (2022) Diagnostic accuracy of blood-based biomarker panels: a systematic review. Front Aging Neurosci 14:683689. https://doi.org/10.3389/fnagi.2022.683689
Majbour NK, Vaikath NN, Van Dijk KD et al (2016) Oligomeric and phosphorylated alpha-synuclein as potential CSF biomarkers for Parkinson’s disease. Mol Neurodegener 11:1–15. https://doi.org/10.1186/s13024-016-0072-9
Williams SM, Schulz P, Sierks MR (2016) Oligomeric alpha-synuclein and beta-amyloid variants as potential biomarkers for Parkinson’s and Alzheimer’s diseases. Eur J Neurosci 43:3–16. https://doi.org/10.1111/ejn.13056
Wang X, Yu S, Li F, Feng T (2015) Detection of α-synuclein oligomers in red blood cells as a potential biomarker of Parkinson’s disease. Neurosci Lett 599:115–119. https://doi.org/10.1016/j.neulet.2015.05.030
Zhang X, Yin X, Yu H et al (2011) Quantitative proteomic analysis of serum proteins in patients with Parkinson’s disease using an isobaric tag for relative and absolute quantification labeling, two-dimensional liquid chromatography, and tandem mass spectrometry. Analyst 137:490–495. https://doi.org/10.1039/c1an15551b
Genereux JC, Qu S, Zhou M et al (2015) Unfolded protein response-induced ERdj3 secretion links ER stress to extracellular proteostasis. EMBO J 34:4–19. https://doi.org/10.15252/embj.201488896
Bräuer P, Parker JL, Gerondopoulos A et al (2019) Structural basis for pH-dependent retrieval of ER proteins from the Golgi by the KDEL receptor. Science 363:1103–1107. https://doi.org/10.1126/science.aaw2859
Martínez G, Duran-Aniotz C, Cabral-Miranda F et al (2017) Endoplasmic reticulum proteostasis impairment in aging. Aging Cell 16:615–623. https://doi.org/10.1111/acel.12599
Miller IN, Cronin-Golomb A (2010) Gender differences in Parkinson’s disease: clinical characteristics and cognition. Mov Disord 25:2695–2703. https://doi.org/10.1002/mds.23388
Ren H, Zhai W, Lu X, Wang G (2021) The cross-links of endoplasmic reticulum stress, autophagy, and neurodegeneration in Parkinson’s disease. Front Aging Neurosci 13:691881. https://doi.org/10.3389/fnagi.2021.691881
Kim S, Kim DK, Jeong S, Lee J (2022) The common cellular events in the neurodegenerative diseases and the associated role of endoplasmic reticulum stress. Int J Mol Sci 23:5894. https://doi.org/10.3390/IJMS23115894
Jiang P, Gan M, Lin WL, Yen SHC (2014) Nutrient deprivation induces α-synuclein aggregation through endoplasmic reticulum stress response and SREBP2 pathway. Front Aging Neurosci 6:268. https://doi.org/10.3389/fnagi.2014.00268
Cóppola-Segovia V, Cavarsan C, Maia FG et al (2017) ER stress induced by tunicamycin triggers α-synuclein oligomerization, dopaminergic neurons death and locomotor impairment: a new model of Parkinson’s disease. Mol Neurobiol 54:5798–5806. https://doi.org/10.1007/s12035-016-0114-x
Si X, Tian J, Chen Y et al (2019) Central nervous system-derived exosomal alpha-synuclein in serum may be a biomarker in Parkinson’s disease. Neuroscience 413:308–316. https://doi.org/10.1016/j.neuroscience.2019.05.015
Wang HL, Lu CS, Yeh TH et al (2019) Combined assessment of serum alpha-synuclein and RAB35 is a better biomarker for Parkinson’s disease. J Clin Neurol 15:488–495. https://doi.org/10.3988/jcn.2019.15.4.488
Chang C-W, Yang S-Y, Yang C-C et al (2020) Plasma and serum alpha-synuclein as a biomarker of diagnosis in patients with Parkinson’s disease. Front Neurol 10:1388. https://doi.org/10.3389/fneur.2019.01388
Barbour R, Kling K, Anderson JP et al (2008) Red blood cells are the major source of alpha-synuclein in blood. Neurodegener Dis 5:55–59. https://doi.org/10.1159/000112832
Postuma RB, Berg D, Stern M et al (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1601. https://doi.org/10.1002/mds.26424
Tarr JM, Winyard PG, Ryan B et al (2010) Extracellular calreticulin is present in the joints of patients with rheumatoid arthritis and inhibits FasL (CD95L)-mediated apoptosis of T cells. Arthritis Rheum 62:2919–2929. https://doi.org/10.1002/ART.27602
Apostolou A, Shen Y, Liang Y et al (2008) Armet, a UPR-upregulated protein, inhibits cell proliferation and ER stress-induced cell death. Exp Cell Res 314:2454–2467. https://doi.org/10.1016/J.YEXCR.2008.05.001
Mesgarzadeh JS, Buxbaum JN, Luke Wiseman R (2022) Stress-responsive regulation of extracellular proteostasis. J Cell Biol 221(4):e202112104. https://doi.org/10.1083/JCB.202112104
Giusti L, Baldini C, Ciregia F et al (2010) Is GRP78/BiP a potential salivary biomarker in patients with rheumatoid arthritis? Proteomics Clin Appl 4:315–324. https://doi.org/10.1002/PRCA.200900082
Gwark S, Ahn HS, Yeom J et al (2021) Plasma proteome signature to predict the outcome of breast cancer patients receiving neoadjuvant chemotherapy. Cancers (Basel) 13(24):6267. https://doi.org/10.3390/CANCERS13246267
Cohen AC (1959) Simplified estimators for the normal distribution when samples are singly censored or truncated. Technometrics 1:217–237. https://doi.org/10.2307/1266442
Jovanovic BD (1991) Subset selection in regression. Stat Med 10:1164–1165. https://doi.org/10.1002/sim.4780100719
Spiegelhalter DJ (1986) Probabilistic prediction in patient management and clinical trials. Stat Med 5:421–433. https://doi.org/10.1002/sim.4780050506
Picard RR, Cook RD (1984) Cross-validation of regression models. J Am Stat Assoc 79:575–583. https://doi.org/10.1080/01621459.1984.10478083
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36. https://doi.org/10.1148/radiology.143.1.7063747
Vickers AJ, Elkin EB (2006) Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making 26:565–574. https://doi.org/10.1177/0272989X06295361
Acknowledgements
The authors are very grateful to all participants who kindly agreed to participate in this study and to all who assisted in the recruitment of volunteers, including Galway Parkinson’s Association, An Teaghlach Uilinn Nursing Home, and St. Mary’s Nursing Home. We express our gratitude to the phlebotomy service at University Hospital Galway for blood collection.
Funding
This publication has emanated from research conducted with the financial support of Enterprise Ireland Innovation Partnership Programme (IP 2016 0480), Precision Oncology Ireland, which is part-funded by the Science Foundation Ireland (SFI) Strategic Partnership Programme (18/SPP/3522), EU H2020 MSCA RISE-734749 (INSPIRED), (H2020-MSCA-IF-2016), Medtrain (MSCA COFUND-713690), EU H2020 MSCA ITN-675448 (TRAINERS).
Author information
Authors and Affiliations
Contributions
Research project conception: A.M.G and A.S. Organization: K. Mnich, A.M.G., and A.S. Execution: K. Mnich, P.B., and S.P.F. Statistical analysis design: K. Mnich and S.M. Execution: K. Mnich and S.M. Review and critique: S.M., P.B., K. Martin, C.R., and A.M.G. Writing of the first draft: K. Mnich and S.M. Review and critique: P.B., T.C., S.P.F., K. Martin, C.R., A.S., and A.M.G. Obtaining funding: K. Mnich, T.C., K. Martin, C.R., and A.M.G.
Corresponding author
Ethics declarations
Ethics Approval
The cross-sectional pilot study was approved by the University Hospital Galway Research Ethics committee.
Consent to Participate
Written informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not applicable.
Competing Interests
Adrienne M. Gorman and Afshin Samali are cofounders of Cell Stress Discoveries, Ltd. Kenneth Martin and Ciaran Richardson are employed by Randox Teoranta. Stephen P. Fitzgerald is employed by Randox Holdings. This work was conducted in collaboration with Randox Teoranta, which contributed to the funding. The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mnich, K., Moghaddam, S., Browne, P. et al. Endoplasmic Reticulum Stress-Regulated Chaperones as a Serum Biomarker Panel for Parkinson’s Disease. Mol Neurobiol 60, 1476–1485 (2023). https://doi.org/10.1007/s12035-022-03139-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-022-03139-0