Abstract
Purpose of Review
Abnormal interoception has been consistently observed across eating disorders despite limited inclusion in diagnostic conceptualization. Using the alimentary tract as well as recent developments in interoceptive neuroscience and predictive processing as a guide, the current review summarizes evidence of gastrointestinal interoceptive dysfunction in eating disorders.
Recent Findings
Eating is a complex process that begins well before and ends well after food consumption. Abnormal prediction and prediction-error signals may occur at any stage, resulting in aberrant gastrointestinal interoception and dysregulated gut sensations in eating disorders. Several interoceptive technologies have recently become available that can be paired with computational modeling and clinical interventions to yield new insights into eating disorder pathophysiology.
Summary
Illuminating the neurobiology of gastrointestinal interoception in eating disorders requires a new generation of studies combining experimental probes of gut physiology with computational modeling. The application of such techniques within clinical trials frameworks may yield new tools and treatments with transdiagnostic relevance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
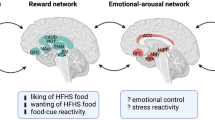
Eating disorders are psychiatric conditions characterized by aberrant eating and compensatory behavior patterns that are associated with severe medical complications, psychological comorbidities, and increased mortality [1]. Neurobiological models of eating disorders commonly emphasize the role of interactions among psychological traits and various cognitive functions (e.g., cognitive control, habit-learning), value processing (e.g., reward learning), and affective functioning (e.g., fear learning/generalization) [2,3,4,5,6]. Although interoceptive signaling is often linked with these processes, less attention is paid to the role of interoception.
The current review critically re-evaluates the role of interoception in eating disorders, with a focus on gastrointestinal interoception. It is organized around the potential points of altered interoception throughout the gastrointestinal tract and considers the associated implications for eating disorders.Footnote 1 While prior reviews have touched on the role of interoception in eating disorders [7,8,9], gastrointestinal symptoms [10, 11], or related processes such as hunger/thirst [12], here we emphasize the importance of understanding gastrointestinal interoception through the lens of predictive processing, whereby the nervous system is engaged in predicting upcoming states in relation to current states, and refining these predictions via error signaling. Finally, we highlight several methodological developments relevant to the study of gastrointestinal interoception and discuss their implications for advancing the clinical understanding and treatment of eating disorders.
Interoception Overview
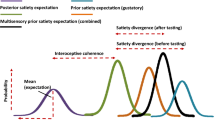
Interoception refers to the process by which the nervous system senses, interprets, and integrates signals originating from within the body, providing a moment-by-moment mapping of the body’s internal landscape across conscious and unconscious levels [13]. Interoception has traditionally been considered to be a one-way street in which “bottom-up” signals traveling from the body to the brain cause sensation and elicit “top-down” regulatory responses when bodily homeostasis is disrupted [14••]. More recently, interoception has been adopted into the conceptual framework of Bayesian inference (a method of statistical inference in which new observations are used to continuously update or infer the statistical probability that a hypothesis/outcome may be true), based on the premise that afferent sensory input to the brain is constantly shaped and modified by the individual’s expectations [15,16,17,18]. Thus, interoception can be reconceptualized as a bidirectional process between the brain and the body, with feedback and feedforward loops that constantly update an internal model aimed at predicting and regulating future states of the body [19••]. Despite these theoretical advances and evidence supporting the idea that the brain and the body cannot be fully understood when studied separately, most explanatory neuroscientific approaches attempting to understand cognitive, emotional, and behavioral functioning in eating disorders have not integrated these two dimensions.
Neurobiology of Interoception
The brain sits at the interface between the external world, which it samples through the exteroceptive senses, and the inner world of the body, which it accesses through interoceptive sensory channels. Interoceptive brain regions play primary roles in directly mapping the autonomic, chemosensory, endocrine, and immune systems, which relay information through peripheral nerves and direct neurochemical interfaces to the brainstem, hypothalamus, thalamus, and ultimately into cortical sectors including principally the insular and somatosensory cortices (for a detailed review see [14••]). The processing of information across these channels occurs in a hierarchical fashion, with multiple feedback loops starting in the autonomic nervous system and lower brainstem [20], providing a scaffold to delineate peripheral from central interoceptive dysfunction.
Perceptual Inference and Predictive Processing
While distinct from interoception, perceptual inference is an overlapping construct referring to the process by which a person generates beliefs or explanations about the causes and effects of events occurring in the world [21]. Perceptual inferences are strongly influenced by expectations. They may be explicit or implicit and can rapidly change depending on the environmental context. Eating disorders are conditions that can be characterized by erroneous perceptual inferences—about appetitive, cognitive, sensory, affective, and interoceptive phenomena. Because they reflect beliefs, it is natural that these inferences can form the basis of subsequent disorder-specific behaviors (e.g., restrictive eating, binge eating, or purging).
Computational neuroscience has provided mechanistic insights into the underpinnings of causal inference in the nervous system. In predictive processing models [22], neurons transmitting predictions about sensory states communicate with neurons detecting deviations from those predictions (so-called “prediction errors”) to develop an explanation for the perceptual information received via a “generative model” [23]. Over time, when the observed information deviates from what is predicted, the generative model is updated through learning, and thus perception emerges from processing the external or internal world within the context of a prior model. In addition, the metacognitive evaluation of perceptual content plays a role in generating awareness states [24], and it is conceivable that abnormalities in the neural circuitry underlying metacognition (i.e., the awareness and understanding of one’s own thought processes) underpin aspects of eating disorder symptomatology [25], particularly in relation to interoceptive signaling.
A Call to Reorient Interoceptive Investigations of Eating Disorders
Despite an early physiological focus on gut processing [26,27,28,29,30,31,32,33], progress in understanding the links between interoception and eating pathology has been limited by a predominant and selective reliance on self-report scales (see [34] and supplemental discussion in [13]). No experimental studies of interoception in eating disorders have utilized model-based analyses, which could formally test for altered predictive processing. Additionally, most existing studies focus narrowly on one feature (e.g., interoceptive accuracy) or one sensory channel (e.g., perception of heartbeats), ignoring the multifaceted interoceptive processes that may impact individuals with eating pathology. As mounting evidence suggests that individuals with eating disorders demonstrate maladaptive responses to food and eating-related sensations [35,36,37], new studies focused on gastrointestinal interoception are warranted. Such work would clarify associations of the neural circuitry central to the representation of gastrointestinal system with the affective and behavioral consequences of alterations within this system.
Current Evidence of Gastrointestinal Dysfunction in Eating Disorders
Individuals with anorexia nervosa (AN) show an extreme ability to voluntarily ignore hunger/thirst signals to restrict caloric intake. This prolonged, severe food restriction, in turn, impacts the state of the gastrointestinal tract [38]. In clinical settings, patients with AN commonly report gastrointestinal complaints such as exaggerated fullness in response to small meals (i.e., postprandial fullness), early satiety, and abdominal pain [39•]. They also report bowel and bladder symptoms outside of mealtimes, such as fullness, bloating, and constipation [40,41,42], and frequently exhibit gastrointestinal disorders [43] as well as functional gastrointestinal disorders [44]. The physiology underlying these abnormal perceptions has not been examined extensively in laboratory settings. Most available studies have used naturalistic designs following inpatients during the refeeding process. For example, within inpatient settings, individuals with AN report premature fullness after eating small amounts of food [45,46,47]. Fructose-sorbitol bolus ingestion disproportionately provokes gastrointestinal symptoms [48], further suggesting a heightened visceral sensitivity in acutely ill inpatients. After short-term refeeding to promote weight gain and restore homeostatic balance to the gut, persons with AN continue to report exaggerated fullness [47], although to a somewhat lower extent [46]. These symptoms decrease substantially in the 6 months following inpatient treatment [49], raising the possibility that they reflect an indicator of successful treatment response.
Individuals with binge-eating disorder (BED) and bulimia nervosa (BN) engage in recurrent cycles of food overconsumption, and those with BN also engage in compensatory behaviors (e.g., restriction, self-induced vomiting, laxative misuse, excessive exercise). These behaviors influence and may be perpetuated by alterations in the gastrointestinal tract. Gastrointestinal complaints including bloating, nausea, and constipation are also common in BN and improve with treatment [50]. Childhood onset of gastrointestinal complaints is associated with earlier onset of bulimic symptoms[51]; however, it remains unclear whether gastrointestinal alterations precede or follow the development of binge eating and purging behaviors for most individuals. More laboratory studies have focused on the physiological underpinnings of these symptoms and characteristic behaviors in BN and BED than in AN. Results indicate disturbances in the perception of satiety [52] and reduced sensitivity to gastric distension [53] in BN and in BED [54•], which are associated with altered gastric motor function [54•] and abnormal gut hormone release (e.g., cholecystokinin [55]).
Finally, it has been noted that those with avoidant/restrictive food intake disorder (ARFID) may demonstrate elevated sensitivity in response to gastrointestinal symptoms; however, the extent to which heightened gastrointestinal sensitivity is driven by heightened sensory input from peripheral cues, or by heightened central sensory processes is currently unknown [11]. More work in this area is needed.
Methodological Challenges and Solutions to Studying Gastrointestinal Interoception
Most attempts to examine the conscious perception of gastrointestinal sensations have used invasive approaches. These involve insertion of inflatable balloons into the esophagus [56,57,58], stomach [59], colon [60], or rectum [61,62,63,64], or direct gastric perfusion with chemical irritants [65]. While such mechanosensory approaches can be used to engage putative interoceptive cortical neural circuitry (i.e., insular and somatosensory cortices) [66,67,68], the invasiveness of these procedures is limiting, and they may provoke additional, confounding distress among eating disorder patients who have high levels of body image concerns.
Less invasive approaches exist but these, too, have certain constraints. For example, a water loading test involves ad-libitum ingestion of water until reaching a feeling of fullness [69]. This procedure can only be repeated once per testing session, hindering the ability to computationally model the perceptual processes underlying gastrointestinal sensation, and the protocol provides no information related to the processing of solid food. Other approaches have involved delivery of small amounts of tastants directly onto the tongue, such as sucrose solution [70], or milkshakes [71]. These approaches have contributed greatly to the understanding of the neurobiology of taste in eating disorders. However, they purposefully do not evoke the perceptual processes occurring in the gut after swallowing food, which represent most of the postprandial state.
Fortunately, recent developments provide a diversity of pharmacological and non-pharmacological approaches that are compatible with both experimental and observational methods for studying gastrointestinal interoception in eating disorders (Table 1). For example, we recently developed a minimally invasive probe for stimulating mechanosensory sensations in the stomach, via ingestion of a vibrating capsule [72]. Using a Bayesian computational modeling approach based on active inference, we could identify individual differences the evolution of prior beliefs during the task and their interactions with internal estimates of the reliability of gastrointestinal signals [73••]. Beyond the advantages of a minimally invasive method, notable benefits include the ability to administer repeated stimulations, thus facilitating sophisticated analyses. Several other commonly available approaches are relevant. Hydrogel capsules are a minimally invasive means capable of stimulating fullness sensations [74•]; the absence of caloric input associated with this approach allows for more naturalistic experiments separating the mechanosensory impact of gut distension from the caloric contents of a meal. Ingestible capsules for passive sensing of gut pressure, pH and temperature [75], and high-density electrogastrogram (EGG) arrays [76•] have been developed, which could facilitate laboratory as well as ambulatory (i.e., real-world) assessments of gut physiology in eating disorders across different stages of illness recovery. The discovery of a cortical “gastric network” in the brain using simultaneous analysis of resting EGG and brain fMRI recordings [77•] lays the groundwork for experimental studies testing the state-specific role of this network as a homeostatic regulator of food intake and of motivationally relevant hunger and satiety cues [78]. Glucagon-like peptide-1 (GLP1) receptor stimulation represents a noteworthy target for potential food craving modulation [79•] and is currently employed as an effective weight loss intervention in overweight or obese individuals [80]. A judicious and time-limited application of this approach as a research assessment tool in carefully screened eating disordered individuals may be warranted. For example, investigating the role of GLP1 agonism in modulating food craving and associated interoceptive neural circuitry in overweight individuals with BED would seem to be an appropriate approach, whereas similar studies in individuals with AN (or those engaging in prolonged fasting) might potentially increase harm by reinforcing food avoidance and propagating weight reduction. The motilin receptor agonist erythromycin has been shown to induce gastric contractions, hunger signals, and increased food intake [81], suggesting potential utility as an experimental probe of susceptibility to binge-eating behavior. The blockade of oral sucrose receptors [82] allows an opportunity to directly examine the influence of sucrose detecting cells in the stomach [83] in humans, particularly in relation to food cue processing in eating disorders. Finally, acute fasting represents a potent means of naturalistically modulating the strength of neurochemical hunger signaling with direct impacts on interoceptive neurocircuity [84••]. Collectively, these methods represent a diverse array of available tools for assessing the predictive value of individual differences in gastrointestinal interoception in eating disorders.
From Expectation to Ingestion to Digestion: a Predictive Processing Account of Gastrointestinal Interoception
Food consumption involves a series of anticipatory processing steps beginning with foraging during the cephalic phase followed by commencement of the ingestive process (Fig. 1). The cephalic phase includes processing via exteroceptive senses such as viewing and smelling. The motoric act of eating starts with tasting and chewing and is demarcated by swallowing, a key volitional checkpoint during which the ingested stimulus acquires the characteristics of an endogenous sensory signal [14••]. Subsequent steps with key relevance to interoception include esophageal transit, gastric filling and emptying, small intestine filling and emptying, and finally, colorectal filling and emptying. We suggest that abnormal interoception in eating disorders can manifest at each step via dysregulated bottom-up and top-down neural circuit interactions influenced by innate and developmental predisposing factors and various cognitive, valuative, and affective functions. In the following sections, we outline potential points throughout the alimentary tract for assessment and modulation of gastrointestinal interoception that may inform future research questions (Table 2) and, potentially, clinical applications targeting gastrointestinal interoceptive dysfunction in eating disorders.
Phases of food consumption from foraging to expulsion. Starting with the cephalic phase, each phase involves predictive processing and likely has a dedicated gastrointestinal interoceptive neurocircuitry. Studies of interoception in eating disorders have preferentially focused on the cephalic rather than the ingestive phase of the digestive process. See text for details
Procuring and Preparing
Exposure to food cues elicits cephalic phase responses (CPRs; i.e., physiological changes which prepare the body for digestion) [85]. Because foraging relies on the formulation of a hunger concept and an ensuing set of behaviors focused on obtaining food, from a predictive processing standpoint, we would argue that CPRs occur during the act of shopping, cooking, or simply ordering at a restaurant, and come with perceptible sensations. This stage thus requires the sensory predictive processing of hunger or desire and a future-oriented perspective that triggers a series of decision-making steps and ensuing actions. It is furthest from the receipt of the expected sensory signals that come from eating, and given the energy expenditures involved, requires the most in terms of motivation to maintain the necessary behaviors. The role of reward learning mechanisms has clear applications to this stage [86], and there is some evidence that individuals with eating disorders show goal-directed impairments in food and non-food related contexts [87, 88]. Yet, no studies have addressed the role of gastrointestinal interoception at this stage of food processing.
Viewing and Smelling
Foraging is terminated by the arrival of food, when processing of the associated visual and olfactory sensory signals ensues. This cephalic stage of processing has been extensively studied in eating disorders, and abundant evidence indicates aberrant activation in interoceptive neural circuits in response to food images [36]. For example, individuals with AN show atypical relationships between stomach sensations and neural responses to food images in limbic and ventral striatal brain regions, both of which comprise key components of neurally-mediated interoceptive pathways that connect with the insular cortex [89]. Studies consistently report altered insula activation in response to food images in AN and BN, but the direction of these alterations has been inconsistent. As such, abnormal interoceptive processing in response to visual food cues may play a role in both disorders, but precisely how this processing is altered and how it might contribute to disordered eating remains unclear.
Though less studied than visual cues, responses to smells may be particularly important for gastrointestinal predictive processing. For example, parotid salivary secretion (the main component of appetitive salivary anticipation) depends upon exposure to olfactory signals [90], and olfactomotor responses to odors vary according to perceptions of pleasantness [91]. Hedonic ratings of food smells are associatively learned and depend upon the food- and hunger-related context [92]. Evidence that individuals with eating disorders show a heightened sensitivity to smells [93, 94] raises the possibility that interoceptive processing abnormalities triggered by olfactory stimulation play a reinforcing role.
Tasting and Chewing
There is a longstanding debate regarding the extent to which taste is an interoceptive experience. Neurobiological arguments that taste is an interoceptive sense suggest that there are shared neural correlates of gustatory/taste experiences and interoceptive experiences, for example, within overlapping regions of the insula [95]. Taste signals are conveyed by similar channels as other interoceptive signals, and it has been suggested that defining gustatory neural representations could inform the understanding of interoceptive signals that are difficult to consciously access [96]. Conversely, studies of consummatory food reward suggest that gustatory signals may be more accurately conceptualized as exteroceptive [97, 98]. Debating the interoceptive versus exteroceptive categorization of taste perception is well outside the scope of the current review. However, recent studies have found that orosensory (e.g., taste) stimulation elicits overlapping and distinct neural activation patterns with interoceptive signals associated with gastric distension [99••]. As such, further investigation regarding the extent to which taste might represent a process that contributes to or maintains eating disorder psychopathology seems warranted.
In recent years, taste perception has garnered interest as a potential mechanism underlying food choice and eating behavior in individuals with eating disorders [100, 101]. Neuroimaging studies have shown anatomical alterations in women with eating disorders in brain regions centrally involved in taste and its valuation (e.g., medial orbitofrontal cortex, insula, striatum) [102]. Prior findings also suggest that women with acute restricting-type AN [103] and those recovered from AN or BN show aberrant anterior insula responses to sucralose [104, 105]. Women with restricting-type AN display a reduced ability to discriminate between sucrose, artificial saliva, or no solution, compared to healthy women and to women recovered from AN [106]. Additional findings suggest that individuals across the spectrum of eating disorders demonstrate abnormal ventral striatal-hypothalamic activation during a sucrose taste classical conditioning paradigm, with elevated prediction-error responses (violations of learned associations between conditioned visual and unconditioned taste stimuli) in AN [107] and reduced prediction-error responses in BN [108]. Altogether, although the taste-interoception debate has yet to be settled, taste-related deficits clearly play a role in eating disorder pathology.
Chewing is an understudied area of eating disorders, despite the fact that chewing and spitting behaviors are observed frequently in adolescent females [109]. Orosensory stimulation may be reinforcing in some individuals with eating disorders, as evidenced by the fact that social stress increases chewing rates in AN as compared to healthy individuals [110], and by modified sham feeding observations that women with BN sip more liquids [111] and women with AN sip less liquids [112] (independent of swallowing) than healthy individuals. More laboratory studies linking eating behaviors with gastrointestinal interoception are needed.
Swallowing and Esophageal Transit
Deglutition, the action or process of swallowing, is a voluntary behavior that involves the triggering of a coordinated set of reflexes between the pharynx and upper and lower esophageal sphincter, which work together to transport food from the mouth through the esophagus. Under typical circumstances, the ingestion of food or liquid via swallowing marks a decision to move nutrients into the body as a metabolic means of maintaining homeostasis and survival, leading to a reflexive opening of the gastroesophageal sphincter for approximately 8 s [113]. Swallowing difficulties have been linked to posterior insular cortex stimulation [114], suggesting it may be a key node in the cortical neurocircuitry of this visceromotor action. We have previously argued that swallowing is a decisional checkpoint that serves as a pragmatic demarcation of the transition from object to interoceptive signal within the gastrointestinal system [14••].
Physical complications or disorders that interfere with this process can perturb the system and lead to distress, anxiety, and eating avoidance. Oropharyngeal dysphagia refers to difficulty with swallowing or transporting a food or liquid bolus from the mouth into the esophagus. Although commonly observed across eating disorders [115,116,117] dysphagia has been infrequently studied in relation to eating pathology. In ARFID, emerging evidence suggests that food avoidance and restriction develops in the context of medical conditions characterized by dysphagia or related fears of aversive outcomes associated with swallowing [118]. In AN, some individuals develop symptoms of dysphagia; this can be accompanied by the sensation of food getting stuck in the esophagus. For example, one case series suggested that dysphagia may occur in severe AN and can be treated using neuromuscular electrical stimulation in conjunction with swallowing therapy [119]. However, to date, no studies have examined the neurophysiological underpinnings of deglutition in eating disorders, suggesting further research in this area is needed.
Swallow studies provide a validated means of clinically assessing characteristics of swallowing, including oral sensation, chewing, salivation, and oromuscular coordination of food bolus transit. These tests use a radiopaque artificial food bolus for a contrast-enhanced fluoroscopic evaluation of swallowing [120]. They have revealed some evidence of abnormal swallowing sensations in AN [121] and could be used more broadly to interrogate esophageal interoception in eating disorders. Most studies of individuals with purging have focused on the reversal of the sensation of fullness in the stomach. However, assessing relationships among esophageal interoception, dysphagia, and self-induced vomiting behaviors (i.e., systematic reversals of esophageal transit) may pinpoint new mechanistic targets for treatment. In addition, many patients with BN report symptoms of esophageal acid reflux, but these may occur in the absence of abnormal esophageal or gastric mucosa [122]. Research investigating potential conditioned associations among swallowing sensations, negative affect, and urges to purge would help to delineate the regulatory influence of chronic vomiting on esophageal interoception.
Gastric transit
The mechanosensory impact of gastric filling and emptying is a primary component of stomach sensation [123]. Altered postprandial gastric sensations are well-documented in eating disorders, and research to date suggests that these may arise from true (not just perceived) alterations in gastric function. In restrictive eating disorders, common reports of increased postprandial fullness and early satiety may relate to delayed gastric emptying and slowed orocecal transit [46, 124], and in BN and BED, delayed satiety may relate to reduced sensitivity to gastric distension [53, 54•]. To begin to elucidate how altered gastric predictive processing may maintain disordered eating, future studies could focus on integrating multilevel measures of gastric interoceptive accuracy (the correspondence between perceived gastric distension and objectively measured distension), beliefs about gastric interoceptive sensitivity, and subjective ratings of confidence in gastric interoceptive accuracy, with the correspondence or mismatch between confidence and accuracy [125]. Previous data suggest that large mismatches between objectively measured heartbeat perception accuracy and self rated sensitivity (conceptualized as “interoceptive trait prediction errors”) distinguish some individuals with autism spectrum conditions from healthy individuals, and that these “prediction errors” are inversely related to emotional sensitivity [126]. A similar mismatch between expectation and experience, but in the gastric domain, may maintain eating disorder symptoms. Thus, individuals with eating disorders may have abnormally and inaccurately strong expectations about situations that elicit gastric change (i.e., hyperprecise priors [127]), and they may have great difficulty adjusting these expectations in response to environmental changes. Characterizing abnormalities in gastric predictive processing could yield modifiable targets for novel eating disorder interventions.
Small Intestinal Transit
Primary functions of the small intestine include the breakdown of semi-solid food in the proximal (duodenal) segment followed by nutrient and water absorption from the distal (jejunal and ileal) segments. Although not commonly investigated, there are both mechanoreceptors and chemoreceptors present in this region of the gut [128], and fasting as well as eating both influence the rate of filling/relaxation [129]. Mechanostimulation of the jejunum via balloon distension and chemostimulation via capsaicin (the active component of chili peppers) both induce feelings of pressure/fullness or cramping/pain and are typically localized in the same central abdominal region [130]. Thus, from an interoceptive standpoint, there are likely overlapping sets of sensory signaling processes at this segment of the gut. To date, there have been few experimental studies of small intestinal interoception in eating disorders, though one study suggested delayed small bowel transit times in individuals with AN [131], and a case study reported evidence of jejunal blockage in an individual with AN [132]. It is presently unclear to what extent abnormal processing of small bowel sensations plays a role in symptom generation in eating disorders.
Colorectal Transit
The primary sensations associated with the distal end of the GI tract are linked to colorectal filling and emptying. In AN, high rates of defecatory disorders, constipation, and obstructive defecation syndrome suggest there may be slower than normal colonic transit timing [133]. These symptoms are supported by preliminary findings indicating delayed colonic transit times in individuals with AN who report chronic constipation [134]. Some individuals with AN also report abnormal sensation of rectal filling during anorectal manometry [134]. However, delayed colonic transit times normalize with refeeding [134], and data from a small group of patients with AN suggest that abnormalities in rectal sensation, internal anal sphincter relaxation threshold, rectal compliance, sphincter pressures, or expulsion patterns, normalize following weight restoration [135]. Additional work is needed to determine the extent to which sensorimotor rectal function is caused or maintained by interoceptive mechanisms (e.g., alterations in interoceptive network activation and increased or decreased perception of stimuli/sensations in the rectum) in eating disorders.
As previously noted, constipation is often reported by individuals with BN, and constipation and bowel hypofunction are common side-effects of laxative misuse [136]. These symptoms can, in turn, lead to increased sensations of bloating, promoting further eating-disorder behaviors. Medical complications often associated with chronic laxative or diuretic use (e.g., rectal prolapse) are also reported across eating disorders. The extent to which purgative eating disorder behaviors may be preceded by or contribute to aberrant colorectal interoception is unknown. Overall, there is presently great potential for the minimally invasive approaches (outlined in Table 1) to shed light on the causal neurobiological mechanisms related to gastric or colorectal transit of food signals and eating disorder symptoms.
Non-Gastrointestinal Interoception in Eating Disorders
While the current review is primarily focused on gastrointestinal interoception, it is important to note that alterations broadly spanning other interoceptive domains (e.g., cardiac, respiratory, pain, soft cutaneous touch, temperature) have been postulated to contribute to a wide range of AN and BN symptoms: from extreme restriction despite starvation, out-of-control overeating episodes, and purging behavior to those that are less directly related to the gastrointestinal system such as body image distortion, anxiety, and alexithymia [137,138,139,140]. For example, a recent network analysis indicated that body mistrust, and not feeling safe in one’s body, most linked self-reported interoceptive awareness to severe eating disorder psychopathology [141]. These findings suggest that that mistrust of one’s interoceptive afferents in general is associated with eating disorder symptoms.
In the last 5 years, research focused on cardiac and respiratory systems in eating disorders has shed light on the abnormal anticipation and processing of interoceptive afferents that may underpin this mistrust. Women with current or past eating disorders show an altered brain response when attending to cardiorespiratory signals [142], and before and during perturbations in these systems. For example, women with a history of BN show insular hyperactivation during the anticipation of aversive breathing restriction and abnormally declining activation during this aversive interoceptive experience, whereas women with a history of AN show hypoactivation during the anticipation of breathing restriction and abnormally steep increases in activation during breathing restriction [143, 144]. These results support a potential role for interoceptive predictive processing, and specifically prediction errors, in both disorders. In addition, affective reactions to aversive respiratory sensations are elevated in AN and in BN [145•], suggesting that interoceptive signals may be not only “untrustworthy” but also more distressing. Notably, non-gastrointestinal interoception and gastrointestinal-related interoception likely interact to maintain eating disorder symptoms. For example, in AN, the anticipation of eating is associated with heightened sensations of heart palpitations, dyspnea, and anxiety, all of which decrease after meal completion [146, 147]; these studies raise the possibility of multisensory integration deficits in eating disorders via interactions between gastrointestinal and cardiorespiratory afferent signaling.
Clinical Implications and New Horizons
Recent advances in the ability to modulate interoception provide new tools that may inform the development of individualized models and clinical interventions for eating disorders. For example, emerging evidence suggests that interoceptive exposure techniques targeting the gastrointestinal interoceptive cues (e.g., fullness, bloating) triggering anxiety and aversive states may attenuate symptom severity in adults and adolescents with eating disorders [148, 149, 150•]. Neuromodulation approaches such as vagus nerve stimulation (VNS) may have a physiological role in enhancing cardiovagal interoceptive processing [151], but auricular VNS does not modulate vagally-mediated heart rate variability [152], and the clinical applicability of non-invasive VNS for eating disorders is presently uncertain. Finally, reduced environmental stimulation therapy (aka floatation therapy) has received increasing study as a potential non-pharmacological anxiolytic. This approach is noteworthy in that it increases cardiorespiratory sensations while leaving gastrointestinal sensations unaffected [153]. After an early-phase trial showed this intervention to be safe, well tolerated, and associated with reduced anxiety and improved body-image symptoms in individuals with AN [154•], we are currently conducting a randomized efficacy trial. Despite initial hints of progress with respect to symptomatology, additional research is needed to clarify the extent to which these approaches effectively target interoceptive processes (especially predictive processing) that may contribute to or maintain pathological behaviors across the different phases of food consumption.
Conclusions
In the current review, we have described a predictive processing approach to interrogating interoception at relevant points throughout the alimentary system. We have emphasized key conceptual definitions, methodological advances, and clinical implications that remain unexplored. There are still many gaps in our knowledge, but several existing tools could be easily applied to assess the role of gastrointestinal interoception in eating disorders. By revealing the basic neural circuitry involved in predicting and sensing gut feelings and defining those that are disrupted by eating disorders, these methods pave the way for a new generation of enterically focused assessments and clinical interventions for eating disorders.
Notes
There are also emerging suggestions that the microbiome plays a role in eating disorders. However, the complexities of this “world within a world” combined with a limited knowledge of microbiome-host interactions at the level of interoceptive signaling renders this topic too early for us to review.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7):724–31. https://doi.org/10.1001/archgenpsychiatry.2011.74.
Fassino S, Amianto F, Gramaglia C, Facchini F, Abbate DG. Temperament and character in eating disorders: ten years of studies. Eating and Weight Disorders. 2004;9(2):81–90. https://doi.org/10.1007/BF03325050.
Steinglass JE, Berner LA, Attia E. Cognitive neuroscience of eating disorders. Psychiatr Clin North Am. 2019;42(1):75–91. https://doi.org/10.1016/j.psc.2018.10.008.
Friederich HC, Herzog W. Cognitive-behavioral flexibility in anorexia nervosa. Curr Top Behav Neurosci. 2011;6:111–23. https://doi.org/10.1007/7854_2010_83.
Zhang Z, Robinson L, Jia T, Quinlan EB, Tay N, Chu C, et al. Development of disordered eating behaviors and comorbid depressive symptoms in adolescence: neural and psychopathological predictors. Biol Psychiatry. 2020. https://doi.org/10.1016/j.biopsych.2020.06.003.
Kaye WH, Wierenga CE, Knatz S, Liang J, Boutelle K, Hill L, et al. Temperament-based treatment for anorexia nervosa. Eur Eat Disord Rev. 2015;23(1):12–8. https://doi.org/10.1002/erv.2330.
Khalsa SS, Lapidus RC. Can interoception improve the pragmatic search for biomarkers in psychiatry? Front Psych. 2016;7:121. https://doi.org/10.3389/fpsyt.2016.00121.
Klabunde M, Collado D, Bohon C. An interoceptive model of bulimia nervosa: a neurobiological systematic review. J Psychiatr Res. 2017;94(Supplement C):36–46. https://doi.org/10.1016/j.jpsychires.2017.06.009.
Jacquemot AMMC, Park R. The role of interoception in the pathogenesis and treatment of anorexia nervosa: a narrative review. Front Psych. 2020;11(281). https://doi.org/10.3389/fpsyt.2020.00281.
Zucker NL, Bulik CM. On bells, saliva, and abdominal pain or discomfort: early aversive visceral conditioning and vulnerability for anorexia nervosa. Int J Eat Disord. 2020;53(4):508–12. https://doi.org/10.1002/eat.23255.
Frank GKW, Golden NH, Murray HB. Introduction to a special issue on eating disorders and gastrointestinal symptoms-the chicken or the egg? Int J Eat Disord. 2021;54(6):911–2. https://doi.org/10.1002/eat.23558.
Stevenson RJ, Mahmut M, Rooney K. Individual differences in the interoceptive states of hunger, fullness and thirst. Appetite. 2015;95:44–57. https://doi.org/10.1016/j.appet.2015.06.008.
Khalsa SS, Adolphs R, Cameron OG, Critchley HD, Davenport PW, Feinstein JS, et al. Interoception and mental health: a roadmap. Biol Psychiatry: Cognitive Neuroscience and Neuroimaging. 2018;3(6):501–13. https://doi.org/10.1016/j.bpsc.2017.12.004.
•• Berntson GG, Khalsa SS. Neural circuits of interoception. Trends Neurosci. 2021;44(1):17-28. https://doi.org/10.1016/j.tins.2020.09.011. A state-of-the-art summary of the neurocircutiry of interoception.
Seth AK, Suzuki K, Critchley HD. An interoceptive predictive coding model of conscious presence. Front Psychol. 2011;2:395. https://doi.org/10.3389/fpsyg.2011.00395.
Pezzulo G, Rigoli F, Friston K. Active inference, homeostatic regulation and adaptive behavioural control. Prog Neurobiol. 2015;134:17–35. https://doi.org/10.1016/j.pneurobio.2015.09.001.
Stephan KE, Manjaly ZM, Mathys CD, Weber LA, Paliwal S, Gard T, et al. Allostatic self-efficacy: a metacognitive theory of dyshomeostasis-induced fatigue and depression. Front Hum Neurosci. 2016;10:550. https://doi.org/10.3389/fnhum.2016.00550.
Barrett LF, Simmons WK. Interoceptive predictions in the brain. Nat Rev Neurosci. 2015;16(7):419–29. https://doi.org/10.1038/nrn3950.
•• Petzschner FH, Garfinkel SN, Paulus MP, Koch C, Khalsa SS. Computational models of interoception and body regulation. Trends Neurosci. 2021;44(1):63-76. https://doi.org/10.1016/j.tins.2020.09.012. A state-of-the-art summary of computational modeling approaches to interoception.
Smith R, Thayer JF, Khalsa SS, Lane RD. The hierarchical basis of neurovisceral integration. Neurosci Biobehav Rev. 2017;75:274–96. https://doi.org/10.1016/j.neubiorev.2017.02.003.
Teufel C, Fletcher PC. Forms of prediction in the nervous system. Nat Rev Neurosci. 2020;21(4):231–42. https://doi.org/10.1038/s41583-020-0275-5.
Keller GB, Mrsic-Flogel TD. Predictive processing: a canonical cortical computation. Neuron. 2018;100(2):424–35. https://doi.org/10.1016/j.neuron.2018.10.003.
Walsh KS, McGovern DP, Clark A, O’Connell RG. Evaluating the neurophysiological evidence for predictive processing as a model of perception. Ann N Y Acad Sci. 2020;1464(1):242–68. https://doi.org/10.1111/nyas.14321.
Fleming SM. Awareness as inference in a higher-order state space. Neuroscience of Consciousness. 2020;2020(1):niz020. https://doi.org/10.1093/nc/niz020.
Georgantopoulos G, Konstantakopoulos G, Michopoulos I, Dikeos D, Gonidakis F. The relationship between metacognitive beliefs and symptoms in eating disorders. Psychiatriki. 2020;31(3):225–35. https://doi.org/10.22365/jpsych.2020.313.225.
Creighton C. Unconscious memory in visceral neuroses. Illustrations of unconscious memory in disease including a theory of alteratives. H. K. Lewis, London; 1886. p. 101–16.
Pearcy JF, Allen TD. Reflexes from the gastro-intestinal tract to the eye. Am J Physiol. 1927;82:56–8.
Wolf S. The relation of gastric function to nausea in man. J Clin Investig. 1943;22:877–82. https://doi.org/10.1172/JCI101462.
Wolf S, Wolff HG. Pain arising from the stomach and mechanisms underlying gastric symptoms. Research Publications of the Association for Research in Nervous & Mental Disease. 1943;23:289–301.
Hall WG. Visceral hypersensitivity and impaired accommodation in refractory diabetic gastroparesis. Appetite. 1985;6(4):333–56.
James WT, Gilbert TF. Elimination of eating behavior by food injection in weaned puppies. Psychol Rep. 1957;3:167–8. https://doi.org/10.2466/PR0.3.3.167-168.
Moyer KE, Bunnell BN. Effect of stomach distention caused by water on food and water consumption in the rat. J Comp Physiol Psychol. 1962;55(4):652–5. https://doi.org/10.1037/h0041423.
Coddington RD, Bruch H. Gastric perceptivity in normal, obese and schizophrenic subjects. Psychosomatics. 1970;11(6):571–9.
Jenkinson PM, Taylor L, Laws KR. Self-reported interoceptive deficits in eating disorders: a meta-analysis of studies using the eating disorder inventory. J Psychosom Res. 2018;110:38–45. https://doi.org/10.1016/j.jpsychores.2018.04.005.
Racine SE, Hebert KR, Benning SD. Emotional reactivity and appraisal of food in relation to eating disorder cognitions and behaviours: evidence to support the motivational conflict hypothesis. Eur Eat Dis Rev. 2018;26(1):3–10. https://doi.org/10.1002/erv.2567.
Lloyd EC, Steinglass JE. What can food-image tasks teach us about anorexia nervosa? A systematic review J Eat Disord. 2018;6:31. https://doi.org/10.1186/s40337-018-0217-z.
Kessler U, Rekkedal GA, Ro O, Berentsen B, Steinsvik EK, Lied GA, et al. Association between gastrointestinal complaints and psychopathology in patients with anorexia nervosa. Int J Eat Disord. 2020;53(5):532–6. https://doi.org/10.1002/eat.23243.
Westmoreland P, Krantz MJ, Mehler PS. Medical complications of anorexia nervosa and bulimia. Am J Med. 2016;129(1):30–7. https://doi.org/10.1016/j.amjmed.2015.06.031.
• Schalla MA, Stengel A. Gastrointestinal alterations in anorexia nervosa - a systematic review. Eur Eat Dis Rev. 2019;27(5):447-61. https://doi.org/10.1002/erv.2679. A systematic review of gastrointestinal alterations in AN, summarizing evidence that AN is often the cause (versus the result of) gastrointestinal dysfunction.
Sato Y, Fukudo S. Gastrointestinal symptoms and disorders in patients with eating disorders. Clin J Gastroenterol. 2015;8(5):255–63. https://doi.org/10.1007/s12328-015-0611-x.
Halmi KA, Sunday SR. Temporal patterns of hunger and fullness ratings and related cognitions in anorexia and bulimia. Appetite. 1991;16(3):219–37.
Robinson PH. Perceptivity and paraceptivity during measurement of gastric emptying in anorexia and bulimia nervosa. Br J Psychiatry. 1989;154:400–5.
Lin JA, Woods ER, Bern EM. Common and emergent oral and gastrointestinal manifestations of eating disorders. Gastroenterol Hepatol (N Y). 2021;17(4):157–67.
Wiklund CA, Rania M, Kuja-Halkola R, Thornton LM, Bulik CM. Evaluating disorders of gut-brain interaction in eating disorders. Int J Eat Disord. 2021;54(6):925–35. https://doi.org/10.1002/eat.23527.
Heruc GA, Little TJ, Kohn M, Madden S, Clarke S, Horowitz M, et al. Appetite perceptions, gastrointestinal symptoms, Ghrelin, Peptide YY and State Anxiety Are Disturbed in Adolescent Females with Anorexia Nervosa and Only Partially Restored with Short-Term Refeeding. Nutrients. 2018;11(1). https://doi.org/10.3390/nu11010059.
Bluemel S, Menne D, Milos G, Goetze O, Fried M, Schwizer W, et al. Relationship of body weight with gastrointestinal motor and sensory function: studies in anorexia nervosa and obesity. BMC Gastroenterol. 2017;17(1):4. https://doi.org/10.1186/s12876-016-0560-y.
Peterson CM, Tissot AM, Matthews A, Hillman JB, Peugh JL, Rawers E, et al. Impact of short-term refeeding on appetite and meal experiences in new onset adolescent eating disorders. Appetite. 2016;105:298–305. https://doi.org/10.1016/j.appet.2016.05.037.
Friesen N, Hansen RD, Abraham SF, Kellow JE. Fructose-sorbitol ingestion provokes gastrointestinal symptoms in patients with eating disorders. World J Gastroenterol. 2009;15(42):5295–9.
Salvioli B, Pellicciari A, Iero L, Di Pietro E, Moscano F, Gualandi S, et al. Audit of digestive complaints and psychopathological traits in patients with eating disorders: a prospective study. Dig Liver Dis. 2013;45(8):639–44. https://doi.org/10.1016/j.dld.2013.02.022.
Chami TN, Andersen AE, Crowell MD, Schuster MM, Whitehead WE. Gastrointestinal symptoms in bulimia nervosa: effects of treatment. Am J Gastroenterol. 1995;90(1):88–92.
Gendall KA, Joyce PR, Carter FA, McIntosh VV, Bulik CM. Childhood gastrointestinal complaints in women with bulimia nervosa. Int J Eat Disord. 2005;37(3):256–60. https://doi.org/10.1002/eat.20088.
Kissileff HR, Wentzlaff TH, Guss JL, Walsh BT, Devlin MJ, Thornton JC. A direct measure of satiety disturbance in patients with bulimia nervosa. Physiol Behav. 1996;60(4):1077–85. https://doi.org/10.1016/0031-9384(96)00086-8.
Zimmerli EJ, Walsh BT, Guss JL, Devlin MJ, Kissileff HR. Gastric compliance in bulimia nervosa. Physiol Behav. 2006;87(2):441–6. https://doi.org/10.1016/j.physbeh.2005.11.010.
• van Dyck Z, Schulz A, Blechert J, Herbert BM, Lutz APC, Vogele C. Gastric interoception and gastric myoelectrical activity in bulimia nervosa and binge-eating disorder. Int J Eat Disord. 2021;54(7):1106-15. https://doi.org/10.1002/eat.23291. First study to evaluate binge-eating behaviors and gastric motor function in combination with other components of gastric interoception in individuals with eating disorders. The study observed evidence of delayed response to satiation in treatment-seeking adults with eating disorders, compared to healthy comparisons, suggesting that afferent interoceptive signals are altered in eating disorders.
Devlin MJ, Walsh BT, Guss JL, Kissileff HR, Liddle RA, Petkova E. Postprandial cholecystokinin release and gastric emptying in patients with bulimia nervosa. Am J Clin Nutr. 1997;65(1):114–20.
Aziz Q, Andersson JL, Valind S, Sundin A, Hamdy S, Jones AK, et al. Identification of human brain loci processing esophageal sensation using positron emission tomography. Gastroenterology. 1997;113(1):50–9.
Hobson AR, Sarkar S, Furlong PL, Thompson DG, Aziz Q. A cortical evoked potential study of afferents mediating human esophageal sensation. Am J Physiol Gastrointest Liver Physiol. 2000;279(1):G139–47.
Remes-Troche JM, Attaluri A, Chahal P, Rao SS. Barostat or dynamic balloon distention test: which technique is best suited for esophageal sensory testing? Dis Esophagus. 2012;25(7):584–9. https://doi.org/10.1111/j.442-2050.11.01294.x (Epub 13 Dec 2011).
Geeraerts B, Van Oudenhove L, Dupont P, Vanderghinste D, Bormans G, Van Laere K, et al. Different regional brain activity during physiological gastric distension compared to balloon distension: a H2 15O-PET study. Neurogastroenterol Motil. 2011;23(6):533-e203. https://doi.org/10.1111/j.365-2982.010.01642.x (Epub 14 Dec 2010).
Holzl R, Erasmus LP, Moltner A. Detection, discrimination and sensation of visceral stimuli. Biol Psychol. 1996;42(1–2):199–214.
Hobday DI, Hobson A, Furlong PL, Thompson DG, Aziz Q. Comparison of cortical potentials evoked by mechanical and electrical stimulation of the rectum. Neurogastroenterol Motil. 2000;12(6):547–54.
Sun WM, Read NW, Prior A, Daly JA, Cheah SK, Grundy D. Sensory and motor responses to rectal distention vary according to rate and pattern of balloon inflation. Gastroenterology. 1990;99(4):1008–15.
Toma TP, Zighelboim J, Phillips SF, Talley NJ. Methods for studying intestinal sensitivity and compliance: in vitro studies of balloons and a barostat. Neurogastroenterol Motil. 1996;8(1):19–28. https://doi.org/10.1111/j.1365-2982.1996.tb00238.x.
Haas S, Brock C, Krogh K, Gram M, Nissen TD, Lundby L, et al. Cortical evoked potentials in response to rapid balloon distension of the rectum and anal canal. Neurogastroenterol Motil. 2014;26(6):862–73. https://doi.org/10.1111/nmo.12341 (Epub 20 Apr 2014).
Yang M, Li ZS, Xu XR, Fang DC, Zou DW, Xu GM, et al. Characterization of cortical potentials evoked by oesophageal balloon distention and acid perfusion in patients with functional heartburn. Neurogastroenterol Motil. 2006;18(4):292–9.
Aziz Q, Schnitzler A, Enck P. Functional neuroimaging of visceral sensation. J Clin Neurophysiol. 2000;17(6):604–12.
Aziz Q, Thompson DG, Ng VWK, Hamdy S, Sarkar S, Brammer MJ, et al. Cortical processing of human somatic and visceral sensation. J Neurosci. 2000;20(7):2657–63.
Naliboff BD, Berman S, Suyenobu B, Labus JS, Chang L, Stains J, et al. Longitudinal change in perceptual and brain activation response to visceral stimuli in irritable bowel syndrome patients. Gastroenterology. 2006;131(2):352–65.
van Dyck Z, Vogele C, Blechert J, Lutz AP, Schulz A, Herbert BM. The water load test as a measure of gastric interoception: development of a two-stage protocol and application to a healthy female population. PLoS One. 2016;11(9): e0163574. https://doi.org/10.1371/journal.pone.0163574.
Frank GK, Oberndorfer TA, Simmons AN, Paulus MP, Fudge JL, Yang TT, et al. Sucrose activates human taste pathways differently from artificial sweetener. Neuroimage. 2008;39(4):1559–69. https://doi.org/10.1016/j.neuroimage.2007.10.061.
Bohon C, Stice E, Spoor S. Female emotional eaters show abnormalities in consummatory and anticipatory food reward: a functional magnetic resonance imaging study. Int J Eat Disord. 2009;42(3):210–21. https://doi.org/10.1002/eat.20615.
Mayeli A, Al Zoubi O, White EJ, Chappelle S, Kuplicki R, Smith R, et al. Neural indicators of human gut feelings. BioRxiv. 2021. https://doi.org/10.1101/2021.02.11.430867.
•• Smith R, Mayeli A, Taylor S, Al Zoubi O, Naegele J, Khalsa SS. Gut inference: a computational modelling approach. Biol Psychol. 2021;164:108152. https://doi.org/10.1016/j.biopsycho.2021.108152. This novel study combined minimally invasive mechansoensory stimulation of stomach afferents via a vibrating capsule with Bayesian computational modeling in healthy individuals. The study showed that prior beliefs regarding the state of the stomach evolve during the task as individuals learn through exposure to stimulation. This type of approach is ideal for investigations of gastrointestinal interoception in eating disorders.
• Greenway FL, Aronne LJ, Raben A, Astrup A, Apovian CM, Hill JO, et al. A randomized, double-blind, placebo-controlled study of Gelesis100: a novel nonsystemic oral hydrogel for weight loss. Obesity. 2019;27(2):205-16. https://doi.org/10.1002/oby.22347. A hydrogel capsule which increases the volume and elasticity of stomach and small intestine contents, a minimally invasive perturbation method that could be integrated with other assessments in eating disorders research.
Monti A, Porciello G, Panasiti MS, Aglioti SM. Gut markers of bodily self-consciousness BioRxiv. 2021. https://doi.org/10.1101/2021.03.05.434072.
• Carson DA, O'Grady G, Du P, Gharibans AA, Andrews CN. Body surface mapping of the stomach: new directions for clinically evaluating gastric electrical activity. Neurogastroenterol Motil. 2021;33(3):e14048. https://doi.org/10.1111/nmo.14048. A high-resolution method for non-invasively mapping spatial patterns of gastric activity in relation to gastrointestinal symptoms, that could be applied to eating disorders.
• Rebollo I, Devauchelle AD, Beranger B, Tallon-Baudry C. Stomach-brain synchrony reveals a novel, delayed-connectivity resting-state network in humans. eLife. 2018;7. https://doi.org/10.7554/eLife.33321. A noteworthy approach to probing resting state networks between the brain and stomach, that could be applied to inform the study of gastrointestinal interoception in eating disorders.
Porciello G, Monti A, Aglioti SM. How the stomach and the brain work together at rest. eLife. 2018;7. https://doi.org/10.7554/eLife.37009.
• Baggio LL, Drucker DJ. Glucagon-like peptide-1 receptors in the brain: controlling food intake and body weight. J Clin Invest. 2014;124(10):4223-6. https://doi.org/10.1172/JCI78371. This review outlines the mechanisms of GLP-1 agonsim, showing that sites of action within the nervous system include those prominently involved in interoception including the vagus nerve, brainstem (nucleus of the solitary tract, area postrema) and hypothalamus (arcuate nucleus). We suggest that this approach is worth studying in certain eating disorders (such as BED) to modulate hunger signals, food craving, and interoceptive neurocircuitry.
Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384(11):989. https://doi.org/10.1056/NEJMoa2032183.
Deloose E, Vos R, Janssen P, Van den Bergh O, Van Oudenhove L, Depoortere I, et al. The motilin receptor agonist erythromycin stimulates hunger and food intake through a cholinergic pathway. Am J Clin Nutr. 2016;103(3):730–7. https://doi.org/10.3945/ajcn.115.113456.
Pickrahn S, Dawid C, Babinger T, Schmid C, Brockhoff A, Meyerhof W, et al. Sensory-guided multidimensional exploration of antisweet principles from Gymnema sylvestre (Retz) Schult. J Agric Food Chem. 2021;69(19):5510–27. https://doi.org/10.1021/acs.jafc.1c00994.
Kaelberer MM, Rupprecht LE, Liu WW, Weng P, Bohorquez DV. Neuropod cells: the emerging biology of gut-brain sensory transduction. Annu Rev Neurosci. 2020;43:337–53. https://doi.org/10.1146/annurev-neuro-091619-022657.
•• Kaye WH, Wierenga CE, Bischoff-Grethe A, Berner LA, Ely AV, Bailer UF, et al. Neural insensitivity to the effects of hunger in women remitted from anorexia nervosa. Am J Psychiatry. 2020;177(7):601-10. https://doi.org/10.1176/appi.ajp.2019.19030261. Using a 16-hour fast, this study found that manipulating hunger elicited opposing responses on functional coupling between the insula and ventral caudal putamen in AN. According to the ensuing model, hunger-induced alterations of insular activation leads to feed-forward modulation of dopaminergic activity in the striatum resulting in abnormal food-related motivation and impaired motoric execution of consummatory behaviors.
Nederkoorn C, Smulders FT, Jansen A. Cephalic phase responses, craving and food intake in normal subjects. Appetite. 2000;35(1):45–55. https://doi.org/10.1006/appe.2000.0328.
Schaefer LM, Steinglass JE. Reward Learning through the lens of RDoC: a review of theory, assessment, and empirical findings in the eating disorders. Curr Psychiatry Rep. 2021;23(1):2. https://doi.org/10.1007/s11920-020-01213-9.
Foerde K, Daw ND, Rufin T, Walsh BT, Shohamy D, Steinglass JE. Deficient goal-directed control in a population characterized by extreme goal pursuit. J Cogn Neurosci. 2021;33(3):463–81. https://doi.org/10.1162/jocn_a_01655.
Kristjansson A, Helgadottir A, Kristjansson T. Eating disorder symptoms and foraging for food related items. J Eat Disord. 2021;9(1):18. https://doi.org/10.1186/s40337-021-00373-0.
Kerr KL, Moseman SE, Avery JA, Bodurka J, Simmons WK. Influence of visceral interoceptive experience on the brain’s response to food images in anorexia nervosa. Psychosom Med. 2017;79(7):777–84. https://doi.org/10.1097/PSY.0000000000000486.
Pangborn RM, Witherly SA, Jones F. Parotid and whole-mouth secretion in response to viewing, handling, and sniffing food. Perception. 1979;8(3):339–46. https://doi.org/10.1068/p080339.
Ferdenzi C, Fournel A, Thevenet M, Coppin G, Bensafi M. Viewing olfactory affective responses through the sniff prism: effect of perceptual dimensions and age on olfactomotor responses to odors. Front Psychol. 2015;6:1776. https://doi.org/10.3389/fpsyg.2015.01776.
Yeomans MR. Olfactory influences on appetite and satiety in humans. Physiol Behav. 2006;89(1):10–4. https://doi.org/10.1016/j.physbeh.2006.04.010.
Islam MA, Fagundo AB, Arcelus J, Aguera Z, Jimenez-Murcia S, Fernandez-Real JM, et al. Olfaction in eating disorders and abnormal eating behavior: a systematic review. Front Psychol. 2015;6:1431. https://doi.org/10.3389/fpsyg.2015.01431.
Bentz M, Guldberg J, Vangkilde S, Pedersen T, Plessen KJ, Jepsen JR. Heightened olfactory sensitivity in young females with recent-onset anorexia nervosa and recovered individuals. PLoS ONE. 2017;12(1): e0169183. https://doi.org/10.1371/journal.pone.0169183.
Avery JA, Kerr KL, Ingeholm JE, Burrows K, Bodurka J, Simmons WK. A common gustatory and interoceptive representation in the human mid-insula. Hum Brain Mapp. 2015;36(8):2996–3006. https://doi.org/10.1002/hbm.22823.
Critchley HD, Harrison NA. Visceral influences on brain and behavior. Neuron. 2013;77(4):624–38. https://doi.org/10.1016/j.neuron.2013.02.008.
Weltens N, Zhao D, Van Oudenhove L. Where is the comfort in comfort foods? Mechanisms linking fat signaling, reward, and emotion. Neurogastroenterol Motil. 2014;26(3):303–15. https://doi.org/10.1111/nmo.12309.
Rolls ET, Critchley HD, Verhaagen JV, Kadohisa M. The representation of information about taste and odor in the orbitofrontal cortex. Chemosens Percept. 2010;3:16–33. https://doi.org/10.1007/s12078-009-9054-4.
•• Roelofs TJM, Luijendijk MCM, van der Toorn A, Camps G, Smeets PAM, Dijkhuizen RM, et al. Good taste or gut feeling? A new method in rats shows oro-sensory stimulation and gastric distention generate distinct and overlapping brain activation patterns. Int J Eat Disord. 2021;54(7):1116-26. https://doi.org/10.1002/eat.23354. This functional neuroimaging study in rats observed ventral tegmental, brainstem, and insular cortex responses to repeated sucrose in rats. Gastric distension in the same animals produced greater brainstem and insula activation. This epitomizes a reverse-translational model for human/animal studies of gastrointestinal interoception.
Chao AM, Roy A, Franks AT, Joseph PV. A systematic review of taste differences among people with eating disorders. Biol Res Nurs. 2020;22(1):82–91. https://doi.org/10.1177/1099800419872824.
Marzola E, Cavallo F, Pradella P, Brustolin A, Abbate-Daga G. A tasting experiment comparing food and nutritional supplement in anorexia nervosa. Appetite. 2020;155: 104789. https://doi.org/10.1016/j.appet.2020.104789.
Frank GK, Shott, M.E., Hagman, J.O, Mittal, V.A. Alterations in brain structures related to taste reward circuitry in ill and recovered anorexia nervosa and in bulimia nervosa. Am J Psychiatry. 2013;170(10):1152-60. https://doi.org/10.1176/appi.ajp.2013.12101294.
Wagner A, Aizenstein H, Mazurkewicz L, Fudge J, Frank GK, Putnam K, et al. Altered insula response to taste stimuli in individuals recovered from restricting-type anorexia nervosa. Neuropsychopharmacology. 2008;33(3):513–23.
Wagner A, Simmons AN, Oberndorfer TA, Frank GK, McCurdy-McKinnon D, Fudge JL, et al. Altered sensitization patterns to sweet food stimuli in patients recovered from anorexia and bulimia nervosa. Psychiatry Res. 2015;234(3):305–13. https://doi.org/10.1016/j.pscychresns.2015.10.010.
Setsu R, Hirano Y, Tokunaga M, Takahashi T, Numata N, Matsumoto K, et al. Increased subjective distaste and altered insula activity to umami tastant in patients with bulimia nervosa. Front Psych. 2017;8:172. https://doi.org/10.3389/fpsyt.2017.00172.
Frank GK, Shott ME, Keffler C, Cornier MA. Extremes of eating are associated with reduced neural taste discrimination. Int J Eat Disord. 2016;49(6):603–12. https://doi.org/10.1002/eat.22538.
Frank GKW, Shott ME, Stoddard J, Swindle S, Pryor TL. Association of brain reward response with body mass index and ventral striatal-hypothalamic circuitry among young women with eating disorders. JAMA Psychiat. 2021. https://doi.org/10.1001/jamapsychiatry.2021.1580.
Frank GKW, Reynolds JR, Shott ME, O’Reilly RC. Altered temporal difference learning in bulimia nervosa. Biol Psychiat. 2011;70(8):728–35.
Aouad P, Hay P, Soh N, Touyz S, Mannan H, Mitchison D. Chew and spit (CHSP) in a large adolescent sample: prevalence, impact on health-related quality of life, and relation to other disordered eating features. Eating Disorders. 2019:1–14. https://doi.org/10.1080/10640266.2019.1695449.
Schmalbach I, Herhaus B, Passler S, Schmalbach B, Berth H, Petrowski K. Effects of stress on chewing and food intake in patients with anorexia nervosa. Int J Eat Disord. 2021;54(7):1160–70. https://doi.org/10.1002/eat.23500.
Klein D, Schenbendach J, Brown A, Smith G, Walsh B. Modified sham feeding of sweet solutions in women with and without bulimia nervosa. Physiol Behav. 2009;96(1):44–50.
Klein DA, Schebendach JE, Gershkovich M, Smith GP, Walsh BT. Modified sham feeding of sweet solutions in women with anorexia nervosa. Physiol Behav. 2010;101(1):132–40. https://doi.org/10.1016/j.physbeh.2010.04.030.
Camilleri M. Gastrointestinal function. In: Robertson D, Biaggioni I, Burnstock G, Low PA, Paton JF, editors. Primer on the autonomic nervous system. 3rd ed. London: Elsevier; 2012. p. 205–9.
Soros P, Al-Otaibi F, Wong SW, Shoemaker JK, Mirsattari SM, Hachinski V, et al. Stuttered swallowing: electric stimulation of the right insula interferes with water swallowing. A case report BMC Neurol. 2011;11:20. https://doi.org/10.1186/1471-2377-11-20.
Cremonini F, Camilleri M, Clark MM, Beebe TJ, Locke GR, Zinsmeister AR, et al. Associations among binge eating behavior patterns and gastrointestinal symptoms: a population-based study. Int J Obes. 2009;33(3):342–53. https://doi.org/10.1038/ijo.2008.272.
Holmes SR, Sabel AL, Gaudiani JL, Gudridge T, Brinton JT, Mehler PS. Prevalence and management of oropharyngeal dysphagia in patients with severe anorexia nervosa: a large retrospective review. Int J Eat Disord. 2016;49(2):159–66. https://doi.org/10.1002/eat.22441.
Riedlinger C, Schmidt G, Weiland A, Stengel A, Giel KE, Zipfel S, et al. Which symptoms, complaints and complications of the gastrointestinal tract occur in patients with eating disorders? A systematic review and quantitative analysis. Front Psych. 2020;11:195. https://doi.org/10.3389/fpsyt.2020.00195.
Nicely TA, Lane-Loney S, Masciulli E, Hollenbeak CS, Ornstein RM. Prevalence and characteristics of avoidant/restrictive food intake disorder in a cohort of young patients in day treatment for eating disorders. J Eat Disord. 2014;2(1):21. https://doi.org/10.1186/s40337-014-0021-3.
Holmes SR, Gudridge TA, Gaudiani JL, Mehler PS. Dysphagia in severe anorexia nervosa and potential therapeutic intervention: a case series. Ann Otol Rhinol Laryngol. 2012;121(7):449–56. https://doi.org/10.1177/000348941212100705.
Hosotsubo M, Magota T, Egusa M, Miyawaki T, Matsumoto T. Fabrication of artificial food bolus for evaluation of swallowing. PLoS One. 2016;11(12): e0168378. https://doi.org/10.1371/journal.pone.0168378.
Santos CM, Cassiani RA, Dantas RO. Videofluoroscopic evaluation of swallows in anorexia nervosa. Arq Gastroenterol. 2016;53(3):136–40. https://doi.org/10.1590/S0004-28032016000300003.
Kiss A, Wiesnagrotzki S, Abatzi TA, Meryn S, Haubenstock A, Base W. Upper gastrointestinal endoscopy findings in patients with long-standing bulimia nervosa. Gastrointest Endosc. 1989;35(6):516–8. https://doi.org/10.1016/s0016-5107(89)72901-1.
Wijlens AGM, Erkner A, Alexander E, Mars M, Smeets PAM, de Graaf C. Effects of oral and gastric stimulation on appetite and energy intake. Obesity. 2012;20(11):2226–32. https://doi.org/10.1038/oby.2012.131.
Malczyk Z, Oswiecimska JM. Gastrointestinal complications and refeeding guidelines in patients with anorexia nervosa. Psychiatr Pol. 2017;51(2):219–29. https://doi.org/10.12740/PP/65274.
Garfinkel SN, Seth AK, Barrett AB, Suzuki K, Critchley HD. Knowing your own heart: distinguishing interoceptive accuracy from interoceptive awareness. Biol Psychol. 2015;104:65–74. https://doi.org/10.1016/j.biopsycho.2014.11.004.
Garfinkel SN, Tiley C, O’Keeffe S, Harrison NA, Seth AK, Critchley HD. Discrepancies between dimensions of interoception in autism: implications for emotion and anxiety. Biol Psychol. 2016;114:117–26. https://doi.org/10.1016/j.biopsycho.2015.12.003.
Paulus MP, Feinstein JS, Khalsa SS. An active inference approach to interoceptive psychopathology. Annu Rev Clin Psychol. 2019;15:97–122. https://doi.org/10.1146/annurev-clinpsy-050718-095617.
Mellander A, Jarbur K, Sjovall H. Pressure and frequency dependent linkage between motility and epithelial secretion in human proximal small intestine. Gut. 2000;46(3):376–84. https://doi.org/10.1136/gut.46.3.376.
Edelbroek M, Horowitz M, Dent J, Sun WM, Malbert C, Smout A, et al. Effects of duodenal distention on fasting and postprandial antropyloroduodenal motility in humans. Gastroenterology. 1994;106(3):583–92. https://doi.org/10.1016/0016-5085(94)90689-0.
Schmidt B, Hammer J, Holzer P, Hammer HF. Chemical nociception in the jejunum induced by capsaicin. Gut. 2004;53(8):1109–16. https://doi.org/10.1136/gut.2003.029793.
Hirakawa M, Okada T, Iida M, Tamai H, Kobayashi N, Nakagawa T, et al. Small bowel transit time measured by hydrogen breath test in patients with anorexia nervosa. Dig Dis Sci. 1990;35(6):733–6. https://doi.org/10.1007/BF01540176.
Inui A, Namiki M, Morita S, Okada M, Kasuga M. Anorexia nervosa and intussusception. Lancet. 1996;347(8998):399. https://doi.org/10.1016/s0140-6736(96)90576-0.
Sileri P, Franceschilli L, De Lorenzo A, Mezzani B, Todisco P, Giorgi F, et al. Defecatory disorders in anorexia nervosa: a clinical study. Tech Coloproctol. 2014;18(5):439–44. https://doi.org/10.1007/s10151-013-1068-x.
Chiarioni G, Bassotti G, Monsignori A, Menegotti M, Salandini L, Di Matteo G, et al. Anorectal dysfunction in constipated women with anorexia nervosa. Mayo Clin Proc. 2000;75(10):1015–9. https://doi.org/10.4065/75.10.1015.
Chun AB, Sokol MS, Kaye WH, Hutson WR, Wald A. Colonic and anorectal function in constipated patients with anorexia nervosa. Am J Gastroenterol. 1997;92(10):1879–83.
Cooke W. Laxative abuse. Clin Gastroenterol. 1977;6(3):659–73.
Nunn K, Framptom I, Fuglset T, Torzsok-Sonnevend M, Lask B. Anorexia nervosa and the insula. Med Hypotheses. 2011;76:353–7.
Zucker NL, Merwin RM, Bulik CM, Moskovich A, Wildes JE, Groh J. Subjective experience of sensation in anorexia nervosa. Behav Res Ther. 2013;51(6):256–65. https://doi.org/10.1016/j.brat.2013.01.010.
Pollatos O, Kurz A-L, Albrecht J, Schreder T, Kleemann A, Schopf V, et al. Reduced perception of bodily signals in anorexia nervosa. Eat Behav. 2008;9:381–8. https://doi.org/10.1016/j.eatbeh.2008.02.001.
Kerr KL, Moseman SE, Avery JA, Bodurka J, Zucker NL, Simmons WK. Altered insula activity during visceral interoception in weight-restored patients with anorexia nervosa. Neuropsychopharmacology. 2016;41(2):521–8. https://doi.org/10.1038/npp.2015.174.
Brown TA, Vanzhula IA, Reilly EE, Levinson CA, Berner LA, Krueger A, et al. Body mistrust bridges interoceptive awareness and eating disorder symptoms. J Abnorm Psychol. 2020;129(5):445–56. https://doi.org/10.1037/abn0000516.
Kerr K, Moseman S, Avery J, Bodurka J, Zucker N, Kyle SW. Altered insula activity during visceral interoception in weight-restored patients with anorexia nervosa Neuropsychopharm. 2016;41(2):521–8. https://doi.org/10.1038/npp.2015.174.
Berner LA, Simmons AN, Wierenga CE, Bischoff-Grethe A, Paulus MP, Bailer UF, et al. Altered anticipation and processing of aversive interoceptive experience among women remitted from bulimia nervosa. Neuropsychopharmacology. 2019;44(7):1265–73. https://doi.org/10.1038/s41386-019-0361-4.
Berner LA, Simmons AN, Wierenga CE, Bischoff-Grethe A, Paulus MP, Bailer UF, et al. Altered interoceptive activation before, during, and after aversive breathing load in women remitted from anorexia nervosa. Psychol Med. 2018;48(1):142–54. https://doi.org/10.1017/S0033291717001635.
• Lapidus RC, Puhl M, Kuplicki R, Stewart JL, Paulus MP, Rhudy JL, et al. Heightened affective response to perturbation of respiratory but not pain signals in eating, mood, and anxiety disorders. PLoS One. 2020;15(7):e0235346. https://doi.org/10.1371/journal.pone.0235346. A study demonstrating that heightened sensitivity to respiratory sensations is a characteristic of individuals with eating disorders above and beyond indivudals with mood and/or anxiety disorders.
Khalsa SS, Craske MG, Li W, Vangala S, Strober M, Feusner JD. Altered interoceptive awareness in anorexia nervosa: effects of meal anticipation, consumption and bodily arousal. Int J Eat Disord. 2015;48(7):889–97. https://doi.org/10.1002/eat.22387.
Khalsa SS, Hassanpour MS, Strober M, Craske MG, Arevian AC, Feusner JD. Interoceptive anxiety and body representation in anorexia nervosa. Front Psych. 2018;9:444. https://doi.org/10.3389/fpsyt.2018.00444.
Boswell JF, Anderson LM, Oswald JM, Reilly EE, Gorrell S, Anderson DA. A preliminary naturalistic clinical case series study of the feasibility and impact of interoceptive exposure for eating disorders. Behav Res Ther. 2019;117:54–64. https://doi.org/10.1016/j.brat.2019.02.004.
Plasencia M, Sysko R, Fink K, Hildebrandt T. Applying the disgust conditioning model of food avoidance: a case study of acceptance-based interoceptive exposure. Int J Eat Disord. 2019;52(4):473–7. https://doi.org/10.1002/eat.23045.
• Zucker NL, LaVia MC, Craske MG, Foukal M, Harris AA, Datta N, et al. Feeling and body investigators (FBI): ARFID division-an acceptance-based interoceptive exposure treatment for children with ARFID. The International journal of eating disorders. 2019;52(4):466-72. https://doi.org/10.1002/eat.22996. A novel acceptance-based approach to interoceptive exposure for children using playful cartooons and developmentally appropriate exposures that helps them to link interoceptive sensations with conceptual representations.
Richter F, Garcia AM, Rodriguez Arriagada N, Yoris A, Birba A, Huepe D, et al. Behavioral and neurophysiological signatures of interoceptive enhancements following vagus nerve stimulation. Hum Brain Mapp. 2021;42(5):1227–42. https://doi.org/10.1002/hbm.25288.
Wolf V, Kuhnel A, Teckentrup V, Koenig J, Kroemer NB. Does transcutaneous auricular vagus nerve stimulation affect vagally mediated heart rate variability? A living and interactive Bayesian meta-analysis. Psychophysiology. 2021:e13933. https://doi.org/10.1111/psyp.13933.
Feinstein JS, Khalsa SS, Yeh H, Al Zoubi O, Arevian AC, Wohlrab C, et al. The elicitation of relaxation and interoceptive awareness using floatation therapy in individuals with high anxiety sensitivity. Biological Psychiat: Cognitive Neuroscience and Neuroimaging. 2018;3(6):555–62. https://doi.org/10.1016/j.bpsc.2018.02.005.
• Khalsa SS, Moseman SE, Yeh HW, Upshaw V, Persac B, Breese E, et al. Reduced environmental stimulation in anorexia nervosa: an early-phase clinical trial. Frontiers in psychology. 2020;11:567499. https://doi.org/10.3389/fpsyg.2020.567499. This safety trial found that acute exposure to flotation therapy is safe and well tolerated in individuals with AN. Additionally, there was evidence that the floatation environment increased cardiac and respiratory but not gastrointestinal interoception.
Funding
Preparation of this work was supported by the National Institute of Mental Health [R01MH127225 (S. S. K.), K23MH112949 (S. S. K.), K23MH118418 (L. A. B.), K23MH123910 (L. M. A.)], the William K. Warren Foundation (S. S. K.), and by a NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation (L. A. B.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the official views of the National Institutes of Health. Figure 1 created with BioRender.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Eating Disorders
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khalsa, S.S., Berner, L.A. & Anderson, L.M. Gastrointestinal Interoception in Eating Disorders: Charting a New Path. Curr Psychiatry Rep 24, 47–60 (2022). https://doi.org/10.1007/s11920-022-01318-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11920-022-01318-3