Opinion statement
Cerebral edema is very common in patients with acute liver failure and encephalopathy. In severe cases, it produces brain tissue shift and potentially fatal herniation. Brain swelling in acute liver failure is produced by a combination of cytotoxic (cellular) and vasogenic edema. Accumulation of ammonia and glutamine leads to disturbances in the regulation of cerebral osmolytes, increased free radical production and calcium-mediated mitochondrial injury, and alterations in glucose metabolism (inducing high levels of brain lactate), resulting in astrocyte swelling. Activation of inflammatory cytokines can cause increased blood-brain barrier permeability leading to vasogenic edema, although the relative contribution of vasogenic edema is probably minor compared with cellular swelling. Cerebral blood flow is disturbed and generally increased in patients with acute liver failure; persistent vasodilatation and loss of autoregulation may generate hyperemia, and the consequent augmentation in cerebral blood volume may exacerbate brain edema.
Adequate management of intracranial hypertension demands continuous monitoring of intracranial pressure and cerebral perfusion pressure. Coagulation status should be assessed and bleeding diathesis should be treated prior to insertion of the intracranial pressure monitor. Standard treatment measures such as hyperventilation and osmotic agents (e.g., mannitol, hypertonic saline) remain useful first-line interventions. Although hypertonic saline may be preferred in patients with coexistent hyponatremia, the rate of correction of hyponatremia must be gradual to avoid the risk of osmotic demyelination. Barbiturate coma and intravenous indomethacin are available options in refractory cases. The most promising novel therapeutic alternative is the induction of moderate hypothermia (aiming for a core temperature of 32–34°C). However, the safety and efficacy of therapeutic hypothermia for brain swelling caused by liver failure still needs to be proven in randomized, controlled clinical trials. Management of intracranial pressure in patients with acute liver failure should be guided by well-defined treatment protocols.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Encephalopathy is very prevalent in patients with acute liver failure (ALF). When severe, it is typically associated with brain edema [1–4,5•,6]. Prominent brain edema is only very rarely encountered in cases of cirrhosis, though it may be seen in patients with “acute on chronic liver failure” [7]. In fulminant ALF, brain edema can be massive and can result in potentially fatal intracranial hypertension.
The pathophysiology of brain edema in ALF is complex and remains to be fully unraveled. It is predominantly cellular (cytotoxic) and is characterized by astrocyte swelling [8]. Hyperammonemia is considered the key element for the development of brain edema in ALF, and arterial ammonia concentrations greater than 200 μmol/L have been strongly associated with marked intracranial hypertension and cerebral herniation [9]. The most commonly held concept is that ammonia in combination with glutamate is converted into glutamine by the enzyme glutamine synthetase in the cytosol of the astrocyte. Glutamine (acting as a Trojan horse) is then transported into the mitochondria and deaminated back to ammonia and glutamate by glutaminase. Glutamine would act as an organic osmolyte causing osmotic loading of the mitochondria. Meanwhile, increased intracellular concentrations of ammonia and glutamine would also cause oxidative stress by promoting the generation of reactive oxygen species through mechanisms such as activation of the N-methyl-D aspartate (NMDA) glutamate receptor and upregulation of inducible nitric oxide synthase [1,4,5•,6]. Therefore, brain edema in ALF appears to result mainly from a state of energy failure related to severe mitochondrial dysfunction [10]. However, increases in brain lactate, altered expression of aquaporin-4, cerebral hyperemia, and activation of inflammatory cytokines could also play important roles by increasing cerebral blood volume and enhancing blood-brain barrier permeability (by means of greater pinocytosis) [1,4,5•,6,11]. Loss of autoregulation is frequent in cases of ALF complicated with brain edema; when present, hemodynamic augmentation can worsen the intracranial hypertension.
Patients at highest risk for brain edema are those with high-grade hepatic encephalopathy (grades III or IV), elevated serum ammonia levels (greater than 100 μmol/L), hyperacute progression of liver failure (evolution from jaundice to encephalopathy in fewer than 7 days), presence of systemic inflammatory response syndrome, and the need for vasopressors or renal replacement therapy [12,13]. Younger age may also increase the risk for this major complication [12]. Consequently, evaluation and monitoring for signs of brain edema should be intensively pursued in patients with these risk factors.
Diagnosis
Symptoms of raised intracranial pressure (ICP), such as headache, vomiting, confusion, and eventually decreased alertness, are neither sufficiently sensitive nor sufficiently specific for the timely recognition of brain edema. Physical signs are not much more useful. Patients are often hypertonic and hyperreflexic, but those findings can be seen in the absence of intracranial hypertension. Papilledema is useful when present, but its absence does not exclude the possibility of brain edema. Pupillary changes (typically dilatation) and the manifestations of the Cushing reflex (hypertension, bradycardia, and irregular breathing) only appear late. Consequently, traditional semiology does not provide enough information to guide management.
Brain imaging may reliably identify brain edema, but scans need to be interpreted carefully. CT scans can be valuable, not only to exclude hemorrhage in these patients, who are very often coagulopathic, but also to visualize signs of cerebral edema (Fig. 1). Sulcal and cisternal effacement, loss of distinction between gray and white matter, and poor delineation of the lenticular nuclei are subtle yet fairly reliable markers of edema, which are all too often missed or disregarded. Nonetheless, MRI is more sensitive. Diffusion-weighted imaging offers clear visualization of the localization and severity of edema (Fig. 2), and apparent diffusion coefficients allow discrimination between cellular and vasogenic components [14,15]. Additional MR techniques can have specific roles; for instance, diffusion tensor imaging may define more accurately the relative contribution of different types of edema [16,17], but this modality has been evaluated mostly in patients with cirrhosis.
CT scan of the head showing signs of global cerebral edema in a patient with advanced hypertensive encephalopathy from acute liver failure. Notice sulcal effacement, loss of differentiation between the gray and white matter and the boundaries of the lenticular nucleus, and partial effacement of basilar cisterns.
MRI of the brain showing evidence of brain edema from acute liver failure. a and b exhibit areas of restricted diffusion on diffusion-weighted imaging, indicating cellular (cytotoxic) edema; an apparent diffusion coefficient map (not shown) showed corresponding dark signal (low diffusion coefficient) in these lesions. c and d exemplify the changes observed on the Fluid Attenuation Inversion Recovery (FLAIR) sequence.
ICP monitoring remains essential for the diagnosis and management of intracranial hypertension. Although placement of the catheter carries the risk of causing hemorrhage, the risk of bleeding is acceptable if coagulopathy is corrected prior to the procedure. Rates of hemorrhage may reach 10%, but only half of cases lead to neurologic decline [18]. Patients may require pretreatment with vitamin K, fresh frozen plasma, platelets, and sometimes cryoprecipitate (if the fibrinogen level is <100 mg/dL). For more severely coagulopathic patients, the cost of administering recombinant factor VIIa may be justified [19]. Using doses lower than the usual 40 μg/kg when the INR is not too high may reduce the risk of thrombosis.
Subdural and epidural catheters (not readily available in the United States) have the lowest risk of hemorrhage, but their measurements are not consistently reliable. Ventriculostomy catheters are typically avoided because of the elevated risk of bleeding associated with their placement. Intraparenchymal probes (Camino catheters) offer the best balance between risk and benefit, and they are favored in most liver units. In fact, the recommendations of the US Acute Liver Failure Study Group for the intensive care of patients with ALF state that ICP monitoring should be considered in all patients listed for liver transplantation with stage III/IV hepatic encephalopathy and in patients with advanced hepatic encephalopathy who are not transplant candidates but have reasonable chances of recovery (eg, patients with acetaminophen-induced ALF) [20••, Class IV].
Multimodality brain monitoring can be achieved by adding the use of 1) jugular bulb catheters to measure venous oxygen saturation (SjvO2) and estimate the status of global cerebral oxygenation (SjvO2 >75% is often indicative of hyperemia and SjvO2 <50% may signal insufficient oxygen supply), 2) brain tissue oxygen probes (such as Licox catheters) to monitor regional/local oxygenation (brain tissue oxygen <20 mm Hg indicates hypoxia and values <10 mm Hg are associated with ischemia), 3) microdialysis to assess brain metabolic activity (a lactate/pyruvate ratio >25 denotes energy failure), and 4) electrophysiologic monitoring. However, jugular bulb catheters, brain tissue oxygen monitoring, and microdialysis have been studied mostly in patients with severe traumatic brain injury. Little is known about the pros and cons of their application to the management of ALF patients. Electroencephalographic monitoring has a more solid role because subclinical seizures may occur in comatose patients with brain edema from fulminant ALF [21]. Seizures may also complicate the early posttransplantation period and should be strongly considered in the differential diagnosis of patients who fail to regain full consciousness after the surgery [22].
Treatment
-
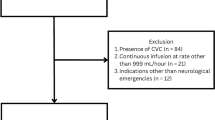
The basic principles for managing patients with advanced hepatic encephalopathy are outlined in Table 1. Using a standardized protocol for the management of intracranial hypertension is highly advisable [23•, Class III]. Table 2 briefly summarizes the details of the main therapeutic options for the treatment of intracranial hypertension in ALF.
Table 1 General principles for the management of patients with acute liver failure, advanced hepatic encephalopathy, and known or suspected brain edema Table 2 Main therapeutic options for the management of intracranial hypertension in acute liver failure -
Patients with advanced hepatic encephalopathy should be treated in a specialized intensive care unit. Short-acting, nondepolarizing neuromuscular blocking agents should be used to facilitate intubation. Stimulation should be limited when intracranial hypertension is known or suspected. For instance, pretreatment with intravenous lidocaine before endotracheal suctioning may minimize the risk of inducing ICP elevations. Adequate sedation can be achieved with propofol or benzodiazepines, and analgesia may require the infusion of a narcotic agent.
-
The patient’s head should be maintained in neutral position with the head of the bed at 30° to favor venous drainage and thus decrease ICP. (Raising the head of the bed to 30° also decreases the risk of ventilator-associated pneumonia.) However, some patients with markedly compromised cerebral perfusion may not tolerate elevation of the head of the bed, so it is important to assess ICP and cerebral perfusion pressure on an individual basis and serially over time in order to define the optimal position for each patient.
-
Patients should be kept well oxygenated. However, high levels of positive end-expiratory pressure (PEEP) can raise ICP in patients with critically reduced intracranial compliance. Ventilatory settings should be adjusted to maintain normocarbia (PCO2 35–40 mm Hg). Therapeutic hyperventilation must be reserved for patients with intracranial hypertension, and it should be used with caution because it induces cerebral vasoconstriction and may provoke ischemia. Thus, hyperventilation should be aimed at achieving a PCO2 between 28 and 34 mm Hg and its use should be stopped as soon as the intracranial hypertension can be controlled by other means.
-
Body temperature must be closely monitored. Fever demands aggressive treatment because it can exacerbate intracranial hypertension [24]. Cooling blankets and ice packs are typically effective in ALF patients because they have peripheral vasodilatation. Acetaminophen should be avoided because of the risk of worsening the liver injury, and nonsteroidal anti-inflammatory drugs are not recommended because of the risk of bleeding and associated renal and gastric toxicity. If shivering occurs, warming gloves, intravenous magnesium, increased sedation, or meperidine can be used.
-
Infections are common in patients with ALF, and their initial manifestations are often insidious. Consequently, daily surveillance cultures and chest x-rays are recommended in these patients, and broad-spectrum prophylactic antimicrobials (antibacterial, antifungal, and antiviral) should be strongly considered if the patient develops fever or other signs of systemic inflammatory response syndrome [20••, Class IV].
-
Hemodynamic management must be tailored to optimize cerebral perfusion pressure. Patients should be kept euvolemic, and hypotension should be avoided. Mean arterial pressures should be sufficient to maintain a cerebral perfusion pressure above 60 mm Hg. Some experts favor the use of SjvO2 to guide hemodynamic targets: higher systemic blood pressures would be necessary when SjvO2 is low, but they could be detrimental in patients with SjvO2 suggesting luxury perfusion [25]. This management paradigm is theoretically sensible, but its value has not been proven in ALF. When hemodynamic augmentation is needed, norepinephrine is usually the first choice [20••, Class IV]. In cases of circulatory collapse, the possibility of adrenal insufficiency should be entertained and a trial of hydrocortisone (300 mg/d) may be pertinent [26].
-
Blood testing should include measurements of serum sodium, glucose, renal function, ammonia levels, and coagulation values. Hyponatremia demands correction because it can worsen brain edema and lower the seizure threshold. However, it is important to remember that excessively rapid correction (>10 mmol/L over 24 h) may precipitate osmotic myelinolysis. Severe hyperglycemia and even mild degrees of hypoglycemia should be promptly treated. Renal failure may necessitate continuous or intermittent dialysis. The level of serum ammonia has prognostic value. Lactulose and rifaximin are always used in hyperammonemic patients with less advanced degrees of encephalopathy. In patients with fulminant liver failure who are candidates for liver transplantation, these medications are sometimes avoided to prevent colonic distension, which may complicate emergency transplantation surgery [1]. If they are administered, abdominal distension should be monitored very closely [20••]. N-acetyl-cysteine is indicated in cases of acetaminophen-induced ALF.
Pharmacologic options
-
Osmotic agents constitute the mainstay of the pharmacologic treatment of brain edema in ALF. They should be administered when the ICP is greater than 20 mm Hg (or cerebral perfusion pressure is <60 mm Hg) for more than 5–10 min. The options are mannitol 20% or various concentrations of hypertonic saline [27, Class IV]. These two alternatives have not been compared in patients with ALF.
-
In refractory cases, barbiturate coma can be induced to minimize cerebral metabolic activity. However, therapeutic hypothermia may be a preferred alternative to barbiturate coma. Indomethacin, a cerebral vasoconstrictor, can also be prescribed as a salvage therapy. Steroids do not have a role in the treatment of brain edema from ALF [20••,28; Class II].
Mannitol
Mannitol is an osmotic diuretic, which acts by creating a relative osmotic gradient leading to the movement of water from the brain tissue to the blood vessels, thereby reducing brain volume. This osmolar effect depends on the presence of an intact blood-brain barrier, which is at least structurally preserved in ALF. However, the nonosmotic effects of mannitol may be equally or more important. Mannitol boluses reduce blood viscosity and increase cerebral blood flow. The subsequent autoregulatory response of arteriolar vasoconstriction leads to a reduction in cerebral blood volume and ICP. Thus, mannitol may be much less effective in patients with altered or abolished vasomotor reactivity. Mannitol also has antioxidant (free radical scavenging) and antiapoptotic effects.
- Standard dosage:
-
Mannitol is typically administered as a 20% solution in intravenous boluses of 0.25–1 g/kg. Boluses can be repeated every 4–6 h depending on ICP. Serum osmolality should be measured prior to each dose, because osmolality greater than 320 mOsm/kg is associated with increased risk of renal tubular toxicity. Hence, the typical goal is to achieve and maintain a serum osmolality of 300–320 mOsm/kg. Mannitol may continue to be used safely even after higher serum osmolalities have been reached, as long as intravascular volume depletion is carefully avoided by providing adequate rehydration. Of note, serum concentrations of mannitol actually correlate better with the osmolar gap (measured osmolality minus calculated osmolality) [29], and targeting an osmolar gap of 50 might be a physiologically sounder alternative.
- Contraindications/precautions:
-
Hypersensitivity to mannitol, severe kidney disease (especially anuric or oliguric renal failure), and severe dehydration are contraindications. Mannitol should be used cautiously in patients with decompensated cardiac failure, who may not tolerate an osmotic load.
- Main drug interactions:
-
Diuretic-induced hyponatremia may enhance lithium toxicity, and hypokalemia/hypomagnesemia may enhance the toxicity of antiarrhythmics.
- Main adverse effects:
-
Mannitol is a potent diuretic and can induce intravascular volume depletion, low cardiac output, hypotension, and kidney injury from tubular necrosis. Mannitol has been associated with severe electrolyte disturbances such as hyperkalemia, hyponatremia, and hypernatremia. Bolus dosing of mannitol constitutes a large osmotic load and acutely may precipitate congestive heart failure in susceptible individuals. Other complications include hemolysis, seizures, and extravasation necrosis.
- Special points:
-
Intravascular volume depletion must be strictly avoided when mannitol is administered. Maintaining a neutral or positive fluid balance is crucial. Volume contraction may result in renal failure and cause secondary brain damage by compromising cerebral perfusion. The blood-brain barrier is not completely impermeable to mannitol (reflection coefficient of 0.9), so mannitol may accumulate in brain tissue over time even in patients with intact blood-brain barrier function. Brain tissue accumulation of mannitol increases the risk for “rebound” cerebral edema and rises in ICP if mannitol is discontinued suddenly. Although this concern is more applicable to diseases that compromise the blood-brain barrier, it is nonetheless advisable to taper the administration of mannitol gradually.
Hypertonic saline
The mechanisms of action of hypertonic saline are similar to those of mannitol. Hypertonic saline also has osmotic and nonosmotic properties. As an osmotic agent, it creates an osmotic gradient favoring the movement of water from the brain tissue to the circulation. The main nonosmotic actions are hemodynamic. Infusion of hypertonic saline leads to rapid intravascular volume expansion and increases cardiac output, which in turn enhances cerebral blood flow. The reactive cerebral arteriolar vasoconstriction is responsible for the reduction in cerebral blood volume and ICP. Other potential mechanisms include attenuation of inflammatory and neuroendocrine responses at the microcirculatory level.
- Standard dosage:
-
Several preparations and concentrations of hypertonic saline have been used to treat cerebral edema, from continuous infusions of 3% sodium chloride (available in premixed bags of 500 mL) to boluses of 30 mL of 23.4% sodium chloride (from concentrated vials originally intended for dilution). Continuous infusion of 3% sodium chloride at 1–2 mL/kg per hour can be titrated to achieve a serum sodium level of 150–160 mmol/L. In my experience, this continuous infusion is well tolerated but less effective in reducing ICP than intermittent boluses of higher saline concentration. Solutions of 7.5% or 10% sodium chloride can be prepared by the pharmacy and administered as boluses of 2 mL/kg of body weight over 20–30 min. Boluses of 30 mL of 23.4% sodium chloride are very effective in lowering ICP and can even reverse signs of brain herniation [30] they must be administered as slow push, and the safety of doses greater than 60 mL over 24 h has not been established. Hypertonic sodium chloride solution can induce hyperchloremic metabolic acidosis. Preparations combining sodium chloride with sodium acetate in a 50:50 mixture (or plain sodium acetate) should be used in these situations. All hypertonic saline solutions in concentrations of 3% or higher should be infused through central venous access to prevent phlebitis.
- Contraindications/precautions:
-
Congestive heart failure.
- Main drug interactions:
-
None.
- Main adverse effects:
-
Rapid infusion can induce transient hypotension, and increased intravascular volume may precipitate decompensation of congestive heart failure with pulmonary edema in predisposed patients. Acute hemolytic reactions can occur rarely, and a form of coagulopathy has been related to inhibition of platelets and coagulation proteins [31]. Extreme hypernatremia can exacerbate the encephalopathy and provoke seizures. In addition, very rapid elevations in serum sodium level can produce osmotic myelinolysis thus, hypertonic saline should be used very cautiously in patients with hyponatremia at baseline. Potassium supplementation is necessary to prevent hypokalemia with its attendant risk of arrhythmias. Magnesium supplementation is also often needed. Patients should be monitored for the development of hyperchloremic metabolic acidosis and be switched to sodium acetate solutions if it occurs.
- Special points:
-
Hypertonic saline is almost completely excluded by the intact blood-brain barrier (reflection coefficient close to 1). Thus, the risk of accumulation in the brain parenchyma and rebound exacerbation of brain edema after sudden discontinuation should be lower than with mannitol. Even so, it is prudent to taper the administration of hypertonic saline over time after any prolonged use. Hyponatremia is common in patients with ALF. Using high concentrations of hypertonic saline could be dangerous for hyponatremic patients serum sodium levels should be followed carefully and treatment should be titrated to avoid rises in serum sodium greater than 10–12 mmol/L over 24 h to prevent the risk of osmotic demyelination [32].
Pentobarbital
In patients with recalcitrant intracranial hypertension, barbiturate coma can be induced by pentobarbital (5–10 mg/kg intravenous bolus followed by a maintenance infusion of 1–3 mg/kg per hour). This therapy demands continuous electroencephalographic monitoring because the rate of barbiturate administration should be titrated to keep the patient on burst suppression. Adverse effects are very frequent and include hypotension, cardiac depression, infections (most commonly pneumonia) from immunosuppression, exacerbation of liver failure, and ileus. Rescue therapy with barbiturates has been replaced by therapeutic hypothermia in many liver units.
Indomethacin
Bolus doses of indomethacin (25 mg intravenously over 1 min) have been shown to be effective in selected ALF patients with intracranial hypertension refractory to osmotic agents [33]. Indomethacin acts by inducing cerebral vasoconstriction, so it may be most effective in patients with hyperemia. Because it can compromise cerebral blood flow, its use should be discouraged in patients with low perfusion pressure.
Emerging therapies
Therapeutic hypothermia
Experimental models have shown that moderate hypothermia produces various effects that attenuate brain edema, including decreasing cerebral blood flow, reducing uptake of ammonia by the brain, preventing rises in lactate concentration, lowering extracellular glutamate, diminishing the intracellular load of organic osmolytes, and modulating cytokine responses [34,35,36•]. Based on this solid theoretical rationale and favorable experimental data, preliminary studies of moderate therapeutic hypothermia have been conducted in small populations of patients with ALF complicated by brain edema. Promising initial results have shown that hypothermia may be an effective bridge therapy in patients with refractory intracranial hypertension who are good candidates for liver transplantation [34,36•,37–39; Class IV]. It may also be applied successfully in selected patients with severe brain edema from ALF who have good potential for liver recovery, such as cases of acetaminophen toxicity [40]. Although these favorable preliminary experiences need to be confirmed in a large-scale, randomized, controlled trial, induction of moderate hypothermia is currently implemented as a rescue treatment for brain edema in some of the largest liver units of various countries.
- Standard procedure:
-
Surface cooling is highly effective in patients with ALF because they typically have marked cutaneous vasodilatation, thus allowing for a very efficient heat exchange with external cooling measures. The target is a core temperature of 32°–33°C. Transplant candidates should be kept cooled until they are stable following transplantation. Other patients can be kept hypothermic for 3–5 days before rewarming is attempted. Rewarming should always proceed slowly to minimize the risk of complications, including rebound brain edema. Rewarming rates averaging 1°C every 12 h have been proposed to be most prudent [41].
- Complications:
-
The complications associated with the induction of moderate therapeutic hypothermia and with subsequent rewarming are summarized in Table 3. In our experience, the incidence of pneumonia is very high when hypothermia is maintained for more than 72 h. Rewarming appears to be particularly dangerous for patients with ALF who do not undergo transplantation, but patients with ALF induced by acetaminophen toxicity (in whom hepatic regeneration tends to be faster) may be exceptions.
Table 3 Complications of therapeutic hypothermia and rewarming - Special points:
-
Shivering should be treated to prevent increased metabolic brain demand options include skin warming (eg, warming mittens), infusion of magnesium sulfate, intermittent doses of meperidine (which should be used cautiously because it decreases the seizure threshold), propofol, dexmedetomidine, or neuromuscular paralysis.
Liver support systems
Artificial and bioartificial liver support systems have been developed recently [42]. Artificial liver support systems (such as albumin dialysis) can remove protein-bound and water-soluble toxins, thus decreasing serum ammonia concentrations, improving cerebral hemodynamics, and ameliorating the proinflammatory cytokine response. Bioartificial liver support systems use hepatocytes connected to the patient’s circulation through an extracorporeal device to provide synthetic function in addition to the clearance of toxins. When these forms of liver support are technically perfected in the future, they may become very effective in preventing and treating brain edema due to liver failure.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Blei AT: Brain edema in acute liver failure. Crit Care Clin 2008, 24:99–114, ix.
Detry O, De Roover A, Honore P, Meurisse M: Brain edema and intracranial hypertension in fulminant hepatic failure: pathophysiology and management. World J Gastroenterol 2006, 12:7405–7412.
Haussinger D, Schliess F: Pathogenetic mechanisms of hepatic encephalopathy. Gut 2008, 57:1156–1165.
Larsen FS, Wendon J: Brain edema in liver failure: basic physiologic principles and management. Liver Transpl 2002, 8:983–989.
Vaquero J, Butterworth RF: Mechanisms of brain edema in acute liver failure and impact of novel therapeutic interventions. Neurol Res 2007, 29:683–690. This article presents a clear and thoughtful review of traditional and new views on the pathophysiology of brain edema in ALF and the traditional and novel treatment alternatives for this complication.
Wendon J, Lee W: Encephalopathy and cerebral edema in the setting of acute liver failure: pathogenesis and management. Neurocrit Care 2008, 9:97–102.
Donovan JP, Schafer DF, Shaw BW Jr, Sorrell MF: Cerebral oedema and increased intracranial pressure in chronic liver disease. Lancet 1998, 351:719–721.
Norenberg MD, Rao KV, Jayakumar AR: Mechanisms of ammonia-induced astrocyte swelling. Metab Brain Dis 2005, 20:303–318.
Clemmesen JO, Larsen FS, Kondrup J, et al.: Cerebral herniation in patients with acute liver failure is correlated with arterial ammonia concentration. Hepatology 1999, 29:648–653.
Bjerring PN, Hauerberg J, Frederiksen HJ, et al.: Cerebral glutamine concentration and lactate-pyruvate ratio in patients with acute liver failure. Neurocrit Care 2008, 9:3–7.
Tofteng F, Jorgensen L, Hansen BA, et al.: Cerebral microdialysis in patients with fulminant hepatic failure. Hepatology 2002, 36:1333–1340.
Tofteng F, Hauerberg J, Hansen BA, et al.: Persistent arterial hyperammonemia increases the concentration of glutamine and alanine in the brain and correlates with intracranial pressure in patients with fulminant hepatic failure. J Cereb Blood Flow Metab 2006, 26:21–27.
Bernal W, Hall C, Karvellas CJ, et al.: Arterial ammonia and clinical risk factors for encephalopathy and intracranial hypertension in acute liver failure. Hepatology 2007, 46:1844–1852.
Fridman V, Galetta SL, Pruitt AA, Levine JM: MRI findings associated with acute liver failure. Neurology 2009, 72:2130–2131.
Arnold SM, Els T, Spreer J, Schumacher M: Acute hepatic encephalopathy with diffuse cortical lesions. Neuroradiology 2001, 43:551–554.
Rai V, Nath K, Saraswat VA, et al.: Measurement of cytotoxic and interstitial components of cerebral edema in acute hepatic failure by diffusion tensor imaging. J Magn Reson Imaging 2008, 28:334–341.
Nath K, Saraswat VA, Krishna YR, et al.: Quantification of cerebral edema on diffusion tensor imaging in acute-on-chronic liver failure. NMR Biomed 2008, 21:713–722.
Vaquero J, Fontana RJ, Larson AM, et al.: Complications and use of intracranial pressure monitoring in patients with acute liver failure and severe encephalopathy. Liver Transpl 2005, 11:1581–1589.
Shami VM, Caldwell SH, Hespenheide EE, et al.: Recombinant activated factor VII for coagulopathy in fulminant hepatic failure compared with conventional therapy. Liver Transpl 2003, 9:138–143.
Stravitz RT, Kramer AH, Davern T, et al.: Intensive care of patients with acute liver failure: recommendations of the US Acute Liver Failure Study Group. Crit Care Med 2007, 35:2498–2508. This consensus statement was authored by members of the US Acute Liver Failure Study Group, which includes some of the most experienced clinicians and researchers in the field of ALF. It presents an updated overview of the main aspects of intensive care of ALF and a comprehensive list of the most valuable references.
Ellis AJ, Wendon JA, Williams R: Subclinical seizure activity and prophylactic phenytoin infusion in acute liver failure: a controlled clinical trial. Hepatology 2000, 32:536–541.
Choi EJ, Kang JK, Lee SA, et al.: New-onset seizures after liver transplantation: clinical implications and prognosis in survivors. Eur Neurol 2004, 52:230–236.
Raschke RA, Curry SC, Rempe S, et al.: Results of a protocol for the management of patients with fulminant liver failure. Crit Care Med 2008, 36:2244–2248. This study analyzes the value of a structured protocol of intensive care applied to the management of 22 consecutive patients with intracranial hypertension from acute liver failure.
Munoz SJ, Moritz MJ, Bell R, et al.: Factors associated with severe intracranial hypertension in candidates for emergency liver transplantation. Transplantation 1993, 55:1071–1074.
Larsen FS, Wendon J: Prevention and management of brain edema in patients with acute liver failure. Liver Transpl 2008, 14(Suppl 2):S90–S96.
Harry R, Auzinger G, Wendon J: The effects of supraphysiological doses of corticosteroids in hypotensive liver failure. Liver Int 2003, 23:71–77.
Rabinstein AA: Treatment of cerebral edema. Neurologist 2006, 12:59–73.
Randomised trial of steroid therapy in acute liver failure. Report from the European Association for the Study of the Liver (EASL). Gut 1979, 20:620–623.
Garcia-Morales EJ, Cariappa R, Parvin CA, et al.: Osmole gap in neurologic-neurosurgical intensive care unit: its normal value, calculation, and relationship with mannitol serum concentrations. Crit Care Med 2004, 32:986–991.
Koenig MA, Bryan M, Lewin JL 3rd, et al.: Reversal of transtentorial herniation with hypertonic saline. Neurology 2008, 70:1023–1029.
Wilder DM, Reid TJ, Bakaltcheva IB: Hypertonic resuscitation and blood coagulation: in vitro comparison of several hypertonic solutions for their action on platelets and plasma coagulation. Thromb Res 2002, 107:255–261.
Rabinstein AA, Wijdicks EF: Hyponatremia in critically ill neurological patients. Neurologist 2003, 9:290–300.
Clemmesen JO, Hansen BA, Larsen FS: Indomethacin normalizes intracranial pressure in acute liver failure: a twenty-three-year-old woman treated with indomethacin. Hepatology 1997, 26:1423–1425.
Jalan R, Rose C: Hypothermia in acute liver failure. Metab Brain Dis 2004, 19:215–221.
Vaquero J, Rose C, Butterworth RF: Keeping cool in acute liver failure: rationale for the use of mild hypothermia. J Hepatol 2005, 43:1067–1077.
Stravitz RT, Larsen FS: Therapeutic hypothermia for acute liver failure. Crit Care Med 2009, 37:S258–S264. This is a very informative review of the use of therapeutic hypothermia for the treatment of brain edema in patients with ALF, including the mechanisms and experimental and clinical data.
Jalan R, Olde Damink SW, Deutz NE, et al.: Moderate hypothermia for uncontrolled intracranial hypertension in acute liver failure. Lancet 1999, 354:1164–1168.
Jalan R, Olde Damink SW, Deutz NE, et al.: Moderate hypothermia prevents cerebral hyperemia and increase in intracranial pressure in patients undergoing liver transplantation for acute liver failure. Transplantation 2003, 75:2034–2039.
Jalan R, Olde Damink SW, Deutz NE, et al.: Moderate hypothermia in patients with acute liver failure and uncontrolled intracranial hypertension. Gastroenterology 2004, 127:1338–1346.
Jacob S, Khan A, Jacobs ER, et al.: Prolonged hypothermia as a bridge to recovery for cerebral edema and intracranial hypertension associated with fulminant hepatic failure. Neurocrit Care 2009, 11:242–246.
Stravitz RT, Lee WM, Kramer AH, et al.: Therapeutic hypothermia for acute liver failure: toward a randomized, controlled trial in patients with advanced hepatic encephalopathy. Neurocrit Care 2008, 9:90–96.
Stadlbauer V, Wright GA, Jalan R: Role of artificial liver support in hepatic encephalopathy. Metab Brain Dis 2009, 24:15–26.
Disclosures
No potential conflict of interest relevant to this article was reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rabinstein, A.A. Treatment of Brain Edema in Acute Liver Failure. Curr Treat Options Neurol 12, 129–141 (2010). https://doi.org/10.1007/s11940-010-0062-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-010-0062-0