Abstract
Male infertility along with altered semen parameters have been related to smoking. Smoking-related elevations in serum and seminal lead (Pb) and arsenic (As) may play a role in mediating the toxic effects of smoking on seminogram. This research aims to determine whether smoking has any significant impact on Pb and As levels in the seminal plasma and serum, as well as on the various semen parameters, when compared to nonsmokers. In total, 80 adult males were included: 60 smokers and 20 age-matched nonsmokers. Based on the number of cigarettes smoked/day (CPD), the smokers were categorized into mild (1–10), moderate (11–20), and severe (> 20). The analysis of semen was conducted in accordance with the 2010 WHO laboratory manual. Using an atomic absorption spectrophotometer, Pb and As concentrations in the serum and seminal plasma of all groups were determined. Compared to nonsmokers, smokers had a significantly reduced sperm count, motility, and viability, as well as a larger percentage of aberrant forms (P = 0.001, 0.025, 0.034, 0.002 respectively). Smokers had higher Pb concentrations in their serum and seminal fluid than nonsmokers (P = 0.002, 0.001 respectively). Seminal Pb had a significant negative correlation with sperm count (P = 0.004, r = -0.320). Serum Pb levels were found to positively correlate with seminal Pb levels (P 0.001, r = 0.648), and cigarette smokers had substantially greater seminal As levels than nonsmokers (P = 0.024). Sperm viability was strongly inversely related to seminal As (P = 0.042, r = -0.264). Seminal As levels and aberrant sperm shapes were found to be significantly correlated (P = 0.001, r = 0.414). In smokers, a significant positive relationship between seminal As and seminal Pb was observed. Therefore, semen parameters could be adversely affected by smoking through high levels of Pb and As (P = 0.012, r = 0.298).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Smoking is one of the most common behaviors among men, especially those of reproductive age [1]. Cigarette smoking can have toxic effects on spermatogenesis either directly or indirectly [2]. Tobacco smoke contains over 4,000 compounds, some of which are heavy metals like Pb and As [3].
Pb, a versatile and ubiquitous metal, has been used since prehistoric times. It is now ubiquitous and has been mobilized in the environment [4]. Multisystemic, deleterious effects of chronic Pb exposure occur via a variety of biochemical processes. Heavy Pb exposure has been related to various health problems, such as anemia, hypertension, brain and kidney damage, and premature death in both adults and children. Also, researchers discovered that male fertility declines with prolonged exposure to Pb [5].
Pb accumulation was observed in the testis and epididymis as the concentration increased, accompanied by a decrease in the activities of alkaline phosphate and Na + /K + -ATPase, both of which are known to be involved in spermatogenesis and spermiogenesis, respectively. Seminiferous tubule lumen accumulation of immature cells, complete cessation of spermatogenesis, and epididymal basement membrane injury were observed as histological alterations induced by higher concentrations of Pb [6]. An overproduction of inhibin B has been related to Sertoli cell dysfunction caused by high levels of Pb exposure, which may explain the decreased levels of follicular stimulating hormone (FSH) [7].
Toxic forms of the element As can be found throughout nature. Gastroenteritis, neurological symptoms, vascular alterations, diabetes, and various malignancies (including those of the bladder, lung, liver, kidney, and prostate) are just a few of the health problems related to As exposure [8, 9]. The male reproductive system may be negatively impacted by As due to its direct effects on the testis. Eventually, this produces a disruption in the neuroendocrine system and hormone production, which has repercussions for spermatogenesis [10].
The objective of this study was to determine the potential correlation between the consumption of cigarettes and the amounts of Pb and As found in serum and seminal plasma.
Materials and Methods
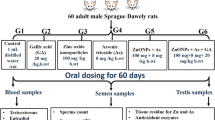
This case–control study was performed on 80 married individuals, ages ranging from 30 to 50 years old, attending the andrology clinic at our institution. These individuals were classified into two groups. Group 1 included 60 smokers who had smoked for more than one year and was subdivided into three subgroups, each with 20 smokers according to the number of cigarettes per day (CPD): mild (1–10 CPD), moderate (11–20 CPD), severe (> 21 CPD) [11]. Group 2 included 20 healthy nonsmoker volunteers as a control group.
We excluded patients with occupational exposure to Pb and/or As. Moreover, patients with drug intake or who had operations that may affect semen parameters were excluded. Subjects with abnormal genital examination, abnormal sex hormones, and abnormal secondary sexual characters were also excluded. Each participant underwent a comprehensive review of their personal, marital, and medical history. There was both a general and local examination.
Laboratory Investigation
Approximately 5 mL of blood was withdrawn from each participant under aseptic conditions, left to clot for half an hour, then centrifuged at 3000 rpm/min for 15 min, and the serum was kept at -20 °C until the serum was digested for determination of Pb and As concentrations. Serum digestion procedure was performed by adding 2 mL of nitric acid (70%) and 1 mL of perchloric acid (70%) to 0.5 mL of serum in a Pyrex tube and then heating this compound using a water bath over a hot plate. Then, the mixture was placed at 160 °C for 1 h and cooled; it was finally completed to 10 mL with (30%) hydrochloric acid. This compound was also heated with a water bath on a hot plate at 160 °C in order to obtain the absolute digestion of serum and vaporization of acids [12].
Collection of semen was done by masturbation into a sterile cup after 2–5 days of abstinence. Semen analysis was conducted using computer-assisted semen analysis. Ejaculate volume and liquefaction time were measured. In accordance with WHO standards 2010, sperm count, viability, motility, and morphology were evaluated after sperm samples were melted at 37 °C [13]. Then, isolation of seminal plasma was done and kept at -20 °C. Moreover, 100 μl of seminal plasma was digested with 500 μl of super-grade 0.8 M HNO3 in a glass tube. The residue of digested seminal plasma and serum was dissolved in 1 ml of 1% HNO3 and applied to a graphite tube for detection of Pb and As using an atomic absorption spectrophotometer (Varian SpectrAA 200Z, USA). The recovery of Pb in spiked semen and serum samples was 97%, respectively. The instrument was calibrated using 5, 10, and 15 μg/l standards for Pb. A sample blank was prepared with each set of samples to control for possible metal contamination from external sources. The level of detection for Pb was 0.1 μg/l. Calibration curves for As concentrations of 0, 0.1, 0.5, 1, 5, 10, 20, and 50 μg L-1 were analyzed. The standard reference (0.1 and 1 ppb) was injected into every tenth sample to assess instrumental sensitivity and stability. Furthermore, the calibration blank was measured to assess any background carryover, and duplicate samples were analyzed to observe reproducibility during analysis. The limit of detection was 0.2 μg/l.
Statistical Analysis
Data were analyzed on an IBM PC with SPSS version 19 (SPSS, Inc., Chicago, Illinois, USA). Mean (X-), standard deviation (SD), range, and numbers and percentages were used to represent quantitative and qualitative data. A chi-square test (χ2) was employed to examine the correlation between two qualitative variables. Mann–Whitney test was used to compare two nonnormally distributed quantitative groups. The relationship between quantitative and qualitative ordinal variables was measured using Spearman’s correlation (r). A P value ≤ 0.05 signifies statistical significance.
Results
Age, duration of marriage, number of children, and age of youngest kid were not significantly distinct among smokers and nonsmokers. Intercourse frequency was significantly lower in smokers than in nonsmokers, indicating a significant variation between the two groups (Table 1).
There were no significant differences between smokers and nonsmokers in terms of semen volume, liquefaction time, or pus cell count (P > 0.05 for all). Sperm count and motility were significantly lower in smokers than those in nonsmokers (34.3 ± 28.4 million/ml vs. 70.4 ± 27.9 million/ml and 31.7 ± 16%, vs. 41.1 ± 14.3%, P = 0.001 and 0.025, respectively). Sperm motility was significantly higher in mild smokers than in moderate and severe smokers (39.5 ± 13.5%, vs. 27.4 ± 17.1%, and 28.2 ± 15.4%; P = 0.017 and 0.016, respectively). Smokers had significantly lower sperm viability than nonsmokers (55.1 ± 19.7 vs. 65.5 ± 15.2%; P = 0.034). Severe smokers showed significantly lower sperm viability compared to mild smokers (45.7 ± 19.3%, vs. 64.5 ± 16.9%; P = 0.011). In smokers, the percentage of abnormally formed sperm was significantly higher than in nonsmokers (50.0 ± 19.3%, vs. 34.8 ± 15.2%; P = 0.002). In severe smokers, the percentage of abnormally formed sperm was significantly higher than in mild and moderate smokers (61.3 ± 14.9%, vs. 39.7 ± 17.9%, and 48.9 ± 19.2%, P = 0.001 and 0.022, respectively) (Table 2).
Smokers had substantially higher levels of seminal Pb than nonsmokers (4.85 ± 4.81 ug/L vs. 2.25 ± 1.47 ug/L; P = 0.001). Moreover, serum Pb level was significantly higher in smokers than nonsmokers (16.4 ± 12.8 µg/dL vs. 8.05 ± 3.41 µg/dL; P = 0.002). There were no significant differences in seminal and serum Pb regarding different grades of smoking (Table 3). Seminal Pb was significantly inversely related to sperm count (P = 0.004; r = -0.320) (Fig. 1a). However, there were nonsignificant correlations between seminal or serum Pb levels and age, number of CPD, and other semen parameters (P > 0.05 for all).
Correlation between seminal Pb & As levels and semen parameters. a Correlation between seminal Pb level and sperm count (million/ml) among smokers. b Correlation between seminal As level and sperm viability (%) among smokers. c Correlation between seminal As level and abnormal forms (%) of sperms among smokers
Seminal As level was significantly higher in smokers than nonsmokers (6.44 ± 2.36 ug/L vs. 4.85 ± 2.36 ug/L; P = 0.024). Moreover, seminal As level was substantially lower in mild smokers than in moderate and severe smoker groups (4.28 ± 2.60 ug/L vs. 6.62 ± 2.27 ug/L and 6.44 ± 2.36 ug/L). There was no significant difference among the studied groups concerning serum As level (P = 0.339) (Table 3). Seminal As had a significant negative correlation with sperm viability (P = 0.042; r = -0.264) (Fig. 1b). And seminal As and sperm abnormal forms had a significant positive correlation (P = 0.001; r = 0.414) (Fig. 1c). However, there were nonsignificant correlations between seminal or serum As levels and age, number of CPD, and other semen parameters (P > 0.05 for all) (data not shown).
A substantial positive association was observed between the levels of Pb in the serum and Pb in the seminal fluid (P = 0.001; r = 0.648) (Fig. 2). However, a significant positive relationship between the levels of Pb and As in seminal fluid was observed (P = 0.012, r = 0.298) (Fig. 3).
Discussion
Statistical analysis of the findings indicated that there was a significant decrease in the frequency of intercourse among smokers than nonsmokers. This observation is in agreement with the results of Weber et al. [14]. To explain this result, Biebel et al. revealed that cigarette smoking is one of the risk factors that might lead to erectile dysfunction [15].
As previously reported [16,17,18], we observed in this study that the smokers had significantly lower sperm density, percent of actively motile sperms and sperms viability as well as higher percent of abnormal forms compared to non-smokers. However, Pasqualotto et al. did not find any relationship between smoking and different semen parameters other than a decrease in semen volume. The authors suggested that the decline in semen volume may precede alterations in motility, sperm concentration, and morphology as an early indicator of poor semen quality [19].
Concerning seminal volume and liquefaction time, other studies were found to be in agreement with our results [20, 21]. However, Fawzy et al. reported a significant delay of liquefaction among smokers compared to nonsmokers, which could be due to their inclusion of both shisha and cigarette smokers [22].
How does cigarette smoking affect semen parameters? It could be due to the hormonal changes, the toxic content found in cigarette smoking that might have harmful effects on male germ cells, elevated reactive oxygen species, and decreased scavenging antioxidant activity in the seminal plasma of smokers [23]. Also, a decrease in essential elements and elevated levels of toxic heavy metals in all biological fluid may have significant negative effects on human reproductive health through their adverse impacts on the physiological and pathological functions [24, 25].
Compared to nonsmokers, smokers had significantly higher serum and seminal Pb levels, with a significant positive correlation between the two. This is consistent with the findings by other authors who concluded that Pb contaminates the smoke from cigarettes since it is burned up with the rest of the cigarette. Due to their small size, smoke particles can lodge in the most remote parts of the lungs and be absorbed directly into the bloodstream. It seems that no genital tract barrier can prevent Pb from entering the male reproductive tract [3, 26,27,28,29,30]. This was supported by the results reported by Debnath et al., who found a positive correlation between semen and serum Pb [31]. Further research discovered insignificant variations in serum and seminal Pb levels between smokers and nonsmokers, possibly because both were occupationally exposed to Pb [32,33,34].
Furthermore, in the smoker group, there was no correlation between both serum and seminal Pb levels and CPD. This was in agreement with Fatima et al., who stated that smokers did not show any significant difference in their semen Pb levels depending on the number of CPD [30]. However, Hsu et al. stated that both smokers and nonsmokers may have been exposed to Pb at work, which could account for the correlation between daily cigarette consumption and blood Pb levels.
Concerning the correlation between the seminal plasma Pb and the main items of semen parameters, the research demonstrated that seminal Pb is significantly negatively correlated to sperm count only and not to other semen parameters. However, previous studies are controversial and showed wide variations. To the best of our knowledge, one research reported a connection between Pb content in seminal plasma and only sperm count, which is statistically significant [35]. Rather than being the result of altered hypothalamic-pituitary function, the association between Pb concentration in sperm or sperm count could be due to a direct detrimental effect of Pb on spermatogenesis [36]. Many other studies reported that a statistically significant inverse association exists between the Pb concentration in seminal plasma and the count, motility, and morphology of sperm [37,38,39]. However, other studies failed to report any relationship between seminal plasma Pb and semen parameters, which may be attributed to the fact that these studies were conducted on a smaller number of individuals [31, 40,41,42].
Regarding As concentrations, the present study revealed a significantly higher seminal plasma (not serum) As level detected in smokers than non smokers. Also, Souza et al. and Nunzio et al. reported the same result [43, 44]. The authors concluded that the testes and the accessory organs may concentrate As in the seminal plasma. This may explain its elevation in the seminal plasma and not in serum in our investigated smoker males. However, Khoramdel et al. reported that there were correlations between high serum As level and abnormality of sperm morphology and a decrease in sperm chromatin condensation. Khoramdel et al.’s result can be explained due to exposure of their cases to different sources of As as drinking groundwater. Furthermore, genetic predisposition may play a role [45].
The seminal plasma As levels in smokers are significantly negatively correlated to sperm viability and positively correlated to the percentage of abnormal forms of sperm. Many authors were found to agree with these results and reported that infertile individuals may have decreased sperm viability due to As exposure, which might have affected sperm morphology and cytoskeletal structure [46,47,48].
In agreement with Nandi et al. [47], we noted that there was a significant positive relationship between seminal Pb and As levels. These both heavy metals (Pb and As) may have a singular or synergistic effect on seminal parameters. More research is required to explain the molecular mechanisms underlying the deleterious effects caused by these agents on reproductive function and spermatozoal integrity.
Also, Khoramdel et al. revealed that there was an association between these elevated serum Pb and As levels and poor sperm count, aberrant morphology, and impaired sperm motility. Pb and As concentrations in the serum of infertile men were significantly greater than those of fertile men. Pb and As concentrations in the serum of fertile men were substantially lower. This may be because histone-to-protamine replacement is significantly reduced in the sperm of infertile males, which reduces chromatin condensation and leads to infertility [45].
There is no well-defined mechanism for how heavy metals cause harm to male reproductive systems. Animal research suggests that these xenobiotics may limit androgen biosynthesis in Leydig cells, cause lipid peroxidation of the cell membrane, and contribute to oxidative destruction of DNA by inducing mitochondrial dysfunction, increasing free radical generation, or decreasing antioxidant levels. Increased morphological abnormalities, decreased motility, and reduced fertilization potential are likely all interrelated aspects of spermatozoa health [49].
Conclusion
Semen parameters are affected adversely by smoking through high levels of heavy metals like Pb and As. These detrimental effects are related to the cumulative effect of smoking.
Data Availability
No datasets were generated or analysed during the current study.
References
Dai JB, Wang ZX, Qiao ZD (2015) The hazardous effects of tobacco smoking on male fertility. Asian J Androl 17(6):954–960. https://doi.org/10.4103/1008-682X.150847
Yu B, Qi Y, Liu D, Gao X, Chen H, Bai C, Huang Z (2014) Cigarette smoking is associated with abnormal histone-to-protamine transition in human sperm. Fertil Steril J 101(1):51–57. https://doi.org/10.1016/j.fertnstert.2013.09.001
Hsu PC, Chang HY, Guo YL, Liu YC, Shih TS (2009) Effect of smoking on blood lead levels in workers and role of reactive oxygen species in lead-induced sperm chromatin DNA damage. J Fertil Steril 91(4):1096–1103. https://doi.org/10.1016/j.fertnstert.2008.01.005
Tong S, Schirnding YE, Prapamontol T (2000) Environmental lead exposure: a public health problem of global dimensions. Bull World Health Organ 78(9):1068–1077
Sokol RZ, Wang S, Wan YJ, Stanczyk FZ, Gentzschein E, Chapin RE (2002) Long-term, low-dose lead exposure alters the gonadotropin-releasing hormone system in the male rat. Environ Health Perspect J 110(9):871–874. https://doi.org/10.1289/ehp.02110871
Rafique M, Khan N, Perveen K, Naqvi A (2009) The effects of lead and zinc on the quality of semen of albino rats. J Coll Physicians Surg Pak 19(8):510–513
Mahmoud A, Kiss P, Vanhoorne M, De Bacquer D, Comhaire F (2005) Is inhibin B involved in the toxic effect of lead on male reproduction? Int J Androl 28(3):150–155. https://doi.org/10.1111/j.1365-2605.2005.00524.x
Calatayud M, Barrios JA, Velez D, Devesa V (2012) In vitro study of transporters involved in intestinal absorption of inorganic arsenic. Chem Res Toxicol 25(2):446–453. https://doi.org/10.1021/tx200491f
Chanihoon GQ, Afridi HI, Unar A, Talpur FN, Kalochi HB, Nassani R, Laghari N, Uddin N, Ghulam A, Chandio AU (2022) Selenium and mercury concentrations in biological samples from patients with COVID-19. J Trace Elem Med Biol 73:127038. https://doi.org/10.1016/j.jtemb.2022.127038
Okpashi VE, Ebunta AF (2021) Predicting the Outcome of Arsenic Toxicity on Exposed Juvenile Male-Humans: A Shift to Infertility. Arsenic Toxicity: Challenges and Solutions, pp 1–25. https://doi.org/10.1007/978-981-33-6068-6_1
Chkhaidze I, Maglakelidze N, Maglakelidze T, Khaltaev N (2013) Prevalence of and factors influencing smoking among medical and non-medical students in Tbilisi, Georgia. J Bras Pneumol 39(5):579–584. https://doi.org/10.1590/S1806-37132013000500008
Ji X, Ren J (2002) Determination of copper and zinc in serum by derivative atomic absorption spectrometry using the microsampling technique. Analyst 127(3):416–419. https://doi.org/10.1039/B109367N
WHO (2010) laboratory manual for the examination and processing of human semen- 5th edn. Switzerland, p 271
Weber MF, Smith DP, O’Connell DL, Patel MI, de Souza PL, Sitas F, Banks E (2013) Risk factors for erectile dysfunction in a cohort of 108 477. Aust Med J 199(2):107–111. https://doi.org/10.5694/mja12.11548
Biebel MG, Burnett AL, Sadeghi-Nejad H (2016) Male sexual function and smoking. J Sex Med 4(4):366–375. https://doi.org/10.1016/j.sxmr.2016.05.001
Ramlau-Hansen CH, Thulstrup AM, Aggerholm AS, Jensen MS, Toft G, Bonde JP (2007) Is smoking a risk factor for decreased semen quality? A cross-sectional analysis. Hum Reprod J 22(1):188–196. https://doi.org/10.1093/humrep/del364
Niu ZH, Liu JB, Shi TY, Yuan Y, Shi HJ (2010) Impact of cigarette smoking on human sperm DNA integrity. Natl J Androl 16(4):300–304
Asare-Anane H, Bannison SB, Ofori EK, Ateko RO, Bawah AT, Amanquah SD, Oppong SY, Gandau BB, Ziem JB (2016) Tobacco smoking is associated with decreased semen quality. Reprod Health 13(1):1–6. https://doi.org/10.1186/s12978-016-0207-z
Pasqualotto FF, Sobreiro BP, Hallak J, Pasqualotto EB, Lucon AM (2006) Cigarette smoking is related to a decrease in semen volume in a population of fertile men. BJU Int 97(2):324–326. https://doi.org/10.1111/j.1464-410X.2005.05906.x
Künzle R, Mueller MD, Hänggi W, Birkhäuser MH, Drescher H, Bersinger NA (2003) Semen quality of male smokers and nonsmokers in infertile couples. Fertil Steril J 79(2):287–291. https://doi.org/10.1016/s0015-0282(02)04664-2
Kumosani TA, Elshal MF, Al-Jonaid AA, Abduljabar HS (2008) The influence of smoking on semen quality, seminal microelements and Ca2+-ATPase activity among infertile and fertile men. Clin Biochem 41(14–15):1199–1203. https://doi.org/10.1016/j.clinbiochem.2008.07.013
Fawzy IA, Kamal NN, Abdulla AM (2011) Reproductive toxicity of tobacco shisha smoking on semen parameters and hormones levels among adult Egyptian men. Res J Environ Toxicol 5(5):282–292. https://doi.org/10.3923/rjet.2011.282.292
Zenzes MT (2000) Smoking and reproduction: gene damage to human gametes and embryos. Hum Reprod Updat 6(2):122–131. https://doi.org/10.1093/humupd/6.2.122
Afridi HI, Kazi TG, Talpur FN, Baig JA, Chanihoon GQ (2022) Essential trace and Toxic elemental concentrations in biological samples of male adult referent and Eunuch subjects. Clin Chim Acta 529:96–103. https://doi.org/10.1016/j.cca.2022.02.010
Chanihoon GQ, Afridi HI, Kazi TG, Talpur FN, Baig JA (2021) Evaluation of zinc and cadmium levels in the biological samples of Ewing sarcomas patients and healthy subjects. Clin Chim Acta 522:1–7. https://doi.org/10.1016/j.cca.2021.08.002
Fatima P, Debnath BC, Hossain MM, Rahman D, Banu J (2008) Effect of smoking on blood and semen lead level in male partners of infertile couple. J Chittagong Med Coll Teach Assoc 19(2):3–6. https://doi.org/10.1177/1557988316643383
Lanocha-Arendarczyk N, Kosik-Bogacka DI, Prokopowicz A, Kalisinska E, Sokolowski S, Karaczun M, Zietek P, Podlasińska J, Pilarczyk B, Tomza-Marciniak A, Baranowska-Bosiacka I (2015) The effect of risk factors on the levels of chemical elements in the tibial plateau of patients with osteoarthritis following knee surgery. Biomed Res Int e650282:1–10. https://doi.org/10.1155/2015/650282
Al-Ghabban SI (2018) Blood lead levels among cigarette smokers. Kufa Med J 9:431–435. https://www.researchgate.net/publication/322790056_Blood_Lead_Levels_among_Cigarette_Smokers
Hashim A, Fathima H, Muhammed RC, Neevan DD (2019) Analysis of lead, cadmium, and nickel in blood donors in relation to smoking—a comparative study. J Environ Pathol Toxicol Oncol 38(2):165–172. https://doi.org/10.1615/JEnvironPatholToxicolOncol.2019028792
Lee E, Park B, Chung WY, Park JE, Hwang SC, Park KJ, Sheen SS, Ahn SV, Park JB, Ahn CM, Lee SH (2020) Blood lead levels in relation to smoking and chronic obstructive pulmonary disease (COPD): a study from Korean National Health and Nutrition Examination Survey (KNHANES). J Thorac Dis 12(6):3135–3147. https://doi.org/10.21037/jtd-20-739
Debnath BC, Ibrahim M, Fatima P (2010) Study of blood lead and semen lead concentration in male infertility. Pulse 4(1):10–13. https://doi.org/10.3329/pulse.v4i1.6956
Singh G, Singh V, Wang ZX, Voisin G, Lefebvre F, Navenot JM, Evans B, Verma M, Anderson DW, Schneider JS (2018) Effects of developmental lead exposure on the hippocampal methylome: Influences of sex and timing and level of exposure. Toxicol Lett 290:63–72. https://doi.org/10.1016/j.toxlet.2018.03.021
Fouad AA, Foda NT, Diab IH, Badr El Dine FM, Balah MI (2020) Evaluation of possible molecular toxicity induced by occupational exposure to lead and concomitant effect of smoking. Environ Sci Pollut Res 27:411–423. https://doi.org/10.1007/s11356-019-06879-0
Steven Serafini S, O’Flaherty C (2022) Redox regulation to modulate phosphorylation events in human spermatozoa. Antioxid Redox Signal J 37(7–9):437–450. https://doi.org/10.1089/ars.2021.0117
Wu HM, Lin-Tan DT, Wang ML, Huang HY, Lee CL, Wang HS, Soong YK, Lin JL (2012) Lead level in seminal plasma may affect semen quality for men without occupational exposure to lead. Reprod Biol Endocrinol J 10(1):1–5. https://doi.org/10.1186/1477-7827-10-91
Allouche L, Hamadouche M, Touabti A (2009) Chronic effects of low lead levels on sperm quality, gonadotropins and testosterone in albino rats. Exp Toxicol Pathol 61(5):503–510. https://doi.org/10.1016/j.etp.2008.12.003
Kahraman S, Hassa H, Karatas A, Ilgin H (2012) The effect of blood and seminal plasma heavy metal and trace element levels on sperm quality. Turkiye Klinikleri Tip Bilimleri Dergisi 32(6):1560–1568. https://doi.org/10.5336/medsci.2011-26578
Pant N, Kumar G, Upadhyay AD, Gupta YK, Chaturvedi PK (2015) Correlation between lead and cadmium concentration and semen quality. Andrologia 47(8):887–891. https://doi.org/10.1111/and.12342
Li CJ, Yeh CY, Chen RY, Tzeng CR, Han BC, Chien LC (2015) Biomonitoring of blood heavy metals and reproductive hormone level related to low semen quality. J Hazard Mater 300:815–822. https://doi.org/10.1016/j.jhazmat.2015.08.027
Dobrakowski M, Kaletka Z, Machoń-Grecka A, Kasperczyk S, Horak S, Birkner E, Zalejska-Fiolka J, Kasperczyk A (2018) The role of oxidative stress, selected metals, and parameters of the immune system in male fertility. Oxid Med Cell Longev e6249536:1–8. https://doi.org/10.1155/2018/6249536
Marzec-Wróblewska U, Kamiński P, Łakota P, Szymański M, Wasilow K, Ludwikowski G, Jerzak L, Stuczyński T, Woźniak A, Buciński A (2019) Human sperm characteristics with regard to cobalt, chromium, and lead in semen and activity of catalase in seminal plasma. Biol Trace Elem Res 188:251–260. https://doi.org/10.1007/s12011-018-1416-9
Tuncay G, Karaer A, Tanrikut E, Ozgul O (2021) The effect of seminal plasma cadmium and lead levels on semen parameters in male subjects of infertile couples: a prospective cohort study. J Obstet Gynaeco 41(6):946–950. https://doi.org/10.1080/01443615.2020.1820459
Souza AC, Marchesi SC, Ferraz RP, Lima GD, Oliveira JA, Machado-Neves M (2016) Effects of sodium arsenate and arsenite on male reproductive functions in Wistar rats. J Toxicol Environ Health 79(6):274–286. https://doi.org/10.1080/15287394.2016.1150926
Nunzio AD, Giarra A, Toscanesi M, Amoresano A, Piscopo M, Ceretti E, Zani C, Lorenzetti S, Trifuoggi M, Montano L (2022) Comparison between macro and trace element concentrations in human semen and blood serum in highly polluted areas in Italy. Int J Environ Res Public Health 19(18):11635.1–17. 1660–4601/19/18/11635
Khoramdel H, Farzadinia P, Shariati M, Mokhtari M, Bargahi A (2021) Determination of lead and arsenic concentrations in the serum and its effect on sperm parameters and sperm quality in patients referred to omid persian gulf infertility center of bushehr. J Biol Sci 8(3):168–173. https://sid.ir/paper/977971/en
Sengupta M, Deb I, Sharma GD, Kar KK (2013) Human sperm and other seminal constituents in male infertile patients from arsenic and cadmium rich areas of Southern Assam. Syst Biol Reprod Med 59(4):199–209. https://doi.org/10.3109/19396368.2013.783143
Nandi P, Varghese AC, Das MC, Banerjee P, Murmu N, Banerjee SK, Banerjee SK (2015) Lead, cadmium and arsenic content in seminal plasma and its effects on seminogram. Int J Sci Eng Technol (3) 204–207. CorpusID:212484107
Wang YX, Wang P, Feng W, Liu C, Yang P, Chen YJ, Sun L, Sun Y, Yue J, Gu LJ, Zeng Q (2017) Relationships between seminal plasma metals/metalloids and semen quality, sperm apoptosis and DNA integrity. Environ Pollut 224:224–234. https://doi.org/10.1016/j.envpol.2017.01.083
Patra RC, Rautray AK, Swarup D (2011) Oxidative stress in lead and cadmium toxicity and its amelioration. J Vet Med e457327:1–9. https://doi.org/10.4061/2011/457327
Acknowledgements
All of the authors want to thank the entire research team as well as all the healthy volunteers who took part in our study.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). No sources of funding were used to conduct this study or prepare this manuscript.
Author information
Authors and Affiliations
Contributions
Farag AGA: critical literature review, study conception, and planning Badr EA: Data analysis and interpretation Khalifa MN: Data collection and analysis Kholif AO: Data collection and analysis Ghanem MM: Data analysis and interpretation, literature review, writing the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
In accordance with the principles outlined in the Helsinki Declaration (World Medical Assembly), this research was approved by the local ethics committee, and all of the participants in the study gave their written informed permission. The record number for this investigation is 9/2021DERM43.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Farag, A.G.A., Badr, E.AE., Kholif, A.O.A. et al. Serum and Seminal Plasma Levels of Lead and Arsenic in Cigarette Smokers and Their Relation to the Semen Parameters. Biol Trace Elem Res (2024). https://doi.org/10.1007/s12011-023-04039-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12011-023-04039-7