Abstract
Purpose of Review
This review presents an overview of how advanced imaging techniques may help to overcome shortcomings of anatomical MRI for response assessment in patients with brain metastases who are undergoing stereotactic radiosurgery, immunotherapy, or combinations thereof.
Recent Findings
Study results suggest that parameters derived from amino acid PET, diffusion- and perfusion-weighted MRI, MR spectroscopy, and newer MRI methods are particularly helpful for the evaluation of the response to radiosurgery or checkpoint inhibitor immunotherapy and provide valuable information for the differentiation of radiotherapy-induced changes such as radiation necrosis from brain metastases. The evaluation of these imaging modalities is also of great interest in the light of emerging high-throughput analysis methods such as radiomics, which allow the acquisition of additional data at a low cost.
Summary
Preliminary results are promising and should be further evaluated. Shortcomings are different levels of PET and MRI standardization, the number of patients enrolled in studies, and the monocentric and retrospective character of most studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stereotactic radiosurgery delivers focused, highly conformal, ionizing radiation to a tumor delineated using high-resolution imaging, with low toxicity to adjacent brain structures. Its precision is particularly valuable for tumors located within critical functional tissue such as the brainstem, the optic pathway, or basal ganglia. In patients with brain metastases, randomized controlled and prospective trials have demonstrated higher local control rates and improved preservation of cognitive functions after stereotactic radiosurgery compared to whole-brain radiotherapy [1,2]. Additionally, in terms of overall survival, stereotactic radiosurgery without whole-brain radiotherapy in patients with 5–10 brain metastases is non-inferior to that in patients with 2–4 brain metastases [3]. Its minimal-invasive nature makes it an attractive alternative to neurosurgical resection. Stereotactic radiosurgery can act as the primary modality in treating brain metastasis or serve as (neo)adjuvant treatment to surgery.
The advent of immunotherapy using immune checkpoint inhibitors has considerably improved the prognosis of extracranial cancer, especially in patients with melanoma, lung cancer, or breast cancer. Recent trials have demonstrated that patients with brain metastases may also benefit from these agents. In particular, the blockade of immune checkpoints such as the cytotoxic T lymphocyte-associated protein 4 or programmed cell death receptor-1 axis (PD-1 and PD-L1) has resulted in a significant improvement of overall survival [4,5,6,7].
Furthermore, besides targeted therapies, checkpoint inhibitor immunotherapy also allows for the concurrent delivery with radiosurgery, with possible additive or synergistic effects, expediting the treatment of both extracranial and intracranial metastatic disease. For example, data from 150 patients with more than 1000 brain metastases revealed that the application of radiosurgery concurrent to checkpoint inhibitor immunotherapy (defined as ± 5 biological half-lives) was associated with the highest overall response rate and most extended response durability [8].
However, imaging findings on anatomical contrast-enhanced MRI following radiosurgery combined with targeted therapies or checkpoint inhibitor immunotherapy may be highly variable and equivocal, making the differentiation of treatment-related effects from local brain metastases recurrence challenging [9••,10••]. For example, a checkpoint inhibitor-related pseudoprogression or even symptomatic radiation necrosis may occur [11,12,13,14,15,16,17], considerably affecting the response assessment.
For response assessment, the Response Assessment in Neuro-Oncology (RANO) Brain Metastases committee reported consensus criteria for non-measurable (e.g., contrast-enhancing lesions < 10 mm in diameter on anatomical MRI, leptomeningeal disease, cyst-only lesions) and measurable brain metastases (contrast-enhancing lesions of ≥ 10 mm) [18]. Importantly, response evaluation for non-measurable metastases is based only on qualitative assessments of present, absent, and unequivocal disease progression on follow-up MR imaging [18]. Furthermore, patients with small brain metastases < 5–10 mm in diameter are not infrequent and have, therefore, non-measurable disease according to these criteria. Thus, these considerations make the inclusion of such patients in clinical trials involving newer treatment options challenging.
We here aim at providing an overview of alternative imaging techniques that may help to overcome these challenges.
Potential of Advanced MRI
While anatomical MRI provides detailed structural information with high spatial resolution on both the healthy brain and brain tumors, advanced MRI methods provide additional quantitative information at the functional, physiologic, and molecular levels. Due to the increasing number of available MRI scanners with higher field strengths (i.e., an ultra-high field at 7 T) and spatial resolution, smaller lesions (< 5–10 mm in diameter) can also be evaluated. Parameters obtained from perfusion- or diffusion-based MRI and MR spectroscopy are most frequently used for advanced MR imaging. Current MRI research also focuses on the chemical exchange saturation transfer (CEST), including the amide proton transfer for brain tumor imaging.
Early Response Assessment Using Advanced MRI
Predicting which patients are likely to demonstrate a favorable response to radiosurgery within a short period has a significant clinical impact. For evaluating the response to radiosurgery in patients with brain metastases using perfusion MRI, predominantly, the relative cerebral blood volume [19] and flow [20], and the efflux rate of gadolinium contrast from blood plasma into the tissue [21,22,23] have been evaluated. These studies’ main finding is that early changes of these parameters within the first weeks (range, 6–12 weeks) after stereotactic radiosurgery allow predicting long-term response (range, 6–12 months). A more recent study evaluated newer perfusion MRI metrics such as intravoxel incoherent motion in comparison to the relative cerebral blood volume for response assessment at baseline, 1 week, and 1 month after stereotactic radiosurgery [24]. However, these parameters could not differentiate responders from non-responders.
Another option for the evaluation of response to radiosurgery in patients with brain metastases is diffusion MRI. Predominantly apparent diffusion coefficients calculated from diffusion MRI have been evaluated. A few studies have suggested that these values increased during follow-up after radiosurgery in patients showing a treatment response [25,26,27]. Conversely, another study reported that especially lower apparent diffusion coefficients already at 1 week and 1 month identified responders to radiosurgery [28]. Lee and colleagues described that pretreatment apparent diffusion coefficients could predict response with a sensitivity and specificity of 86% and 73%, respectively [29].
Single voxel proton MR spectroscopy data obtained from 26 patients with brain metastases before treatment suggested that both a higher lipid signal at baseline and a decrease of the lipid peak at follow-up are associated with a favorable outcome [30].
Desmond and co-workers used CEST imaging, including amide proton transfer-weighted images, to evaluate radiosurgery effects at 1 week and 1 month compared to baseline imaging in 25 patients with brain metastases [31]. The study results suggest that various CEST imaging parameter changes can predict tumor volume changes at 1 month after stereotactic radiosurgery, indicating its potential for early response assessment.
Differentiation of Treatment-Related Effects from Brain Metastasis Recurrence Using Advanced MRI
Chuang and colleagues [32] examined the value of various parameters derived from perfusion MRI and MR spectroscopy to differentiate treatment-related necrosis from brain metastasis recurrence. The main finding of that meta-analysis, including 95 patients with brain metastases, was that MR spectroscopy and perfusion MRI might increase the accuracy of differentiating recurrent tumors from radiation-induced necrosis. In particular, various MR spectroscopy metabolite ratios and the relative cerebral blood volume derived from perfusion MRI in contrast-enhancing lesions were significantly different in recurrent brain metastases than radiation necrosis. Notably, available studies on perfusion-weighted MR imaging reported a considerable variability of diagnostic performance (i.e., sensitivity and specificity) and thresholds for relative cerebral blood volumes [33,34,35,36,37,38]. Although this technique separates radiation-induced changes from brain metastases recurrence with reasonable accuracy in individual studies, the significant variability of reported thresholds and methodology indicates that further studies and standardization are warranted.
In comparison to relative cerebral blood volumes and amino acid PET parameters, apparent diffusion coefficients calculated from diffusion MRI do not seem to be of value for distinguishing of radiation-induced injury from brain metastases recurrence after stereotactic radiotherapy of brain metastases [39,40].
A preliminary study in 16 patients treated with radiosurgery suggested that various amide proton transfer CEST MR imaging metrics allow a statistically significant separation between radiation necrosis and brain metastases recurrence [41].
Potential of Pet
For brain tumor imaging using PET, many radiotracers are available, which target a high number of molecular and metabolic processes with considerable specificity [42,43,44]. Especially radiolabeled amino acids are of particular interest for PET imaging of brain metastases because of their increased uptake in metastatic tissue but low uptake in the healthy brain parenchyma, resulting in an improved tumor-to-brain contrast [45]. Recently, the PET RANO group has analyzed the clinical value of amino acid PET in the diagnostic evaluation in this group of patients. This report highlights the value of this imaging technique over and above conventional MRI especially for differentiating treatment-related changes from brain metastases recurrence [46]. Within the group of amino acid PET tracers, especially in Europe, the tracer O-(2-[18F]-fluoroethyl)-l-tyrosine (FET) is frequently used [43••, 47, 48]. In both gliomas and brain metastases, increased uptake of radiolabeled amino acids is related to transporters of the l-type (subtypes LAT1/2), which are overexpressed in these types of tumor tissue [49,50,51,52]. Thus, the LAT transporter overexpression in brain metastases makes these tumors a compelling target for amino acid PET imaging [52].
Furthermore, to evaluate the anti-tumoral activity of various treatment options in patients with brain metastases, other tracers than radiolabeled amino acids may also be of interest. For example, the radiolabeled analog to the nucleoside thymidine 3′-deoxy-3′-[18F]-fluorothymidine (FLT) was developed to assess cellular proliferation by tracking the thymidine salvage pathway [53].
Moreover, recent efforts have focused on Immuno-PET, which uses antibody-based radiotracers to image specifically the expression of tumor-associated antigens such as immune checkpoints on T-cells or tumor cells [54]. Additionally, advances in antibody-engineering provide the prerequisite to develop antibody-based molecules coupled with anticancer drugs for the use as Immuno-PET radiotracers.
Early Response Assessment Using PET
A recent study in a larger series of patients (n=40) with melanoma or non-small cell lung cancer brain metastases (n=107) treated with checkpoint inhibitors or targeted therapy combined with radiosurgery reported that FET PET provides important diagnostic information in terms of response assessment [55••]. In contrast to response determination based on contrast-enhanced MRI changes, metabolic responders on FET PET had a significantly longer progression-free survival.
A prospective PET study evaluated the tracer FLT to determine cellular proliferation as a surrogate marker for treatment response [56]. Data suggested that in a subset of patients with melanoma brain metastases treated with checkpoint inhibitors or targeted therapy, metabolic responders may have improved survival. Importantly, FLT PET responders showed reduced proliferative tumor activity despite predominantly unchanged contrast enhancement on MRI.
The steadily increasing use of immune checkpoint inhibitors has also prompted the development of PET tracers to image the expression of immune checkpoints PD-1 or PD-L1 [57]. A first-in-human study [58] suggests that Immuno-PET using nivolumab labeled with Zirconium-89 may be valuable for response assessment. In that study, all extracranial non-small cell lung cancers of 13 patients exhibited increased uptake in whole-body PET/CT scans. Furthermore, 2 of these 13 patients had brain metastases, and tracer accumulation in the majority, but not in all brain metastases, was observed. This finding was most probably related to small lesion size or low PD-1 expression [58].
Differentiation of Treatment-Related Effects from Brain Metastasis Recurrence Using PET
Mostly amino acid PET has been studied to differentiate radiosurgery-induced changes such as necrosis from brain metastasis recurrence. For example, PET using [11C]-methyl-l-methionine (MET) and 3,4-dihydroxy-6-[18F]-fluoro-l-phenylalanine (FDOPA) has consistently demonstrated high sensitivity and specificity in the range of 80% for this clinically significant differentiation [59,60,61,62]. Another study compared FDOPA PET with perfusion MRI for this indication [37]. In that study, FDOPA PET parameters out-performed perfusion MRI metrics. Another study suggested that the diagnostic performance of MET PET also seems to be superior to apparent diffusion coefficients calculated from diffusion-weighted MR imaging [39]. Compared to MET and FDOPA PET, static and dynamic FET PET parameters showed similar diagnostic performance for this differentiation with high sensitivity and specificity of 80–90% [63,64,65].
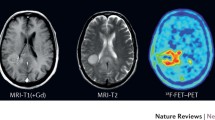
A further study in patients with melanoma brain metastases suggested that amino acid PET using FET can identify checkpoint inhibitor-related pseudoprogression [66•]. In that pilot study comprising 5 patients, imaging findings were correlated with the clinical course after the initiation of the checkpoint inhibitor therapy with ipilimumab. In the case of pseudoprogression, FET PET showed in contrast to the progressive MRI only insignificant tracer uptake, and the patient had a favorable outcome with a progression-free survival longer than 6 months. An illustrative case with treatment-related effects following combined immune checkpoint blockade with ipilimumab and nivolumab identified using FDOPA PET is presented in Fig. 1.
Contrast-enhanced MRI and FDOPA PET of a 56-year-old male patient with a PD-L1-positive and BRAF-mutated malignant melanoma with metastases in the liver, axillary and inguinal lymph nodes, lung, and brain (i.e., in the left cerebellum, left insular cortex, and right precentral and postcentral gyrus). The systemic first-line therapy consisted of encorafenib and binimetinib; the brain metastases were treated concurrently with radiosurgery. After 10 months, new metastases in the lung and left kidney prompted a change in treatment. Radiologically, the brain metastases showed no signs of tumor progression. Two months after initiation of immune checkpoint blockade with ipilimumab and nivolumab, MRI suggested tumor progression of the pretreated metastasis in the left cerebellum (bottom row). In contrast, additional FDOPA PET showed no increased metabolic activity indicating checkpoint inhibitor-related pseudoprogression.
Potential of Radiomics
Although various imaging modalities are available for patients with brain tumors, including brain metastases, clinical image interpretation usually uses only a fraction of the underlying complex, high-dimensional digital information from the acquired imaging data. The growing availability of high-performance computing allows the extraction of quantitative imaging features from medical images that are usually beyond human perception. Especially, radiomics allows the extraction of quantitative features from standard-of-care neuroimages from CT, MRI, or PET, and may provide additional, potentially relevant diagnostic information for decision-making [67]. Since these features’ computation is possible on already acquired neuroimages during routine follow-up, this information can be provided at a low cost. Furthermore, radiomics features can be used either independently or combined with other clinical information to generate predictive mathematical models. Subsequently, these models can be tested for various important diagnostic indications in neuro-oncology, e.g., to differentiate between treatment-related changes and brain tumor recurrence or to predict treatment response.
Radiomics can be divided into feature-based and deep learning-based radiomics [68]. Feature-based radiomics (e.g., textural features) use predefined imaging features extracted from preprocessed and segmented medical images. Using machine learning techniques, a subset of these features is selected for the model generation related to the research question. On the other hand, deep learning-based radiomics does not require image segmentation or predefined imaging features. Here, artificial neural networks imitate the human visual system’s function and automatically extract high-dimensional features from the original images at different abstraction levels. Subsequently, these artificial neural networks learn autonomously characteristic patterns and classify them.
In patients with brain metastases, the additional diagnostic value of both conventional/advanced MRI [69,70] and amino acid PET radiomics [71,72] has been reported to differentiate radiation-induced changes from brain metastases recurrence. Therefore, the question arises whether a combined MRI and amino acid PET radiomics analysis encode more diagnostic information for this differentiation than either modality alone. Accordingly, a more recent study has addressed the value of combining FET PET and MRI radiomics for this critical question [73•]. Fifty-two patients with progressive contrast-enhancing lesions on MRI after radiosurgery were additionally investigated using FET PET. Textural features were extracted from MR and FET PET images. Feature selection was limited to a maximum of 5 parameters to avoid overfitting, and logistic regression models were generated for the combined PET/MRI features and each modality alone. The combination of MRI and FET PET features achieved the highest diagnostic accuracy of 89% (specificity, 96%; sensitivity, 85%), supporting the use of multimodal radiomics analyses for clinically relevant diagnostic purposes.
Conclusion
The current body of literature suggests that both amino acid PET and advanced MRI methods are of great value for assessing brain metastases with the potential to overcome the limitations of conventional MRI. On the other hand, it should be noted that the available studies in the field have predominantly retrospective character, were performed mostly in single centers, and typically included only a low number of patients. Prospective studies with a higher number of patients, ideally in a multicenter setting with standardized MR imaging protocols, are warranted to overcome these shortcomings.
From the methodological point of view, amino acid PET is a robust and attractive approach for clinicians. It provides comparable results across different scanners, which is related to national and international efforts regarding the standardization of PET acquisition and evaluation for brain tumor imaging. Recently, joint practice guidelines were developed by the European Association of Nuclear Medicine (EANM), the Society of Nuclear Medicine and Molecular Imaging (SNMMI), the European Association of Neuro-Oncology (EANO), and the RANO PET committee [74••]. In contrast, although the standardization of both MRI acquisition protocols and advanced MRI methods is ongoing [75, 76••], to date, self-developed or self-optimized MRI acquisition protocols, as well as pre- and post-processing tools, are frequently used in clinical routine, which hampers comparability and reproducibility of the results.
To conclude, advanced MRI combined with amino acid PET has the potential to become an essential diagnostic tool for improving the clinical management of patients with brain metastases. The evaluation of these imaging modalities is also of great interest in the light of emerging high-throughput analysis methods such as radiomics. The increasing advent of hybrid PET/MRI scanners offers a great research potential for comparative studies using both modalities in a single session, but the clinical benefits of hybrid imaging need to be balanced against this approach’s relatively high costs. Furthermore, the increasing availability of ultra-high field MRI scanners with higher spatial resolution may help develop novel advanced MRI techniques in neuro-oncology because almost all MRI contrasts benefit from the improved signal-to-noise ratio. Finally, further implementation of various advanced MRI methods, as well as amino acid PET in clinical routine, requires the validation of neuroimaging findings by neuropathology.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kocher M, Soffietti R, Abacioglu U, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26,001 study. J Clin Oncol. 2011;29(2):134–41.
Brown PD, Jaeckle K, Ballman KV, et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. Jama. 2016;316(4):401–9.
Yamamoto M, Serizawa T, Shuto T, et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol. 2014;15(4):387–95.
Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–23.
Kluger HM, Chiang V, Mahajan A, et al. Long-term survival of patients with melanoma with active brain metastases treated with pembrolizumab on a phase II trial. J Clin Oncol. 2019;37(1):52–60.
Tawbi HA, Forsyth PA, Algazi A, et al. combined nivolumab and ipilimumab in melanoma metastatic to the brain. N Engl J Med. 2018;379(8):722–30.
Long GV, Atkinson V, Lo S, et al. Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: a multicentre randomised phase 2 study. Lancet Oncol. 2018;19(5):672–81.
Kotecha R, Kim JM, Miller JA, et al. The impact of sequencing PD-1/PD-L1 inhibitors and stereotactic radiosurgery for patients with brain metastasis. Neuro Oncol. 2019;21(8):1060–8.
•• Okada H, Weller M, Huang R, et al. Immunotherapy response assessment in neuro-oncology: a report of the RANO working group. Lancet Oncol. 2015; 16(15):e534–542. iRANO group report addressing the clinical problem of immunotherapy-related pseudoprogression.
•• Galldiks N, Kocher M, Ceccon G, et al. Imaging challenges of immunotherapy and targeted therapy in patients with brain metastases: response, progression, and pseudoprogression. Neuro Oncol. 2020; 22(1):17–30. Comprehensive review of imaging challenges following various treatment options for brain metastases.
Martin AM, Cagney DN, Catalano PJ, et al. Immunotherapy and symptomatic radiation necrosis in patients with brain metastases treated with stereotactic radiation. JAMA Oncol. 2018;4(8):1123–4.
Alomari AK, Cohen J, Vortmeyer AO, et al. Possible interaction of anti-PD-1 therapy with the effects of radiosurgery on brain metastases. Cancer Immunol Res. 2016;4(6):481–7.
Cohen JV, Alomari AK, Vortmeyer AO, et al. Melanoma brain metastasis pseudoprogression after pembrolizumab treatment. Cancer Immunol Res. 2016;4(3):179–82.
Colaco RJ, Martin P, Kluger HM, Yu JB, Chiang VL. Does immunotherapy increase the rate of radiation necrosis after radiosurgical treatment of brain metastases? J Neurosurg. 2016;125(1):17–23.
Weingarten N, Kruser TJ, Bloch O. Symptomatic radiation necrosis in brain metastasis patients treated with stereotactic radiosurgery and immunotherapy. Clin Neurol Neurosurg. 2019;179:14–8.
Zhuang H, Tao L, Wang X, et al. Tyrosine kinase inhibitor resistance increased the risk of cerebral radiation necrosis after stereotactic radiosurgery in brain metastases of non-small-cell lung cancer: a multi-institutional retrospective case-control study. Front Oncol. 2020;10:12.
Trommer-Nestler M, Marnitz S, Kocher M, et al. Robotic stereotactic radiosurgery in melanoma patients with brain metastases under simultaneous anti-PD-1 treatment. Int J Mol Sci 2018; 19(9).
Lin NU, Lee EQ, Aoyama H, et al. Response assessment criteria for brain metastases: proposal from the RANO group. Lancet Oncol. 2015;16(6):e270–8.
Essig M, Waschkies M, Wenz F, Debus J, Hentrich HR, Knopp MV. Assessment of brain metastases with dynamic susceptibility-weighted contrast-enhanced MR imaging: initial results. Radiology. 2003;228(1):193–9.
Weber MA, Thilmann C, Lichy MP, et al. Assessment of irradiated brain metastases by means of arterial spin-labeling and dynamic susceptibility-weighted contrast-enhanced perfusion MRI: initial results. Invest Radiol. 2004;39(5):277–87.
Taunk NK, Oh JH, Shukla-Dave A, et al. Early posttreatment assessment of MRI perfusion biomarkers can predict long-term response of lung cancer brain metastases to stereotactic radiosurgery. Neuro Oncol. 2018;20(4):567–75.
Kuchcinski G, Le Rhun E, Cortot AB, et al. Dynamic contrast-enhanced MR imaging pharmacokinetic parameters as predictors of treatment response of brain metastases in patients with lung cancer. Eur Radiol. 2017;27(9):3733–43.
Jakubovic R, Sahgal A, Soliman H, et al. Magnetic resonance imaging-based tumour perfusion parameters are biomarkers predicting response after radiation to brain metastases. Clin Oncol (R Coll Radiol). 2014;26(11):704–12.
Kapadia A, Mehrabian H, Conklin J, et al. Temporal evolution of perfusion parameters in brain metastases treated with stereotactic radiosurgery: comparison of intravoxel incoherent motion and dynamic contrast enhanced MRI. J Neurooncol. 2017;135(1):119–27.
Chen Z, Zu J, Li L, Lu X, Ni J, Xu J. Assessment of stereotactic radiosurgery treatment response for brain metastases using MRI based diffusion index. Eur J Radiol Open. 2017;4:84–8.
Huang CF, Chiou SY, Wu MF, Tu HT, Liu WS, Chuang JC. Apparent diffusion coefficients for evaluation of the response of brain tumors treated by Gamma Knife surgery. J Neurosurg. 2010;113:97–104.
Huang CF, Chou HH, Tu HT, Yang MS, Lee JK, Lin LY. Diffusion magnetic resonance imaging as an evaluation of the response of brain metastases treated by stereotactic radiosurgery. Surg Neurol. 2008;69(1):62–8.
Jakubovic R, Zhou S, Heyn C, et al. The predictive capacity of apparent diffusion coefficient (ADC) in response assessment of brain metastases following radiation. Clin Exp Metastasis. 2016;33(3):277–84.
Lee CC, Wintermark M, Xu Z, Yen CP, Schlesinger D, Sheehan JP. Application of diffusion-weighted magnetic resonance imaging to predict the intracranial metastatic tumor response to gamma knife radiosurgery. J Neurooncol. 2014;118(2):351–61.
Sjobakk TE, Johansen R, Bathen TF, et al. Metabolic profiling of human brain metastases using in vivo proton MR spectroscopy at 3 T. BMC Cancer. 2007;7:141.
Desmond KL, Mehrabian H, Chavez S, et al. Chemical exchange saturation transfer for predicting response to stereotactic radiosurgery in human brain metastasis. Magn Reson Med. 2017;78(3):1110–20.
Chuang MT, Liu YS, Tsai YS, Chen YC, Wang CK. Differentiating radiation-induced necrosis from recurrent brain tumor using mr perfusion and spectroscopy: a meta-analysis. PloS one. 2016;11(1):e0141438.
Mitsuya K, Nakasu Y, Horiguchi S, et al. Perfusion weighted magnetic resonance imaging to distinguish the recurrence of metastatic brain tumors from radiation necrosis after stereotactic radiosurgery. J Neurooncol. 2010;99(1):81–8.
Barajas RF, Chang JS, Sneed PK, Segal MR, McDermott MW, Cha S. Distinguishing recurrent intra-axial metastatic tumor from radiation necrosis following gamma knife radiosurgery using dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. AJNR Am J Neuroradiol. 2009;30:367–72.
Huang J, Wang AM, Shetty A, et al. Differentiation between intra-axial metastatic tumor progression and radiation injury following fractionated radiation therapy or stereotactic radiosurgery using MR spectroscopy, perfusion MR imaging or volume progression modeling. Magn Reson Imaging. 2011;29(7):993–1001.
Hoefnagels FW, Lagerwaard FJ, Sanchez E, et al. Radiological progression of cerebral metastases after radiosurgery: assessment of perfusion MRI for differentiating between necrosis and recurrence. J Neurol. 2009;256(6):878–87.
Cicone F, Minniti G, Romano A, et al. Accuracy of F-DOPA PET and perfusion-MRI for differentiating radionecrotic from progressive brain metastases after radiosurgery. Eur J Nucl Med Mol Imaging. 2015;42(1):103–11.
Hatzoglou V, Yang TJ, Omuro A, et al. A prospective trial of dynamic contrast-enhanced MRI perfusion and fluorine-18 FDG PET-CT in differentiating brain tumor progression from radiation injury after cranial irradiation. Neuro Oncol. 2016;18(6):873–80.
Tomura N, Kokubun M, Saginoya T, Mizuno Y, Kikuchi Y. Differentiation between treatment-induced necrosis and recurrent tumors in patients with metastatic brain tumors: comparison among (11)C-methionine-PET, FDG-PET, MR permeability imaging, and MRI-ADC-preliminary results. AJNR Am J Neuroradiol. 2017;38(8):1520–7.
Knitter JR, Erly WK, Stea BD, et al. Interval change in diffusion and perfusion mri parameters for the assessment of pseudoprogression in cerebral metastases treated with stereotactic radiation. AJR Am J Roentgenol. 2018;211(1):168–75.
Mehrabian H, Desmond KL, Soliman H, Sahgal A, Stanisz GJ. Differentiation between radiation necrosis and tumor progression using chemical exchange saturation transfer. Clin Cancer Res. 2017;23(14):3667–75.
Galldiks N, Lohmann P, Albert NL, Tonn JC, Langen KJ. Current status of PET imaging in neuro-oncology. Neurooncol Adv. 2019; 1(1):vdz010.
•• Langen KJ, Galldiks N, Hattingen E, Shah NJ. Advances in neuro-oncology imaging. Nat Rev Neurol. 2017; 13(5):279–289. Overview of the use of amino acid PET and advanced MRI for brain tumor management.
Herholz K. Brain tumors: an update on clinical PET research in gliomas. Semin Nucl Med. 2017;47(1):5–17.
Unterrainer M, Galldiks N, Suchorska B, et al. (18)F-FET PET uptake characteristics in patients with newly diagnosed and untreated brain metastasis. J Nucl Med. 2017;58(4):584–9.
Galldiks N, Langen KJ, Albert NL, et al. PET imaging in patients with brain metastasis-report of the RANO/PET group. Neuro Oncol. 2019;21(5):585–95.
Galldiks N, Langen KJ, Pope WB. From the clinician’s point of view - what is the status quo of positron emission tomography in patients with brain tumors? Neuro Oncol. 2015;17(11):1434–44.
Langen KJ, Stoffels G, Filss C, et al. Imaging of amino acid transport in brain tumours: Positron emission tomography with O-(2-[(18)F]fluoroethyl)-L-tyrosine (FET). Methods. 2017;130:124–34.
Okubo S, Zhen HN, Kawai N, Nishiyama Y, Haba R, Tamiya T. Correlation of L-methyl-11C-methionine (MET) uptake with L-type amino acid transporter 1 in human gliomas. J Neurooncol. 2010;99(2):217–25.
Wiriyasermkul P, Nagamori S, Tominaga H, et al. Transport of 3-fluoro-L-alpha-methyl-tyrosine by tumor-upregulated L-type amino acid transporter 1: a cause of the tumor uptake in PET. J Nucl Med. 2012;53(8):1253–61.
Youland RS, Kitange GJ, Peterson TE, et al. The role of LAT1 in (18)F-DOPA uptake in malignant gliomas. J Neurooncol. 2013;111(1):11–8.
Papin-Michault C, Bonnetaud C, Dufour M, et al. Study of LAT1 expression in brain metastases: towards a better understanding of the results of positron emission tomography using amino acid tracers. PloS one. 2016;11(6):e0157139.
Shields AF, Grierson JR, Dohmen BM, et al. Imaging proliferation in vivo with [F-18]FLT and positron emission tomography. Nat Med. 1998;4(11):1334–6.
Wei W, Jiang D, Ehlerding EB, Luo Q, Cai W. Noninvasive PET imaging of T cells. Trends Cancer. 2018;4(5):359–73.
•• Galldiks N, Abdulla DS, Scheffler M, et al. Treatment monitoring of immunotherapy and targeted therapy using (18)F-FET PET in patients with melanoma and lung cancer brain metastases: initial experiences. J Nucl Med. 2020. Study in a higher number of patients that identified a survival benefit in metabolic FET PET responders.
Nguyen NC, Yee MK, Tuchayi AM, Kirkwood JM, Tawbi H, Mountz JM. Targeted therapy and immunotherapy response assessment with F-18 fluorothymidine positron-emission tomography/magnetic resonance imaging in melanoma brain metastasis: a pilot study. Front Oncol. 2018;8:18.
Kasten BB, Udayakumar N, Leavenworth JW, et al. Current and future imaging methods for evaluating response to immunotherapy in neuro-oncology. Theranostics. 2019;9(17):5085–104.
Niemeijer AN, Leung D, Huisman MC, et al. Whole body PD-1 and PD-L1 positron emission tomography in patients with non-small-cell lung cancer. Nat Commun. 2018;9(1):4664.
Terakawa Y, Tsuyuguchi N, Iwai Y, et al. Diagnostic accuracy of 11C-methionine PET for differentiation of recurrent brain tumors from radiation necrosis after radiotherapy. J Nucl Med. 2008;49(5):694–9.
Tsuyuguchi N, Sunada I, Iwai Y, et al. Methionine positron emission tomography of recurrent metastatic brain tumor and radiation necrosis after stereotactic radiosurgery: is a differential diagnosis possible? J Neurosurg. 2003;98(5):1056–64.
Minamimoto R, Saginoya T, Kondo C, et al. Differentiation of brain tumor recurrence from post-radiotherapy necrosis with 11C-methionine pet: visual assessment versus quantitative assessment. PloS one. 2015;10(7):e0132515.
Lizarraga KJ, Allen-Auerbach M, Czernin J, et al. (18)F-FDOPA PET for differentiating recurrent or progressive brain metastatic tumors from late or delayed radiation injury after radiation treatment. J Nucl Med. 2014;55(1):30–6.
Galldiks N, Stoffels G, Filss CP, et al. Role of O-(2-18F-fluoroethyl)-L-tyrosine PET for differentiation of local recurrent brain metastasis from radiation necrosis. J Nucl Med. 2012;53(9):1367–74.
• Ceccon G, Lohmann P, Stoffels G, et al. Dynamic O-(2-18F-fluoroethyl)-L-tyrosine positron emission tomography differentiates brain metastasis recurrence from radiation injury after radiotherapy. Neuro Oncol. 2017; 19(2):281–288. FET PET study that highlights the diagnostic value of dynamic PET acquisition.
Romagna A, Unterrainer M, Schmid-Tannwald C, et al. Suspected recurrence of brain metastases after focused high dose radiotherapy: can [18F]FET-PET overcome diagnostic uncertainties? Radiat Oncol. 2016;11(1):139.
• Kebir S, Rauschenbach L, Galldiks N, et al. Dynamic O-(2-[18F]fluoroethyl)-L-tyrosine PET imaging for the detection of checkpoint inhibitor-related pseudoprogression in melanoma brain metastases. Neuro Oncol. 2016; 18(10):1462–1464. Case series that addresses the potential of amino acid PET to detect checkpoint inhibitor-related pseudoprogression.
Lohmann P, Galldiks N, Kocher M, et al. Radiomics in neuro-oncology: basics, workflow, and applications. Methods. 2020.
Lohmann P, Kocher M, Ruge MI, et al. PET/MRI radiomics in patients with brain metastases. Front Neurol. 2020;11:1.
Peng L, Parekh V, Huang P, et al. Distinguishing true progression from radionecrosis after stereotactic radiation therapy for brain metastases with machine learning and radiomics. Int J Radiat Oncol Biol Phys. 2018;102(4):1236–43.
Zhang Z, Yang J, Ho A, et al. A predictive model for distinguishing radiation necrosis from tumour progression after gamma knife radiosurgery based on radiomic features from MR images. Eur Radiol. 2018;28(6):2255–63.
Lohmann P, Stoffels G, Ceccon G, et al. Radiation injury vs. recurrent brain metastasis: combining textural feature radiomics analysis and standard parameters may increase (18)F-FET PET accuracy without dynamic scans. Eur Radiol. 2017;27(7):2916–27.
Hotta M, Minamimoto R, Miwa K. 11C-methionine-PET for differentiating recurrent brain tumor from radiation necrosis: radiomics approach with random forest classifier. Sci Rep. 2019;9(1):15666.
• Lohmann P, Kocher M, Ceccon G, et al. Combined FET PET/MRI radiomics differentiates radiation injury from recurrent brain metastasis. Neuroimage Clin. 2018; 20:537–542. Study results address the additional diagnostic value of combined PET/MRI radiomics.
•• Law I, Albert NL, Arbizu J, et al. Joint EANM/EANO/RANO practice guidelines/SNMMI procedure standards for imaging of gliomas using PET with radiolabelled amino acids and [(18)F]FDG: version 1.0. Eur J Nucl Med Mol Imaging. 2019; 46(3):540–557. International effort to provide guidelines for PET imaging.
Boxerman JL, Quarles CC, Hu LS, et al. Consensus recommendations for a dynamic susceptibility contrast MRI protocol for use in high-grade gliomas. Neuro Oncol. 2020.
•• Kaufmann TJ, Smits M, Boxerman J, et al. Consensus recommendations for a standardized brain tumor imaging protocol for clinical trials in brain metastases. Neuro Oncol. 2020; 22(6):757–772. International effort to provide recommendations for a standardized MRI protocol.
Funding
Open Access funding enabled and organized by Projekt DEAL. Supported by the Deutsche Forschungsgemeinschaft (DFG), project number 428090865/SPP 2177 (N.G. and P.L.), and the Cologne Clinician Scientist Program (CCSP)/Faculty of Medicine/University of Cologne, funded by the DFG, FI 773/15-1 (J.-M.W.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Norbert Galldiks declares that he has no conflict of interest. Jan-Michael Werner declares that he has no conflict of interest. Philipp Lohmann declares that he has no conflict of interest. Martin Kocher declares that he has no conflict of interest. Gereon R. Fink declares that he has no conflict of interest. Karl-Josef Langen declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neuro-oncology
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Galldiks, N., Werner, JM., Lohmann, P. et al. Imaging of Response to Radiosurgery and Immunotherapy in Brain Metastases: Quo Vadis?. Curr Treat Options Neurol 23, 7 (2021). https://doi.org/10.1007/s11940-021-00664-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s11940-021-00664-6