Abstract
Objectives
The thyroid nodule is one of the most common endocrine system diseases. Risk classification models based on ultrasonic features have been created by multiple professional societies, including the American College of Radiology (ACR), which published the Thyroid Imaging Reporting and Data System (TI-RADS) in 2017. The effect of the size in the diagnostic value of ultrasound remains not well defined. The purposes of our study aims to explore diagnostic value of the ACR TI-RADS on different-sized thyroid nodules.
Methods
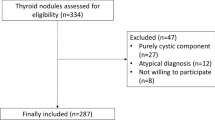
A total of 1183 thyroid nodules were selected from 952 patients with thyroid nodules confirmed by surgical pathology from January 2021 to October 2022. Based on the maximum diameters of the nodules, they were stratified into groups A ( ≤ 10 mm), B ( > 10 mm, < 20 mm) and C ( ≥ 20 mm). The ultrasonic features of the thyroid nodules in each group were evaluated and scored based on ACR TI-RADS, and the receiver operating characteristic curve (ROC) was plotted to determine the optimal cut-off value for the ACR TI-RADS scores and categories in each group. Finally, the diagnostic efficacy of ACR TI-RADS on different-sized thyroid nodules was analyzed.
Results
Among the 1183 thyroid nodules, 340 were benign, 10 were low-risk and 833 were malignant. For the convenience of statistical analysis, low-risk thyroid nodules were classified as malignant in this study. The ACR TI-RADS scores and categorical levels of malignant thyroid nodules in each group were higher than those of benign ones (p < 0.05). The areas under the ROCs (AUCs) plotted based on scores were 0.741, 0.907, and 0.904 respectively in the three groups, and the corresponding optimal cut-off values were > 6 points, > 5 points and > 4 points respectively. While the AUCs of the ACR TI-RADS categories were 0.668, 0.855, and 0.887 respectively in each group, with the optimal cut-off values were all > TR4. Besides, for thyroid nodules of larger sizes, ACR TI-RADS exhibited weaker sensitivity with lower positive prediction value (PPV), but the specificity and negative prediction value (NPV) were both higher, presenting with statistically significant differences (p < 0.05).
Conclusion
For thyroid nodules of different sizes, the diagnostic efficacy of ACR TI-RADS varies as well. The system shows better diagnostic efficacy on thyroid nodules of > 10 mm than on those ≤ 10 mm. Considering the favorable prognosis of thyroid microcarcinoma and the low diagnostic efficacy of ACR TI-RADS on it, the scoring and classification of thyroid micro-nodules can be left out in appropriate cases, so as to avoid the over-diagnosis and over-treatment of thyroid microcarcinoma to a certain extent.








Similar content being viewed by others
References
E.K. Alexander, E.S. Cibas, Diagnosis of thyroid nodules. Lancet Diabetes Endocrinol. 10(7), 533–539 (2022). https://doi.org/10.1016/S2213-8587(22)00101-2
K. Kobaly, C.S. Kim, S.J. Mandel, Contemporary Management of Thyroid Nodules. Annu. Rev. Med. 27(8), 517–528 (2022). https://doi.org/10.1146/annurev-med-042220-015032
M.R. Haymart, Progress and Challenges in Thyroid Cancer Management. Endocr. Pr. 27(12), 1260–1263 (2017). https://doi.org/10.1016/j.eprac.2021.09.006
F.N. Tessler, W.D. Middleton, E.G. Grant, J.K. Hoang, L.L. Berland, S.A. Teefey, J.J. Cronan, M.D. Beland, T.S. Desser, M.C. Frates, L.W. Hammers, U.M. Hamper, J.E. Langer, C.C. Reading, L.M. Scoutt, A.T. Stavros, ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J. Am. Coll. Radio. 14(5), 587–595 (2017). https://doi.org/10.1016/j.jacr.2017.01.046
J.K. Hoang, W.D. Middleton, F.N. Tessler, Update on ACR TI-RADS: Successes, Challenges, and Future Directions, From the AJR Special Series on Radiology Reporting and Data Systems. AJR Am. J. Roentgenol. 216, 570–578 (2021). https://doi.org/10.2214/AJR.20.24608
X. Chen, M. Gao, L. Hu, J. Zhu, S. Zhang, X. Wei, The diagnostic value of the ultrasound gray scale ratio for different sizes of thyroid nodules. Cancer Med. 8(18), 7644–7649 (2019). https://doi.org/10.1002/cam4.2653
O. Mete, B.M. Wenig, Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Overview of the 2022 WHO Classification of Head and Neck Neuroendocrine Neoplasms. Head. Neck Pathol. 16, 123–142 (2022). https://doi.org/10.1007/s12105-022-01435-8
G. Rindi, O. Mete, S. Uccella, O. Basturk, S. La Rosa, L.A.A. Brosens, S. Ezzat, WW. de Herder, DS. Klimstra, M. Papotti, SL. Asa, Overview of the 2022 WHO Classification of Neuroendocrine Neoplasms. Endocr. Pathol. 33(1), 115–154 (2022). https://doi.org/10.1007/s12022-022-09708-2
R.R. Tappouni, J.N. Itri, T.S. McQueen, N. Lalwani, J.J. Ou, ACR TI-RADS: Pitfalls, Solutions, and Future Directions. Radiographics 39(7), 2040–2052 (2019). https://doi.org/10.1148/rg.2019190026
J. Wang, W. Wei, R. Guo, Ultrasonic elastography and conventional ultrasound in the diagnosis of thyroid micro-nodules. Pak. J. Med. Sci. 35(6), 1526–1531 (2019). https://doi.org/10.12669/pjms.35.6.777
Q.L. Li, T. Ma, Z.J. Wang, L. Huang, W. Liu, M. Chen, T. Sang, X.G. Ren, J. Tong, C.L. Cao, J. Dong, J. Li, The value of contrast-enhanced ultrasound for the diagnosis of metastatic cervical lymph nodes of papillary thyroid carcinoma: A systematic review and meta-analysis. J. Clin. Ultrasound 50(1), 60–69 (2022). https://doi.org/10.1002/jcu.23073
X. Tian, Q. Song, F. Xie, L. Ren, Y. Zhang, J. Tang, Y. Zhang, Z. Jin, Y. Zhu, M. Zhang, Y. Luo, Papillary thyroid carcinoma: an ultrasound-based nomogram improves the prediction of lymph node metastases in the central compartment. Eur. Radio. 30(11), 5881–5893 (2020). https://doi.org/10.1007/s00330-020-06906-6
Q. Peng, C. Niu, M. Zhang, Q. Peng, S. Chen, Sonographic Characteristics of Papillary Thyroid Carcinoma with Coexistent Hashimoto’s Thyroiditis: Conventional Ultrasound, Acoustic Radiation Force Impulse Imaging and Contrast-Enhanced Ultrasound. Ultrasound Med. Biol. 45(2), 471–480 (2019). https://doi.org/10.1016/j.ultrasmedbio.2018.10.020
Q. Zhang, L. Liao, Q. Peng, K. Tang, Y. Xu, R. Zhang, M. Liu, C. Niu, Value of Contrast-Enhanced Ultrasound in Differentiating Clinically Atypical Subacute Thyroiditis from Papillary Thyroid Carcinomas. Ultrasound Med. Biol. 47(12), 3384–3392 (2021). https://doi.org/10.1016/j.ultrasmedbio.2021.09.001
L. Yang, H. Zhao, Y. He, X. Zhu, C. Yue, Y. Luo, B. Ma, Contrast-Enhanced Ultrasound in the Differential Diagnosis of Primary Thyroid Lymphoma and Nodular Hashimoto’s Thyroiditis in a Background of Heterogeneous Parenchyma. Front. Oncol. 10, 597975 (2021). https://doi.org/10.3389/fonc.2020.597975
W. Zhao, Q. Kang, F. Qian, K. Li, J. Zhu, B. Ma, Convolutional Neural Network-Based Computer-Assisted Diagnosis of Hashimoto’s Thyroiditis on Ultrasound. J. Clin. Endocrinol. Metab. 107(4), 953–963 (2022). https://doi.org/10.1210/clinem/dgab870
F. Ragusa, P. Fallahi, G. Elia, D. Gonnella, S.R. Paparo, C. Giusti, L.P. Churilov, S.M. Ferrari, A. Antonelli, Hashimotos’ thyroiditis: Epidemiology, pathogenesis, clinic and therapy. Best. Pr. Res Clin. Endocrinol. Metab. 33(6), 101367 (2019). https://doi.org/10.1016/j.beem.2019.101367
F. Magri, S. Chytiris, V. Capelli, M. Gaiti, F. Zerbini, R. Carrara, A. Malovini, M. Rotondi, R. Bellazzi, L. Chiovato, Comparison of elastographic strain index and thyroid fine-needle aspiration cytology in 631 thyroid nodules. J. Clin. Endocrinol. Metab. 98, 4790–4797 (2013). https://doi.org/10.1210/jc.2013-2672
W. Zeng, S. Tan, T.F.J. King, Subacute thyroiditis presenting as a painful suspicious thyroid nodule. Endocrinol. Diabetes Metab. Case Rep. 2022, 21–0135 (2022). https://doi.org/10.1530/EDM-21-0135
C. Cappelli, I. Pirola, E. Gandossi, A.M. Formenti, B. Agosti, M. Castellano, Ultrasound findings of subacute thyroiditis: a single institution retrospective review. Acta Radio. 55(4), 429–433 (2014). https://doi.org/10.1177/0284185113498721
R. Liu, L. Gao, Y. Xia, X. Li, Q. Liao, Y. Jiang, Q. Zhang, C. Chen, L. Zhang, Z. Liang, Y. Jiang, Three ultrasound phenotypes of non-invasive follicular thyroid neoplasm with papillary-like nuclear features proposed for imaging-pathology analysis: single center experience. Gland Surg. 10(1), 307–318 (2021). https://doi.org/10.21037/gs-20-612
K. Holzer, D.K. Bartsch, Struma nodosa [Nodular goiter]. Chirurg 91(9), 712–719 (2020). https://doi.org/10.1007/s00104-020-01218-3. German
Y. Yan, F. Zhang, H. Ge, L. Miao, L. Zhang, Y. Xiong, Q. Fu, H. Liu, Effect of the size of benign thyroid degenerative nodules on ACR TI-RADS categories. J. Med Ultrason (2001). 49(1), 71–76 (2022). https://doi.org/10.1007/s10396-021-01163-6
Q.X. Huang, X.W. Huang, Comments on “Effect of the size of benign thyroid degenerative nodules on ACR TI-RADS categories”. J. Med Ultrason (2001). 49(3), 503–512 (2022). https://doi.org/10.1007/s10396-022-01214-6
W.J. Choi, J.S. Park, K.G. Kim, S.Y. Kim, H.R. Koo, Y.J. Lee, Computerized analysis of calcification of thyroid nodules as visualized by ultrasonography. Eur. J. Radio. 84(10), 1949–1953 (2015). https://doi.org/10.1016/j.ejrad.2015.06.021
C.M. Thomas, S.L. Asa, S. Ezzat, A.M. Sawka, D. Goldstein, Diagnosis and pathologic characteristics of medullary thyroid carcinoma-review of current guidelines. Curr. Oncol. 26(5), 338–344 (2019). https://doi.org/10.3747/co.26.5539
K. Tajiri, M. Hirokawa, A. Suzuki, N. Takada, H. Ota, M. Oshita, M. Fukushima, K. Kobayashi, A. Miyauchi, Can Ultrasound Alone Predict Papillary Thyroid Carcinoma with Desmoid-Type Fibromatosis? A Retrospective Analysis of 13 Cases, Focusing on the Stromal Area. Ultrasound Int. Open 4(2), 39–44 (2018). https://doi.org/10.1055/a-0591-6163
Y. Peng, W. Zhou, W.W. Zhan, S.Y. Xu, Ultrasonographic Assessment of Differential Diagnosis Between Degenerating Cystic Thyroid Nodules and Papillary Thyroid Microcarcinomas. World J. Surg. 41(10), 2538–2544 (2017). https://doi.org/10.1007/s00268-017-4060-1
I. Cengic, D. Tureli, H. Altas, F. Ozden, O. Bugdayci, E. Aribal, Effects of nodule characteristics on sampling number and duration of thyroid fine-needle aspiration biopsy: size does not matter, but cystic degeneration ratio does. Acta. Radio. 58(3), 286–291 (2017). https://doi.org/10.1177/0284185116649797
L. Scappaticcio, M.I. Maiorino, S. Iorio, G. Docimo, M. Longo, A. Grandone, C. Luongo, I. Cozzolino, A. Piccardo, P. Trimboli, E. Miraglia Del Giudice, K. Esposito, G. Bellastella, Exploring the Performance of Ultrasound Risk Stratification Systems in Thyroid Nodules of Pediatric Patients. Cancers (Basel) 13(21), 5304–5312 (2021). https://doi.org/10.3390/cancers13215304
J. Zhou, L. Yin, X. Wei, S. Zhang, Y. Song, B. Luo, J. Li, L. Qian, L. Cui, W. Chen, C. Wen, Y. Peng, Q. Chen, M. Lu, M. Chen, R. Wu, W. Zhou, E. Xue, Y. Li, L. Yang, C. Mi, R. Zhang, G. Wu, G. Du, D. Huang, W. Zhan, Superficial Organ and Vascular Ultrasound Group of the Society of Ultrasound in Medicine of the Chinese Medical Association; Chinese Artificial Intelligence Alliance for Thyroid and Breast Ultrasound. 2020 Chinese guidelines for ultrasound malignancy risk stratification of thyroid nodules: the C-TIRADS. Endocrine 70(2), 256–279 (2020). https://doi.org/10.1007/s12020-020-02441-y
B.R. Haugen, E.K. Alexander, K.C. Bible, G.M. Doherty, S.J. Mandel, Y.E. Nikiforov, F. Pacini, G.W. Randolph, A.M. Sawka, M. Schlumberger, K.G. Schuff, S.I. Sherman, J.A. Sosa, D.L. Steward, R.M. Tuttle, L. Wartofsky, 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26(1), 1–133 (2016). https://doi.org/10.1089/thy.2015.0020
Acknowledgements
The authors would like to thank Home for Researchers editorial team for language editing service.
Author contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by W.M.L., J.M.C., F.Y., C.Y., and X.F.F. Analysis was performed by W.M.L., J.M.C., and X.F.F. The first draft of the manuscript was written by WM L and FY, and the final version was edited by C.Y. and D.X.; All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. W.M.L. and J.M.C. made the equal contribution to this article.
Funding
This work were supported by Maternal and Child Health Promotion Project of Wuxi (FYTG202103) and Project of National Natural Science Foundation of China (82071946).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, W., Chen, J., Ye, F. et al. The diagnostic value of ultrasound on different-sized thyroid nodules based on ACR TI-RADS. Endocrine 82, 569–579 (2023). https://doi.org/10.1007/s12020-023-03438-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03438-z