Abstract
Background
Despite the widely reported success of total joint arthroplasty (TJA) in reducing pain and improving quality of life and function for patients with hip or knee osteoarthritis, rates of TJA use vary widely throughout the United States, with broad disparities based on geographic, racial, and socioeconomic factors. Shared decision-making approaches, which require an exchange of information between patients and their physicians, can be helpful in improving patient satisfaction with their treatment decision and appropriate use of TJA.
Questions/hypotheses
Expected-value decision analysis models incorporating evidence-based outcome data with individual patient preferences regarding health states and willingness to pay, when used in shared decision-making models, will improve satisfaction among patients with hip or knee osteoarthritis and lead to more appropriate use of TJA.
Proposed Program
Patients with hip or knee osteoarthritis will be randomized to usual care or participation in a shared decision-making intervention. Patients in the shared decision-making intervention arm will have their preferences for individual health states related to osteoarthritis and TJA measured using the time trade-off technique, and these values will be incorporated in an expected-value decision analysis model, which also will incorporate the patient’s willingness to pay for a particular treatment intervention and evidence-based outcome probabilities. The patient’s decision for operative versus nonoperative care and their level of satisfaction with their decision will be compared using chi square and Mann-Whitney rank-sum tests.
Significance
Information regarding patient preferences for particular health states and willingness to pay can be combined with evidence-based outcome data in expected-value decision analysis models, which will help inform shared clinical decision making between surgeons and their patients with hip or knee osteoarthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Questions/hypotheses
Expected-value decision analysis models incorporating evidence-based outcome data with individual patient preferences regarding health states and willingness to pay, when used in shared decision-making models, will improve satisfaction among patients with hip or knee osteoarthritis and lead to more appropriate use of TJA.
Background
TJA decreases pain and improves function and quality of life for patients with disabling osteoarthritis (OA) of the hip and knee [19]. However, some investigators have documented substantial geographic variation in TJA procedure rates and use of premium TJA implants (eg, hard-on-hard bearings) that cannot be explained by differences in population characteristics alone [4, 18, 22, 24]. Researchers from the Dartmouth Center for Evaluative Clinical Sciences [13, 14, 23] have suggested one potentially helpful tool to address geographic variation in practice patterns would be an increased emphasis on informing patients, eliciting their preferences, and involving them in the choice of treatment. Others have noted an important prerequisite for successful shared decision-making (SDM) is gathering and synthesizing evidence-based outcome data with which to educate patients so that their choices are as informed as possible [1, 2].
SDM, as opposed to more traditional authoritative and paternalistic models of the patient-practitioner relationship, requires information exchange between the clinician and the patient, who then deliberate together and decide on the optimal treatment option [11]. Researchers have recognized the need to temper the role of so-called “medical opinion” and enhance the role of patient preference in medical decision making [9, 11, 17]. Some investigators [6, 7] have noted that although some patients want complete control over their healthcare decision making and others want physicians to make all treatment decisions, most would prefer to share the decision making with their physicians. Hawker et al. [9] have shown professional opinion concerning a patient’s need for TJA can differ from the patient’s preferences.
Although physicians often have superior knowledge regarding the pathophysiology of a patient’s disease and the risks and benefits of specific treatment options, they lack information regarding individual patient preferences important in formulating a treatment plan for a particular patient. Expected-value decision analysis models can be used to supplement more traditional shared decision-making tools (eg, DVDs and booklets describing treatment alternatives) by incorporating the best available evidence-based outcome data with individual patient preferences, as measured from direct preference assessment. The purpose of an expected-value decision analysis model is to help patients and clinicians choose between two or more treatment alternatives, each of which can lead to several possible outcomes, with chance determining the outcome experienced by an individual patient (Fig. 1).
A simple decision tree for THA versus nonoperative care is shown. The square indicates a decision node representing a choice between two or more treatments being considered (eg, THA and nonoperative care). The circles are chance nodes, reflecting possible mutually exclusive outcomes with the probability shown below each branch. The triangles are terminal nodes for the final outcomes and to the right of each terminal node is the “reward,” which can be utility, QALYs, cost, or any other quantitative measure of interest associated with each outcome. The expected value of each choice is calculated by multiplying the probability of each branch by its reward in a weighted average in a process known as “folding back.” In the case above, the expected value of THA is 9.6, which is favored over the expected value of nonoperative care of 5.4.
Health state utility, which is preference-based measure of health status ranging from 1.0 (perfect health) to 0.0 (death), refers to the desirability or preference that individuals or societies have for a given health outcome [16]. Utility scores also can be used to weigh time spent in each health state to estimate quality-adjusted life years (QALYs) gained, which then can be used as the denominator in cost-utility analyses and cost-effectiveness analyses. The three most commonly used approaches for direct assessment of utility are the time trade-off (TTO), standard-gamble, and visual analog scale (also referred to as rating scale) techniques [21]. The TTO technique (Fig. 2) derives values for various health states by asking patients how many years in their current state of health they would be willing to give up to live a fixed number of years in excellent health [8]. Another technique for direct preference assessment is the standard-gamble technique (Fig. 3), which involves offering the patient two treatment alternatives. Alternative 1 is a treatment with two possible outcomes: either the patient returns to normal health and lives for an additional finite number of years (probability p) or the patient dies immediately. Alternative 2 has the certain outcome of a chronic state of illness or disability (i) for a finite period of time. The probability (p) is varied until the subject is indifferent between the two alternatives, at which point the value for chronic state i is set equal to p [15]. Finally, the visual analog scale (or rating scale) technique involves asking patients to simply locate various health states on a linear scale from 0 to 1 [15]. Although it has been suggested this technique is the simplest to administer and easiest for patients to understand, one drawback of the technique is the tendency for most patients to rate their health as “average” versus the health of their peers and thus to center-bias the utility assessments [20]. However, the visual analog scale technique is valid and reproducible for measuring utility in patients with OA and TJA [3].
A graph illustrates the TTO technique for direct preference assessment. This technique derives values for various health states by asking patients how many years in their current state of health they would be willing to give up to live a fixed number of years in excellent health (x) or the time living the rest of their lives in their current state of health (t). i is the direct preference score for the health state. Time, x, varies in values until the respondent is indifferent between the two choices. The higher the value a person places on the state i, the greater the time x would be required for the respondent to be indifferent between the choices being presented [8].
A flowchart illustrates the standard-gamble technique for direct preference assessment. This technique involves offering the patient two treatment alternatives. In this example, Alternative 1 is a treatment with two possible outcomes: either the patient returns to normal health and lives for an additional finite number of years (probability p) or the patient dies immediately (probability 1 − p). Alternative 2 has the certain outcome of a chronic state of illness or disability (i) for a finite period of time. The probability (p) is varied until the subject is indifferent between the two alternatives, at which point the value for chronic state i is set equal to p [15].
In addition to considering individual patient preferences for various health states and downstream consequences associated with their care, decision aids should also incorporate patient preferences and values regarding the cost of care. As consumer-focused health plans that require patients to assume a larger burden of healthcare costs have increased in popularity in the United States, cost considerations have become increasingly important for individual patients when seeking the best value for their healthcare dollars. Thus, SDM tools will need to incorporate not only patient preferences regarding individual health states and health outcomes but also information regarding their willingness to pay for a particular treatment intervention or desired health state.
Proposed Program
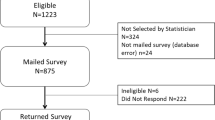
All patients who are referred for evaluation and treatment of hip or knee OA will be asked to participate in a randomized controlled trial (RCT). Patients who choose to participate will be randomized to one of two groups (SDM intervention [Group 1] and usual care [Group 2]). All patients will receive standard patient education materials, including literature regarding OA, TJA, and the opportunity to participate in a patient education class regarding TJA taught by a clinical nurse specialist (per our standard treatment protocol for all patients). Patients in Group 1 will also be offered the opportunity to participate in the SDM program, and patients in Group 2 will not be offered this option. Individual patient preferences for patients in Group 1 will be determined by direct preference assessment using the TTO method as described above, and willingness to pay will be measured using a validated questionnaire. With the help of a trained research nurse, patients will be given the opportunity to enter their preferences and willingness to pay into an expected-value decision analysis model that also will include evidence-based outcome probabilities for each treatment option, and to discuss with their surgeon which treatment option (surgical versus nonsurgical) would provide them with the greatest short- and long-term benefits in terms of QALYs gained and cost/QALY, based on the model output and the sensitivity analysis.
The primary outcome measures will be the decision to undergo operative (eg, TJA) or nonoperative treatment and patient satisfaction with their decision measured using the satisfaction with decision scale described previously and validated for use in healthcare decision making by Holmes-Rovner et al. [10]. To determine the effect of the SDM intervention on choice of treatment, the treatment option (operative versus nonoperative) chosen by patients in Group 1 and Group 2 will be compared using the chi square test. Satisfaction with decision values for each group will be compared using the Mann-Whitney rank-sum test. Statistical significance will be based on an α level of 0.05.
Limitations
Despite the novel concepts outlined in our proposed program, there are several potential pitfalls and limitations that we need to be prepared to address. First, patients may prefer to have their surgeon make their treatment decision for them and therefore may be reluctant to participate in the RCT. The demographic, socioeconomic, and clinical characteristics of patients who choose to participate in the RCT versus those who decline will be tracked and compared to look for biases that may affect the generalizability of the results. Second, patients and surgeons may have difficulty grasping the concept of incorporating their stated preferences for particular health states and evidence from the literature regarding treatment outcomes for hip and knee OA into their medical decision making. Furthermore, patients rarely pay out of pocket for their medical care and therefore often are insensitive to the cost of care, which may bias their responses to the willingness to pay questionnaire. However, even if this is the case, we will be able to study the impact of the proposed intervention on treatment choice (eg, operative versus nonoperative) and patient satisfaction. Finally, as clinical decision making and patient satisfaction are influenced by many factors, it may be difficult to assess the impact of the SDM intervention on treatment choice and patient satisfaction. However, the RCT study design will help mitigate some of the bias associated with other independent factors affecting treatment choice and patient satisfaction.
Next Steps
Although SDM tools have the potential to improve patient satisfaction and lead to more appropriate use of scarce healthcare resources, incorporating them into general clinical practice, especially busy outpatient orthopaedic practices, may prove to be challenging. Many physician practices already are feeling pressured by increasing overhead and flat reimbursement, and adding a potentially beneficial but relatively unproven intervention that could add time and expense without any clear financial benefit to their practice may be met with resistance by clinicians and office managers. These challenges will need to be addressed in several ways before SDM approaches are widely adopted in clinical practice. First, to investigate the feasibility of implementing a SDM program into busy orthopaedic surgical practices, we plan to measure and compare total visit time and provider satisfaction for each encounter for patients in Groups 1 and 2. It is possible having patients review evidence-based information regarding treatment alternatives before their office visit could improve the efficiency of the visit by allowing the surgeon to focus on helping the patient reach a treatment decision, rather than spending time answering questions regarding what treatment options are available for hip or knee OA. Second, some states and policymakers are considering expanding legislation that would provide funding to study the use of SDM programs and in some cases require such programs to be offered to patients as part of the informed-consent process [12]. Finally, the recently passed federal Patient Protection and Affordable Care Act (PPACA) includes several demonstration projects that would provide additional reimbursement to clinicians who incorporate SDM approaches into their practice, which could offset some of the costs associated with implementation and stimulate more physician practices to adopt SDM tools into their clinical practices, especially if studies like ours are able to show value in terms of improved patient satisfaction and more efficient use of resources.
Implications and Future Directions
An increase in consumer demand has led to a sharp rise in the volume of publicly available information regarding chronic disease processes such as OA and treatment options such as TJA. At the same time, increased emphasis on direct-to-consumer advertising in OA and TJA [5] have led to concerns by clinicians and policy makers regarding the source and accuracy of information patients use when making important decisions regarding their healthcare. With an increasing trend toward public reporting of information regarding the cost and quality of healthcare, patients are being asked to take on a larger role in their healthcare decision making and to share a greater burden of the costs associated with their care. As these trends evolve, SDM tools will become increasingly important in helping patients and clinicians reach decisions regarding the treatment of chronic conditions such as OA.
Several health services researchers and policy makers have suggested rates of use of TJA may be more dependent on the supply of orthopaedic surgeons than the prevalence of disease [4, 18, 22, 24]. Understanding how patient and provider choices regarding the timing of TJA with respect to the severity of pain, disability, and functional decline, choice of implant, and type of procedure impact clinical outcomes is important in helping inform true SDM between patients and clinicians. Expected-value decision analysis models incorporating evidence-based outcome data with individual patient preferences regarding health states and willingness to pay could be extremely valuable for patients and clinicians when considering treatment options for patients with hip or knee OA.
References
Abellan Perpinan JM, Sanchez Martinez FI, Martinez Perez JE. [How should patients’ utilities be incorporated into clinical decisions? 2008 SESPAS Report][in Spanish]. Gac Sanit. 2008;22 (Suppl 1):179–185.
Barratt A. Evidence based medicine and shared decision making: the challenge of getting both evidence and preferences into health care. Patient Educ Couns. 2008;73:407–412.
Bennett KJ, Torrance GW, Moran LA, Smith F, Goldsmith CH. Health state utilities in knee replacement surgery: the development and evaluation of McKnee. J Rheumatol. 1997;24:1796–1805.
Birkmeyer JD, Sharp SM, Finlayson SR, Fisher ES, Wennberg JE. Variation profiles of common surgical procedures. Surgery. 1998;124:917–923.
Bozic KJ, Smith AR, Hariri S, Adeoye S, Gourville J, Maloney WJ, Parsley B, Rubash HE. The 2007 ABJS Marshall Urist Award: The impact of direct-to-consumer advertising in orthopaedics. Clin Orthop Relat Res. 2007;458:202–219.
Clark JP, Hudak PL, Hawker GA, Coyte PC, Mahomed NN, Kreder HJ, Wright JG. The moving target: a qualitative study of elderly patients’ decision-making regarding total joint replacement surgery. J Bone Joint Surg Am. 2004;86:1366–1374.
Deber RB, Kraetschmer N, Urowitz S, Sharpe N. Do people want to be autonomous patients? Preferred roles in treatment decision-making in several patient populations. Health Expect. 2007;10:248–258.
Drummond MF, Richardson WS, O’Brien BJ, Levine M, Heyland D. Users’ guides to the medical literature: XIII. How to use an article on economic analysis of clinical practice. A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA. 1997;277:1552–1557.
Hawker GA, Wright JG, Badley EM, Coyte PC, Consortium TAHSR. Perceptions of, and willingness to consider, total joint arthroplasty in a population-based cohort of individuals with disabling hip and knee arthritis. Arthritis Care & Research. 2004;51:635–641.
Holmes-Rovner M, Kroll J, Schmitt N, Rovner DR, Breer ML, Rothert ML, Padonu G, Talarczyk G. Patient satisfaction with health care decisions: the satisfaction with decision scale. Med Decis Making. 1996;16:58–64.
Hudak PL, Clark JP, Hawker GA, Coyte PC, Mahomed NN, Kreder HJ, Wright JG. “You’re perfect for the procedure! Why don’t you want it?” Elderly arthritis patients’ unwillingness to consider total joint arthroplasty surgery: a qualitative study. Med Decis Making. 2002;22:272–278.
Landro L. Lawmakers ask: what if patients shared in medical decisions. WSJ Blog; August 3, 2009.
Lurie JD, Bell JE, Weinstein J. What rate of utilization is appropriate in musculoskeletal care? Clin Orthop Relat Res. 2009;467:2506–2511.
Lurie JD, Weinstein JN. Shared decision-making and the orthopaedic workforce. Clin Orthop Relat Res. 2001;385:68–75.
Nord E. Cost-Value Analysis in Health Care. Making Sense Out of QALYs. Cambridge, UK: The Press Syndicate of the University of Cambridge; 1999.
Robinson R. Cost-utility analysis. BMJ. 1993;307:859–862.
Schneller ES, Wilson NA. Professionalism in 21st century professional practice: autonomy and accountability in orthopaedic surgery. Clin Orthop Relat Res. 2009;467:2561–2569.
Skinner J, Zhou W, Weinstein J. The influence of income and race on total knee arthroplasty in the United States. J Bone Joint Surg Am. 2006;88:2159–2166.
Soderman P, Malchau H, Herberts P, Zugner R, Regner H, Garellick G. Outcome after total hip arthroplasty: Part II. Disease-specific follow-up and the Swedish National Total Hip Arthroplasty Register. Acta Orthop Scand. 2001;72:113–119.
Sutton M. Personal paper: how to get the best health outcome for a given amount of money. BMJ. 1997;315:47–49.
Tosteson AN, Hammond CS. Quality-of-life assessment in osteoporosis: health-status and preference-based measures. Pharmacoeconomics. 2002;20:289–303.
Weinstein JN, Bronner KK, Morgan TS, Wennberg JE. Trends and geographic variations in major surgery for degenerative diseases of the hip, knee, and spine. Health Aff (Millwood). 2004;Suppl Web Exclusives:VAR81-89.
Weinstein JN, Clay K, Morgan TS. Informed patient choice: patient-centered valuing of surgical risks and benefits. Health Aff (Millwood). 2007;26:726–730.
Wennberg JE. Practice variation: implications for our health care system. Manag Care. 2004;13(9 suppl):3–7.
Acknowledgment
We thank David Shearer MD, MPH, for assistance in preparing this manuscript.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr. Bozic is a board member/officer of the Orthopaedic Research and Education Foundation (Rosemont, IL), the California Orthopaedic Association (Sacramento, CA), and the American Joint Replacement Registry (Rosemont, IL), and a paid consultant for Integrated Healthcare Association (Oakland, CA), United Health Care (Minnetonka, MN), Center for Medicare and Medicaid Services (MEDCAC) (Baltimore, MD), and the Pacific Business Group on Health (San Francisco, CA).
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Bozic, K.J., Chiu, V. Emerging Ideas: Shared Decision Making in Patients with Osteoarthritis of the Hip and Knee. Clin Orthop Relat Res 469, 2081–2085 (2011). https://doi.org/10.1007/s11999-010-1740-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-010-1740-7