Abstract
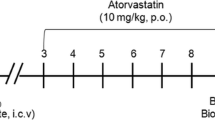
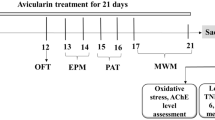
Amyloid-β (Aβ) peptides play a significant role in the pathogenesis of Alzheimer’s disease (AD). Neurotoxic effects promoted by Aβ peptides involve glutamate transmission impairment, decrease of neurotrophic factors, mitochondrial dysfunction, oxidative stress, synaptotoxicity, and neuronal degeneration. Here, we assessed the early events evoked by Aβ1–40 on the hippocampus. Additionally, we sought to unravel the molecular mechanisms of atorvastatin preventive effect on Aβ-induced hippocampal damage. Mice were treated orally (p.o.) with atorvastatin 10 mg/kg/day during 7 consecutive days before the intracerebroventricular (i.c.v.) infusion of Aβ1–40 (400 pmol/site). Twenty-four hours after Aβ1–40 infusion, a reduced content of mature BDNF/proBDNF ratio was observed in Aβ-treated mice. However, there is no alteration in synaptophysin, PSD-95, and doublecortin immunocontent in the hippocampus. Aβ1–40 promoted an increase in reactive oxygen species (ROS) and nitric oxide (NO) generation in hippocampal slices, and atorvastatin prevented this oxidative burst. Mitochondrial OXPHOS was measured by high-resolution respirometry. At this time point, Aβ1–40 did not alter the O2 consumption rates (OCR) related to phosphorylating state associated with complexes I and II, and the maximal OCR. However, atorvastatin increased OCR of phosphorylating state associated with complex I and complexes I and II, maximal OCR of complexes I and II, and OCR associated with mitochondrial spare capacity. Atorvastatin treatment improved mitochondrial function in the rodent hippocampus, even after Aβ infusion, pointing to a promising effect of improving brain mitochondria bioenergetics. Therefore, atorvastatin could act as an adjuvant in battling the symptoms of AD to preventing or delaying the disease progression.





Similar content being viewed by others
Abbreviations
- Aβ:
-
Amyloid-beta
- Aβ1–40 :
-
Amyloid-beta1–40 peptide
- AD:
-
Alzheimer’s disease
- Ator:
-
Atorvastatin
- BDNF:
-
Brain-derived neurotrophic factor
- ETS:
-
Electron transport system
- HMG-CoA:
-
hydroxy-methylglutaryl-CoA
- i.c.v.:
-
Intracerebroventricular
- NMDA:
-
N-methyl-D-aspartate
- NO:
-
Nitric oxide
- NOS2:
-
Inducible nitric oxide synthase
- OCR:
-
Oxygen consumption rate
- OXPHOS:
-
Mitochondrial oxidative phosphorylation
- Δψmit:
-
Mitochondrial membrane potential
- PSD-95:
-
Postsynaptic protein of 95 kDaltons
- ROS:
-
Reactive oxygen species.
References
Billings LM, Oddo S, Green KN, McGaugh JL, LaFerla FM (2005) Intraneuronal A?? causes the onset of early Alzheimer’s disease-related cognitive deficits in transgenic mice. Neuron 45:675–688. https://doi.org/10.1016/j.neuron.2005.01.040
De Felice FG, Velasco PT, Lambert MP et al (2007) Abeta oligomers induce neuronal oxidative stress through an N-methyl-D-aspartate receptor-dependent mechanism that is blocked by the Alzheimer drug memantine. J Biol Chem 282:11590–11601. https://doi.org/10.1074/jbc.M607483200
Kayed R, Lasagna-Reeves CA (2013) Molecular mechanisms of amyloid oligomers toxicity. In: Alzheimer’s disease: advances for a new century
Imtiaz B, Tolppanen A-M, Kivipelto M, Soininen H (2014) Future directions in Alzheimer’s disease from risk factors to prevention. Biochem Pharmacol 88:661–670. https://doi.org/10.1016/j.bcp.2014.01.003
Hamel E, Royea J, Ongali B, Tong XK (2016) Neurovascular and cognitive failure in Alzheimer???s disease: benefits of cardiovascular therapy. Cell Mol Neurobiol 36:219–232
Stone J (2008) What initiates the formation of senile plaques? The origin of Alzheimer-like dementias in capillary haemorrhages. Med Hypotheses 71:347–359. https://doi.org/10.1016/j.mehy.2008.04.007
Arbor SC, Lafontaine M, Cumbay M (2016) Amyloid-beta Alzheimer targets — protein processing, lipid rafts, and amyloid-beta pores. Yale J Biol Med 89(1):5-21. PMC:4797837 PMID: 27505013
Prince M, Wimo A, Guerchet M et al (2015) World Alzheimer Report 2015: the global impact of dementia - an analysis of prevalence, incidence, cost and trends. Alzheimers Dis Int 84:140–144. https://doi.org/10.1111/j.0963-7214.2004.00293.x
Götz J, Lim YA, Ke YD et al (2010) Dissecting toxicity of tau and β-amyloid. In: Neurodegenerative diseases
Motter R, Vigo-Pelfrey C, Kholodenko D, Barbour R, Johnson-Wood K, Galasko D, Chang L, Miller B et al (1995) Reduction of β-amyloid peptide42 in the cerebrospinal fluid of patients with Alzheimer’s disease. Ann Neurol 38:643–648. https://doi.org/10.1002/ana.410380413
Karran E, De Strooper B (2016) The amyloid cascade hypothesis: are we poised for success or failure? J Neurochem 139:237–252. https://doi.org/10.1111/jnc.13632
Masters CL, Selkoe DJ (2012) Biochemistry of amyloid β-protein and amyloid deposits in Alzheimer disease. Cold Spring Harb Perspect Med 2(6):a006262. https://doi.org/10.1101/cshperspect.a006262
Piaceri I, Rinnoci V, Bagnoli S, Failli Y, Sorbi S (2012) Mitochondria and Alzheimer’s disease. J Neurol Sci 322:31–34. https://doi.org/10.1016/j.jns.2012.05.033
Demuro A, Parker I, Stutzmann GE (2010) Calcium signaling and amyloid toxicity in Alzheimer disease. J Biol Chem 285:12463–12468. https://doi.org/10.1074/jbc.R109.080895
Shin MK, Kim HG, Baek SH, Jung WR, Park DI, Park JS, Jo DG, Kim KL (2014) Neuropep-1 ameliorates learning and memory deficits in an Alzheimer’s disease mouse model, increases brain-derived neurotrophic factor expression in the brain, and causes reduction of amyloid beta plaques. Neurobiol Aging 35:990–1001. https://doi.org/10.1016/j.neurobiolaging.2013.10.091
Poo M ming (2001) Neurotrophins as synaptic modulators. Nat Rev Neurosci 2:24–32. https://doi.org/10.1038/35049004
Ehrlich I, Klein M, Rumpel S, Malinow R (2007) PSD-95 is required for activity-driven synapse stabilization. Proc Natl Acad Sci 104:4176–4181. https://doi.org/10.1073/pnas.0609307104
Sze CI, Troncoso JC, Kawas C et al (1997) Loss of the presynaptic vesicle protein synaptophysin in hippocampus correlates with cognitive decline in Alzheimer disease. J Neuropathol Exp Neurol 56:933–944. https://doi.org/10.1097/00005072-199708000-00011
Murphy MP (2009) How mitochondria produce reactive oxygen species. Biochem J 417:1–13. https://doi.org/10.1042/BJ20081386
Du H, Guo L, Yan S et al (2010) Early deficits in synaptic mitochondria in an Alzheimer’s disease mouse model. Proc Natl Acad Sci U S A 107:18670–18675. https://doi.org/10.1073/pnas.1006586107
Moreira PI, Carvalho C, Zhu X et al (2010) Mitochondrial dysfunction is a trigger of Alzheimer’s disease pathophysiology. Biochim Biophys Acta Mol Basis Dis 1802(1):2-10. https://doi.org/10.1016/j.bbadis.2009.10.006
Swerdlow RH, Khan SM (2009) The Alzheimer’s disease mitochondrial cascade hypothesis: an update. Exp Neurol 218:308–315
Hu H, Li M (2016) Mitochondria-targeted antioxidant mitotempo protects mitochondrial function against amyloid beta toxicity in primary cultured mouse neurons. Biochem Biophys Res Commun 478:174–180. https://doi.org/10.1016/j.bbrc.2016.07.071
Crouch PJ, Blake R, Duce JA et al (2005) Copper-dependent inhibition of human cytochrome c oxidase by a dimeric conformer of amyloid-beta1-42. J Neurosci. https://doi.org/10.1523/JNEUROSCI.4276-04.2005
Westermann B (2009) Nitric oxide links mitochondrial fission to Alzheimer’s disease. Sci Signal
Angelova PR, Abramov AY (2014) Interaction of neurons and astrocytes underlies the mechanism of Aβ-induced neurotoxicity. Biochem Soc Trans 42:1286–1290. https://doi.org/10.1042/BST20140153
Lanctôt KL, Rajaram RD, Herrmann N (2009) Therapy for Alzheimer’s disease: how effective are current treatments? Ther Adv Neurol Disord 2(3):163-80. https://doi.org/10.1177/1756285609102724
Feldman HH, Doody RS, Kivipelto M, Sparks DL, Waters DD, Jones RW, Schwam E, Schindler R et al (2010) Randomized controlled trial of atorvastatin in mild to moderate Alzheimer disease: LEADe. Neurology 74:956–964. https://doi.org/10.1212/WNL.0b013e3181d6476a
Geifman N, Brinton RD, Kennedy RE, Schneider LS, Butte AJ (2017) Evidence for benefit of statins to modify cognitive decline and risk in Alzheimer’s disease. Alzheimers Res Ther 9:10. https://doi.org/10.1186/s13195-017-0237-y
Liang T, Li R, Cheng O (2015) Statins for treating Alzheimer’s disease: truly ineffective? Eur Neurol 73:360–366. https://doi.org/10.1159/000382128
Carlsson CM, Xu G, Wen Z et al (2012) Effects of atorvastatin on cerebral blood flow in middle-aged adults at risk for Alzheimer’s disease: a pilot study. Curr Alzheimer Res. https://doi.org/10.2174/156720512803251075
Lu D, Goussev A, Chen J, Pannu P, Li Y, Mahmood A, Chopp M (2004) Atorvastatin reduces neurological deficit and increases synaptogenesis, angiogenesis, and neuronal survival in rats subjected to traumatic brain injury. J Neurotrauma 21:21–32. https://doi.org/10.1089/089771504772695913
Reis PA, Alexandre PCB, D’Avila JC, Siqueira LD, Antunes B, Estato V, Tibiriça EV, Verdonk F et al (2017) Statins prevent cognitive impairment after sepsis by reverting neuroinflammation, and microcirculatory/endothelial dysfunction. Brain Behav Immun 60:293–303. https://doi.org/10.1016/j.bbi.2016.11.006
Boimel M, Grigoriadis N, Lourbopoulos A, Touloumi O, Rosenmann D, Abramsky O, Rosenmann H (2009) Statins reduce the neurofibrillary tangle burden in a mouse model of tauopathy. J Neuropathol Exp Neurol 68:314–325. https://doi.org/10.1097/NEN.0b013e31819ac3cb
Piermartiri TCB, Figueiredo CP, Rial D, Duarte FS, Bezerra SC, Mancini G, de Bem AF, Prediger RDS et al (2010) Atorvastatin prevents hippocampal cell death, neuroinflammation and oxidative stress following amyloid-β(1-40) administration in mice: evidence for dissociation between cognitive deficits and neuronal damage. Exp Neurol 226:274–284
Martins WC, dos Santos VV, dos Santos AA, Vandresen-Filho S, Dal-Cim TA, de Oliveira KA, Mendes-de-Aguiar CBN, Farina M et al (2015) Atorvastatin prevents cognitive deficits induced by intracerebroventricular amyloid-β1–40 administration in mice: involvement of glutamatergic and antioxidant systems. Neurotox Res 28:32–42. https://doi.org/10.1007/s12640-015-9527-y
Bicca MA, Figueiredo CP, Piermartiri TC, Meotti FC, Bouzon ZL, Tasca CI, Medeiros R, Calixto JB (2011) The selective and competitive N-methyl-D-aspartate receptor antagonist, (-)-6-phosphonomethyl-deca-hydroisoquinoline-3-carboxylic acid, prevents synaptic toxicity induced by amyloid-β in mice. Neuroscience 192:631–641. https://doi.org/10.1016/j.neuroscience.2011.06.038
Prediger RDS, Medeiros R, Pandolfo P, Duarte FS, Passos GF, Pesquero JB, Campos MM, Calixto JB et al (2008) Genetic deletion or antagonism of kinin B1 and B2 receptors improves cognitive deficits in a mouse model of Alzheimer’s disease. Neuroscience 151:631–643. https://doi.org/10.1016/j.neuroscience.2007.11.009
Medeiros R, Prediger RDS, Passos GF, Pandolfo P, Duarte FS, Franco JL, Dafre AL, di Giunta G et al (2007) Connecting TNF-alpha signaling pathways to iNOS expression in a mouse model of Alzheimer’s disease: relevance for the behavioral and synaptic deficits induced by amyloid beta protein. J Neurosci 27:5394–5404. https://doi.org/10.1523/JNEUROSCI.5047-06.2007
Ehrenberg B, Montana V, Wei MD, Wuskell JP, Loew LM (1988) Membrane potential can be determined in individual cells from the nernstian distribution of cationic dyes. Biophys J 53:785–794. https://doi.org/10.1016/S0006-3495(88)83158-8
Perry SW, Norman JP, Barbieri J, Brown EB, Gelbard HA (2011) Mitochondrial membrane potential probes and the proton gradient: a practical usage guide. Biotechniques 50:98–115
Lorrio S, Gómez-Rangel V, Negredo P et al (2013) Novel multitarget ligand ITH33/IQM9.21 provides neuroprotection in in vitro and in vivo models related to brain ischemia. Neuropharmacology. https://doi.org/10.1016/j.neuropharm.2012.12.001
Ferreira AGK, Da Cunha AA, MacHado FR et al (2012) Experimental hyperprolinemia induces mild oxidative stress, metabolic changes, and tissue adaptation in rat liver. J Cell Biochem 113:174–183. https://doi.org/10.1002/jcb.23342
Hernanz R, Briones AM, Martín Á, Beltrán AE, Tejerina T, Salaices M, Alonso MJ (2008) Ouabain treatment increases nitric oxide bioavailability and decreases superoxide anion production in cerebral vessels. J Hypertens 26:1944–1954. https://doi.org/10.1097/HJH.0b013e328308de55
Oliveira CS, Rigon AP, Leal RB, Rossi FM (2008) The activation of ERK1/2 and p38 mitogen-activated protein kinases is dynamically regulated in the developing rat visual system. Int J Dev Neurosci 26:355–362. https://doi.org/10.1016/j.ijdevneu.2007.12.007
Peterson GL (1977) A simplification of the protein assay method of Lowry et al. which is more generally applicable. Anal Biochem. https://doi.org/10.1016/0003-2697(77)90043-4
Cassina A, Radi R (1996) Differential inhibitory action of nitric oxide and peroxynitrite on mitochondrial electron transport. Arch Biochem Biophys 328:309–316. https://doi.org/10.1006/abbi.1996.0178
Fischer JC, Ruitenbeek W, Berden JA, Trijbels JMF, Veerkamp JH, Stadhouders AM, Sengers RCA, Janssen AJM (1985) Differential investigation of the capacity of succinate oxidation in human skeletal muscle. Clin Chim Acta 153:23–36. https://doi.org/10.1016/0009-8981(85)90135-4
Rustin P, Chretien D, Bourgeron T, Gérard B, Rötig A, Saudubray JM, Munnich A (1994) Biochemical and molecular investigations in respiratory chain deficiencies. Clin Chim Acta 228:35–51. https://doi.org/10.1016/0009-8981(94)90055-8
Burtscher J, Zangrandi L, Schwarzer C, Gnaiger E (2015) Differences in mitochondrial function in homogenated samples from healthy and epileptic specific brain tissues revealed by high-resolution respirometry. Mitochondrion 25:104–112. https://doi.org/10.1016/j.mito.2015.10.007
Gnaiger E (2014) Mitochondrial pathways and respiratory control an introduction to OXPHOS analysis
Amoêdo ND, Rodrigues MF, Pezzuto P, Galina A, da Costa RM, de Almeida FCL, el-Bacha T, Rumjanek FD (2011) Energy metabolism in H460 lung cancer cells: effects of histone deacetylase inhibitors. PLoS One 6:e22264. https://doi.org/10.1371/journal.pone.0022264
Martins WC, Niebisch CH, Cláudia B (2018) Atorvastatin and amyloid-Beta 1-40 promote differential gene expression of proteins involved on glutamatergic transmission in the cerebral cortex and hippocampus. 1:1–8. http://www.thebiomedica.org/articles/jppr.002.pdf
Piermartiri TCB, Figueiredo CP, Rial D, Duarte FS, Bezerra SC, Mancini G, de Bem AF, Prediger RDS et al (2010) Atorvastatin prevents hippocampal cell death, neuroinflammation and oxidative stress following amyloid-β1-40 administration in mice: evidence for dissociation between cognitive deficits and neuronal damage. Exp Neurol 226:274–284. https://doi.org/10.1016/j.expneurol.2010.08.030
Ludka FK, Cunha MP, Dal-Cim T, Binder LB, Constantino LC, Massari CM, Martins WC, Rodrigues ALS et al (2017) Atorvastatin protects from Aβ1–40-induced cell damage and depressive-like behavior via ProBDNF cleavage. Mol Neurobiol 54:6163–6173. https://doi.org/10.1007/s12035-016-0134-6
Lanznaster D, Mack JM, Coelho V, Ganzella M, Almeida RF, Dal-Cim T, Hansel G, Zimmer ER et al (2017) Guanosine prevents anhedonic-like behavior and impairment in hippocampal glutamate transport following amyloid-β1–40 administration in mice. Mol Neurobiol 54:5482–5496. https://doi.org/10.1007/s12035-016-0082-1
Bathina S, Das UN (2015) Brain-derived neurotrophic factor and its clinical implications. Arch Med Sci 6:1164–1178
Peng S, Wuu J, Mufson EJ, Fahnestock M (2005) Precursor form of brain-derived neurotrophic factor and mature brain-derived neurotrophic factor are decreased in the pre-clinical stages of Alzheimer’s disease. J Neurochem 93:1412–1421. https://doi.org/10.1111/j.1471-4159.2005.03135.x
Iwasaki Y, Negishi T, Inoue M, Tashiro T, Tabira T, Kimura N (2012) Sendai virus vector-mediated brain-derived neurotrophic factor expression ameliorates memory deficits and synaptic degeneration in a transgenic mouse model of Alzheimer’s disease. J Neurosci Res 90:981–989. https://doi.org/10.1002/jnr.22830
Zhou X-F, Li W-P, Zhou FH-H, Zhong JH, Mi JX, Wu LLY, Xian CJ (2005) Differential effects of endogenous brain-derived neurotrophic factor on the survival of axotomized sensory neurons in dorsal root ganglia: a possible role for the p75 neurotrophin receptor. Neuroscience 132:591–603. https://doi.org/10.1016/j.neuroscience.2004.12.034
Chen J, Li CR, Yang H, Liu J, Zhang T, Jiao SS, Wang YJ, Xu ZQ (2016) proBDNF attenuates hippocampal neurogenesis and induces learning and memory deficits in aged mice. Neurotox Res 29:47–53. https://doi.org/10.1007/s12640-015-9568-2
Puig B, Brenna S, Magnus T (2018) Molecular communication of a dying neuron in stroke. Int J Mol Sci 19(9):2834. https://doi.org/10.3390/ijms19092834
Yuki D, Sugiura Y, Zaima N, Akatsu H, Takei S, Yao I, Maesako M, Kinoshita A et al (2014) DHA-PC and PSD-95 decrease after loss of synaptophysin and before neuronal loss in patients with Alzheimer’s disease. Sci Rep 4. https://doi.org/10.1038/srep07130
Decker H, Jürgensen S, Adrover MF, Brito-Moreira J, Bomfim TR, Klein WL, Epstein AL, de Felice FG et al (2010) N-methyl-d-aspartate receptors are required for synaptic targeting of Alzheimer’s toxic amyloid-β peptide oligomers. J Neurochem 115:1520–1529. https://doi.org/10.1111/j.1471-4159.2010.07058.x
Bernardi A, Frozza RL, Meneghetti A et al (2012) Indomethacin-loaded lipid-core nanocapsules reduce the damage triggered by Aβ1-42 in Alzheimer’s disease models. Int J Nanomedicine. https://doi.org/10.2147/IJN.S35333
Gutierrez-Vargas JA, Muñoz-Manco JI, Garcia-Segura LM, Cardona-Gómez GP (2014) GluN2B N-methyl-D-aspartic acid receptor subunit mediates atorvastatin-induced neuroprotection after focal cerebral ischemia. J Neurosci Res 92:1529–1548. https://doi.org/10.1002/jnr.23426
Aluise CD, Robinson RA, Beckett TL et al (2010) Preclinical Alzheimer disease: brain oxidative stress, abeta peptide and proteomics. Neurobiol Dis 39:221–228. https://doi.org/10.1016/j.nbd.2010.04.011
Sultana R, Mecocci P, Mangialasche F, Cecchetti R, Baglioni M, Butterfield DA (2011) Increased protein and lipid oxidative damage in mitochondria isolated from lymphocytes from patients with Alzheimer’s disease: insights into the role of oxidative stress in Alzheimer’s disease and initial investigations into a potential biomarker for this. J Alzheimers Dis 24:77–84. https://doi.org/10.3233/JAD-2011-101425
Barone E, Di Domenico F, Butterfield DA (2014) Statins more than cholesterol lowering agents in Alzheimer disease: their pleiotropic functions as potential therapeutic targets. Biochem Pharmacol 88:605–616
Kurata T, Miyazaki K, Morimoto N, Kawai H, Ohta Y, Ikeda Y, Abe K (2013) Atorvastatin and pitavastatin reduce oxidative stress and improve IR/LDL-R signals in Alzheimer’s disease. Neurol Res 35:193–205. https://doi.org/10.1179/1743132812Y.0000000127
Kann O, Kovács R (2007) Mitochondria and neuronal activity. Am J Physiol Cell Physiol 292:C641–C657. https://doi.org/10.1152/ajpcell.00222.2006
Gu XM, Huang HC, Jiang ZF (2012) Mitochondrial dysfunction and cellular metabolic deficiency in Alzheimer’s disease. Neurosci Bull 28:631–640
Hroudová J, Singh N, Fišar Z, Ghosh KK (2016) Progress in drug development for Alzheimer’s disease: an overview in relation to mitochondrial energy metabolism. Eur J Med Chem 121:774–784
Parks JK, Smith TS, Trimmer PA, Bennett JP Jr, Parker WD Jr (2001) Neurotoxic Aβ peptides increase oxidative stress in vivo through NMDA-receptor and nitric-oxide-synthase mechanisms, and inhibit complex IV activity and induce a mitochondrial permeability transition in vitro. J Neurochem 76:1050–1056. https://doi.org/10.1046/j.1471-4159.2001.00112.x
Yao J, Irwin RW, Zhao L, Nilsen J, Hamilton RT, Brinton RD (2009) Mitochondrial bioenergetic deficit precedes Alzheimer’s pathology in female mouse model of Alzheimer’s disease. Proc Natl Acad Sci U S A 106:14670–14675. https://doi.org/10.1073/pnas.0903563106
Pesta D, Gnaiger E (2012) High-resolution respirometry: OXPHOS protocols for human cells and permeabilized fibers from small biopsies of human muscle. Methods Mol Biol 810:25–58. https://doi.org/10.1007/978-1-61779-382-0_3
Herbst EAF, Holloway GP (2015) Permeabilization of brain tissue in situ enables multiregion analysis of mitochondrial function in a single mouse brain. J Physiol 593:787–801. https://doi.org/10.1113/jphysiol.2014.285379
Makrecka-Kuka M, Krumschnabel G, Gnaiger E (2015) High-resolution respirometry for simultaneous measurement of oxygen and hydrogen peroxide fluxes in permeabilized cells, tissue homogenate and isolated mitochondria. Biomolecules 5:1319–1338. https://doi.org/10.3390/biom5031319
Dias C, Barbosa RM, Laranjinha J, Ledo A (2014) Evaluation of mitochondrial function in the CNS of rodent models of Alzheimer’s disease - high resolution respirometry applied to acute hippocampal slices. Free Radic Biol Med 75:S37. https://doi.org/10.1016/j.freeradbiomed.2014.10.780
Bouitbir J, Charles AL, Echaniz-Laguna A, Kindo M, Daussin F, Auwerx J, Piquard F, Geny B et al (2012) Opposite effects of statins on mitochondria of cardiac and skeletal muscles: a “mitohormesis” mechanism involving reactive oxygen species and PGC-1. Eur Heart J 33:1397–1407. https://doi.org/10.1093/eurheartj/ehr224
Yadava N, Nicholls DG (2007) Spare respiratory capacity rather than oxidative stress regulates glutamate excitotoxicity after partial respiratory inhibition of mitochondrial complex I with rotenone. J Neurosci 27:7310–7317. https://doi.org/10.1523/JNEUROSCI.0212-07.2007
Desler C, Hansen TL, Frederiksen JB, Marcker ML, Singh KK, Juel Rasmussen L (2012) Is there a link between mitochondrial reserve respiratory capacity and aging? J Aging Res 2012:1–9
Nicholls DG (2008) Oxidative stress and energy crises in neuronal dysfunction. In: Annals of the New York Academy of Sciences, pp. 53–60
Parihar A, Parihar MS, Zenebe WJ, Ghafourifar P (2012) Statins lower calcium-induced oxidative stress in isolated mitochondria. Hum Exp Toxicol 31:355–363. https://doi.org/10.1177/0960327111429141
Zhao Z, Cui W, Zhang H, Gao H, Li X, Wang Y, Hu H, Li B (2015) Pre-treatment of a single high-dose of atorvastatin provided cardioprotection in different ischaemia/reperfusion models via activating mitochondrial KATP channel. Eur J Pharmacol 751:89–98. https://doi.org/10.1016/j.ejphar.2015.01.036
Apostolopoulou M, Corsini A, Roden M (2015) The role of mitochondria in statin-induced myopathy. Eur J Clin Investig 45:745–754. https://doi.org/10.1111/eci.12461
Martin SB, Cenini G, Barone E, Dowling ALS, Mancuso C, Butterfield DA, Murphy MP, Head E (2011) Coenzyme Q10 and cognition in atorvastatin treated dogs. Neurosci Lett 501:92–95. https://doi.org/10.1016/j.neulet.2011.06.054
Funding
This research is supported by grants from the Brazilian funding agencies: FAPESC (Fundação de Amparo à Pesquisa e Inovação do Estado de Santa Catarina) and CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico) – INCT for Excitotoxicity and Neuroprotection; Universal 401065/2014-6; CNPq Productivity Fellowship. G.M. is recipient of post-doctoral fellowship from CNPq (154859/2018-4), and W.C.M. was recipient of a PhD fellowship from CAPES.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Experiments followed the “Principles of Laboratory Animal Care” (NIH 2011) and approved by the Ethic Committee on Animal Use of the Federal University of Santa Catarina (CEUA/UFSC PP00955).
Disclosures
The financial support agencies had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mancini, G., Martins, W.C., de Oliveira, J. et al. Atorvastatin Improves Mitochondrial Function and Prevents Oxidative Stress in Hippocampus Following Amyloid-β1–40 Intracerebroventricular Administration in Mice. Mol Neurobiol 57, 4187–4201 (2020). https://doi.org/10.1007/s12035-020-02026-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-020-02026-w