Abstract
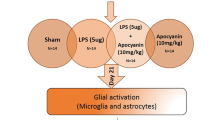
Lipocalin-2 (LCN2) is an important regulator of both neuroinflammation and iron homeostasis. Upregulated LCN2 was observed in reactive astrocytes in the Parkinson’s disease (PD) models. In the present study, we reported iron chelator deferoxamine (DFO) abolished lipopolysaccharide (LPS)-induced LCN2 upregulation in primary astrocytes, although iron overload had no effects. The suppressive effects of DFO were consistent with autophagy inducer rapamycin or carfilzomib, blocked by autophagy inhibitor 3-methyladenine rather than chloroquine or bafilomycin A1, meanwhile, while were not dependent on proteasome system and NF-κB pathway. DFO was not able to ameliorate LCN2 upregulation in α-synuclein-treated astrocytes, because DFO failed to induce autophagy in these cells. We further demonstrated that DFO could not enhance autophagy lysosomal degradation, however promoted secretory autophagy in primary astrocytes with LPS insults. These data suggest that DFO could serve as an autophagy activator, capable of ameliorating the upregulation of LCN2 in astrocytes by acting on the formation of autophagosomes and secretory autophagy. This provides better understandings of DFO-mediated neuroprotection against neuroinflammation and provides new insights that autophagy activation could be beneficial approaches in PD.








Similar content being viewed by others
Data Availability
All data in our study are available upon request.
References
Jankovic J, Tan EK (2020) Parkinson’s disease: etiopathogenesis and treatment. J Neurol Neurosurg Psychiatry 91(8):795–808
Bloem BR, Okun MS, Klein C (2021) Parkinson’s disease. Lancet 397(10291):2284–2303
Verstraeten A, Theuns J, Van Broeckhoven C (2015) Progress in unraveling the genetic etiology of Parkinson disease in a genomic era. Trends Genet 31(3):140–149
Bellou V et al (2016) Environmental risk factors and Parkinson’s disease: an umbrella review of meta-analyses. Parkinsonism Relat Disord 23:1–9
Trist BG, Hare DJ, Double KL (2019) Oxidative stress in the aging substantia nigra and the etiology of Parkinson’s disease. Aging Cell 18(6):e13031
Gelders G, Baekelandt V, Van der Perren A (2018) Linking neuroinflammation and neurodegeneration in Parkinson’s disease. J Immunol Res 2018:4784268
Jiang P, Dickson DW (2018) Parkinson’s disease: experimental models and reality. Acta Neuropathol 135(1):13–32
Yun SP et al (2018) Block of A1 astrocyte conversion by microglia is neuroprotective in models of Parkinson’s disease. Nat Med 24(7):931–938
Joshi AU et al (2019) Fragmented mitochondria released from microglia trigger A1 astrocytic response and propagate inflammatory neurodegeneration. Nat Neurosci 22(10):1635–1648
Fellner L et al (2013) Toll-like receptor 4 is required for α-synuclein dependent activation of microglia and astroglia. Glia 61(3):349–360
Rannikko EH, Weber SS, Kahle PJ (2015) Exogenous α-synuclein induces toll-like receptor 4 dependent inflammatory responses in astrocytes. BMC Neurosci 16:57
Kim C et al (2018) Immunotherapy targeting toll-like receptor 2 alleviates neurodegeneration in models of synucleinopathy by modulating α-synuclein transmission and neuroinflammation. Mol Neurodegener 13(1):43
Xiao X, Yeoh BS, Vijay-Kumar M (2017) Lipocalin 2: an emerging player in iron homeostasis and inflammation. Annu Rev Nutr 37:103–130
Xing C et al (2014) Neuronal production of lipocalin-2 as a help-me signal for glial activation. Stroke 45(7):2085–2092
Al Nimer F et al (2016) Lipocalin-2 is increased in progressive multiple sclerosis and inhibits remyelination. Neurol Neuroimmunol Neuroinflamm 3(1):e191
Llorens F et al (2020) Cerebrospinal fluid lipocalin 2 as a novel biomarker for the differential diagnosis of vascular dementia. Nat Commun 11(1):619
Choi J, Lee HW, Suk K (2011) Increased plasma levels of lipocalin 2 in mild cognitive impairment. J Neurol Sci 305(1–2):28–33
Kang SS et al (2018) Lipocalin-2 protects the brain during inflammatory conditions. Mol Psychiatry 23(2):344–350
Jin M, Jang E, Suk K (2014) Lipocalin-2 acts as a neuroinflammatogen in lipopolysaccharide-injected mice. Exp Neurobiol 23(2):155–162
Kim BW et al (2016) Pathogenic upregulation of glial lipocalin-2 in the Parkinsonian dopaminergic system. J Neurosci 36(20):5608–5622
Zucca FA et al (2017) Interactions of iron, dopamine and neuromelanin pathways in brain aging and Parkinson’s disease. Prog Neurobiol 155:96–119
Du G et al (2016) Quantitative susceptibility mapping of the midbrain in Parkinson’s disease. Mov Disord 31(3):317–324
Sun J et al (2020) Quantitative evaluation of iron content in idiopathic rapid eye movement sleep behavior disorder. Mov Disord 35(3):478–485
Tambasco N et al (2019) T2*-weighted MRI values correlate with motor and cognitive dysfunction in Parkinson’s disease. Neurobiol Aging 80:91–98
Martin-Bastida A et al (2021) Iron and inflammation: in vivo and post-mortem studies in Parkinson’s disease. J Neural Transm (Vienna) 128(1):15–25
Liu C et al (2018) S-Nitrosylation of divalent metal transporter 1 enhances iron uptake to mediate loss of dopaminergic neurons and motoric deficit. J Neurosci 38(39):8364–8377
Urrutia P et al (2013) Inflammation alters the expression of DMT1, FPN1 and hepcidin, and it causes iron accumulation in central nervous system cells. J Neurochem 126(4):541–549
Wang J et al (2013) Pro-inflammatory cytokines modulate iron regulatory protein 1 expression and iron transportation through reactive oxygen/nitrogen species production in ventral mesencephalic neurons. Biochim Biophys Acta 1832(5):618–625
Bousset L et al (2013) Structural and functional characterization of two alpha-synuclein strains. Nat Commun 4:2575
Abdelmotilib H et al (2017) α-Synuclein fibril-induced inclusion spread in rats and mice correlates with dopaminergic Neurodegeneration. Neurobiol Dis 105:84–98
Cui J et al (2020) Hepcidin-to-ferritin ratio is decreased in astrocytes with extracellular alpha-synuclein and iron exposure. Front Cell Neurosci 14:47
Freundt EC, Czapiga M, Lenardo MJ (2007) Photoconversion of Lysotracker Red to a green fluorescent molecule. Cell Res 17(11):956–958
Ma Y et al (2011) MG132 treatment attenuates cardiac remodeling and dysfunction following aortic banding in rats via the NF-κB/TGFβ1 pathway. Biochem Pharmacol 81(10):1228–1236
Zhang XM et al (2020) MG-132 attenuates cardiac deterioration of viral myocarditis via AMPK pathway. Biomed Pharmacother 126:110091
De Domenico I, Ward DM, Kaplan J (2009) Specific iron chelators determine the route of ferritin degradation. Blood 114(20):4546–4551
Altmann C et al (2016) Progranulin overexpression in sensory neurons attenuates neuropathic pain in mice: Role of autophagy. Neurobiol Dis 96:294–311
Guan J et al (2015) Lysosomal dysfunction and impaired autophagy underlie the pathogenesis of amyloidogenic light chain-mediated cardiotoxicity. EMBO Mol Med 7(5):688
Kimura S, Noda T, Yoshimori T (2007) Dissection of the autophagosome maturation process by a novel reporter protein, tandem fluorescent-tagged LC3. Autophagy 3(5):452–460
Nickel W, Rabouille C (2018) Unconventional protein secretion: diversity and consensus. Semin Cell Dev Biol 83:1–2
Dupont N et al (2011) Autophagy-based unconventional secretory pathway for extracellular delivery of IL-1β. Embo J 30(23):4701–4711
Lee HJ et al (2010) Direct transfer of alpha-synuclein from neuron to astroglia causes inflammatory responses in synucleinopathies. J Biol Chem 285(12):9262–9272
McAlpine CS et al (2021) Astrocytic interleukin-3 programs microglia and limits Alzheimer’s disease. Nature 595(7869):701–706
Przedborski S (2017) The two-century journey of Parkinson disease research. Nat Rev Neurosci 18(4):251–259
Sorrentino ZA, Giasson BI, Chakrabarty P (2019) α-Synuclein and astrocytes: tracing the pathways from homeostasis to neurodegeneration in Lewy body disease. Acta Neuropathol 138(1):1–21
Chavarría C et al (2018) Impact of monomeric, oligomeric and fibrillar alpha-synuclein on astrocyte reactivity and toxicity to neurons. Biochem J 475(19):3153–3169
Moreau C et al (2018) Iron as a therapeutic target for Parkinson’s disease. Mov Disord 33(4):568–574
Song N, Xie J (2018) Iron, dopamine, and α-synuclein interactions in at-risk dopaminergic neurons in Parkinson’s disease. Neurosci Bull 34(2):382–384
Cerri S, Mus L, Blandini F (2019) Parkinson’s Disease in Women and Men: What’s the Difference? J Parkinsons Dis 9(3):501–515
Xu M et al (2019) Differential regulation of estrogen in iron metabolism in astrocytes and neurons. J Cell Physiol 234(4):4232–4242
Owen JE, Bishop GM, Robinson SR (2016) Uptake and toxicity of hemin and iron in cultured mouse astrocytes. Neurochem Res 41(1–2):298–306
Ip JP et al (2011) Lipocalin 2 in the central nervous system host response to systemic lipopolysaccharide administration. J Neuroinflammation 8:124
Ni W et al (2015) Role of lipocalin-2 in brain injury after intracerebral hemorrhage. J Cereb Blood Flow Metab 35(9):1454–1461
Devireddy LR et al (2005) A cell-surface receptor for lipocalin 24p3 selectively mediates apoptosis and iron uptake. Cell 123(7):1293–1305
Dekens DW et al (2021) Lipocalin 2 as a link between ageing, risk factor conditions and age-related brain diseases. Ageing Res Rev 70:101414
Suk K (2016) Lipocalin-2 as a therapeutic target for brain injury: an astrocentric perspective. Prog Neurobiol 144:158–172
Listwak SJ, Rathore P, Herkenham M (2013) Minimal NF-κB activity in neurons. Neuroscience 250:282–299
Parmar T et al (2018) Lipocalin 2 plays an important role in regulating inflammation in retinal degeneration. J Immunol 200(9):3128–3141
Zhao W, Bendickson L, Nilsen-Hamilton M (2020) The lipocalin2 gene is regulated in mammary epithelial cells by NFκB and C/EBP in response to mycoplasma. Sci Rep 10(1):7641
Dimopoulos M et al (2020) Carfilzomib, dexamethasone, and daratumumab versus carfilzomib and dexamethasone for patients with relapsed or refractory multiple myeloma (CANDOR): results from a randomised, multicentre, open-label, phase 3 study. Lancet 396(10245):186–197
Mishima Y et al (2015) Ricolinostat (ACY-1215) induced inhibition of aggresome formation accelerates carfilzomib-induced multiple myeloma cell death. Br J Haematol 169(3):423–434
Jarauta V et al (2016) Inhibition of autophagy with chloroquine potentiates carfilzomib-induced apoptosis in myeloma cells in vitro and in vivo. Cancer Lett 382(1):1–10
Kim KH, Lee MS (2014) Autophagy–a key player in cellular and body metabolism. Nat Rev Endocrinol 10(6):322–337
Chen LL et al (2019) Iron dysregulation in Parkinson’s disease: focused on the autophagy-lysosome pathway. ACS Chem Neurosci 10(2):863–871
Song L, Zhang L (2020) Tau accumulation and defective autophagy: a common pathological mechanism underlying repeat-expansion-induced neurodegenerative diseases? Neurosci Bull 36(12):1411–1413
Moon JH, Jeong JK, Park SY (2015) Deferoxamine inhibits TRAIL-mediated apoptosis via regulation of autophagy in human colon cancer cells. Oncol Rep 33(3):1171–1176
Rakshit J et al (2020) Iron chelator Deferoxamine protects human neuroblastoma cell line SH-SY5Y from 6-Hydroxydopamine-induced apoptosis and autophagy dysfunction. J Trace Elem Med Biol 57:126406
Mizushima N, Yoshimori T, Levine B (2010) Methods in mammalian autophagy research. Cell 140(3):313–326
Klionsky DJ et al (2021) Guidelines for the use and interpretation of assays for monitoring autophagy (4th edition)(1). Autophagy 17(1):1–382
Yang C et al (2017) Curcumin induces apoptosis and protective autophagy in castration-resistant prostate cancer cells through iron chelation. Drug Des Devel Ther 11:431–439
Rainey NE et al (2019) Iron chelation by curcumin suppresses both curcumin-induced autophagy and cell death together with iron overload neoplastic transformation. Cell Death Discov 5:150
Tury S et al (2018) The iron chelator deferasirox synergises with chemotherapy to treat triple-negative breast cancers. J Pathol 246(1):103–114
Ponpuak M et al (2015) Secretory autophagy. Curr Opin Cell Biol 35:106–116
Ejlerskov P et al (2013) Tubulin polymerization-promoting protein (TPPP/p25α) promotes unconventional secretion of α-synuclein through exophagy by impairing autophagosome-lysosome fusion. J Biol Chem 288(24):17313–17335
Nilsson P et al (2013) Aβ secretion and plaque formation depend on autophagy. Cell Rep 5(1):61–69
Winslow AR et al (2010) α-Synuclein impairs macroautophagy: implications for Parkinson’s disease. J Cell Biol 190(6):1023–1037
Tanik SA et al (2013) Lewy body-like α-synuclein aggregates resist degradation and impair macroautophagy. J Biol Chem 288(21):15194–15210
Yap TL et al (2011) Alpha-synuclein interacts with Glucocerebrosidase providing a molecular link between Parkinson and Gaucher diseases. J Biol Chem 286(32):28080–28088
Yap TL et al (2013) Membrane-bound α-synuclein interacts with glucocerebrosidase and inhibits enzyme activity. Mol Genet Metab 108(1):56–64
Mazzulli JR et al (2011) Gaucher disease glucocerebrosidase and α-synuclein form a bidirectional pathogenic loop in synucleinopathies. Cell 146(1):37–52
Choi I et al (2020) Microglia clear neuron-released α-synuclein via selective autophagy and prevent neurodegeneration. Nat Commun 11(1):1386
Chen L et al (2021) Corynoxine protects dopaminergic neurons through inducing autophagy and diminishing neuroinflammation in rotenone-induced animal models of Parkinson’s disease. Front Pharmacol 12:642900
Acknowledgements
None.
Funding
This work was supported by the National Natural Science Foundation of China (31771124, 32170984, and 31871049), the Natural Science Foundation of Shandong Province (ZR2021MC116), the Excellent Innovative Team of Shandong Province, and the Taishan Scholars Construction Project.
Author information
Authors and Affiliations
Contributions
Ning Song and Junxia Xie designed and revised the article; Juntao Cui, Yu Yuan, and Jun Wang performed the experiments and analyzed the data. Ning Song and Juntao Cui wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics Approval
Procedures were carried out in accordance with the NIH Guide for the Care and Use of Laboratory Animals and were approved by the Ethical Committee of the Medical College of Qingdao University.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cui, J., Yuan, Y., Wang, J. et al. Desferrioxamine Ameliorates Lipopolysaccharide-Induced Lipocalin-2 Upregulation via Autophagy Activation in Primary Astrocytes. Mol Neurobiol 59, 2052–2067 (2022). https://doi.org/10.1007/s12035-021-02687-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-021-02687-1