Abstract
Introduction
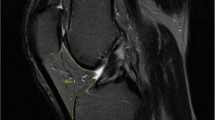
Knee osteoarthritis (OA) is a disease affecting all the neighboring articular tissues including the infrapatellar fat pad (IPFP). Although not yet as widely studied as other tissues in the knee, the IPFP has been recognized to have important metabolic activities and is a key player in OA.
Methods
In this commentary, we will briefly describe the different methodologies employed for the MRI morphological measurement of this tissue and depict the findings in regard to OA.
Results
The morphology of this tissue, monitored mainly with the use of magnetic resonance imaging (MRI), demonstrates changes during OA. However, studies of the IPFP morphological alterations and their association with the OA process have shown conflicting results, including a detrimental or beneficial role or no role at all. Although many reasons could explain such mixed findings, one might be the different methodologies used for the MRI measurement of area, volume, or signal intensity. In addition, several techniques are also employed for measuring the volume and signal intensity. An additional level of complexity is related to the presence within the IPFP of two different types of signal intensities, hyper-intensity, and hypo-intensity.
Conclusion
A consensus of a procedure to measure the morphology of the IPFP is urgently needed to fully appreciate the role of this tissue in the pathology of OA, as well as its uses for clinical decision-making.
Similar content being viewed by others
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
References
Zeng N, Yan ZP, Chen XY, Ni GX. Infrapatellar fat pad and knee osteoarthritis. Aging Dis. 2020;11:1317–28.
Ioan-Facsinay A, Kloppenburg M. An emerging player in knee osteoarthritis: the infrapatellar fat pad. Arthritis Res Ther. 2013;15:225.
Harkey MS, Davis JE, Lu B, et al. Early pre-radiographic structural pathology precedes the onset of accelerated knee osteoarthritis. BMC Musculoskelet Disord. 2019;20:241.
Zapata-Linares N, Eymard F, Berenbaum F, Houard X. Role of adipose tissues in osteoarthritis. Curr Opin Rheumatol. 2021;33:84–93.
Ushiyama T, Chano T, Inoue K, Matsusue Y. Cytokine production in the infrapatellar fat pad: another source of cytokines in knee synovial fluids. Ann Rheum Dis. 2003;62:108–12.
Conde J, Scotece M, Lopez V, et al. Differential expression of adipokines in infrapatellar fat pad (IPFP) and synovium of osteoarthritis patients and healthy individuals. Ann Rheum Dis. 2014;73:631–3.
Favero M, El-Hadi H, Belluzzi E, et al. Infrapatellar fat pad features in osteoarthritis: a histopathological and molecular study. Rheumatology (Oxford). 2017;56:1784–93.
Vera-Perez E, Sanchez-Bringas G, Ventura-Rios L, et al. Sonographic characterization of Hoffa’s fat pad. A pilot study. Rheumatol Int. 2017;37:757–64.
Gutierrez LB, Morgan TA, Link T, Feeley B, Motamedi D. Utility of musculoskeletal ultrasound in the diagnosis and treatment of suprapatellar fat pad impingement: a case report. J Clin Case Rep. 2016;6:837.
Kitagawa T, Nakase J, Takata Y, Shimozaki K, Asai K, Tsuchiya H. Use of ultrasonography to evaluate the dynamics of the infrapatellar fat pad after anterior cruciate ligament reconstruction: a feasibility study. J Med Ultrason. 2019;46:147–51.
Basha MAA, Eldib DB, Aly SA, et al. Diagnostic accuracy of ultrasonography in the assessment of anterior knee pain. Insights Imaging. 2020;11:107.
Dragoo JL, Johnson C, McConnell J. Evaluation and treatment of disorders of the infrapatellar fat pad. Sports Med. 2012;42:51–67.
Draghi F, Ferrozzi G, Urciuoli L, Bortolotto C, Bianchi S. Hoffa’s fat pad abnormalities, knee pain and magnetic resonance imaging in daily practice. Insights Imaging. 2016;7:373–83.
Roemer FW, Jarraya M, Felson DT, et al. Magnetic resonance imaging of Hoffa’s fat pad and relevance for osteoarthritis research: a narrative review. Osteoarthr Cartil. 2016;24:383–97.
Han W, Cai S, Liu Z, et al. Infrapatellar fat pad in the knee: is local fat good or bad for knee osteoarthritis? Arthritis Res Ther. 2014;16:R145.
Pan F, Han W, Wang X, et al. A longitudinal study of the association between infrapatellar fat pad maximal area and changes in knee symptoms and structure in older adults. Ann Rheum Dis. 2015;74:1818–24.
Cowan SM, Hart HF, Warden SJ, Crossley KM. Infrapatellar fat pad volume is greater in individuals with patellofemoral joint osteoarthritis and associated with pain. Rheumatol Int. 2015;35:1439–42.
Wallace KG, Pfeiffer SJ, Pietrosimone LS, et al. Changes in infrapatellar fat pad volume from 6 to 12 months following anterior cruciate ligament reconstruction and associations with patient-reported knee function. J Athl Train. 2021;56:1173–9.
Bonakdari H, Tardif G, Abram F, Pelletier JP, Martel-Pelletier J. Serum adipokines/related inflammatory factors and ratios as predictors of infrapatellar fat pad volume in osteoarthritis: applying comprehensive machine learning approaches. Sci Rep. 2020;10:9993.
Jacobson JA, Lenchik L, Ruhoy MK, Schweitzer ME, Resnick D. MR imaging of the infrapatellar fat pad of Hoffa. Radiographics. 1997;17:675–91.
Saddik D, McNally EG, Richardson M. MRI of Hoffa’s fat pad. Skelet Radiol. 2004;33:433–44.
Han W, Aitken D, Zhu Z, et al. Signal intensity alteration in the infrapatellar fat pad at baseline for the prediction of knee symptoms and structure in older adults: a cohort study. Ann Rheum Dis. 2016;75:1783–8.
Davis JE, Ward RJ, MacKay JW, et al. Effusion-synovitis and infrapatellar fat pad signal intensity alteration differentiate accelerated knee osteoarthritis. Rheumatology (Oxford). 2019;58:418–26.
Han W, Aitken D, Zhu Z, et al. Hypointense signals in the infrapatellar fat pad assessed by magnetic resonance imaging are associated with knee symptoms and structure in older adults: a cohort study. Arthritis Res Ther. 2016;18:234.
Hunter DJ, Guermazi A, Lo GH, et al. Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthr Cartil. 2011;19:990–1002.
Lu M, Chen Z, Han W, et al. A novel method for assessing signal intensity within infrapatellar fat pad on MR images in patients with knee osteoarthritis. Osteoarthr Cartil. 2016;24:1883–9.
Teichtahl AJ, Wulidasari E, Brady SR, et al. A large infrapatellar fat pad protects against knee pain and lateral tibial cartilage volume loss. Arthritis Res Ther. 2015;17:318.
Ragab E, Serag D. Infrapatellar fat pad area on knee MRI: does it correlate with the extent of knee osteoarthritis? Egypt J Radiol Nucl Med. 2021;52:1–9.
Masaki T, Takahashi K, Hashimoto S, et al. Volume change in infrapatellar fat pad is associated not with obesity but with cartilage degeneration. J Orthop Res. 2019;37:593–600.
Fontanella CG, Belluzzi E, Rossato M, et al. Quantitative MRI analysis of infrapatellar and suprapatellar fat pads in normal controls, moderate and end-stage osteoarthritis. Ann Anat. 2019;221:108–14.
Cai J, Xu J, Wang K, et al. Association between infrapatellar fat pad volume and knee structural changes in patients with knee osteoarthritis. J Rheumatol. 2015;42:1878–84.
Steidle-Kloc E, Culvenor AG, Dorrenberg J, Wirth W, Ruhdorfer A, Eckstein F. Relationship between knee pain and infrapatellar fat pad morphology: a within- and between-person analysis from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken). 2018;70:550–7.
Chuckpaiwong B, Charles HC, Kraus VB, Guilak F, Nunley JA. Age-associated increases in the size of the infrapatellar fat pad in knee osteoarthritis as measured by 3T MRI. J Orthop Res. 2010;28:1149–54.
Han W, Aitken D, Zheng S, et al. Association between quantitatively measured infrapatellar fat pad high signal-intensity alteration and magnetic resonance imaging-assessed progression of knee osteoarthritis. Arthritis Care Res (Hoboken). 2019;71:638–46.
Wang K, Ding C, Hannon MJ, Chen Z, Kwoh CK, Hunter DJ. Quantitative signal intensity alteration in infrapatellar fat pad predicts incident radiographic osteoarthritis: the Osteoarthritis Initiative. Arthritis Care Res (Hoboken). 2019;71:30–8.
Acknowledgements
The authors are grateful to Santa Fiori for preparing the manuscript.
Funding
This work was supported in part by the Osteoarthritis Research Unit of the University of Montreal Hospital Research Centre and the Chair in Osteoarthritis from the University of Montreal.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation and data collection were performed by Johanne Martel-Pelletier and Ginette Tardif. The first draft of the manuscript was written by Johanne Martel-Pelletier and all the authors commented on the previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
Johanne Martel-Pelletier and Jean-Pierre Pelletier are shareholders in ArthroLab Inc. Ginette Tardif declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Osteoarthritis
Rights and permissions
About this article
Cite this article
Martel-Pelletier, J., Tardif, G. & Pelletier, JP. An Open Debate on the Morphological Measurement Methodologies of the Infrapatellar Fat Pad to Determine Its Association with the Osteoarthritis Process. Curr Rheumatol Rep 24, 76–80 (2022). https://doi.org/10.1007/s11926-022-01057-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11926-022-01057-7