Abstract
Background
Critical closing pressure (CrCP) and resistance-area product (RAP) have been conceived as compasses to optimize cerebral perfusion pressure (CPP) and monitor cerebrovascular resistance, respectively. However, for patients with acute brain injury (ABI), the impact of intracranial pressure (ICP) variability on these variables is poorly understood. The present study evaluates the effects of a controlled ICP variation on CrCP and RAP among patients with ABI.
Methods
Consecutive neurocritical patients with ICP monitoring were included along with transcranial Doppler and invasive arterial blood pressure monitoring. Internal jugular veins compression was performed for 60 s for the elevation of intracranial blood volume and ICP. Patients were separated in groups according to previous intracranial hypertension severity, with either no skull opening (Sk1), neurosurgical mass lesions evacuation, or decompressive craniectomy (DC) (patients with DC [Sk3]).
Results
Among 98 included patients, the correlation between change (Δ) in ICP and the corresponding ΔCrCP was strong (group Sk1 r = 0.643 [p = 0.0007], group with neurosurgical mass lesions evacuation r = 0.732 [p < 0.0001], and group Sk3 r = 0.580 [p = 0.003], respectively). Patients from group Sk3 presented a significantly higher ΔRAP (p = 0.005); however, for this group, a higher response in mean arterial pressure (change in mean arterial pressure p = 0.034) was observed. Exclusively, group Sk1 disclosed reduction in ICP before internal jugular veins compression withholding.
Conclusions
This study elucidates that CrCP reliably changes in accordance with ICP, being useful to indicate ideal CPP in neurocritical settings. In the early days after DC, cerebrovascular resistance seems to remain elevated, despite exacerbated arterial blood pressure responses in efforts to maintain CPP stable. Patients with ABI with no need of surgical procedures appear to remain with more effective ICP compensatory mechanisms when compared with those who underwent neurosurgical interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The interaction between the brain tissue, the cerebrospinal fluid (CSF), and the intracranial blood volume, inside an almost inexpansible skull [1], are the determinants of the intracranial pressure (ICP) [2]. ICP is the driving force that, in combination with the brain vascular network reactivity, especially to arterial pressure and CO2 changes, regulate cerebrovascular resistance (CVR) [3]. It is known that the counterforce between mean arterial blood pressure (MAP) and mean ICP indicates the resulting pressure with which the brain tissue will be perfused, known as cerebral perfusion pressure (CPP) [4]. In the case of acute brain injury (ABI), this relationship may not remain as accurate as for healthy study participants because of cerebrovascular autoregulation (CA) impairment [5, 6].
Acute brain damages related to traumatic brain injury, subarachnoid hemorrhage, and both hemorrhagic or ischemic strokes lead to either diffuse or focal injuries that rationally would conduce to a nonhomogeneous compromise of CPP, challenging the veracity of CPP remaining exclusively on the interactions of MAP and ICP [7]. Furthermore, severely ill patients receive arterial blood pressure (ABP) monitoring derived from a brachial arterial line that may overestimate CPP by up to 40 mm Hg, as central arteries handle lower resistance and pressures than peripheral arteries [8,9,10].
Therefore, assessment of cerebral hemodynamics is crucial for the neurocritical patient because ignoring it may lead to ventilatory, volemic, and pressure mismanagement [11]. Transcranial Doppler (TCD) is one of the most useful tools that can be employed at the bedside to assess cerebral hemodynamics by means of measurements of cerebral blood velocities (CBvs). Despite its excellent temporal resolution and usefulness to perform a number of critical diagnoses, the potential of TCD could be extended even further by providing beat-to-beat estimates of critical closing pressure (CrCP), the value of MAP with which capillary arteries blood flow stops [7, 12] and resistance-area product (RAP) [13, 14]. CrCP indicates the MAP value where cerebral blood flow reaches zero, which has been consistently shown to be well above 0 mm Hg in the cerebral circulation [7, 15]. RAP represents the slope of the instantaneous pressure–velocity relationship for each cardiac cycle [16, 17]. Although it could be seen as an alternative estimation of the CVR, the analogy is not entirely rigorous due to the presence of CrCP [16]. Because the brain capillaries and venules are more easily collapsible than the large vessels, not being observed in conventional tomographies and TCD examinations, CrCP and RAP have the potential to transmit more precise information about the impact of ICP over the microcirculation [18].
It is important to highlight that the brain is located within a rigid skull structure known as a fragile environment for changes in pressures as complications following ABI. Hence, the present study tests the hypothesis that changes in CrCP and RAP are strongly associated with changes in ICP in patients with ABI.
Methods
This is a single center, prospective, observational study performed at Hospital das Clínicas, São Paulo University, Brazil. The study protocol was approved by the local Ethics Committee, in May/23/2017 (REB register 66721217.0.0000.0068) and registered under number NCT03144219 (available at ClinicalTrials.gov). All methods were performed in accordance with the relevant guidelines and regulations, and informed consent was obtained from all legally authorized representatives or next of kin instead of the patients because of illness severity.
Participants and Protocol
The inclusion criteria were patients with a diagnosis of ABI within 5 days of hospital admission submitted to ICP monitoring according to the guidelines of the Brain Trauma Foundation for patients with traumatic brain injury and tomographic evaluation in the case of nontraumatic patients. Exclusion criteria were absence of TCD acoustic windows, neurological examination indicative of brain death, and absence of informed consent. Computed tomography (CT) scans, performed within 24 h prior or posterior to inclusion, were assessed to separate patients in groups according to injury severity, corresponding to the following: no skull opening group (Sk1), surgical mass evacuation group (Sk2), and primary decompressive craniectomy (DC) group (Sk3). Decision for surgical management was performed according to the local institutional neurosurgical guidelines. Nevertheless, surgical management was based either on the presence of mass lesions greater than 30 cm3, midline shift more than 0.5 cm, or imminent risk of herniation in the case of severe brain swelling on admission CT scans. Clinical and laboratory variables were collected at the day of study inclusion.
Physiological Measurements
CBv was recorded bilaterally in the middle cerebral arteries (MCAs) with TCD (Doppler Box; DWL Compumedics, Singen, Germany) equipped with a 2-MHz probe. Recording was initiated after the best MCA signal quality was acquired and without insonation angle variation during the session. Intraventricular ICP was measured with the Neurovent monitoring system using a solid-state transducer (Raumedic®, Munchberg, Germany). ABP was recorded invasively with a radial artery catheter. The pressure transducer was leveled and zeroed to the intersection of the anterior axillary line and the fifth intercostal space. End-tidal CO2 (EtCO2) was measured continuously with an infrared capnograph (Dixtal, DX 1265 EtCO2; Capnogard, Manaus, Brazil). Prior to data collection, an ultrasound examination was performed to discard significant intracranial stenosis [19]. Monitoring was performed for 10 min at rest; at minute 7, an ultrasound guided (Sonosite Micromaxx 13 MHz, USA) sudden manual bilateral internal jugular veins compression (IJVC) was performed for 60 s. The U.S. guidance was used to standardize the compression technique for all patients and to ensure no compression of the carotid arteries. For patients with intracranial hypertension, the IJVC was precluded or aborted in the case of dampened CBv verified prior or during the maneuver [20]. Continuous and simultaneous measurements of CBv, ABP, and ICP were integrated by using the analog-to-digital converter of the Doppler Box at 100 samples/s and stored for off-line editing and analysis.
Data Editing
Beat-to-beat data were analyzed by using in-house custom software written in Fortran. Continuous recordings were visually inspected and narrow artifacts (< 100 ms) were removed by linear interpolation. Spikes in the CBv channels were removed with a median filter and all signals were low-pass filtered with a zero-phase eighth-order Butterworth filter with a cut-off frequency of 20 Hz. The beginning and end of each cardiac cycle was detected in the ABP signal, visually checked, and used to obtain beat-to-beat values of heart rate, MAP, mean CBv, and ICP. The instantaneous relationship between ABP and CBv was used to estimate CrCP and RAP for each cardiac cycle using the first harmonic method [7]. Beat-to-beat data were spline interpolated and resampled at 5 Hz to produce signals with a uniform time base.
Data Analysis
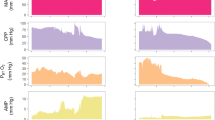
The resampled time-series of ICP was visually inspected, and the beginning of compression was marked. All recorded variables were then synchronized with the instant of compression placed at time = 60 s within a 3-min data window (Fig. 1), and the population coherent average and standard deviation were obtained for each variable (MAP, ICP, CPP, CBv, CrCP, and RAP) for each of the skull condition groups. Patients of any age and sex were included, from children to older people, although their influence on results was analyzed separately. Baseline values were calculated as the mean for the first 60 s, before the beginning of compression. Mean values calculated for the first 30 s of compression were used with baseline values to obtain the change (Δ) in each variable due to compression.
Population average of cerebral hemodynamic parameters following temporary compression of the internal jugular vein in patients with traumatic brain injury. The vertical black arrow marks the beginning of compression. a Mean arterial blood pressure (MAP); b cerebral blood velocity; c intracranial pressure (ICP), with notably spontaneous ICP lowering after 20 s of IJVC (interval between red arrows) exclusively for group Sk1; d critical closing pressure (CrCP); e cerebral perfusion pressure (CPP) (CPP = MAP − ICP); and f resistance-area product (RAP). Representation corresponds to group Sk1 (undamaged skull, continuous line, n = 23), group Sk2 (craniotomy, dotted line, n = 35), and group Sk3 (decompressive craniectomy, dashed line, n = 22). The error bars represent ± 1 SE at the time of occurrence. BP, blood pressure; CBFV, cerebral blood flow velocity; IJVC, internal jugular veins compression; SE, standard error of the mean
Statistical Analysis
Parameter distributions were expressed as mean ± standard deviation. The Shapiro–Wilk W test was applied for normality determination. Student’s t test was used for pairwise comparisons and one-way analysis of variance for the effects of skull condition. In the case of absence of interhemispherical differences, the parameters were averaged. Pearson correlation coefficient and linear regression analysis were used to assess associations between changes in parameters, due to IJVC. Differences between correlation coefficients were tested after log transformation. The General Linear Model was used to test for the effect of skull condition on the slopes of linear regressions. A value of p < 0.05 was adopted to represent statistical significance. Statistical analysis was performed with STATISTICA (Statsoft Inc., Tulsa, OK).
Results
We report the inclusion of 98 eligible patients admitted between August 2017 and May 2020. ICP recordings were of poor quality for nine patients. Data of other four patients were lost, yielding a final sample of 85 patients for analyses. Sixteen patients (19%) had intracranial hypertension (baseline ICP > 20 mm Hg). Right and left hemisphere values of CBv, CrCP, and RAP were averaged following pairwise testing. Table 1 presents patient characteristics classified according to the determined groups. ICP was higher (p = 0.025), and heart rate was lower (p = 0.045) for the group Sk3, but all other variables did not show any significant differences due to skull status.
Effects of Internal Jugular Veins Compression
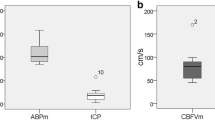
IJVC led to an increase in ICP and CrCP with a drop in CBv and CPP in all groups. RAP did not have significant changes for groups Sk1 and Sk2, but for group Sk3 there was a marked increase of this parameter. Likewise, MAP response was also remarkable in this group (Fig. 1). The response to compression was not uniform and varied according to injury severity (Table 2). With compression, ΔMAP, ΔCPP, ΔCrCP, and ΔRAP were different between groups, but ΔICP was only borderline (p = 0.052). On the other hand, following compression, there was a very strong linear relationship between ΔICP and the corresponding ΔCrCP (Fig. 2), with correlation coefficients of r = 0.643 (p = 0.0007), r = 0.732 (p < 0.0001), and r = 0.580 (p = 0.003) for Sk1, Sk2, and Sk3, respectively. General Linear Model analysis indicated that the three slopes in Fig. 2d were significantly different (p = 0.041). Tukey’s post hoc analysis showed differences in slope between Sk3 and both Sk1 (p = 0.00012) and Sk2 (p = 0.0066). Considering the entire sample (n = 85), a strong relationship between absolute values of CrCP and ICP was observed, either before (p = 0.0007) or after (p = 0.00006) IJVC, as expressed by Pearson’s correlation coefficient.
Change in critical closing pressure (CrCP) as a function of the change in intracranial pressure (ICP) resulting from temporary compression of the internal jugular vein. Linear regression lines with raw data correspond to patients with a undamaged skull (circles, r = 0.643, p = 0.0007), b craniotomy (open squares, r = 0.762, p < 0.0001), and c craniectomy (crosses, r = 0.580, p = 0.003). d Comparison of regression lines corresponding to undamaged skull (dashed line), craniotomies (dotted line), and craniectomy (solid line)
During IJVC, ICP elevation was noted for patients belonging to group Sk1, with the peak of mean ICP values approximately at 20 s of compression onset, followed by a ponderous decrease toward the end of compression. Moreover, after IJVC release, ICP remained lower than baseline for approximately 30 s (Fig. 1c). Similar behavior was not verified for groups Sk2 and Sk3.
Focal Injury
Subanalysis of patients with a clear tomographic focal injury was performed (n = 37). No significant differences were observed for the comparison between injured and noninjured hemispheres for all parameters variations (ΔCBv, ΔCrCP, and ΔRAP) during IJVC (Fig. 3 and Sup. Table 1).
Population average (n = 37) of cerebral hemodynamic parameters following temporary compression of the internal jugular vein in patients with unilateral traumatic brain injury. The vertical arrow marks the beginning of compression. a Mean arterial blood pressure (MABP); b cerebral blood flow velocity (CBFV); c intracranial pressure (ICP); d critical closing pressure (CrCP); e cerebral perfusion pressure (CPP) (CPP = MABP − ICP); and f resistance-area product (RAP). Continuous line indicates measurements from the affected hemisphere, dashed line from the nonaffected hemisphere. The error bars represent ± 1 SE at the time of occurrence. SE, standard error of the mean
Effects of Age
For the parameters in Table 1, age was only correlated with ICP (r = − 0.21, p = 0.048) and RAP (r = 0.40, p = 0.00016). No significant correlations with age were observed for any of the parameters in Table 2. The potential interference of age on the main results of the study was also assessed by removing study participants under 18-years-old and repeating the analyses for the adult study participants only. Overall, the results described previously remained the same. The linear regressions between ΔCrCP and ΔICP were not altered, with similar correlation coefficient values and a significant difference between linear regression slopes (p = 0.028). For the parameters in Table 2, only ΔHR changed by becoming significant (p = 0.028). All other parameters remained significant or nonsignificant as in Table 2.
Discussion
The present study has indicated that the cerebral hemodynamic responses following ICP variations can behave differently among patients in the early stages after ABI, according to the severity of these brain injuries. This was markedly observed among patients who presented with refractory raised ICP and underwent DC. To our knowledge, changes in TCD-derived CrCP and RAP using controlled ICP variations have not been previously reported in this population, eliciting a better understanding of the hemodynamic consequences of ABI. Of considerable relevance, the strong linear association between the changes in CrCP and ICP should stimulate further advances in noninvasive methods for assessment of cerebrovascular function (Fig. 4).
Representative changes in cerebral hemodynamic parameters in a 41-year-old male patient with right traumatic craniotomy for hematoma evacuation. The vertical arrow marks the beginning of jugular veins compression. a Mean arterial blood pressure (MABP); b cerebral blood flow velocity (CBFV); c intracranial pressure (ICP); d critical closing pressure (CrCP); e cerebral perfusion pressure (CPP = MABP − ICP); and f resistance-area product (RAP). Continuous line indicates measurements from the right hemisphere, dashed line from the left hemisphere. ICP was high at the baseline (~ 28 mm Hg) but positively compensated with MABP elevation during compression, leading CPP to not drop lower than 55 mm Hg. CBFV dropped bilaterally but remained under standard values. CrCP elevation was uniform for both hemispheres, whereas RAP elevation was sensitive for the affected (right) hemisphere. BP, blood pressure
Relevance of CrCP and RAP
In the literature, there is an index also called RAP, however, it is derived from ICP pulse amplitude and ICP mean values. This index is estimated for the assessment of intracranial compensatory reserve [21, 22]. Differently, the RAP parameter used in the current study expressed the concept of CVR, considering that blood velocities assessed with TCD suffer the impact of changes on the vessels cross-sectional area. Therefore, the present study evaluated the impact of induced ICP elevation over small vessels and capillary resistance and the contribution of MAP response to keep CPP stable. It is possible to conclude that cerebrovascular physiology is considerably altered after ABI. However, more work is needed to fully understand the causal pathways involved.
Practical Applications
Several investigators have proposed that CrCP could replace ICP in noninvasive estimates of CPP [7, 15, 23,24,25,26]. Highly significant linear correlations between CrCP and ICP were reported by Thees et al. [15] (r = 0.91) in 70 patients and by Czosnyka et al. [24] (r = 0.51) in 98 patients with head injury. In our study, we confirmed this strong association between CrCP and ICP when the entire sample was pooled into the same linear regression, as well as for all three distinct groups separately.
The possibility of obtaining optimal CPP estimation, instead of tethering to fixed ICP thresholds [6, 7, 27], is supported by the close similarity of temporal patterns observed for the ICP and CrCP changes following IJVC and for mathematical modeling showing a linear dependence between CrCP and ICP [7]. Interesting, for Sk1, the slope of the linear regression between ΔCrCP and ΔICP is in good approximation to the slope indicated by mathematical modeling [7].
This reinforces the idea that CrCP could be used as a noninvasive surrogate of ICP. However, it should be emphasized that CrCP is influenced by CO2 changes [18, 28,29,30,31], whereas RAP could be more sensitive to transmural pressure changes in large arteries and arterioles, reflecting their specific myogenic responses to changes in ABP [7, 16, 18, 29, 32,33,34,35]. Our results could not entirely exclude some influence of CO2 on CrCP findings, which strengthen the importance of very close monitoring of this variable.
From this perspective, cerebral hemodynamic responses of small arterioles and capillaries can be assessed according to ABP, ICP, pCO2, and pO2 changes. The information provided by CrCP and RAP can add to the beat-to-beat values of mean CBv obtained from TCD and the associations that we and others have reported warrant further investigation in larger studies of ABI, as well as in other cerebrovascular conditions.
Compensatory Mechanisms
After severe trauma and surgical manipulation of the skull, the loss of natural brain architecture may lead to CSF [36] and venous blood [37, 38] transit impairment. Therefore, the buffering mechanisms of the compensatory reserve, such as CSF displacement toward cervical cisterns and large venous sinuses emptying their volumes to extracranial veins are limited [22, 39]. In our results, this idea was evident because of the distinct ICP behavior between uninjured/not manipulated skulls and the other groups, with ICP beginning to decrease after 20 s of IJVC (Fig. 1c). Otherwise, the plateau during the 60 s of IJVC in cases of craniectomies and craniotomies was sustained.
Recent studies have shown that craniectomized patients may present substantial alterations in intracranial compliance (ICC) (ICC = intracranial volume/pressure) [40], despite consistent drops in ICP values. After DC, we expect an increase in cerebral blood perfusion, possibly due to a lower influence of the rigid cranial vault [38, 41, 42]. On the other hand, TCD and CT perfusion studies reported a wide variety of hemodynamic changes after DC [43,44,45], with normalization of cerebral blood transit not being sufficient for the determination of outcomes in ABI [46, 47].
Our data demonstrated a very close relationship of RAP and MAP in DC group (Table 2), which could indicate the presence of a myogenic response, even with a considerable degree of CA impairment [48], whereas the reduced ΔCrCP could reflect the depressed CA, with less active wall tension resulting from metabolic pathways [49]. Therefore, after DC—despite the ICP control and often the cerebral perfusion increasing due to brain swelling and stretching, as well as the compensatory reserve and CA impairment—ICC may remain compromised [43, 47]. That is, the “war against ICC impairment is not won yet.” This was also observed by Brasil et al. [41] assessing the ICP waveform slopes in the same stage after injury, supported with the fact that brain hemodynamics often improve with cranioplasty [38, 50].
All this reinforces the idea that CA (or cerebral blood flow regulation) is not an all-or-nothing phenomenon, and the decomposition of CVR in two variables (CrCP and RAP) would give a more realistic bedside interpretation of the complex changes in cerebral hemodynamics of neurocritical patients. Likewise, these findings also emphasize the importance of not considering CPP strictly determined by the interaction between MAP and ICP in ABI [48, 51, 52] and advise for an individualized approach using parameters more representative of the real changes in brain hemodynamics, such as CrCP and RAP.
Limitations of the Study
The given observations of the present study were supported by the analysis of data extracted from the early stages of ABI in a single monitoring session. It is acknowledged that a cohort study design would increase the possibility to follow-up physiological changes in this population. Our results are derived from MCA blood transit velocity, instead of actual cerebral blood volume or brain perfusion, and this limitation could have affected our results. IJVC increased ICP and this could have caused a reduction in MCA diameter, thus leading to overestimation of the corresponding drop in CBv, as well as small errors in CrCP and RAP. Despite a large range of ages included, our main findings persisted even with the removal of data from patients under 18 years old. Automated and continuous PaCO2 was not registered, although maintained within controlled limits due to mechanical ventilation and did not show significant changes during monitoring sessions; rather, EtCO2 was used as a proxy of changes in arterial CO2 tension.
To maintain the focus of the study on the main hypothesis outlined in the Introduction, we have not explored other interparameter relationships, such as the association between ΔCrCP and ΔRAP. Changes in RAP due to IJVC and its association with corresponding changes in MAP can reflect the status of dynamic CA, which are under investigation and will be reported elsewhere. Finally, TCD measurements were performed exclusively on main distal branches of internal carotid arteries, the MCAs more specifically, not considering disturbances on the posterior fossa.
Conclusions
Critical closing pressure is correlated with ICP variations and may aid in planning therapeutic interventions based on hemodynamic adjustments. An induced mild ICP elevation in the present study did not impact the CPP of craniectomized patients. These patients demonstrated elevated MAP response to ICP variation, despite the persistence of higher CVR, which may be interpreted as a protection mechanism provided by DC. Patients with ABI not submitted to neurosurgical procedures revealed a higher capacity of handling artificial ICP elevation, which may be attributed to less severe injury, appropriate ICC, and efficient compensatory reserve. These observations altogether reinforce the need for multimodal monitoring of the neurocritical patient.
References
Mascarenhas S, Vilela GH, Carlotti C, et al. The new ICP minimally invasive method shows that the Monro-Kellie doctrine is not valid. Acta Neurochir Suppl. 2012;114:117–20.
Cardoso ER, Rowan JO, Galbraith S. Analysis of the cerebrospinal fluid pulse wave in intracranial pressure. J Neurosurg. 1983;59(5):817–21.
Duffin J, Sobczyk O, McKetton L, et al. Cerebrovascular resistance: the basis of cerebrovascular reactivity. Front Neurosci. 2018;12:409.
Hawryluk GWJ, Citerio G, Hutchinson P, et al. Intracranial pressure: current perspectives on physiology and monitoring. Intensive Care Med. 2022;48:1471–81.
Robba C, Citerio G. How I manage intracranial hypertension. Crit Care. 2019;23(1):243.
Rubiano AM, Figaji A, Hawryluk GW. Intracranial pressure management: moving beyond guidelines. Curr Opin Crit Care. 2022;28(2):101–10.
Panerai RB. The critical closing pressure of the cerebral circulation. Med Eng Phys. 2003;25(8):621–32.
Safar ME, Rizzoni D, Blacher J, Muiesan ML, Agabiti-Rosei E. Macro and microvasculature in hypertension: therapeutic aspects. J Hum Hypertens. 2008;22(9):590–5.
McEniery CM, Cockcroft JR, Roman MJ, Franklin SS, Wilkinson IB. Central blood pressure: current evidence and clinical importance. Eur Heart J. 2014;35(26):1719–25.
Ohte N, Saeki T, Miyabe H, et al. Relationship between blood pressure obtained from the upper arm with a cuff-type sphygmomanometer and central blood pressure measured with a catheter-tipped micromanometer. Heart Vessels. 2007;22(6):410–5.
Castro P, Azevedo E, Sorond F. Cerebral autoregulation in stroke. Curr Atheroscler Rep. 2018;20(8):37.
Lopez-Magana JA, Richards HK, Radolovich DK, et al. Critical closing pressure: comparison of three methods. J Cereb Blood Flow Metab. 2009;29(5):987–93.
Czosnyka M, Guazzo E, Whitehouse M, et al. Significance of intracranial pressure waveform analysis after head injury. Acta Neurochir (Wien). 1996;138(5):531–41 (discussion 41-2).
Panerai RB, Kerins V, Fan L, et al. Association between dynamic cerebral autoregulation and mortality in severe head injury. Br J Neurosurg. 2004;18(5):471–9.
Czosnyka M, Smielewski P, Piechnik S, et al. Critical closing pressure in cerebrovascular circulation. J Neurol Neurosurg Psych. 1999;66:606–11.
Panerai RB, Haunton VJ, Llwyd O, et al. Cerebral critical closing pressure and resistance-area product: the influence of dynamic cerebral autoregulation, age and sex. J Cereb Blood Flow Metab. 2021;41(9):2456–69.
Robertson AD, Edgell H, Hughson RL. Assessing cerebrovascular autoregulation from critical closing pressure and resistance area product during upright posture in aging and hypertension. Am J Physiol Heart Circ Physiol. 2014;307(2):H124–33.
Panerai RB, Minhas JS, Llwyd O, et al. The critical closing pressure contribution to dynamic cerebral autoregulation in humans: influence of PaCO2. J Physiol. 2020;598:1–13.
Alexandrov AV, Sloan MA, Tegeler CH, et al. Practice standards for transcranial Doppler (TCD) ultrasound. Part II. Clinical indications and expected outcomes. J Neuroimaging. 2012;22(3):215–24.
Brasil S, Solla DJF, Nogueira RdC, et al. A novel noninvasive technique for intracranial pressure waveform monitoring in critical care. J Personal Med. 2021;11(12):1302.
Zeiler FA, Kim D-J, Cabeleira M, et al. Impaired cerebral compensatory reserve is associated with admission imaging characteristics of diffuse insult in traumatic brain injury. Acta Neurochir. 2018;160(12):2277–87.
Kim DJ, Czosnyka Z, Keong N, et al. Index of cerebrospinal compensatory reserve in hydrocephalus. Neurosurgery. 2009;64(3):494–501 (discussion-2).
Buhre W, Heinzel FR, Grund S, Sonntag H, Weyland A. Extrapolation to zero-flow pressure in cerebral arteries to estimate intracranial pressure. Br J Anaest. 2003;90:291–5.
Thees C, Scholz M, Schaller C, et al. Relationship between intracranial pressure and critical closing pressure in patients with neurotrauma. Anesthesiology. 2002;96:595–9.
Varsos GV, Richards H, Kasprowicz M, et al. Critical closing pressure determined with a model of cerebrovascular impedance. J Cereb Blood Flow Metab. 2013;33:235–43.
Weyland A, Buhre W, Grund S, et al. Cerebrovascular tone rather than intracranial pressure determines the effective downstream pressure of the cerebral circulation in the absence of intracranial hypertension. J Neurosurg Anest. 2000;12:210–6.
Wijdicks EFM. 10 or 15 or 20 or 40 mmHg? What is increased intracranial pressure and who said so? Neurocrit Care. 2022;36(3):1022–6.
Panerai RB, Deverson ST, Mahony P, Hayes P, Evans DH. Effect of CO2on dynamic cerebral autoregulation measurement. Physiol Meas. 1999;20(3):265–75.
Panerai RB, Eyre M, Potter JF. Multivariate modeling of cognitive-motor stimulation on neurovascular coupling: transcranial Doppler used to characterize myogenic and metabolic influences. Am J Physiol Regul Integr Comp Physiol. 2012;303:R395–407.
Dineen NE, Brodie FG, Robinson TG, Panerai RB. Continuous estimates of dynamic cerebral autoregulation during transient hypocapnia and hypercapnia. J Appl Physiol (1985). 2010;108(3):604–13.
Hancock SM, Mahajan RP, Athanassiou L. Noninvasive estimation of cerebral perfusion pressure and zero flow pressure in healthy volunteers: the effects of changes in end-tidal carbon dioxide. Anesth Analg. 2003;96(3):847–51.
Panerai RB, Moody M, Eames PJ, Potter JF. Cerebral blood flow velocity during mental activation: Interpretation with different models of the passive pressure-velocity relationship. J Appl Physiol. 2005;99:2352–62.
Salinet ASM, Robinson TG, Panerai RB. Cerebral blood flow response to neural activation after acute ischemic stroke: a failure of myogenic autoregulation? J Neurol. 2013;260:2588–95.
van Veen TR, Panerai RB, Haeri S, et al. Cerebral autoregulation in normal pregnancy and preeclampsia. Obstet Gynecol. 2013;122:1064–9.
Nogueira RC, Bor-Seng-Shu E, Santos MR, et al. Dynamic cerebral autoregulation changes during sub-maximal handgrip maneuver. PLoS ONE. 2013;8(8):e70821.
Cherian I, Beltran M, Landi A, et al. Introducing the concept of “CSF-shift edema” in traumatic brain injury. J Neurosci Res. 2018;96(4):744–52.
Zheng S, Mu S, Li J, et al. Cerebral venous hemodynamic responses in a mouse model of traumatic brain injury. Brain Res. 2022;1792:148014.
Carmelo A, Ficola A, Fravolini ML, et al. ICP and CBF regulation: effect of the decompressive craniectomy. Acta Neurochir Suppl. 2002;81:109–11.
Zeiler FA, Kim DJ, Cabeleira M, et al. Impaired cerebral compensatory reserve is associated with admission imaging characteristics of diffuse insult in traumatic brain injury. Acta Neurochir (Wien). 2018;160(12):2277–87.
Ocamoto GN, Russo TL, Mendes Zambetta R, et al. Intracranial compliance concepts and assessment: a scoping review. Front Neurol. 2021;12:756112.
Brasil S, Solla DJF, Nogueira RC, et al. Intracranial compliance assessed by intracranial pressure pulse waveform. Brain Sci. 2021;11(971):1–11.
Wilson MH. Monro-Kellie 2.0: the dynamic vascular and venous pathophysiological components of intracranial pressure. J Cereb Blood Flow Metab. 2016;36:1338–50.
Bor-Seng-Shu E, de-Lima-Oliveira M, Nogueira RC, et al. Decompressive craniectomy for traumatic brain injury: postoperative TCD cerebral hemodynamic evaluation. Front Neurol. 2019;10:354.
Vedantam A, Robertson CS, Gopinath SP. Quantitative cerebral blood flow using xenon-enhanced CT after decompressive craniectomy in traumatic brain injury. J Neurosurg. 2018;129(1):241–6.
Amorim RL, de Andrade AF, Gattas GS, et al. Improved hemodynamic parameters in middle cerebral artery infarction after decompressive craniectomy. Stroke. 2014;45(5):1375–80.
Brasil S, Paiva WS, de Carvalho Nogueira R, Macedo Salinet A, Teixeira MJ. Decompressive craniectomy in TBI: What is beyond static evaluations in terms of prognosis? J Neurosurg. 2018;129(3):845–7.
Bor-Seng-Shu E, Figueiredo EG, Fonoff ET, et al. Decompressive craniectomy and head injury: brain morphometry, ICP, cerebral hemodynamics, cerebral microvascular reactivity, and neurochemistry. Neurosurg Rev. 2013;36(3):361–70.
Brasil S, Nogueira RC, Salinet ASM, et al. The contribution of intracranial pressure to human dynamic cerebral autoregulation after acute brain injury. Am J Physiol Regul Integr Comp Physiol. 2022;34(2):R216-R226. https://doi.org/10.1152/ajpregu.00252.2022
Burton AC. On the physical equilibrium of small blood vessels. Am J Physiol. 1951;164:319–29.
Oliveira AMP, Amorim RLO, Brasil S, et al. Improvement in neurological outcome and brain hemodynamics after late cranioplasty. Acta Neurochir (Wien). 2021;163(10):2931–9.
Bor-Seng-Shu E, Figueiredo EG, Amorim RL, et al. Decompressive craniectomy: a meta-analysis of influences on intracranial pressure and cerebral perfusion pressure in the treatment of traumatic brain injury. J Neurosurg. 2012;117(3):589–96.
Small C, Lucke-Wold B, Patel C, et al. What are we measuring? A refined look at the process of disrupted autoregulation and the limitations of cerebral perfusion pressure in preventing secondary injury after traumatic brain injury. Clin Neurol Neurosurg. 2022;221:107389.
Funding
The present study received no funding.
Author information
Authors and Affiliations
Contributions
SB, RCN, and ASMS conceived and designed the study. RCN provided supervision and training. SB performed measurements and wrote the article. SB and ASMS performed preliminary data analysis. RBP wrote software, performed data analysis, and wrote the article. SB, RCN, ASMS, MHY, MJT, WP, EBSS, and LMSM revised the article. All authors agree to be accountable for all aspects of the work. All persons designated as authors qualify for authorship and all those who qualify for authorship are listed. The data that support the findings of this study are available from the corresponding author upon reasonable request. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval/Informed Consent
The authors confirm compliance with Ethical approval and informed consent for human studies.
Clinical Trial Registration
Trial registration: NCT03144219, Registered 01 May 2017 Retrospectively registered, https://www.clinicaltrials.gov/ct2/show/NCT03144219
ClinicalTrials.gov: NCT03694678.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brasil, S., de Carvalho Nogueira, R., Salinet, Â.S.M. et al. Critical Closing Pressure and Cerebrovascular Resistance Responses to Intracranial Pressure Variations in Neurocritical Patients. Neurocrit Care 39, 399–410 (2023). https://doi.org/10.1007/s12028-023-01691-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-023-01691-8