Abstract
Purpose of Review
Gastric neuroendocrine neoplasms (g-NENs) are a rare type of stomach cancer. The three main subtypes have different pathogeneses, biological behaviours and clinical characteristics, so they require different management strategies. This article will provide an overview of g-NENs and highlight recent advances in the field.
Recent Findings
Molecular profiling has revealed differences between indolent and aggressive g-NENs, as well as a new somatic mutation responsible for some familial type I g-NENs. Novel biomarkers have been developed which will hopefully improve diagnosis, treatment, risk stratification and follow-up. Patient treatment is also changing, as evidence supports the use of less aggressive options (e.g. endoscopic surveillance or resection) in some patients with more indolent tumours.
Summary
g-NEN heterogeneity poses challenges in understanding and managing this rare disease. More basic science research is needed to investigate molecular pathogenesis, and future larger clinical studies will hopefully also further improve treatment and patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
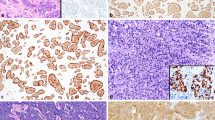
Neuroendocrine neoplasms (NENs) are heterogeneous tumours which have diverse clinical and biological characteristics. They arise from secretory cells of the diffuse neuroendocrine system, can occur at almost any anatomical site and share major molecular morphological and protein expression signatures as well as site-specific markers. Overall, NENs are subdivided into well-differentiated neuroendocrine tumours (NETs), poorly differentiated neuroendocrine carcinomas (NECs) and mixed neuroendocrine-non-neuroendocrine neoplasms (MiNENs), in which both components are substantial and account for at least 30% of the total neoplasm [1]. NEN classification is based on the type of tumour differentiation and the extent of tumour proliferation (grade) as determined by mitotic index and Ki-67 immunohistochemistry (Table 1). An increased risk of angioinvasion and metastatic potential is seen in higher grade and more poorly differentiated tumours, and, if disseminated, such NENs have a poorer prognosis.
Gastric neuroendocrine neoplasms (g-NENs) are relatively rare, and multiple observational studies have shown that they account for approximately 7% of all digestive NENs [2] and less than 1% of all gastric neoplasms [3]. However, the incidence of g-NENs has increased in most countries over recent decades, in part because of greater awareness of the disease among clinicians, improved diagnostic techniques and more widespread use of upper gastrointestinal endoscopy [4]. This has led to improvements in our understanding of disease biology, contributed to changes in management and opened new avenues of research. In this article, we will discuss some the most exciting recent developments in understanding of the molecular pathogenesis, management and prognosis of gastric NENs over the last 5 years. We identified the themes and references that have been included in this article by searching PubMed from 2016 to 2021 using the key search terms ‘gastric, stomach, neuroendocrine, carcinoid, neuroendocrine carcinoma, mixed neuroendocrine-non-neuroendocrine neoplasms’.
Current Classification and Management of Gastric NENs
Gastric NENs are thought to arise from subepithelial, histamine-secreting, enterochromaffin-like (ECL) cells and are conventionally subdivided into three main types which have very different and distinct pathophysiologies (Fig. 1). Type I g-NENs are associated with autoimmune atrophic gastritis and hypochlorhydria, while type II g-NENs develop in some patients who have gastrinomas, increased gastric acid secretion, Zollinger-Ellison syndrome (ZES) and multiple neuroendocrine neoplasia (MEN) type 1. Both type I and type II g-NENs are associated with elevated fasting serum gastrin concentrations, and many patients have a relatively indolent disease course and good prognosis. Hypergastrinaemia exerts a proliferative effect on ECL-cells in the stomach, leading to linear and micronodular ECL-cell hyperplasia and subsequently dysplasia and NEN development. By contrast, type III g-NENs are sporadic tumours, and gastrin is not thought to be involved in their pathogenesis. Type III g-NENs tend to behave more aggressively and often have a poorer prognosis.
Pathophysiology of g-NENs. A Physiological gastric acid secretion: Antral G cells release gastrin after the ingestion of food. Gastrin binds to the CCK2 receptor on corpus-located enterochromaffin-like (ECL) cells, and this cell type then produces histamine. Histamine then binds to H2 receptors on gastric parietal cells resulting in stimulation of acid production and a reduction in the pH in the gastric lumen. This initiates an inhibitory feedback loop to downregulate gastrin release mediated by somatostatin-producing D cells which directly inhibits further release of gastrin from G cells. B Type I g-NENs: Loss of parietal cells disrupts the inhibitory loop leading to antral G cell hyperplasia and hypergastrinaemia. This leads to ECL-cell hyperplasia and eventually type I g-NEN formation. Potential treatment targets on the ECL cell are the CCK2 receptor and the somatostatin receptor (SSR). Netazepide irreversibly binds to the CCK2 receptor, and somatostatin analogues (SSAs) bind to the SSR with anti-proliferative effects. C Type II g-NENs: Ectopic G cell neoplasia leads to hypergastrinaemia and resultant excess gastric acid production that is independent of the normal inhibitory feedback loop. ECL cell and parietal cell hyperplasia are observed. D Type III g-NENs: Sporadic formation of g-NEN derived from ECL cells occurs with no evidence of hypergastrinaemia and no known disturbance of underlying gastric physiology. Created with BioRender.com
In addition to these classical three subtypes, the existence of a type IV g-NEN has been suggested. One proposition has been that this fourth type has similar characteristics to type III g-NENs, but an even more aggressive nature. This type of g-NEN may arise from other types of endocrine cells (that secrete serotonin, gastrin or adrenocorticotrophic hormone) and be a poorly differentiated NEC [5, 6]. In modern NEN classification systems, however, it is likely that this type of type IV g-NEN simply represents a type III g-NEN which has features of a NEC rather than a NET. A second different proposal for a type IV g-NEN involves a g-NEN that has developed in a patient who has an intrinsic defect in the secretion of acid by gastric parietal cells. This type of type-IV g-NEN is characterised by hypochlorhydria, hypergastrinaemia and multiple small gastric polyps (similar to type I), but histological examination of the gastric corpus mucosa classically reveals hypertrophy and hyperplasia of parietal cells, with a vacuolated cytoplasm suggesting a structural abnormality that prevents acid secretion [7,8,9]. This type of g-NEN is very rare, and the mechanism of pathogenesis is similar to type I, so it is not frequently included as a separate entity in g-NEN classification systems.
Clinically, most g-NENs tend to be asymptomatic, and many tumours are identified incidentally during an endoscopy that is being performed to investigate unrelated symptoms or anaemia. Once detected, it is essential to determine the subtype of g-NEN through biochemical, histological and endoscopic assessment in order to provide appropriate management. The three main subtypes of g-NEN have typical clinical and biochemical features (Table 2). Computerised tomography (CT) with gastric distention can be helpful for tumour staging and provides information that is complementary to gastroscopy and histological evaluation. In contrast to well differentiated g-NETs, g-NECs or g-MiNENs are more likely to be found in the gastric fundus and cardia, have larger size, grow infiltratively, have unclear tumour margins, involve the serosa, appear ulcerated, demonstrate heterogeneous enhancement and have metastatic lymph nodes (LN) detected on CT scan [10]. The appearance of intact overlying mucosa with mucosal tenting can also sometimes help in discriminating between g-NECs and gastric adenocarcinomas [11]. Furthermore, a larger size and greater necrotic volume of metastatic LNs can also be a feature of g-NECs rather than gastric adenocarcinoma [11].
The management of a g-NEN critically depends on three key parameters: the tumour subtype, histological grade and tumour stage [12]. Treatment options range through endoscopic surveillance with or without endoscopic polypectomy, to medical management, to aggressive surgery and to oncological therapies. Optimal patient management should be determined by a suitably qualified multidisciplinary team of clinicians and is influenced by the type, size, multiplicity, grade and stage of g-NEN. These features have been summarised in Table 2.
Recent Advances in Understanding the Pathogenesis of Gastric NENs
Molecular Profiling of Gastric Neuroendocrine Tumours
The rarity of neuroendocrine malignancies limits the biomedical scientific community’s ability to develop new therapies; hence, a better understanding of their underlying tumour biology is critical. A number of recent studies have investigated the molecular features that are associated with gastric NETs, NECs, MiNENs and gastric adenocarcinomas in order to determine the similarities and differences between these tumour types and provide insights into oncogenesis, as well as potential therapeutic strategies. Mutations in MEN1, DAXX and ATRX genes are entity-defining for well-differentiated NETs at other sites, whereas NECs often have TP53 or RB1 mutations [13••]. In some cases, the presence of these mutations may help in diagnosis and determining treatment [14].
Regarding gastric NETs, a recent whole-exome sequencing study analysed a family in which 5 of 10 siblings developed type I g-NENs. A germline mutation in the ATP4a gene was found to be associated with the presence of disease, but mutations of this gene were not detected in a validation cohort of 14 patients who had sporadic type I g-NENs [15]. Two other small studies have also investigated the molecular profiles of type I g-NENs, but they only analysed 22 cases in total [16, 17]. Sporadic mutations were found in less than 15% of cases for the genes tested (TP53 14%; RB1 9%; and SMAD4 9%), with mutations in NET-related genes also being rare (MEN1 7%, ATRX 7%, TSC2 7% and PETN 5%). By contrast, a whole-exome sequencing study of gastric NECs found that they exhibited a specific mutational pattern, with a higher mutational burden compared with gastric adenocarcinoma [18], and the most frequently mutated gene was TP53 (which was affected in 53–100% of the cases examined).
The pathogenesis and genetic features of gastric MiNENs remains poorly understood. Furthermore, while the survival of patients who have gastric adenocarcinomas is improving due to the development of targeted novel therapies, there are currently no targeted or tailored therapeutic protocols for gastric MiNENs. Current hypotheses suggest that the adenocarcinoma and neuroendocrine components of MiNENs have a clonal origin [19]. In support of this, Koh et al. recently demonstrated that the majority of somatic mutations, especially pathogenic mutations of TP53, were identically shared by the two separate components of gastric MiNENs, thus providing further genetic evidence for a common ancestor model for these tumours [20]. A further study that compared NECs and MiNENs also identified TP53 as the single cancer-related gene that was most frequently mutated in both tumour types [21].
Type I g-NENs and ATP4a Mutations
Calvete et al. used whole exome sequencing to identify a missense mutation (p.R703C) in the human ATP4a gene [15] as the cause of aggressive familial type I g-NENs in homozygous individuals from a single family. Affected individuals showed tumour development at an early age, gastric hypoacidity, hypergastrinaemia, iron-deficiency anaemia, gastric intestinal metaplasia and frequent LN metastasis, with in one case contemporaneous gastric adenocarcinoma.
Traditionally, autoimmune atrophic gastritis in humans develops as the consequence of an IL-17-dependent innate autoimmune response mediated by CD4+ T cells. These T cells recognise the proton pump H+/K+-ATPase, which is coded by the ATP4a gene on parietal cells [22]. Subsequent activation of the NLRP3 inflammasome-reactive oxygen species pathway results in the destruction of parietal cells [23]. Infection with H. pylori also mimics parietal cell antigens in human autoimmune gastritis, promoting destabilisation of the mitochondria, preventing the adaptive immune response and reducing gastric acidity [24].
The functional significance of this newly identified p.R703C mutation in ATP4a has now been investigated further by creating a knockin mouse model [25]. Homozygous mice recapitulated most of the phenotypic alterations observed in human individuals, strongly suggesting that this mutation is the primary alteration responsible for disease development. The mouse model also suggested that achlorhydria might contribute to tumorigenesis to a greater extent than hypergastrinaemia, as gastric acidification prevented or partially reverted the histological changes and rescued abnormal biochemical parameters. Furthermore, the ATP4a p.R703C mutation was shown to deregulate the acid-base balance within parietal cells, affecting mitochondrial biogenesis in a similar manner to H. pylori infection [26••]. Mitochondrial malfunction activated reactive oxygen species signalling, which in turn triggered caspase-3-mediated apoptosis of parietal cells; this malfunction was also restored when mice were treated with acidified water.
Genetically mediated ATP4a mutation induced gastric atrophy and H. pylori induced gastric atrophy therefore seem to alter mitochondrial function through similar mechanisms, but these are different from those found in classical autoimmune atrophic gastritis. Importantly, mitochondrial function in the mouse model was partially recovered when euchlorhydria/gastric acidity was restored during prevention and reversion experiments. This suggests that restoration of gastric acidity might be helpful in such patients and might even have a role in limiting the progression to H. pylori induced atrophic gastritis.
Development of Potential Novel g-NEN Biomarkers
Biomarkers are important adjuncts in the treatment and follow-up of patients with many diseases. For example, the measurement of secretory markers such as gastrin, insulin, glucagon and vasoactive intestinal peptide can be very helpful in monitoring the success of therapy in patients who have specific functional pancreatic NETs [27]. However, a clinically useful universal g-NEN biomarker which identifies both functional and non-functional tumours, which correlates with disease aggressiveness or progress and which is useful for diagnosis and surveillance does not currently exist. Currently employed serum g-NEN biomarkers such as gastrin and chromogranin A concentrations are unfortunately largely ineffective [28]. For example, elevated fasting serum gastrin concentrations are non-specific, and hypergastrinaemia can result from chronic atrophic gastritis, Zollinger-Ellison syndrome, persistent Helicobacter pylori infection and patients taking proton pump inhibitors [29]. The combination of low pepsinogen I/II ratio with high gastrin levels has therefore been proposed as more specific method to characterise and risk stratify patients who have autoimmune atrophic gastritis and type I g-NENs [30]. Measurement of serum chromogranin A concentration also has significant clinical limitations, particularly its lack of sensitivity in determining tumour stage and location, but the results can also be influenced by the specific assay that is used, limiting direct comparison of results that have been obtained at different laboratories [31]. These limitations have led to interest in developing novel biomarkers for g-NENs. This includes the development of potential novel immunohistochemical biomarkers, as these have been shown to provide valuable prognostic and predictive information in other tumour types [32].
Circulating Biomarkers
Circulating Tumour mRNA
An emerging molecular liquid biopsy method involving circulating tumour RNA, the NETest, has been recently developed for several types of NEN. This innovative approach involves the simultaneous measurement of 51 different NET-related transcripts. These cover a multiverse of neuroendocrine cell and tumour biology, and the test yields a single readout through an undisclosed algorithm [33]. In a recent study by Malczewska et al. involving 46 g-NENs (42 type I and 4 type III, of which 3 were NECs), the NETest was positive in patients who had both type I and type 3 g-NENs [34•] with a sensitivity of 100% , specificity of 87% and overall accuracy of 90%. Elevated test results were found in all patients with who had evidence of macroscopic and microscopic residual disease as well as in some patients who had no macroscopic or microscopic disease (possibly as a consequence of background ECL-cell hyperplasia). Therefore, this sensitive liquid biopsy test has potential utility in the future management and surveillance of g-NENs. Further research studies to determine the usefulness of this test in clinical practice and during follow-up are however needed prior to its routine implementation.
miRNAs
MicroRNAs (miRNAs) represent potential novel biomarkers for g-NENs. miRNAs are a class of endogenous non-protein coding short RNAs that post-transcriptionally regulate approximately 30% of the human genome [35, 36]. As miRNAs control a large proportion of the genome, their expression patterns are tissue-specific, and dysregulation has been observed in many malignancies [37]. This suggests that miRNAs may have a role as biomarkers that may prove useful in determining cancer diagnosis, prognosis and response to therapies. miR-222 expression has been found to be increased in both the stomach and serum of patients who had type I g-NENs as well as hypergastrinaemic patients who had autoimmune atrophic gastritis [38]. Furthermore, treatment with the gastrin/CCK2 receptor antagonist, netazepide, was shown to reduce miR-222 abundance. miR-222 therefore has potential utility as a biomarker for response to gastrin/CCK2R antagonist therapy in g-NETs, but further studies involving larger numbers of patients are again needed prior to implementation of this test into routine clinical practice.
Immunohistochemical Biomarkers
PDL1-MMR-MSI
Immunotherapy with immune checkpoint inhibitors (ICIs) has recently been shown to be effective in several metastatic cancers, including malignant melanoma, non-small lung cancer and renal cell carcinoma [39]. Programmed cell death ligand 1 (PD-L1) and programmed cell death protein 1 (PD-1) are two immune checkpoint proteins that play a major role in cancer immunity [40], and these proteins are the targets of some ICI therapies. In some situations, expression of PD-1 has therefore been shown to help in predicting clinical response to ICIs. Furthermore, microsatellite instability (MSI), which is typically caused by mutations in mismatch repair (MMR) genes including MLH1, MSH2, MSH6 and PMS2, has also emerged as a robust and consistent pan-tumour biomarker that predicts benefit in patients treated with ICIs [41].
MSI has been proposed to promote tumour development in both NECs and MiNENs [42,43,44]. Gastric MSI-NECs and MiNENs have been shown to resemble MSI-gastrointestinal adenocarcinomas in terms of their frequency, molecular profiles and pathogenetic mechanisms [42] and thus potentially represent a subset of patients who may be more likely to respond to ICI therapy. A recent study by Yamashita et al. [45•] also identified high PD-L1 expression in 72% of cases in a cohort of 25 g-NEC/MiNEN patients, while Yang et al. found high PD-L1 expression in 49% of 43 g-NECs, and this correlated with poorer prognosis [46]. Whether these observations have implications for the clinical assessment of MSI and PD-L1 status in g-NECs/MiNENs and whether the findings then represent biomarkers that can used to predict response to ICI therapy and influence prognosis remain to be established. However, this is a potentially exciting area of research that may lead to personalisation of treatment approaches and certainly warrants further evaluation.
ALDH1A1
High ALDH1A1 expression may also be a prognostic indicator in patients who have g-NECs. The aldehyde dehydrogenase (ALDH) family of proteins are present at high levels in stem cells as well as cancer stem cells in a number of malignancies [47,48,49] as well as NETs [50]. In gastric adenocarcinoma, overexpression of ALDH1A1 is significantly associated with depth of tumour invasion and LN metastases [51] and predicts poor prognosis in terms of overall survival and recurrence free survival. Ye et al. recently examined the expression of ALDH1A1 in g-NECs and found similar results [52]. High ALDH1A1 expression levels were associated with LN status, lymphovascular invasion (LVI) and Ki-67 index. Furthermore, strongly positive ALDH1A1 expression was found to be an independent prognostic factor associated with poorer survival rates.
Recent Developments in g-NEN Patient Management
Type I g-NENs
Current European Neuroendocrine Tumour Society (ENETS) guidelines recommend conservative management for most type I g-NENs [53]. For this tumour type, the risk of metastatic potential is directly correlated to tumour size [54]. Most patients who have small tumours are therefore enrolled onto endoscopic surveillance programmes, where tumour number and size are monitored and regular histological assessment is undertaken. Endoscopic surveillance has also been advocated by a number of organisations for all patients who have atrophic gastritis, as previous studies have reported a varying progression rate to gastric adenocarcinoma up to 2% per year during long-term follow-up [55, 56]. Current guidelines therefore suggest annual or 2-yearly endoscopic surveillance of type I g-NENs with biopsy sampling of polyps, and endoscopic resection is advised for lesions measuring more than 10 mm in diameter [53].
Recent analysis of the outcomes of endoscopic surveillance programmes [57, 58] has indicated that about 30% of type I g-NET patients will require intervention in the form of endoscopic resection or surgery at some point during their disease course. A reintervention rate of at least 50% (7/13 patients and 44/84 patients in each study) was noted after a median follow-up of 22 and 11 months after first intervention, with a further 50% of patients experiencing multiple recurrences. Interestingly, both of these studies reported that high fasting serum gastrin concentrations were more likely to be associated with disease progression. Multiple endoscopic techniques have been used to resect type I g-NENs including band and slough technique [59], endoscopic mucosal resection (EMR) [60] and endoscopic submucosal dissection (ESD) [61]. All these techniques are feasible and effective with a good safety profile, but no published research to date has suggested that one technique seems to be more effective than the others [62] .
Netazepide is a gastrin/CCK2 receptor antagonist which has recently been identified as a potential novel treatment for hypergastrinaemia-associated conditions [29], with evidence from non-clinical models as well as clinical studies in healthy volunteers [63, 64]. Furthermore, due to the rarity of g-NENS, it has been designated an orphan medicinal product (with dedicated funding) in Europe and the USA for the treatment of type I g-NENs [65]. Treatment with netazepide over 12 weeks was found to reduce the number and size of type I g-NETS, plasma chromogranin A levels and gastric mucosal biomarkers including chromogranin A [66, 67]. This treatment also resulted in similar responses and had a good long-term safety profile when administered to the same patients over a subsequent 52-week period [68]. Further work investigating the action of netazepide using gene expression profiling noted a reduction in the expression of PAPPA2, a metalloproteinase that increases the bioavailability of insulin-like growth factor (IGF) [69•]. These findings were confirmed using patient biopsies acquired pre and post netazepide treatment and suggest that a novel gastrin-dependent IGF signalling pathway may be important in the development of type I g-NETs. Netazepide is therefore possibly an alternative systemic management strategy for some type I g-NETs, either alone or in combination with endoscopic surveillance, although additional larger clinical trials are needed to confirm these initial findings
An alternative medical management option that has recently been evaluated in type I g-NETs involves the use of long-acting somatostatin analogues (SSAs), as these inhibit gastrin release and thus inhibit endocrine cell proliferation [70, 71]. In a recent meta-analysis of results from selected patients who could not be safely managed by endoscopic follow-up or resection due to multiple or frequently recurring disease, SSAs were shown to induce an excellent response rate (i.e. a cumulative complete response rate of 84.5% when considering six prospective studies) after 12 months of therapy. This treatment also had a good safety profile, but was associated with a high cumulative relapse rate of 30% during 34 months of follow-up [72•].
Surgery, in the form of an antrectomy, has historically been advocated to treat some type I g-NENs. This intervention leads to a reduction in circulating gastrin concentrations by removing the anatomical source of hypergastrinaemia. However, it is not effective in all patients, and it carries the risk of morbidity and mortality [73, 74]. No significant recent advances in the role of surgery in the management of type I g-NETs were identified during the literature search that was undertaken in preparation for this article.
Type III g-NENs
For localised type III g-NENs, due to their potentially more aggressive behaviour, surgical resection, in the form of a partial or total gastrectomy with LN dissection, remains the recommended treatment according to the ENETS consensus guidelines [53]. However, a recent systematic review suggested that the majority of type III g-NENs diagnosed in the modern era have a lower grade than historically reported [75•]. Criteria for selecting patients for endoscopic or local resection (without formal LN dissection) have now been accepted for managing other tumour types, including early gastric adenocarcinomas using endoscopic mucosal resection or laparoscopic wedge resection [76, 77] and selected NENs at other sites such as the appendix (by simple appendectomy) [78] and rectum (through transanal excision) [79]. Similar criteria have recently been proposed for type III g-NENs, by defining those tumour subgroups which are associated with a lower rate of LN metastasis. Three recent studies from Asia [80,81,82] and one from Europe [83•] all concluded that local excision in the form of surgical wedge resection or endoscopic resection is a suitable treatment option for certain type III g-NENs when the following criteria are satisfied: well differentiated histology, low grade (grade 1 and potentially some grade 2 NETs with Ki67 index < 10%), tumour size less than 10 (or possibly 15) mm, depth of invasion confined to the submucosal layer and no evidence of LVI.
Recent Developments in g-NEN Patient Outcomes and Prognostic Indicators
Predicting the outcome of patients with g-NENs is complicated, as these tumours are biologically very heterogeneous, so prognosis and management are affected by a number of factors. Multiple studies have demonstrated that patient age, tumour grade, size and type, gender and marital status are prognostic factors that influence clinical outcome in g-NENs [84,85,86]. Perineural invasion in high grade g-NENs is also a predictor of outcome [87]. Neutrophil to lymphocyte ratio in a preoperative blood sample has also been identified as an independent prognostic factor of recurrence free survival and overall survival after surgery [88]. In resected g-NECs, metastatic LN number more than two, the presence of metastatic disease in more than 10% of resected LNs and involvement of station 2 LNs have all been shown to be significant prognostic indicators associated with a poorer prognosis [89]. These features have recently been incorporated into nomograms which can be used to estimate the survival of individual g-NET and g-NEC patients [90]. However, to date, these nomograms have not accounted for the different NET subtypes; thus, additional research in this area is warranted.
The mainstay of treatment of non-metastatic MiNENs and the only chance of cure remains surgical resection. If an adjuvant treatment is indicated, or if the neoplasm is not resectable, the type of chemotherapy administered is dependent on the histological characteristics of each component malignancy (including grade and differentiation status) and which component is thought to represent the more dominant tumour type [43]. A recent study compared long-term survival and patterns of recurrence among g-NECs, g-MiNENs and gastric adenocarcinomas [91]. Patients with a g-NEC or g-MiNEN had poorer prognoses than those with a gastric adenocarcinoma. The presence of a g-NEC or g-MiNEN was independently associated with poorer disease-free survival and post recurrence free survival as well as an increased likelihood of developing distant tumour recurrence.
Conclusions
The heterogeneity and rarity of gastric neuroendocrine neoplasms pose challenges in the understanding and management of this disease. Despite recent advances in the molecular profiling of cancers in general, due to the fragmentary nature of research and the low incidence of g-NENs, no key pathways have yet been identified that are responsible for the development of these tumours. This is currently limiting attempts to molecularly subclassify these tumours and is also hampering efforts to develop novel and/or personalised therapeutic strategies. More basic science research is therefore needed to investigate the molecular subtypes and tumour pathogenesis. Preclinical models would be invaluable to provide better understanding and insight into treatment options. However, the usefulness of currently available neuroendocrine neoplasm cell lines is questionable [92], none have been derived from the stomach, and there are also limited animal models available [93]. Recently, promising NEC organoid models have been established [94], and such technology may also in future be suitable for modelling g-NETs. Recent clinical studies have demonstrated that less aggressive treatment options such as medical management or endoscopic treatment may be appropriate in patients who have smaller and more indolent g-NETs. However, larger clinical studies are still needed to better define eligibility for these treatment strategies as well as to improve patient outcomes in g-NECs and g-MiNENs.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76(2):182–8.
Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3(10):1335–42.
Yang Z, Wang W, Lu J, Pan G, Pan Z, Chen Q, et al. Gastric neuroendocrine tumors (G-Nets): incidence, prognosis and recent trend toward improved survival. Cell Physiol Biochem. 2018;45(1):389–96.
Chen W-F, Zhou P-H, Li Q-L, Xu M-D, Yao L-Q. Clinical impact of endoscopic submucosal dissection for gastric neuroendocrine tumors: a retrospective study from Mainland of China. Sci World J. 2012;2012:869769.
Kloppel G, Rindi G, Anlauf M, Perren A, Komminoth P. Site-specific biology and pathology of gastroenteropancreatic neuroendocrine tumors. Virchows Arch. 2007;451(Suppl 1):S9–27.
Latta E, Rotondo F, Leiter LA, Horvath E, Kovacs K. Ghrelin- and serotonin-producing gastric carcinoid. J Gastrointest Cancer. 2012;43(2):319–23.
Abraham SC, Carney JA, Ooi A, Choti MA, Argani P. Achlorhydria, parietal cell hyperplasia, and multiple gastric carcinoids: a new disorder. Am J Surg Pathol. 2005;29(7):969–75.
Ooi A, Ota M, Katsuda S, Nakanishi I, Sugawara H, Takahashi I. An unusual case of multiple gastric carcinoids associated with diffuse endocrine cell hyperplasia and parietal cell hypertrophy. Endocr Pathol. 1995;6(3):229–37.
Nakata K, Aishima S, Ichimiya H, Yao T, Matsuura T, Seo M, et al. Unusual multiple gastric carcinoids with hypergastrinemia: report of a case. Surg Today. 2010;40(3):267–71.
Yan S, Liu T, Li Y, Zhu Y, Jiang J, Jiang L, et al. Value of computed tomography evaluation in pathologic classification and prognosis prediction of gastric neuroendocrine tumors. Ann Transl Med. 2019;7(20):545.
Kim SH, Kim SH, Kim MA, Shin CI, Han JK, Choi BI. CT differentiation of poorly-differentiated gastric neuroendocrine tumours from well-differentiated neuroendocrine tumours and gastric adenocarcinomas. Eur Radiol. 2015;25(7):1946–57.
Burkitt MD, Pritchard DM. Review article: pathogenesis and management of gastric carcinoid tumours. Aliment Pharmacol Ther. 2006;24(9):1305–20.
•• Alexandraki KI, Spyroglou A, Kykalos S, Daskalakis K, Kyriakopoulos G, Sotiropoulos GC, et al. Changing biological behaviour of NETs during the evolution of the disease: progress on progression. Endocr Relat Cancer. 2021;28(5):R121–R40 This review article describes key molecular pathways in NETs and NECs.
van der Velden DL, Hoes LR, van der Wijngaart H, van Berge Henegouwen JM, van Werkhoven E, Roepman P, et al. The drug rediscovery protocol facilitates the expanded use of existing anticancer drugs. Nature. 2019;574(7776):127–31.
Calvete O, Reyes J, Zuniga S, Paumard-Hernandez B, Fernandez V, Bujanda L, et al. Exome sequencing identifies ATP4A gene as responsible of an atypical familial type I gastric neuroendocrine tumour. Hum Mol Genet. 2015;24(10):2914–22.
Park HY, Kwon MJ, Kang HS, Kim YJ, Kim NY, Kim MJ, et al. Targeted next-generation sequencing of well-differentiated rectal, gastric, and appendiceal neuroendocrine tumors to identify potential targets. Hum Pathol. 2019;87:83–94.
Wang H, Sun L, Bao H, Wang A, Zhang P, Wu X, et al. Genomic dissection of gastrointestinal and lung neuroendocrine neoplasm. Chin J Cancer Res. 2019;31(6):918–29.
Makuuchi R, Terashima M, Kusuhara M, Nakajima T, Serizawa M, Hatakeyama K, et al. Comprehensive analysis of gene mutation and expression profiles in neuroendocrine carcinomas of the stomach. Biomed Res. 2017;38(1):19–27.
Kim KM, Kim MJ, Cho BK, Choi SW, Rhyu MG. Genetic evidence for the multi-step progression of mixed glandular-neuroendocrine gastric carcinomas. Virchows Arch. 2002;440(1):85–93.
Koh J, Nam SK, Kwak Y, Kim G, Kim KK, Lee BC, et al. Comprehensive genetic features of gastric mixed adenoneuroendocrine carcinomas and pure neuroendocrine carcinomas. J Pathol. 2021;253(1):94–105.
Ishida S, Akita M, Fujikura K, Komatsu M, Sawada R, Matsumoto H, et al. Neuroendocrine carcinoma and mixed neuroendocrinenon-neuroendocrine neoplasm of the stomach: a clinicopathological and exome sequencing study. Hum Pathol. 2021;110:1–10.
Toh BH, Sentry JW, Alderuccio F. The causative H+/K+ ATPase antigen in the pathogenesis of autoimmune gastritis. Immunol Today. 2000;21(7):348–54.
Hu Z, Chai J. Structural mechanisms in NLR inflammasome assembly and signaling. Curr Top Microbiol Immunol. 2016;397:23–42.
Amedei A, Bergman MP, Appelmelk BJ, Azzurri A, Benagiano M, Tamburini C, et al. Molecular mimicry between Helicobacter pylori antigens and H+, K+ --adenosine triphosphatase in human gastric autoimmunity. J Exp Med. 2003;198(8):1147–56.
Calvete O, Varro A, Pritchard DM, Barroso A, Oteo M, Morcillo MA, et al. A knockin mouse model for human ATP4aR703C mutation identified in familial gastric neuroendocrine tumors recapitulates the premalignant condition of the human disease and suggests new therapeutic strategies. Dis Model Mech. 2016;9(9):975–84.
•• Benitez J, Marra R, Reyes J, Calvete O. A genetic origin for acid-base imbalance triggers the mitochondrial damage that explains the autoimmune response and drives to gastric neuroendocrine tumours. Gastric Cancer. 2020;23(1):52–63 This article describes the ATP4Ap.R703C mutation in type Ig-NENs.
Falconi M, Eriksson B, Kaltsas G, Bartsch DK, Capdevila J, Caplin M, et al. ENETS consensus guidelines update for the management of patients with functional pancreatic neuroendocrine tumors and non-functional pancreatic neuroendocrine tumors. Neuroendocrinology. 2016;103(2):153–71.
Hofland J, Zandee WT, de Herder WW. Role of biomarker tests for diagnosis of neuroendocrine tumours. Nat Rev Endocrinol. 2018;14(11):656–69.
Boyce M, Lloyd KA, Pritchard DM. Potential clinical indications for a CCK2 receptor antagonist. Curr Opin Pharmacol. 2016;31:68–75.
Magris R, De Re V, Maiero S, Fornasarig M, Guarnieri G, Caggiari L, et al. Low pepsinogen I/II ratio and high gastrin-17 levels typify chronic atrophic autoimmune gastritis patients with gastric neuroendocrine tumors. Clin Transl Gastroenterol. 2020;11(9):e00238.
Malczewska A, Oberg K, Kos-Kudla B. NETest is superior to chromogranin A in neuroendocrine neoplasia: a prospective ENETS CoE analysis. Endocr Connect. 2021;10(1):110–23.
Uccella S, La Rosa S, Volante M, Papotti M. Immunohistochemical biomarkers of gastrointestinal, pancreatic, pulmonary, and thymic neuroendocrine neoplasms. Endocr Pathol. 2018;29(2):150–68.
Modlin IM, Drozdov I, Kidd M. The identification of gut neuroendocrine tumor disease by multiple synchronous transcript analysis in blood. PLoS One. 2013;8(5):e63364.
• Malczewska A, Procner A, Walter A, Kusnierz K, Zajecki W, Aslanian H, et al. The NETest liquid biopsy is diagnostic for gastric neuroendocrine tumors: observations on the blood-based identification of microscopic and macroscopic residual diseaseOK. BMC Gastroenterol. 2020;20(1):235 This article describes a novel serum biomarker the NETest.
Lewis BP, Burge CB, Bartel DP. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell. 2005;120(1):15–20.
Berezikov E, Guryev V, van de Belt J, Wienholds E, Plasterk RH, Cuppen E. Phylogenetic shadowing and computational identification of human microRNA genes. Cell. 2005;120(1):21–4.
Lu J, Getz G, Miska EA, Alvarez-Saavedra E, Lamb J, Peck D, et al. MicroRNA expression profiles classify human cancers. Nature. 2005;435(7043):834–8.
Lloyd KA, Moore AR, Parsons BN, O'Hara A, Boyce M, Dockray GJ, et al. Gastrin-induced miR-222 promotes gastric tumor development by suppressing p27kip1. Oncotarget. 2016;7(29):45462–78.
Das S, Johnson DB. Immune-related adverse events and anti-tumor efficacy of immune checkpoint inhibitors. J Immunother Cancer. 2019;7(1):306.
Alsaab HO, Sau S, Alzhrani R, Tatiparti K, Bhise K, Kashaw SK, et al. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol. 2017;8:561.
Le DT, Durham JN, Smith KN, Wang H, Bartlett BR, Aulakh LK, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357(6349):409–13.
Sahnane N, Furlan D, Monti M, Romualdi C, Vanoli A, Vicari E, et al. Microsatellite unstable gastrointestinal neuroendocrine carcinomas: a new clinicopathologic entity. Endocr Relat Cancer. 2015;22(1):35–45.
de Mestier L, Cros J, Neuzillet C, Hentic O, Egal A, Muller N, et al. Digestive system mixed neuroendocrine-non-neuroendocrine neoplasms. Neuroendocrinology. 2017;105(4):412–25.
Frizziero M, Chakrabarty B, Nagy B, Lamarca A, Hubner RA, Valle JW, et al. Mixed neuroendocrine non-neuroendocrine neoplasms: a systematic review of a controversial and underestimated diagnosis. J Clin Med. 2020;9(1):273.
• Yamashita S, Abe H, Kunita A, Yamashita H, Seto Y, Ushiku T. Programmed cell death protein 1/programmed death ligand 1 but not HER2 is a potential therapeutic target in gastric neuroendocrine carcinoma. Histopathology. 2021;78(3):381–91 This article describes a new potential therapeutic target for gastric NECs.
Yang MW, Fu XL, Jiang YS, Chen XJ, Tao LY, Yang JY, et al. Clinical significance of programmed death 1/programmed death ligand 1 pathway in gastric neuroendocrine carcinomas. World J Gastroenterol. 2019;25(14):1684–96.
Ginestier C, Hur MH, Charafe-Jauffret E, Monville F, Dutcher J, Brown M, et al. ALDH1 is a marker of normal and malignant human mammary stem cells and a predictor of poor clinical outcome. Cell Stem Cell. 2007;1(5):555–67.
Deng S, Yang X, Lassus H, Liang S, Kaur S, Ye Q, et al. Distinct expression levels and patterns of stem cell marker, aldehyde dehydrogenase isoform 1 (ALDH1), in human epithelial cancers. PLoS One. 2010;5(4):e10277.
Vieira V, Campos LH, Jesus LH, Klabunde C, Gamba TD, Flores IL, et al. Overexpression of ALDH1 and EMT marker profile are linked with unfavorable outcome in head and neck cancer. Med Oral Patol Oral Cir Bucal. 2020;25(6):e752–e61.
Gaur P, Sceusi EL, Samuel S, Xia L, Fan F, Zhou Y, et al. Identification of cancer stem cells in human gastrointestinal carcinoid and neuroendocrine tumors. Gastroenterology. 2011;141(5):1728–37.
Li XS, Xu Q, Fu XY, Luo WS. ALDH1A1 overexpression is associated with the progression and prognosis in gastric cancer. BMC Cancer. 2014;14:705.
Ye Y, Zhang S, Chen Y, Wang X, Wang P. High ALDH1A1 expression indicates a poor prognosis in gastric neuroendocrine carcinoma. Pathol Res Pract. 2018;214(2):268–72.
Delle Fave G, O'Toole D, Sundin A, Taal B, Ferolla P, Ramage JK, et al. ENETS consensus guidelines update for gastroduodenal neuroendocrine neoplasms. Neuroendocrinology. 2016;103(2):119–24.
Vanoli A, La Rosa S, Miceli E, Klersy C, Maragliano R, Capuano F, et al. Prognostic evaluations tailored to specific gastric neuroendocrine neoplasms: analysis of 200 cases with extended follow-up. Neuroendocrinology. 2018;107(2):1–13.
Banks M, Graham D, Jansen M, Gotoda T, Coda S, di Pietro M, et al. British Society of Gastroenterology guidelines on the diagnosis and management of patients at risk of gastric adenocarcinoma. Gut. 2019;68(9):1545–75.
Pimentel-Nunes P, Libanio D, Marcos-Pinto R, Areia M, Leja M, Esposito G, et al. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy. 2019;51(4):365–88.
Chin JL, O'Connell J, Muldoon C, Swan N, Reynolds JV, Ravi N, et al. Selective resection of type 1 gastric neuroendocrine neoplasms and the risk of progression in an endoscopic surveillance programme. Dig Surg. 2021;38(1):38–45.
Daskalakis K, Tsoli M, Karapanagioti A, Chrysochoou M, Thomas D, Sougioultzis S, et al. Recurrence and metastatic potential in Type 1 gastric neuroendocrine neoplasms. Clin Endocrinol. 2019;91(4):534–43.
Hawa F, Sako Z, Nguyen T, Catanzaro AT, Zolotarevsky E, Bartley AN, et al. The band and slough technique is effective for management of diminutive type 1 gastric and duodenal neuroendocrine tumors. Endosc Int Open. 2020;8(6):E717–E21.
Sivandzadeh GR, Ejtehadi F, Shoaee S, Aminlari L, Niknam R, Taghavi AR, et al. Endoscopic mucosal resection: still a reliable therapeutic option for gastrointestinal neuroendocrine tumors. BMC Gastroenterol. 2021;21(1).
Sato Y, Takeuchi M, Hashimoto S, Mizuno K, Kobayashi M, Iwafuchi M, et al. Usefulness of endoscopic submucosal dissection for type I gastric carcinoid tumors compared with endoscopic mucosal resection. Hepato-gastroenterology. 2013;60(126):1524–9.
Chung C-S, Tsai C-L, Chu Y-Y, Chen K-C, Lin J-C, Chen B-C, et al. Clinical features and outcomes of gastric neuroendocrine tumors after endoscopic diagnosis and treatment: a Digestive Endoscopy Society of Tawian (DEST). Medicine. 2018;97(38).
Kidd M, Siddique ZL, Drozdov I, Gustafsson BI, Camp RL, Black JW, et al. The CCK(2) receptor antagonist, YF476, inhibits mastomys ECL cell hyperplasia and gastric carcinoid tumor development. Regul Pept. 2010;162(1-3):52–60.
Boyce M, Warrington S, Black J. Netazepide, a gastrin/CCK2 receptor antagonist, causes dose-dependent, persistent inhibition of the responses to pentagastrin in healthy subjects. Br J Clin Pharmacol. 2013;76(5):689–98.
Boyce M, Thomsen L. Gastric neuroendocrine tumors: prevalence in Europe, USA, and Japan, and rationale for treatment with a gastrin/CCK2 receptor antagonist. Scand J Gastroenterol. 2015;50(5):550–9.
Moore AR, Boyce M, Steele IA, Campbell F, Varro A, Pritchard DM. Netazepide, a gastrin receptor antagonist, normalises tumour biomarkers and causes regression of type 1 gastric neuroendocrine tumours in a nonrandomised trial of patients with chronic atrophic gastritis. PLoS One. 2013;8(10):e76462.
Fossmark R, Sørdal JCS, Qvigstad G, Nordrum IS, Boyce M, et al. Treatment of gastric carcinoids type 1 with the gastrin receptor antagonist netazepide (YF476) results in regression of tumours and normalisation of serum chromogranin A. Aliment Pharmacol Ther. 2012;36(11-12):1067–75.
Boyce M, Moore AR, Sagatun L, Parsons BN, Varro A, Campbell F, et al. Netazepide, a gastrin/cholecystokinin-2 receptor antagonist, can eradicate gastric neuroendocrine tumours in patients with autoimmune chronic atrophic gastritis. Br J Clin Pharmacol. 2017;83(3):466–75.
• Lloyd KA, Parsons BN, Burkitt MD, Moore AR, Papoutsopoulou S, Boyce M, et al. Netazepide inhibits expression of pappalysin 2 in type 1 gastric neuroendocrine tumors. Cell Mol Gastroenterol Hepatol. 2020;10(1):113–32 This article investigates the mechanisms by which netazepide affects the gastrin signalling pathway in Type I g-NENs.
Campana D, Ravizza D, Ferolla P, Faggiano A, Grimaldi F, Albertelli M, et al. Clinical management of patients with gastric neuroendocrine neoplasms associated with chronic atrophic gastritis: a retrospective, multicentre study. Endocrine. 2016;51(1):131–9.
Grozinsky-Glasberg S, Kaltsas G, Gur C, Gal E, Thomas D, Fichman S, et al. Long-acting somatostatin analogues are an effective treatment for type 1 gastric carcinoid tumours. Eur J Endocrinol. 2008;159(4):475–82.
• Rossi RE, Invernizzi P, Mazzaferro V, Massironi S. Response and relapse rates after treatment with long-acting somatostatin analogs in multifocal or recurrent type-1 gastric carcinoids: a systematic review and meta-analysis. United Eur Gastroenterol J. 2020;8(2):140–7 This systematic review describes the use of SSAs in type I g-NENs.
Hirschowitz BI, Griffith J, Pellegrin D, Cummings OW. Rapid regression of enterochromaffinlike cell gastric carcinoids in pernicious anemia after antrectomy. Gastroenterology. 1992;102(4 Pt 1):1409–18.
Ozao-Choy J, Buch K, Strauchen JA, Warner RR, Divino CM. Laparoscopic antrectomy for the treatment of type I gastric carcinoid tumors. J Surg Res. 2010;162(1):22–5.
• Exarchou K, Howes N, Pritchard DM. Systematic review: management of localised low-grade upper gastrointestinal neuroendocrine tumours. Aliment Pharmacol Ther. 2020;51(12):1247–67 This article descibes the advances in the management of low grade NETs.
Hyung WJ, Cheong JH, Kim J, Chen J, Choi SH, Noh SH. Application of minimally invasive treatment for early gastric cancer. J Surg Oncol. 2004;85(4):181–5 discussion 6.
Gotoda T. Endoscopic resection of early gastric cancer. Gastric Cancer. 2007;10(1):1–11.
Pape UF, Niederle B, Costa F, Gross D, Kelestimur F, Kianmanesh R, et al., (eds). ENETS consensus guidelines for neuroendocrine neoplasms of the appendix (excluding goblet cell carcinomas). Neuroendocrinology; 2016: S. Karger AG.
Ramage JK, De Herder WW, Delle Fave G, Ferolla P, Ferone D, Ito T, et al., editors. ENETS consensus guidelines update for colorectal neuroendocrine neoplasms. Neuroendocrinology; 2016: S. Karger AG.
Min B-H, Hong M, Lee JH, Rhee P-L, Sohn TS, Kim S, et al. Clinicopathological features and outcome of type 3 gastric neuroendocrine tumours. Br J Surg. 2018;105(11):1480–6.
Kwon YH, Jeon SW, Kim GH, Kim JI, Chung IK, Jee SR, et al. Long-term follow up of endoscopic resection for type 3 gastric NET. World J Gastroenterol. 2013;19(46):8703–8.
Hirasawa T, Yamamoto N, Sano T. Is endoscopic resection appropriate for type 3 gastric neuroendocrine tumors? Retrospective multicenter study. Dig Endosc. 2021;33(3):408–17.
• Exarchou K, Kamieniarz L, Tsoli M, Victor A, Oleinikov K, Khan MS, et al. Is local excision sufficient in selected grade 1 or 2 type III gastric neuroendocrine neoplasms? Endocrine. 2021;74(2):421–9 This article descibes the advances in the management of low grade type IIIg-NENs.
Sackstein PE, O'Neil DS, Neugut AI, Chabot J, Fojo T. Epidemiologic trends in neuroendocrine tumors: an examination of incidence rates and survival of specific patient subgroups over the past 20 years. Semin Oncol. 2018;45(4):249–58.
Panzuto F, Campana D, Massironi S, Faggiano A, Rinzivillo M, Lamberti G, et al. Tumour type and size are prognostic factors in gastric neuroendocrine neoplasia: a multicentre retrospective study. Dig Liver Dis. 2019;51(10):1456–60.
Song W, Tian C. The Effect of Marital Status on Survival of Patients with Gastrointestinal Stromal Tumors: A SEER Database Analysis. Gastroenterol Res Pract. 2018;2018:5740823.
Zhang Q, Wang H, Xie Y, Huang S, Chen K, Ye B, et al. Tumor size and perineural invasion predict outcome of gastric high grade neuroendocrine neoplasms. Endocr Connect. 2021;10(8):947–54.
Cao LL, Lu J, Lin JX, Zheng CH, Li P, Xie JW, et al. A novel predictive model based on preoperative blood neutrophil-to-lymphocyte ratio for survival prognosis in patients with gastric neuroendocrine neoplasms. Oncotarget. 2016;7(27):42045–58.
Tang X, Chen Y, Guo L, Zhang J, Wang C. Prognostic significance of metastatic lymph node number, ratio and station in gastric neuroendocrine carcinoma. J Gastrointest Surg. 2015;19(2):234–41.
Hu P, Bai J, Liu M, Xue J, Chen T, Li R, et al. Trends of incidence and prognosis of gastric neuroendocrine neoplasms: a study based on SEER and our multicenter research. Gastric Cancer. 2020;23(4):591–9.
Lin J, Zhao Y, Zhou Y, Tian Y, He Q, Lin J, et al. Comparison of survival and patterns of recurrence in gastric neuroendocrine carcinoma, mixed adenoneuroendocrine carcinoma, and adenocarcinoma. JAMA Netw Open. 2021;4(7):e2114180.
Boora GK, Kanwar R, Kulkarni AA, Pleticha J, Ames M, Schroth G, et al. Exome-level comparison of primary well-differentiated neuroendocrine tumors and their cell lines. Cancer Gene Ther. 2015;208(7-8):374–81.
Gahete MD, Jimenez-Vacas JM, Alors-Perez E, Herrero-Aguayo V, Fuentes-Fayos AC, Pedraza-Arevalo S, et al. Mouse models in endocrine tumors. J Endocrinol. 2018.
Dijkstra KK, van den Berg JG, Weeber F, van de Haar J, Velds A, Kaing S, et al. Patient-derived organoid models of human neuroendocrine carcinoma. Front Endocrinol (Lausanne). 2021;12:627819.
Funding
KE is supported by the Royal College of Surgeons of England Research Fellowship, with funding from the Freemasons' Royal Arch Research Fellowship with support from Sir John Fisher Foundation. DMP has received research funding from the 2019 UKINETS/Neuroendocrine Cancer UK research grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Klaire Exarchou has received speaker’s honoraria from Ipsen. Nathan A. Stephens declares that he has no conflict of interest. Andrew R. Moore has received speaker’s honoraria from Dr. Falk Pharma GmbH, and has received reimbursement for travel accommodations/expenses from Ipsen. Nathan R. Howes is supported, in part, by a research grant from the UK and Ireland Neuroendocrine Tumour Society (UKINETS)/Neuroendocrine Cancer UK. D. Mark Pritchard is supported, in part, by a research grant from UKINETS/Neuroendocrine Cancer UK, and has received research funding to investigate the role of netazepide in gastric NETs from Trio Medicines Ltd.; has served as a consultant for Ipsen, Advanced Accelerator Applications, and Laboratoires Mayoly-Spindler, with all compensation going directly to his institution; has served as a guest lecturer/speaker/presenter for Ipsen, Advanced Accelerator Applications, and Laboratoires Mayoly-Spindler, with all compensation going directly to his institution; has received reimbursement for travel accommodations/expenses from Ipsen; has participated on a Data Safety Monitoring Board or Advisory Board for Ipsen and Advanced Accelerator Applications, with all compensation going directly to his institution; and was a member of the British Society of Gastroenterology Council from 2018 to 2020.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neuroendocrine Neoplasms
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Exarchou, K., Stephens, N.A., Moore, A.R. et al. New Developments in Gastric Neuroendocrine Neoplasms. Curr Oncol Rep 24, 77–88 (2022). https://doi.org/10.1007/s11912-021-01175-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-021-01175-y