Abstract
Purpose of review
This paper assesses recent literature on the impact of chronic obstructive pulmonary disease (COPD) in patients with coronary artery disease (CAD) undergoing revascularization. Specifically, to determine if there is an optimal revascularization strategy for this patient population, and if there are other modalities to assess the risks.
Recent findings
There are limited new data in the last year addressing this clinical question. Recently there have been a series of studies which reinforced that COPD is a key independent risk factor for adverse outcomes after revascularization. There is no optimal revascularization strategy; however, there was a nonsignificant signal of potential benefit with percutaneous coronary intervention (PCI) with short-term outcomes in the SYNTAXES trial. Currently, pulmonary function tests (PFT) are limited in clarifying risk assessments prior to revascularization, and there are investigations into the use of biomarkers to provide further insight into this increased risk of adverse outcomes in patients with COPD.
Summary
COPD is a key risk factor for poor outcomes in patients requiring revascularization. More investigations are needed to determine the optimum revascularization strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) affects a significant portion of the US population, roughly 16 million with an increasing prevalence, and substantially impacts the medical healthcare system in terms of hospitalizations and healthcare costs [1, 2]. Recently, it is estimated that the total economic cost from COPD is 49.9 billion each year, with 29.5 billion being related to direct health care expenditures [2].
It is well established that COPD is an independent risk factor for cardiovascular disease, and ischemic heart disease, and one of the leading causes of death in this patient population. This relationship is not purely driven by smoking associations [1, 3]. One-third of patients with ischemic heart disease have chronic obstructive lung disease (COPD), and the prevalence of ischemic heart disease is two-fold higher in patients with COPD than observed in the general population [3]. In a population-based study which adjusted for smoking, Jousilahti et al. revealed that frequent COPD respiratory symptoms were associated with a 50% increase in coronary disease-related deaths [4]. This has been further validated in a series of studies, demonstrating an increased likelihood for cardiovascular-related mortality with patients who have daily cough or sputum production [4,5,6]. Additionally, patient survey data of self-reported COPD was significantly associated with the highest quartile of coronary artery calcium score [7]. While the mechanisms behind this association are still being investigated, there is clearly an epidemiologic association between COPD and coronary artery disease (CAD), suggesting an increased risk for cardiovascular events that may be linearly related to the severity of the underlying disease.
Treatment options: revascularization in COPD: percutaneous coronary intervention vs coronary artery bypasses surgery
Not only is COPD associated with cardiovascular disease, but it is a key risk factor when evaluating potential revascularization strategies. Even in the early days of coronary artery bypass graft (CABG) surgery, COPD was recognized as a key comorbidity that contributed to post-surgical complications [8]. Initially, severe COPD was considered to be a contraindication for CABG surgery; however, this contraindication was eventually revised [8]. Nevertheless, even with advancements in surgical and anesthetic management, recent meta-analyses have demonstrated that COPD is associated with higher rates of post-operative respiratory failure, stroke, renal failure, pneumonia and wound infections [9, 10]. Earlier studies showed that COPD patients may experience higher mortality rates in the immediate aftermath. Most importantly, patients with COPD have reduced long-term survival after CABG compared to patients without COPD [9, 10].
These adverse outcomes and the advent of new revascularization techniques promoted a shift in clinical management of patients with CAD that required intervention, notably with percutaneous coronary intervention being recommended over surgical revascularization [9, 11•]. However, early studies suggested that adverse outcomes remain high in COPD patients undergoing PCI despite avoiding the associated risks of CABG surgery [11•]. This discrepancy has been reported for some time, and in the last few years there have been further studies looking to elucidate optimal revascularization strategy along with the overall impact of COPD on long-term mortality [11•].
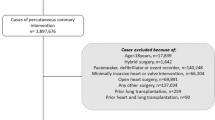
One of the more recent high-quality studies that has come out evaluating this was the SYNTAX Extended Survival (SYNTAXES) Trial, a randomized controlled trial which evaluated patients with triple vessel disease or left main coronary artery disease from March 2005 to April 2007 [11•]. The trial was an international multicenter trial, and eligible patients underwent 1:1 randomization to CABG or PCI. These patients were then followed for up to 10 years, with the goal to evaluate all-cause mortality at 10 years. Secondary outcomes of major adverse cardiovascular and cerebrovascular events, defined as a composite of all cause death, cerebrovascular accident, myocardial infarction or repeat revascularization at 30 days and 5 years were also explored [11•]. COPD was defined in accordance to guidelines established in EuroSCORE, a scoring system to predict early mortality in CABG patients. Importantly, they used definitions of long-term bronchodilator or steroid use for pulmonary disease, with no other symptomatic criteria or pulmonary function test evaluation to clarify the type of lung disease [11•, 12].
Of note, only 8.6% of the cohort (154 out of 1800) had COPD as previously defined. Furthermore, they had higher rates of current smoking, congestive heart failure along with peripheral arterial disease, and patients were less likely to be discharged on appropriate goal-directed medical therapy (GDMT) such as beta blockers or aspirin compared to patients without COPD [11•]. Similarly to prior studies, while patients with COPD had similar outcomes at 30 days, they had significantly higher all-cause mortality at 5 and 10 years compared to patients without COPD [11•].
However, the study provided conflicting results when it came to evaluating the optimal revascularization strategy. With 71 COPD patients randomized to PCI and 83 to CABG, initial results showed an elevated 10-year mortality regardless of revascularization strategy. While there were trends with major adverse cardiac and cerebrovascular events (MACCE) outcomes in COPD patients with PCI versus CABG at 5 years (35.9% vs 47.3%, 95% CI 0.44–1.2) and 10 years (42.3% vs 43.9%, 95% CI 0.59–1.56), neither of these were statistically significant [11•]. After adjustment with a multivariate analysis, COPD was an independent predictor of mortality in CABG patients, but not in patients undergoing PCI [11•].
There are some significant limitations with this trial, which makes it difficult to provide clinically relevant insights. Notably, the inclusion criteria for the SYNTAXES trial are not specific to COPD and may have included a wide range of patients. It is not clear if this trial included patients with other types of obstructive lung disease such as asthma or bronchiectasis, or restrictive lung diseases such as interstitial lung disease or pulmonary fibrosis to name a few. Many of these patients are on chronic bronchodilator or steroid therapy and it is not clear how many of these patients were included in the trial. A recent study by Zheng et al. published in 2022 highlights an effort to investigate the relationship between COPD and CAD revascularization, which includes pulmonary function test as a confirmation and definition of chronic obstructive pulmonary disease [13]. While only a small portion of the study had a PFT-confirmed cohort, this study demonstrated similar results with the SYNTAXES trial showing a statistically non-significant trend of increased major adverse cardiac events (MACE) in the PFT cohort at 450 days [13]. Moreover, there were statistically non-significant trends of increased MACE with increasing GOLD levels of disease severity. All of this emphasizes the importance of further studies with stricter inclusion criteria for confirmed COPD [13].
Finally, while the SYNTAXES trial may not have been adequately powered due to a low percentage of COPD patients, it reemphasized some previously established findings. Again, it showed that patients with COPD had increased long-term mortality regardless of revascularization strategy compared to patients without COPD [11•]. Additionally, the SYNTAXES trial redemonstrated that COPD was an independent risk factor in CABG patients, but not in patients who underwent PCI. Ultimately, while this trial did not demonstrate an ideal revascularization strategy with patients with COPD, it provided useful insights. Without a demonstrable difference in mortality outcomes with either strategy, patients with COPD should not be overlooked for possible surgical evaluation. Lastly, there were trends to suggest a possible benefit of PCI over CABG, but further investigations with adequately powered studies are needed to further explore this signal.
This is even more important currently as patients come through the COVID-19 pandemic, which has had devastating impacts across all aspects of our society. In a study by De Luca et al. published in 2022, they performed a retrospective registry review of 15,686 patients with STEMI treated by PCI from March 2019 to June 2020 [14]. In this study, there was no significant difference in in-hospital mortality or 30-day mortality in patients with COPD after controlling for baseline characteristics [14]. However, more studies need to investigate the impact of COVID-19 on outcomes, as the timeline of this study only captured the first few months of the pandemic.
While there are many future questions to be investigated and answered, what remains clear is the significant importance of COPD as comorbidity in patients with CAD undergoing plans for revascularization. A recent meta-analysis published in March 2023 by Li et al. analyzed 19 papers over the last decade, reconfirming that COPD remains a predictive factor when it comes to both short-term and long-term mortality [15]. More studies need to be done to clarify optimum revascularization strategies, and the role that increasing severity of COPD and medical management of both diseases play in the outcomes of revascularization.
Other treatments: perioperative risk assessment
There are several preoperative risk assessment tools used to approach patients with COPD that require surgery. The most used calculator, the ARISCAT Risk Index, which predicts the overall incidence of postoperative pulmonary complications of any severity and stratifies patients into low-, intermediate-, or high-risk [16]. Other calculators are used to establish the risk of only one single complication (i.e., Gupta calculator for post-operative respiratory failure or pneumonia) or are too complex for clinical use and used primarily in research settings (i.e., Arozullah respiratory failure index) [17,18,19]. These calculators are used to stratify risk before any proposed surgery, and occasionally identify patients most likely to benefit from risk-reduction interventions prior to surgery. However, unique risk stratification assessment specific to cardiac revascularization has yet to be developed.
Prior research has examined the role of preoperative pulmonary function testing and subsequent risk stratification for revascularization based on spirometric COPD severity. Najafi et al. found that patients had increased incidence of post-procedure respiratory failure commensurate with increased level of COPD severity based on the Society of Thoracic Surgeons (STS) definition [20]. Their cohort showed an increased number of CAD risk factors among patients with higher COPD severity, including hypertension and recent MI, which may account for this association. This association was again shown by Alam et al. in their 2020 study that concluded that abnormal PFTs were associated with poor prognosis; however, their study included all elective cardiac surgery patients and was not specific to revascularization [21].
Importantly, while preoperative risk stratification based on PFT abnormalities may accurately predict outcomes after revascularization, it is not clear that spirometry offers any additional insight as compared to the previously validated preoperative risk calculators based on patient data that is more readily attainable at the bedside and/or with laboratory values. The practicality of PFTs prior to all revascularization procedures would pose a significant impact on hospital workflow and resource utilization. Additionally, baseline PFTs and COPD severity as a static preoperative measurement are unlikely to be an immediately modifiable risk factor prior to an urgently needed procedure like cardiac surgery. Furthermore, utllization of pre-operative PFTs in patients with comorbid conditions that may alter the baseline pulmonary function (e.g., heart failure) could potentially result in undo restriction of lifesaving revascularization procedures in individuals who may indeed have the greatest benefit. There may instead be more efficient ways to further stratify preoperative risk using less cumbersome biometric and biomarker data that additionally may provide insights into modifiable risks amenable to intervention and risk reduction.
Emerging therapies
There have been several proposed mechanisms to explain the differential outcomes in patients with COPD who undergo revascularization. The current direction of investigative work is exploring the use of biometric data and serologic biomarkers in order to risk stratify this patient population, and to identify modifiable risk factors or opportunities for therapeutic interventions that improve outcomes.
In the CATEPOC study (impact of spirometrically confirmed chronic obstructive pulmonary disease on arterial stiffness and surfactant protein D after percutaneous coronary intervention), Mailk et al. explored the prognostic association of several physiologic and serologic variables in patients with COPD 1 month after discharge from PCI [22•]. The study found that overall arterial stiffness as determined by pulse wave velocity was increased in patients with COPD as compared to patients without COPD (7.35 m/s vs 6.60 m/s, p = 0.006). Prior studies have established that arterial stiffness was a significant predictor of cardiovascular events in the general public and an independent predictor of major cardiovascular events in patients with ischemic heart disease treated by PCI [23, 24]. Malik et al. also found a statistically significant increase in circulating high-sensitivity troponin T (Hs-TNT) and surfactant protein D (SPD) in patients with COPD as compared to patients without COPD. Hs-TNT is a marker for cardiomyocyte damage that has been shown to have an association with the risk of cardiovascular death in patients after a coronary event as well as to affect prognosis after an acute exacerbation of COPD. Similarly, the study found an increase in circulating SPD, a glycoprotein secreted by type-2 pneumocytes and expressed on endothelium of the cardiovascular system that has been associated with increased long-term cardiovascular mortality [25, 26]. The study is limited to a single center with predominantly male patients, however, establishing the correlation of increased values of arterial stiffness and serum biomarkers in those with COPD undergoing PCI is an area for additional prospective longitudinal investigation.
Another proposed mechanism for worse outcomes after PCI in patients with COPD is the compounded effect of inflammation and oxidative stress. This proposed mechanism allows for the consideration of therapeutic approaches that may affect outcomes. Aquila et al. have previously reported that in patients with stable CAD and concomitant COPD who underwent PCI, outcomes after treatment with ticagrelor for 1-month were superior in improving biological markers of endothelial function as compared to those treated with clopidogrel [27, 28]. In a follow-up study, Aquila et al. have explored the mechanism for this beneficial effect and found that treatment with ticagrelor led to increased levels of SIRT1 and HES1 mRNAs in peripheral blood, two genes that play a protective role in reducing systemic inflammation and oxidative stress [29•]. As compared to other mechanistic hypotheses without readily identifiable therapeutic implications, this association warrants additional prospective investigation.
The relationship of inflammation and long-term outcomes for COPD patients after PCI has been further explored by Zheng et al. by observing the relationship of high levels vs low levels of high sensitivity C-reactive protein (hsCRP) on admission and its association with major adverse cardiac events (MACE) [30•]. The study found a significant increase in MACE in the high-level hsCRP group as compared to the low-level hsCRP group (HR 2.47, 95% CI: 1.22–5.00; p = 0.012). This association could make hsCRP a useful biomarker for prognosis in patients with COPD and CAD who require PCI, though additional studies to accurately determine the most specific cut-off value are necessary.
Conclusions
The bidirectional relationship of COPD and CAD results in a specific subpopulation of patients with uniquely associated risks in undergoing revascularization procedures. COPD is an independent risk factor for worse outcomes following cardiac revascularization, regardless of the chosen revascularization strategy. There is some evidence to suggest that PCI may have better short-term outcomes as compared to CABG; however, more investigations are required to clarify the significance or impact of this signal for benefit. Additionally, the design of these trials must be more selective in defining the diagnostic parameters for COPD in order to further clarify the patient population to which the results can be applied. Pre-operative risk scores can assist to stratify the severity of COPD prior to revascularization; however, further investigations are needed to help with the development of novel pre-operative risk assessment measures and tools. One potential area that may shine light on the mechanisms leading to worse outcomes after revascularization in COPD patients is an investigation of associated biometric data and serologic biomarkers. These markers may assist with pre-operative risk stratification and, more importantly, may provide insights regarding potential interventions or therapies that would lead to risk reduction in post-procedural adverse events.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as:
• Of importance
Sin DD, Man SF. Chronic obstructive pulmonary disease as a risk factor for cardiovascular morbidity and mortality. Proc Am Thorac Soc. 2005;2(1):8–11. https://doi.org/10.1513/pats.200404-032MS. PMID: 16113462.
Morbidity and mortality: 2009 chart book on cardiovascular, lung and blood diseases. National Heart Lung and Blood Institute. 2009.
Hansell AL, Walk JA, Soriano JB. What do chronic obstructive pulmonary disease patients die from? Amultiple cause coding analysis. Eur Respir J. 2003;22(5):809–14.
Jousilahti P, Vartiainen E, Tuomilehto J, Puska P. Symptoms of chronic bronchitis and the risk of coronary disease. Lancet. 1996;348:567–72.
Rosengren A, Wilhelmsen L. Respiratory symptoms and long-term risk of death from cardiovascular disease, cancer and other causes in Swedish men. Int J Epidemiol. 1998;27:962–9.
Camilli AE, Robbins DR, Lebowitz MD. Death certificate reporting of confirmed airways obstructive disease. Am J Epidemiol. 1991;133:795–800.
Newman AB, Naydeck BL, Sutton-Tyrrell K, Feldman A, Edmundowicz D, Kuller LH. Coronary artery calcification in older adults to age 99: prevalence and risk factors. Circulation. 2001;104:2679–84.
O’Boyle F, Mediratta N, Chalmers J, Al-Rawi O, Mohan K, Shaw M, Poullis M. Long-term survival of patients with pulmonary disease undergoing coronary artery bypass surgery. Eur J Cardiothorac Surg. 2013;43(4):697–703. https://doi.org/10.1093/ejcts/ezs454. Epub 2012 Oct 24 PMID: 23096454.
Zhao H, Li L, Yang G, Gong J, Ye L, Zhi S, Zhang X, Li J. Postoperative outcomes of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass grafting surgery: a meta-analysis. Medicine (Baltimore). 2019;98(6):e14388. https://doi.org/10.1097/MD.0000000000014388. PMID: 30732179; PMCID: PMC6380818.
Leavitt BJ, et al. “ong-term survival of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass surgery. Circulation. 2006;114.1_supplement:I-430.
• Wang R, Tomaniak M, Takahashi K, Gao C, Kawashima H, Hara H, Ono M, van Klaveren D, van Geuns RJ, Morice MC, Davierwala PM, Mack MJ, Witkowski A, Curzen N, Berti S, Burzotta F, James S, Kappetein AP, Head SJ, Thuijs DJFM, Mohr FW, Holmes DR, Tao L, Onuma Y, Serruys PW. Impact of chronic obstructive pulmonary disease on 10-year mortality after percutaneous coronary intervention and bypass surgery for complex coronary artery disease: insights from the SYNTAX Extended Survival study. Clin Res Cardiol. 2021;110(7):1083–1095. https://doi.org/10.1007/s00392-021-01833-y. Epub 2021 Mar 12. PMID: 33710385; PMCID: PMC8238698. This paper reaffirmed the significance of COPD as a comorbidity for patients with CAD, and demonstrated that it significantly impacts cardiovascular outcomes. Importantly, this paper is a major investigation into determining the optimal revascularization strategy, with results showing COPD patients have poor outcomes with PCI or CABG.
Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16(1):9–13. https://doi.org/10.1016/s1010-7940(99)00134-7. PMID: 10456395.
Zheng Y, Qi Y, Seery S, Wang W, Zhao W, Shen T, Zhou L, Yang J, Li C, Wang X, Gao J, Meng X, Dong E, Tang YD. Long-term outcomes for Chinese COPD patients after PCI: a propensity score matched, double-cohort study. Front Cardiovasc Med. 20229;9:827635. https://doi.org/10.3389/fcvm.2022.827635. PMID: 35757341; PMCID: PMC9218100.
De Luca G, Nardin M, Algowhary M, Uguz B, Oliveira DC, Ganyukov V, Zimbakov Z, Cercek M, Okkels Jensen L, Loh PH, Calmac L, Roura Ferrer G, Quadros A, Milewski M, Scotto di Uccio F, von Birgelen C, Versaci F, Ten Berg J, Casella G, Wong Sung Lung A, Kala P, Díez Gil JL, Carrillo X, Dirksen M, Becerra-Munoz VM, Lee MK, Arifa Juzar D, de Moura Joaquim R, Paladino R, Milicic D, Davlouros P, Bakraceski N, Zilio F, Donazzan L, Kraaijeveld A, Galasso G, Lux A, Marinucci L, Guiducci V, Menichelli M, Scoccia A, Yamac AH, Ugur Mert K, Flores Rios X, Kovarnik T, Kidawa M, Moreu J, Flavien V, Fabris E, Martínez-Luengas IL, Boccalatte M, Bosa Ojeda F, Arellano-Serrano C, Caiazzo G, Cirrincione G, Kao HL, Sanchis Forés J, Vignali L, Pereira H, Manzo S, Ordoñez S, Özkan AA, Scheller B, Lehtola H, Teles R, Mantis C, Antti Y, Brum Silveira JA, Zoni R, Bessonov I, Savonitto S, Kochiadakis G, Alexopoulos D, Uribe CE, Kanakakis J, Faurie B, Gabrielli G, Gutierrez Barrios A, Bachini JP, Rocha A, Tam FC, Rodriguez A, Lukito AA, Saint-Joy V, Pessah G, Tuccillo A, Cortese G, Parodi G, Bouraghda MA, Kedhi E, Lamelas P, Suryapranata H, Verdoia M. Impact of chronic obstructive pulmonary disease on short-term outcome in patients with ST-elevation myocardial infarction during COVID-19 pandemic: insights from the international multicenter ISACS-STEMI registry. Respir Res. 2022;23(1):207. https://doi.org/10.1186/s12931-022-02128-0. PMID: 35971173; PMCID: PMC9376902.
Li Y, Zheng H, Yan W, Cao N, Yan T, Zhu H, Bao H. The impact of chronic obstructive pulmonary disease on the prognosis outcomes of patients with percutaneous coronary intervention or coronary artery bypass grafting: a meta-analysis. Heart Lung. 2023;60:8–14. https://doi.org/10.1016/j.hrtlng.2023.02.017. Epub ahead of print. PMID: 36868093.
Canet J, Gallart L, Gomar C, Paluzie G, Vallès J, Castillo J, Sabaté S, Mazo V, Briones Z, Sanchis J; ARISCAT Group. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010 Dec;113(6):1338–50. https://doi.org/10.1097/ALN.0b013e3181fc6e0a. PMID: 21045639.
Gupta H, Gupta PK, Fang X, Miller WJ, Cemaj S, Forse RA, Morrow LE. Development and validation of a risk calculator predicting postoperative respiratory failure. Chest. 2011;140(5):1207–15. https://doi.org/10.1378/chest.11-0466. Epub 2011 Jul 14 PMID: 21757571.
Gupta H, Gupta PK, Schuller D, Fang X, Miller WJ, Modrykamien A, Wichman TO, Morrow LE. Development and validation of a risk calculator for predicting postoperative pneumonia. Mayo Clin Proc. 2013;88(11):1241–9. https://doi.org/10.1016/j.mayocp.2013.06.027. PMID: 24182703.
Arozullah AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg. 2000;232(2):242–53. https://doi.org/10.1097/00000658-200008000-00015. PMID: 10903604; PMCID: PMC1421137.
Najafi M, Sheikhvatan M, Mortazavi SH. Do preoperative pulmonary function indices predict morbidity after coronary artery bypass surgery? Ann Card Anaesth. 2015;18(3):293–8. https://doi.org/10.4103/0971-9784.159796. PMID: 26139731; PMCID: PMC4881716.
Alam M, Shehzad MI, Hussain S, Paras I, Kanwal M, Mushtaq A. Spirometry assessment and correlation with postoperative pulmonary complications in cardiac surgery patients. Cureus. 2020;12(10):e11105. https://doi.org/10.7759/cureus.11105. PMID: 33240701; PMCID: PMC7682508.
• Malik K, Diaz-Coto S, de la Asunción Villaverde M, Martinez-Camblor P, Navarro-Rolon A, Pujalte F, De la Sierra A, Almagro P. Impact of spirometrically confirmed chronic obstructive pulmonary disease on arterial stiffness and surfactant protein D after percutaneous coronary intervention. The CATEPOC Study. Int J Chron Obstruct Pulmon Dis. 2022;17:2577–2587. https://doi.org/10.2147/COPD.S373853. PMID: 36267326; PMCID: PMC9578359. Explores the prognostic association of arterial stiffness, circulating levels of Hs-TNT and surfactant protein D in patients with COPD 1 month after discharge from PCI. These physiologic and serologic markers could have significant impact on risk stratification prior to revascularization, and is an important area for additional prospective longitudinal investigation.
Fang Y, Zhong Q. Investigation of the value of carotid-femoral pulse wave velocity and coronary artery lesions in prognosis of percutaneous coronary intervention patients. Am J Transl Res. 2021;13(6):6646.
Chen BW, Wang ZG, Liu Q, Wang X, Dang A. Combination of pulse wave velocity with clinical factors as a promising tool to predict major adverse cardiac events after percutaneous coronary intervention. J Cardiol. 2015;65(4):318–23.
Celli BR, Locantore N, Yates J, et al. Inflammatory biomarkers improve clinical prediction of mortality in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185(10):1065–72.
Hill J, Heslop C, Man SFP, et al. Circulating surfactant protein-D and the risk of cardiovascular morbidity and mortality. Eur Heart J. 2011;32(15):1918–25.
Vieceli Dalla Sega F, Fortini F, Aquila G, Pavasini R, Biscaglia S, Bernucci D, Del Franco A, Tonet E, Rizzo P, Ferrari R, et al. Ticagrelor improves endothelial function by decreasing circulating epidermal growth factor (EGF). Front Physiol. 2018;9:337.
Campo G, Dalla Sega FV, Pavasini R, Aquila G, Gallo F, Fortini F, Tonet E, Cimaglia P, Del Franco A, Pestelli G, et al. Biological effects of ticagrelor over clopidogrel in patients with stable coronary artery disease and chronic obstructive pulmonary disease. Thromb Haemost. 2017;117:1208–1216.
• Aquila G, Vieceli Dalla Sega F, Marracino L, Pavasini R, Cardelli LS, Piredda A, Scoccia A, Martino V, Fortini F, Bononi I, Martini F, Manfrini M, Pannuti A, Ferrari R, Rizzo P, Campo G. Ticagrelor increases SIRT1 and HES1 mRNA levels in peripheral blood cells from patients with stable coronary artery disease and chronic obstructive pulmonary disease. Int J Mol Sci. 2020;21(5):1576. https://doi.org/10.3390/ijms21051576. PMID: 32106619; PMCID: PMC7084534. Therapy with Ticagrelor in COPD patients with stable CAD has been shown to improve biological markers of endothelial function as compared to those treated with clopidogrel. This paper seeks to establish the mechanism of this benefit. The authors identified increased levels of circulating SIRT1 and HES1 mRNA in those treated with Ticagrelor, two genes that play a protective role in reducing systemic inflammation and oxidative stress. This could have important implications for medical management strategies.
• Zheng Y, Qi Y, Seery S, Yang J, Li C, Wang W, Gao J, Meng X, Shao C, Tang YD. Elevated HsCRP in chronic obstructive pulmonary disease: a prospective study of long-term outcomes after percutaneous coronary intervention Int J Chron Obstruct Pulmon Dis. 2022;7(17):2517 2528. https://doi.org/10.2147/COPD.S380194. PMID:36237420;PMCID:PMC9552669. This paper explores the relationship of inflammation and long-term outcomes for COPD patients after PCI, as determined by high vs low levels of high sensitivity CRP (hsCRP) and association with major adverse cardiac events (MACE). The study found a significant increase in MACEs in the high level hsCRP group as compared to the low level hsCRP group, and could make hsCRP a useful prognostic biomarker in patients with COPD and CAD who require PCI.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Matthew Brandorff declares that he has no conflict of interest. Julia Graham declares that she has no conflict of interest. Kirana Gudi declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
The article does not contain any study with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brandorff, M., Graham, J. & Gudi, K. Revascularization Strategies in Patients with Coronary Artery Disease and Chronic Obstructive Lung Disease. Curr Treat Options Cardio Med 25, 273–281 (2023). https://doi.org/10.1007/s11936-023-00993-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11936-023-00993-6