Abstract
Background
Polyethylene wear debris is a major contributor to inflammation and the development of implant loosening, a leading cause of THA revisions. To reduce wear debris, highly crosslinked ultrahigh-molecular-weight polyethylene (UHMWPE) was introduced to improve wear properties of bearing surfaces. As highly crosslinked UHMWPE revision tissues are only now becoming available, it is possible to examine the presence and association of wear debris with inflammation in early implant loosening.
Questions/purposes
We asked: (1) Does the presence of UHMWPE wear debris in THA revision tissues correlate with innate and/or adaptive immune cell numbers? (2) Does the immune cell response differ between conventional and highly crosslinked UHMWPE cohorts?
Methods
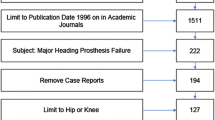
We collected tissue samples from revision surgery of nine conventional and nine highly crosslinked UHMWPE liners. Polarized light microscopy was used to determine 0.5- to 2-μm UHMWPE particle number/mm2, and immunohistochemistry was performed to determine macrophage, T cell, and neutrophil number/mm2.
Results
For the conventional cohort, correlations were observed between wear debris and the magnitude of individual patient macrophage (ρ = 0.70) and T cell responses (ρ = 0.71) and between numbers of macrophages and T cells (ρ = 0.77) in periprosthetic tissues. In comparison, the highly crosslinked UHMWPE cohort showed a correlation between wear debris and the magnitude of macrophage responses (ρ = 0.57) and between macrophage and T cell numbers (ρ = 0.68). Although macrophages and T cells were present in both cohorts, the highly crosslinked UHMWPE cohort had lower numbers, which may be associated with shorter implantation times.
Conclusions
The presence of wear debris and inflammation in highly crosslinked UHMWPE revision tissues may contribute to early implant loosening.




Similar content being viewed by others
References
Abu-Amer Y, Darwech I, Clohisy JC. Aseptic loosening of total joint replacements: mechanisms underlying osteolysis and potential therapies. Arthritis Res Ther. 2007;9(suppl 1):S6.
Altaf H. The Inflammatory Response to Particlulate Wear Debris in the Context of Total Hip Replacement [PhD dissertation]. London, UK: University of London; 2007.
Arora A, Song Y, Chun L, Huie P, Trindade M, Smith RL, Goodman S. The role of the TH1 and TH2 immune responses in loosening and osteolysis of cemented total hip replacements. J Biomed Mater Res A. 2003;64:693–697.
Athanasou NA, Pandey R, de Steiger R, Crook D, McLardy Smith PM. Diagnosis of infection by frozen section during revision arthroplasty. J Bone Joint Surg Br. 1995;77:28–33.
Baldwin L, Flanagan BF, McLaughlin PJ, Parkinson RW, Hunt JA, Williams DF. A study of tissue interface membranes from revision accord knee arthroplasty: the role of T lymphocytes. Biomaterials. 2002;23:3007–3014.
Basle MF, Bertrand G, Guyetant S, Chappard D, Lesourd M. Migration of metal and polyethylene particles from articular prostheses may generate lymphadenopathy with histiocytosis. J Biomed Mater Res. 1996;30:157–163.
Bauer TW, Parvizi J, Kobayashi N, Krebs V. Diagnosis of periprosthetic infection. J Bone Joint Surg Am. 2006;88:869–882.
Baxter RM, Ianuzzi A, Freeman TA, Kurtz SM, Steinbeck MJ. Distinct immunohistomorphologic changes in periprosthetic hip tissues from historical and highly crosslinked UHMWPE implant retrievals. J Biomed Mater Res A. 2010;95:68–78.
Beksac B, Salas A, Gonzalez Della Valle A, Salvati EA. Wear is reduced in THA performed with highly cross-linked polyethylene. Clin Orthop Relat Res. 2009;467:1765–1772.
Boyle WJ, Simonet WS, Lacey DL. Osteoclast differentiation and activation. Nature. 2003;423:337–342.
Bradford L, Baker DA, Graham J, Chawan A, Ries MD, Pruitt LA. Wear and surface cracking in early retrieved highly cross-linked polyethylene acetabular liners. J Bone Joint Surg Am. 2004;86:1271–1282.
Chun L, Yoon J, Song Y, Huie P, Regula D, Goodman S. The characterization of macrophages and osteoclasts in tissues harvested from revised total hip prostheses. J Biomed Mater Res. 1999;48:899–903.
Davies AP, Willert HG, Campbell PA, Learmonth ID, Case CP. An unusual lymphocytic perivascular infiltration in tissues around contemporary metal-on-metal joint replacements. J Bone Joint Surg Am. 2005;87:18–27.
Dean DD, Schwartz Z, Liu Y, Blanchard CR, Agrawal CM, Mabrey JD, Sylvia VL, Lohmann CH, Boyan BD. The effect of ultra-high molecular weight polyethylene wear debris on MG63 osteosarcoma cells in vitro. J Bone Joint Surg Am. 1999;81:452–461.
Elfick APD, Green SM, Krikler S, Unsworth A. The nature and dissemination of UHMWPE wear debris retrieved from periprosthetic tissue of THR. J Biomed Mater Res A. 2003;65:95–108.
Endo M, Tipper JL, Barton DC, Stone MH, Ingham E, Fisher J. Comparison of wear, wear debris and functional biological activity of moderately crosslinked and non-crosslinked polyethylenes in hip prostheses. Proc Inst Mech Eng H. 2002;216:111–122.
Feldman DS, Lonner JH, Desai P, Zuckerman JD. The role of intraoperative frozen sections in revision total joint arthroplasty. J Bone Joint Surg Am. 1995;77:1807–1813.
Frost S, Summers K, Singh B, Chess D, McCalden R, Bourne R, Rorabeck C, MacDonald S. The role of regulatory T cells in periprosthetic osteolysis following primary total hip arthroplasty. J Bone Joint Surg Br. 2008;90:38.
Gallo J, Kaminek P, Ticha V, Rihakova P, Ditmar R. Particle disease: a comprehensive theory of periprosthetic osteolysis: a review. Biomed Pap Med FacUniv Palacky Olomouc Czech Repub. 2002;146:21–28.
Gallo J, Mrazek F, Petrek M. Variation in cytokine genes can contribute to severity of acetabular osteolysis and risk for revision in patients with ABG 1 total hip arthroplasty: a genetic association study. BMC Med Genet. 2009;10:109–119.
Gallo J, Raska M, Mrazek F, Petrek M. Bone remodeling, particle disease and individual susceptibility to periprosthetic osteolysis. Physiol Res. 2008;57:339–349.
Geerdink CH, Grimm B, Ramakrishnan R, Rondhuis J, Verburg AJ, Tonino AJ. Crosslinked polyethylene compared to conventional polyethylene in total hip replacement: pre-clinical evaluation, in-vitro testing and prospective clinical follow-up study. Acta Orthop. 2006;77:719–725.
Gehrke T, Sers C, Morawietz L, Fernahl G, Neidel J, Frommelt L, Krenn V. Receptor activator of nuclear factor kappaB ligand is expressed in resident and inflammatory cells in aseptic and septic prosthesis loosening. Scand J Rheumatol. 2003;32:287–294.
Goldring SR, Clark CR, Wright TM. The problem in total joint arthroplasty: aseptic loosening. J Bone Joint Surg Am. 1993;75:799–801.
Goodman S, Wang JS, Regula D, Aspenberg P. T-lymphocytes are not necessary for particulate polyethylene-induced macrophage recruitment: histologic studies of the rat tibia. Acta Orthop Scand. 1994;65:157–160.
Goodman SB. Wear particulate and osteolysis. Orthop Clin North Am. 2005;36:41–48, vi.
Goodman SB. Wear particles, periprosthetic osteolysis and the immune system. Biomaterials. 2007;28:5044–5048.
Goodman SB, Huie P, Song Y, Schurman D, Maloney W, Woolson S, Sibley R. Cellular profile and cytokine production at prosthetic interfaces: study of tissues retrieved from revised hip and knee replacements. J Bone Joint Surg Br. 1998;80:531–539.
Goodman SB, Knoblich G, O’Connor M, Song Y, Huie P, Sibley R. Heterogeneity in cellular and cytokine profiles from multiple samples of tissue surrounding revised hip prostheses. J Biomed Mater Res. 1996;31:421–428.
Green TR, Fisher J, Stone M, Wroblewski BM, Ingham E. Polyethylene particles of a ‘critical size’ are necessary for the induction of cytokines by macrophages in vitro. Biomaterials. 1998;19:2297–2302.
Greenfield EM, Bi Y, Ragab AA, Goldberg VM, Van De Motter RR. The role of osteoclast differentiation in aseptic loosening. J Orthop Res. 2002;20:1–8.
Harris WH, Muratoglu OK. A review of current cross-linked polyethylenes used in total joint arthroplasty. Clin Orthop Relat Res. 2005;430:46–52.
Haynes DR, Crotti TN, Potter AE, Loric M, Atkins GJ, Howie DW, Findlay DM. The osteoclastogenic molecules RANKL and RANK are associated with periprosthetic osteolysis. J Bone Joint Surg Br. 2001;83:902–911.
Hercus B, Revell PA. Phenotypic characteristics of T lymphocytes in the interfacial tissue of aseptically loosened prosthetic joints. J Mater Sci Mater Med. 2001;12:1063–1067.
Ingham E, Fisher J. The role of macrophages in osteolysis of total joint replacement. Biomaterials. 2005;26:1271–1286.
Ito S, Matsumoto T, Enomoto H, Shindo H. Histological analysis and biological effects of granulation tissue around loosened hip prostheses in the development of osteolysis. J Orthop Sci. 2004;9:478–487.
Jacobs CA, Christensen CP, Greenwald AS, McKellop H. Clinical performance of highly cross-linked polyethylenes in total hip arthroplasty. J Bone Joint Surg Am. 2007;89:2779–2786.
Jacobs JJ, Campbell PA, Konttinen YT; Implant Wear Symposium 2007 Biologic Work Group. How has the biologic reaction to wear particles changed with newer bearing surfaces? J Am Acad Orthop Surg. 2008;16(suppl 1):S49–S55.
Jiranek W, Jasty M, Wang JT, Bragdon C, Wolfe H, Goldberg M, Harris W. Tissue response to particulate polymethylmethacrylate in mice with various immune deficiencies. J Bone Joint Surg Am. 1995;77:1650–1661.
Jones LC, Frondoza C, Hungerford DS. Immunohistochemical evaluation of interface membranes from failed cemented and uncemented acetabular components. J Biomed Mater Res. 1999;48:889–898.
Kim KJ, Chiba J, Rubash HE. In vivo and in vitro analysis of membranes from hip prostheses inserted without cement. J Bone Joint Surg Am. 1994;76:172–180.
Knahr K, Pospischill M, Kottig P, Schneider W, Plenk H Jr. Retrieval analyses of highly cross-linked polyethylene acetabular liners four and five years after implantation. J Bone Joint Surg Br. 2007;89:1036–1041.
Kobayashi A, Bonfield W, Kadoya Y, Yamac T, Freeman MA, Scott G, Revell PA. The size and shape of particulate polyethylene wear debris in total joint replacements. Proc Inst Mech Eng H. 1997;211:11–15.
Kurtz SM. The UHMWPE Biomaterials Handbook: Ultra-High Molecular Weight Polyethylene in Total Joint Replacement and Medical Devices. Burlington, MA: Academic Press; 2009.
Li TF, Santavirta S, Waris V, Lassus J, Lindroos L, Xu JW, Virtanen I, Konttinen YT. No lymphokines in T-cells around loosened hip prostheses. Acta Orthop Scand. 2001;72:241–247.
Lohmann CH, Dean DD, Bonewald LF, Schwartz Z, Boyan BD. Nitric oxide and prostaglandin E2 production in response to ultra-high molecular weight polyethylene particles depends on osteoblast maturation state. J Bone Joint Surg Am. 2002;84:411–419.
Looney RJ, Schwarz EM, Boyd A, O’Keefe RJ. Periprosthetic osteolysis: an immunologist’s update. Curr Opin Rheumatol. 2006;18:80–87.
Mahendra G, Pandit H, Kliskey K, Murray D, Gill HS, Athanasou N. Necrotic and inflammatory changes in metal-on-metal resurfacing hip arthroplasties. Acta Orthop. 2009;80:653–659.
Maitra R, Clement CC, Scharf B, Crisi GM, Chitta S, Paget D, Purdue PE, Cobelli N, Santambrogio L. Endosomal damage and TLR2 mediated inflammasome activation by alkane particles in the generation of aseptic osteolysis. Mol Immunol. 2009;47:175–184.
Malik MH, Bayat A, Jury F, Kay PR, Ollier WE. Genetic susceptibility to total hip arthroplasty failure: positive association with mannose-binding lectin. J Arthroplasty. 2007;22:265–270.
Malik MH, Bayat A, Jury F, Ollier WE, Kay PR. Genetic susceptibility to hip arthroplasty failure: association with the RANK/OPG pathway. Int Orthop. 2006;30:177–181.
Malik MH, Jury F, Bayat A, Ollier WE, Kay PR. Genetic susceptibility to total hip arthroplasty failure: a preliminary study on the influence of matrix metalloproteinase 1, interleukin 6 polymorphisms and vitamin D receptor. Ann Rheum Dis. 2007;66:1116–1120.
Mall NA, Nunley RM, Zhu JJ, Maloney WJ, Barrack RL, Clohisy JC. The incidence of acetabular osteolysis in young patients with conventional versus highly crosslinked polyethylene. Clin Orthop Relat Res. 2010 September 8 [Epub ahead of print].
McKellop H, Shen FW, Lu B, Campbell P, Salovey R. Development of an extremely wear-resistant ultra high molecular weight polyethylene for total hip replacements. J Orthop Res. 1999;17:157–167.
Minoda Y, Kobayashi A, Sakawa A, Aihara M, Tada K, Sugama R, Iwakiri K, Ohashi H, Takaoka K. Wear particle analysis of highly crosslinked polyethylene isolated from a failed total hip arthroplasty. J Biomed Mater Res B Appl Biomater. 2008;86B:501–505.
Mirra JM, Marder RA, Amstutz HC. The pathology of failed total joint arthroplasty. Clin Orthop Relat Res. 1982;170:175–183.
Muratoglu OK, Bragdon CR, O’Connor DO, Jasty M, Harris WH. A novel method of cross-linking ultra-high-molecular-weight polyethylene to improve wear, reduce oxidation, and retain mechanical properties. Recipient of the 1999 HAP Paul Award. J Arthroplasty. 2001;16:149–160.
Olyslaegers C, Defoort K, Simon JP, Vandenberghe L. Wear in conventional and highly cross-linked polyethylene cups: a 5-year follow-up study. J Arthroplasty. 2008;23:489–494.
Pandey R, Berendt AR, Athanasou NA. Histological and microbiological findings in non-infected and infected revision arthroplasty tissues. The OSIRIS Collaborative Study Group. Oxford Skeletal Infection Research and Intervention Service. Arch Orthop Trauma Surg. 2000;120:570–574.
Park YS, Moon YW, Lim SJ, Yang JM, Ahn G, Choi YL. Early osteolysis following second-generation metal-on-metal hip replacement. J Bone Joint Surg Am. 2005;87:1515–1521.
Purdue PE, Koulouvaris P, Potter HG, Nestor BJ, Sculco TP. The cellular and molecular biology of periprosthetic osteolysis. Clin Orthop Relat Res. 2007;454:251–261.
Ren WP, Markel DC, Zhang R, Peng X, Wu B, Monica H, Wooley PH. Association between UHMWPE particle-induced inflammatory osteoclastogenesis and expression of RANKL, VEGF, and Flt-1 in vivo. Biomaterials. 2006;27:5161–5169.
Revell PA. The combined role of wear particles, macrophages and lymphocytes in the loosening of total joint prostheses. J R Soc Interface. 2008;5:1263–1278.
Ries MD, Scott ML, Jani S. Relationship between gravimetric wear and particle generation in hip simulators: conventional compared with cross-linked polyethylene. J Bone Joint Surg Am. 2001;83(suppl 2 pt 2):116–122.
Roato I, Caldo D, D’Amico L, D’Amelio P, Godio L, Patane S, Astore F, Grappiolo G, Boggio M, Scagnelli R, Molfetta L, Ferracini R. Osteoclastogenesis in peripheral blood mononuclear cell cultures of periprosthetic osteolysis patients and the phenotype of T cells localized in periprosthetic tissues. Biomaterials. 2010;31:7519–7525.
Sabokbar A, Fujikawa Y, Neale S, Murray DW, Athanasou NA. Human arthroplasty derived macrophages differentiate into osteoclastic bone resorbing cells. Ann Rheum Dis. 1997;56:414–420.
Saikko V, Calonius O, Keranen J. Wear of conventional and cross-linked ultra-high-molecular-weight polyethylene acetabular cups against polished and roughened CoCr femoral heads in a biaxial hip simulator. J Biomed Mater Res. 2002;63:848–853.
Sandhu J, Waddell JE, Henry M, Boynton EL. The role of T cells in polyethylene particulate induced inflammation. J Rheumatol. 1998;25:1794–1799.
Shanbhag AS, Bailey HO, Hwang DS, Cha CW, Eror NG, Rubash HE. Quantitative analysis of ultrahigh molecular weight polyethylene (UHMWPE) wear debris associated with total knee replacements. J Biomed Mater Res. 2000;53:100–110.
Shanbhag AS, Kaufman AM, Hayata K, Rubash HE. Assessing osteolysis with use of high-throughput protein chips. J Bone Joint Surg Am. 2007;89:1081–1089.
Sundfeldt M, Carlsson LV, Johansson CB, Thomsen P, Gretzer C. Aseptic loosening, not only a question of wear: a review of different theories. Acta Orthop. 2006;77:177–197.
Taki N, Tatro JM, Nalepka JL, Togawa D, Goldberg VM, Rimnac CM, Greenfield EM. Polyethylene and titanium particles induce osteolysis by similar, lymphocyte-independent, mechanisms. J Orthop Res. 2005;23:376–383.
Tipper JL, Galvin A, Williams S, McEwen HM, Stone MH, Ingham E, Fisher J. Isolation and characterization of UHMWPE wear particles down to ten nanometers in size from in vitro hip and knee joint simulators. J Biomed Mater Res A. 2006;78:473–480.
Ulrich SD, Seyler TM, Bennett D, Delanois RE, Saleh KJ, Thongtrangan I, Kuskowski M, Cheng EY, Sharkey PF, Parvizi J, Stiehl JB, Mont MA. Total hip arthroplasties: what are the reasons for revision? Int Orthop. 2008;32:597–604.
Urban RM, Jacobs JJ, Tomlinson MJ, Gavrilovic J, Black J, Peoc’h M. Dissemination of wear particles to the liver, spleen, and abdominal lymph nodes of patients with hip or knee replacement. J Bone Joint Surg Am. 2000;82:457–476.
Willert HG, Buchhorn GH, Fayyazi A, Flury R, Windler M, Koster G, Lohmann CH. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints: a clinical and histomorphological study. J Bone Joint Surg Am. 2005;87:28–36.
Williams PA, Yamamoto K, Masaoka T, Oonishi H, Clarke IC. Highly crosslinked polyethylenes in hip replacements: improved wear performance of paradox? STLE Tribology Trans. 2007;50:227–290.
Yamamoto K, Clarke IC, Masaoka T, Oonishi H, Williams PA, Good VD, Imakiire A. Microwear phenomena of ultrahigh molecular weight polyethylene cups and debris morphology related to gamma radiation dose in simulator study. J Biomed Mater Res. 2001;56:65–73.
Acknowledgments
We thank the participating physicians from the Rothman Institute (Dr. Javad Parvizi) and Case Western Reserve University (Dr. Victor Goldberg) who were instrumental in procuring periprosthetic hip tissue samples. We also are grateful to Lauren L. Jablonowski and Robin Stevenson for their contributions to multiple aspects of tissue sample processing.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors (SMK, MJS) have received funding from the National Institute of Health and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIH R01 AR47904).
Each author certifies that his or her institution has approved the human protocols for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Drexel University.
About this article
Cite this article
Baxter, R.M., Freeman, T.A., Kurtz, S.M. et al. Do Tissues From THA Revision of Highly Crosslinked UHMWPE Liners Contain Wear Debris and Associated Inflammation?. Clin Orthop Relat Res 469, 2308–2317 (2011). https://doi.org/10.1007/s11999-010-1713-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-010-1713-x