Abstract
Autologous ear reconstruction is the preferred treatment in case of partial or total absence of the external ear. The surgery can be very challenging to perform and the aesthetic result highly dependent on the surgeon’s “artistic skills”. In this context a preoperative planning and simulation phase based on the patient’s specific anatomy may result crucial for the surgical outcome. In this work, starting from a case study, the elements necessary for an effective simulation are identified and a strategy for their interactive design and customization is devised with a perspective of a semi-automatization of the procedure.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
1 Introduction
Microtia is a congenital malformation characterized by the absence or deformation of the outer ear in terms of size, orientation, shape and position. Three alternative treatments are used in clinical practice to address this physical malformation [1]: (1) external silicone prosthesis, (2) Medpor implants, (3) reconstruction with autologous cartilage tissue extracted from the ribcage. The prosthetic approach is a non-permanent solution, while the alloplastic approach requires the insertion of a foreign body and is therefore more subjected to rejection. In this context, the third technique, autologous ear reconstruction (AER), represents the preferred clinical treatment for restoring the anatomy of the ear as it is a definitive solution with high degree of integration. This surgery requires the realization of a 3D framework of the ear (Fig. 1b), obtained by carving and sculpting harvested patient’s costal cartilages, before the final implantation into a subcutaneous pocket in the auricular region. According to the technique proposed in [2], the auricular elements to be reconstructed are helix, antihelix, tragus-antitragus (Fig. 1a) plus a support base.
Due to the complexity of the surgical technique and of the 3D geometry to be reproduced, this procedure represents a real challenge for plastic surgeons. The main difficulties are: (i) study of the anatomy of the patient’s healthy ear (HE) to evaluate its volume and size; (ii) isolation of the anatomical elements of the ear involved in the surgery; (iii) optimization of the individual elements removal phase from the costal cartilage; (iv) sculpting and carving of the framework and finally (v) insertion of the framework into the subcutaneous pocket obtained in the auricular region.
In the first phase (i) the healthy reference ear is studied. The key to this process is to analyze the distinctive features of the reference ear in view of the successive 3D framework reconstruction of a framework that faithfully reproduces the anatomy. The aim of this phase is then to obtain a specular model of the reference (healthy) anatomy, so that the future reconstructed ear satisfies face symmetry. Starting from the mirrored model, it is necessary to isolate the elements that are reconstructed during the surgery (ii) (Fig. 1). These elements must be subsequently (iii) retrieved in the available cartilage volume. Typically, cartilage ranging from the sixth to the ninth rib is harvested from the patient. After cutting these elements from the cartilage, the process of sculpting, carving and suturing (iv) of the framework starts. This step is performed by the surgeon using surgical instruments designed specifically for this procedure. In the last step (v) the framework is inserted into the subcutaneous pocket. The complications that can occur at this level are the lack of available material or a particular conformation of the anatomy involved in the pathology.
In order to achieve an aesthetically pleasing result, the reconstructed ear must look natural and sufficiently resembling the HE. To this purpose, the surgeon must be specifically trained both in sculpting and carving to be able to reproduce the ear complex geometry.
For all these reasons, the simulation of the AER is essential, and it results relevant to improve several aspects of the current surgical procedure. The training aims for surgeons to develop an “aesthetic eye” able to identify proportions and harmonies and gain technical skills. Another important advantage of the simulation is the possibility to familiarize with the patient’s specific anatomy, which leads to a higher confidence of the surgeon in the surgery room and the optimization of the costal cartilage harvesting phase, minimizing the invasiveness of the surgery.
In recent years, reverse engineering (RE) and additive manufacturing (AM) techniques are rapidly becoming key tools to support the customization of the simulation process [3]. These technologies make it possible to produce faithful replicas of the patient’s anatomy and to design medical devices, therefore can be used for a customized simulation that enables to meet the suitable training requirements. However, to date, the use of these technologies requires specialized technicians.
In this paper, starting from a case study, the preoperative simulation and planning process is analyzed with the objective to develop an interactive procedure, exploiting RE and AM techniques, that can be accessed directly by medical staff to create patient-specific simulators.
2 Preoperative planning and simulation: case report
In collaboration with the Meyer Children’s Hospital, a patient with unilateral microtia was identified with the aim of investigating the process of design and development of a customized trainer. From the joint analysis of engineers and surgeons on AER, it emerged that, in order to obtain an effective simulation, which consistently helps surgeons to practice all the challenges that this specific surgery foresees, the simulator must include two principal elements: (1) the silicone replica of the patient’s cartilages (purple in Fig. 2) and (2) the mirrored model of the healthy ear (blue in Fig. 2) along with the separate models of the anatomical elements to be reconstructed (red in Fig. 2).
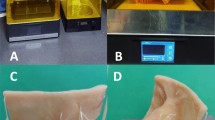
The surgery simulation begins by identifying the areas of cartilage from which the auricular elements can be extracted. This step is performed by opportunely arranging the elements’ models on the cartilage replica, thus performing manual nesting. After optimizing the extraction in terms of cartilage tissue, the surgeon places the individual elements on the cartilage and draws on it their (see Fig. 3a). By following the traced contours, the surgeon cuts the elements and refines the details by sculpting and carving; successively the framework can be sutured (Fig. 3b).
Finally, the aesthetic result is simulated using a 1 mm thick silicone pad to evaluate the effect of the skin over the framework [4]. Specifically, the framework is placed between the pad and a suction device that, vacuuming the air, allows the silicone sheet to adhere to the framework (Fig. 3c).
3 Proposed strategy for custom preoperative planning
The simulation design process of the AER trainer for the specific case study was taken into consideration with the idea of generalizing and therefore standardizing the production phases. The aim is to define a standard workflow that formalizes the main steps for the realization of patient-specific task trainers.
This constitutes the basis to the development of a semi-automatic procedure allowing the physician to obtain the final product autonomously and with just few inputs. In this way, the trainer can be manufactured in compliance with medical requirements without the involvement of RE and CAD modeling experts. This would represent on its own a significant step forward, since the availability of an easy-to-use tool allowing the medical staff to obtain in full autonomy the desired custom trainer leads to a significant reduction of both costs and timings. The resulting workflow is shown in Fig. 4, in blue are depicted the steps leading to the elements required for the preoperative simulation (in red).
In brief, the workflow consists of two parallel processes: one that leads to the creation of the auricular element’s models and one that leads to the manufacturing of the costal cartilage replica. The 3D model of the auricular anatomy of the HE is processed to identify the anatomical elements involved in the simulation. The models are then manufactured using AM techniques. In parallel, acquisitions obtained by means of diagnostic imaging techniques are used to reconstruct the 3D model of costal cartilages, that is then used in a CAD environment for the 3D modeling of molds suitable for the fabrication of silicone replicas.
Cartilage nesting is performed with the two resulting elements, with the aim of minimizing the cartilage material to be used/harvested from the patient. In the case study, the optimization of the cut was obtained experimentally by the surgeon directly with the physical models. If performed this way, also the nesting phase can be considered as an integral part of the AER simulation. It is objective of the present work to automate the nesting phase in order to obtain an optimal result and reduce the simulation time and consequently the surgical times. If on the one hand the workflow phases can be performed manually by experts, on the other hand the automation of the processes can represent a great step forward for the diffusion of the customized simulation of this type of intervention.
In view of the semi-automatization of the production process, it is not only necessary for each step to be automated internally, but also that the output of each step is consistent with the input required by the next. To this aim, the diagram in Fig. 4 was analyzed at each stage to define three main aspects: (1) identification of the best alternative among available methods in terms of results and timing, (2) evaluation of the possibility of developing new methodologies and (3) assessment of the feasibility of automating the step.
4 Conclusions
Starting from a case study, the workflow for the creation of patient-specific AER trainers was determined. The definition of a standard workflow allows to split the process into the principal phases in order to analyze the three aspects for each phase. This lays the foundation for the automation of some processes with the aim of obtaining an interactive procedure allowing the physician to autonomously generate a patient-specific AER trainer. This represents a key point, being AER a very complex surgery for which the introduction of the patient-specific preoperative simulation would significantly mitigate the challenge even for the most experienced surgeons. Thus, the semi-automatization of the simulator production process would facilitate training in a hospital environment. Within this context, this human–machine interaction allows to realize a semi-automatic process which enables, on the one hand, to overcome some limits of the state of the art and, on the other hand, to obtain a trainer that satisfies the medical requirements.
References
Mussi, E., Furferi, R., Volpe, Y., Facchini, F., McGreevy, K.S., Uccheddu, F.: Ear reconstruction simulation: from handcrafting to 3D printing. Bioengineering 6, 14 (2019)
Nagata, S.: A new method of total reconstruction of the auricle for microtia. Plast. Reconstr. Surg. 92, 187–201 (1993)
Giannatsis, J., Dedoussis, V.: Additive fabrication technologies applied to medicine and health care: a review. Int. J. Adv. Manuf. Technol. 40, 116–127 (2009)
Firmin, F., Marchac, A.: A novel algorithm for autologous ear reconstruction. Semin. Plast. Surg. 25, 257–264 (2011)
Funding
Open access funding provided by Università degli Studi di Firenze within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mussi, E., Servi, M., Facchini, F. et al. A computer-aided strategy for preoperative simulation of autologous ear reconstruction procedure. Int J Interact Des Manuf 15, 77–80 (2021). https://doi.org/10.1007/s12008-020-00723-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12008-020-00723-3