Summary
In the last decade, a number of genetic alterations in gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) have been identified. In addition, differences in tumor morphology as well as proliferation index (Ki-67) or number of mitoses have led to changes in the classification of these neoplasms. According to the new World Health Organization (WHO) classification, GEP-NENs are now divided into two genetically and prognostically different categories: (i) well-differentiated neuroendocrine tumors (NET) subdivided into low (G1), intermediate (2) and high (G3) grade tumors, and (ii) poorly differentiated neuroendocrine carcinomas (NEC). In addition, a group of mixed neuroendocrine–non-neuroendocrine neoplasms (MiNEN) has been defined. This review focuses on the clinical, morphological, immunohistochemical and molecular findings of the GEP-NENs and their key diagnostic features that can help the pathologist to differentiate between tumors in this heterogeneous group. In challenging cases, additional immunohistochemical and/or molecular analysis can be helpful to determine the correct diagnosis and proper treatment for the patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) are a rare group of tumors with heterogenous morphological and molecular findings. In recent years, the spectrum of genetic alterations in GEP-NENs has been characterized in more detail, leading to changes in the new World Health Organization (WHO) classification [1]: Based on clinical, histological and molecular findings, these tumors are now divided into two genetically distinct categories with different malignant potential and prognosis, namely well-differentiated neuroendocrine tumors (NET) and poorly differentiated neuroendocrine carcinomas (NEC) [2, 3].
The former group can further be subdivided into low (G1), intermediate (G2), or high (G3) grade NET composed of low to moderately atypical cells in an organoid arrangement with expression of immunohistochemical markers of neuroendocrine differentiation (synaptophysin and chromogranin A; Fig. 1). The grade is determined using the proliferation rate (measured with Ki-67) and/or mitotic number (Table 1). G3 NETs are a new subgroup of well-differentiated NETs defined by a proliferation index of > 20% or a mitotic rate of > 20 per 2 mm2 [1]. In the 2010 WHO classification, these tumors were considered to be NECs (Table 2); however, it has been shown that they have a better prognosis and different molecular alterations than NECs [4, 5]. The prognosis and potential to metastasize depend on the location of the primary tumor, histological type and differentiation (grade).
Histological and immunohistochemical findings. a Well-differentiated neuroendocrine tumor, G1 composed of nest-like and glandular formation of uniform bland tumor cells with fine granular chromatin, abundant cytoplasm and round to oval, monomorphic nuclei with a Ki-67 < 3% (Inset). b Immunohistochemically, tumor expresses chromogranin A and c synaptophysin. d Large cell neuroendocrine carcinoma consisting of intermediate to large, highly atypical cells with abundant cytoplasm and prominent nucleoli with diffuse growth pattern and Ki-67 of 80% (Inset). e Small cell neuroendocrine carcinoma comprised of tumor cells with scarce cytoplasm arranged in solid structures with a Ki-67 of 90% (Inset) and f expression of synaptophysin
Hormone production of NETs may be clinically silent (non-functional (NF)-NET) in > 60% of all pancreatic NENs [6] or associated with hormonal hyperfunction syndrome. In contrast to NF-NETs, functional NETs are referred to as insulinomas, VIPomas, glucagonomas, somatostatinomas, etc., according to the hormone that causes hyperfunction [1].
The second group of the new classification comprises NECs, poorly differentiated NENs composed of highly atypical, small or medium-to-large cells, which can be further divided into two different subtypes with distinct cell size and architecture, namely large-cell (LCNEC) and small-cell (SCNEC) NECs. Proliferation rate (measured by Ki-67) is always high (usually above 55%) with an increased number of mitoses (> 20/2 mm2) [1]. NECs make up only 6–8% of GEP-NENs, while 84% are G1 or G2 NETs and up to 8% are G3 NETs [2, 7].
Tumors consisting of at least one neuroendocrine and one non-neuroendocrine component (typically an adenocarcinoma) with each component making up > 30% of the tumor are classified as “mixed neuroendocrine–non-neuroendocrine neoplasms” (MiNEN) in the new classification [1].
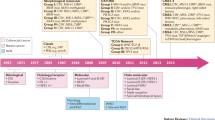
This review aims to provide a comprehensive overview on histology, immunohistochemistry and molecular attributes of NEC, NET and MiNEN of the gastrointestinal (GI) tract and the pancreas. Clinical, histological, immunohistochemical and genetic findings of pancreatic NETs (PanNETs) and NECs (PanNECs) are also summarized in Fig. 2.
Histological, immunohistochemical, genetic and prognostic characteristics of PanNETs and PanNECs (IHC immunohistochemistry, OS overall survival, PanNET pancreatic neuroendocrine tumor, PanNEC pancreatic neuroendocrine carcinoma, Syn Synaptophysin, Chr A Chromogranin A, INSM1 Insulinoma-associated protein 1, SSTR2A Somatostatin receptor 2A)
The TNM classification of well-differentiated NETs is described in the eighth edition (2017) of the Union for International Cancer Control (UICC) TNM Classification and the American Joint Committee on Cancer (AJCC), which conform to the European Neuroendocrine Tumor Society (ENETS) classification. The TNM classification of pancreatic and gastrointestinal NECs follows the scheme of the UICC TNM classification for carcinomas of the exocrine pancreas/the digestive system [8].
Neuroendocrine tumors (NET) G1–G3
Histology
Gastroenteropancreatic NETs consist of uniform bland tumor cells with fine granular chromatin (also called salt and pepper chromatin), abundant cytoplasm and round to oval, monomorphic nuclei. The tumors show an organoid architecture, with nest-like, glandular, trabecular, acinar and other growth patterns. Necroses are absent and mitoses are scarce in most NETs, with exception of G3 NETs where per definition, more than 20 mitoses per 2 mm2 are found. In these high-grade tumors, which are very rare compared to G1 and G2 NETs in the GI tract, Ki-67 is usually below 55% [1, 9]. The determination of the tumor grade by the number of mitoses or Ki-67 proliferation index is elucidated further in Table 1.
Concerning differential diagnosis of G3 NETs, a multicenter study assessing approximately 200 cases of high-grade NENs found that the most useful morphological criteria for setting apart G3 NETs from NECs comprise organoid growth pattern, close association of vessels to tumor cells and absence of desmoplasia [10].
Immunohistochemistry
NETs stain positive for neuroendocrine markers such as synaptophysin and chromogranin A. In L‑cell NETs (e.g. in the appendix), chromogranin B is expressed more commonly than chromogranin A. Functional NETs can also be stained with antibodies for the hormones they produce. In addition, NETs often show a strong expression of somatostatin receptor 2A (SSTR2A), which may be used to indicate eligibility for treatment with somatostatin-analogue therapy [1]. Furthermore, SSTR2A staining can help to discriminate NETs with a high proliferation rate (G3) from NECs, which are only SSTR2A positive in some cases [11]. In addition, loss of ATRX and DAXX nuclear staining is found in a subset of NETs, and this finding can be helpful in challenging cases. p53 and Rb1 stains show normal expression [11, 12].
Insulinoma-associated protein 1 (INSM1) has also been proposed as a very sensitive and specific immunohistochemistry marker for GEP-NENs and has been recommended for diagnostic use by several authors [13,14,15,16,17].
Molecular pathology
In gastrointestinal NETs, epigenetic dysregulation is very common with most NETs showing CpG island methylator phenotype, while somatic mutations appear to be secondary; to date, there is no specific gene mutation that has been described in a substantial amount of cases [1]. The most common alteration is CDNK1B mutation, which is present in 8% of small intestine NETs [18]. Copy number variations in chromosomes are frequent. For example, in the small intestine, most NETs display chromosome 18 deletion even at early stages [19, 20], while chromosome 14 gain can be found in advanced stages and may therefore pose a negative prognostic factor [21].
In the pancreas, 40% of NETs display somatic inactivation of MEN1. Another 40% have inactivating mutations in DAXX or ATRX, which have been described as negative prognostic factors [22,23,24]. Activating mutations of genes involved in the mTOR pathway, including PTEN and TSC2, are present in about 15% of tumors [25]. Associations of PanNETs with hereditary cancer syndromes (i.e. multiple endocrine neoplasia type 1, neurofibromatosis type 1) and in some cases germline mutations in DNA repair genes (MUTYH, CHEK2 and BRCA2) have also been reported [1, 26, 27].
From an evolutionary perspective, it is believed that NETs and NECs are distinct entities; yet a cluster analysis of GEP-NENs has shown that some LCNECs might potentially develop from pre-existing NETs, in particular those where the CTNNB1 gene is dominantly affected by mutation. The same authors have also previously hypothesized two pathways of NET to NEC evolution in the lung. These concepts remain to be investigated further [28, 29]. Within the NET category however, progression of low-grade tumors to high-grade NETs is possible and G3 NETs can often be found as liver metastases of pulmonary or pancreatic NETs [30, 31].
Neuroendocrine carcinomas (NEC)
Histology
Neuroendocrine carcinomas can be divided into two different subtypes based on morphology. Large cell NEC (LCNEC) consists of highly atypical cells of intermediate to large size with abundant cytoplasm and often prominent nucleoli arranged in an organoid pattern (mostly large nests or trabeculae) or grow diffusely, while the tumor cells in small cell NEC (SCNEC) have scarce cytoplasm and typically form solid structures. In both subtypes, necrosis and a high number of mitoses, including atypical mitoses, are present. The mitotic rate must exceed 20 per 2 mm2 and/or the Ki-67 proliferation index must be above 20% [1]. In the pancreas, different clinicopathological attributes of LCNEC and SCNEC have not been observed [32].
In diagnostic routine, it is important to differentiate PanNEC, as well as PanNET G3, from acinar cell carcinoma of the pancreas, which often has a similar histological appearance and focally stains positive for neuroendocrine markers [32]. These entities can be distinguished using neuroendocrine and acinar stains, including trypsin and BCL-10 [7, 31, 33].
Immunohistochemistry
In general, NECs show diffuse to weak expression of neuroendocrine markers such as synaptophysin and chromogranin A. Neuron-specific enolase (NSE), CD56, CDX2 and TTF1 may also be expressed by these tumors; however, these markers are not specific for NECs. Hormone production is rarely found [1].
In addition, SSTR2A may be positive in some NECs, but not as frequent as in NETs. Abnormal p53 immunostaining, which is a strong indicator for TP53 mutation, and lack of Rb1 expression are commonly observed in NECs (in contrast to NETs) which makes p53 and Rb1 stains useful for the differential diagnosis of NET G3 and NEC [11, 12]. ATRX and DAXX stains, which are positive as these genes are not affected by mutations in NECs, may also serve this purpose, although they are not as discriminative as p53 and Rb1, since ATRX and DAXX expression is also preserved in the majority of NETs [11].
According to the 2016 ENETS Consensus Guideline, pathology reports on NEC should always include the morphological subtype (LCNEC or SCNEC), Ki-67 index or mitotic rate and staining for synaptophysin and chromogranin A; staining for SSTR2A is optional, but may be useful [34].
Molecular pathology
LCNEC and SCNEC are not genetically distinct. Typical genetic alterations are mutations in TP53, which leads to the loss of p53 immunohistochemical expression, mutations in RB1 or loss of p16 expression [12].
Several studies have also described genetic similarities between gastrointestinal neuroendocrine carcinomas and colorectal adenocarcinomas [35,36,37,38], since mutations in APC, KRAS and BRAF have been found in NECs. BRAF mutations appear even more frequently in NECs than in conventional adenocarcinomas and have been associated with an unfavorable prognosis [39].
In PanNECs, KRAS mutations as well as SMAD4 mutations (which are typical for ductal adenocarcinoma of the pancreas) have been reported but do not occur regularly [40]. BCL‑2 overexpression is frequent and associated with a high proliferation rate [12]. Inactivation of ATRX and DAXX, which may be present in PanNETs, does not occur in PanNECs [11, 12].
Mixed neuroendocrine–non-neuroendocrine neoplasms (MiNEN)
Tumors consisting of at least two components, including a neuroendocrine and a non-neuroendocrine component, were previously referred to as “mixed adenoneuroendocrine carcinoma” (MANEC; Table 2). Since the non-neuroendocrine component can also present as a different cancer type (not only adenocarcinoma), “MANEC” was replaced by the term “mixed neuroendocrine–non-neuroendocrine neoplasm” (MiNEN) in the 2017 WHO classification of pancreatic neuroendocrine tumors and the 2019 WHO classification of gastrointestinal tumors. In GI pathology, the term “MANEC” was also formerly used to refer to goblet cell adenocarcinomas (also known as goblet cell carcinoids) of the appendix, which in the recent WHO classification are no longer considered to be neuroendocrine neoplasms [1].
MiNEN components are mostly poorly differentiated, with the non-neuroendocrine tumor component typically being an adenocarcinoma in the GI tract and either a ductal adenocarcinoma and/or an acinar cell carcinoma in the pancreas. Each component should comprise at least 30% of the tumor and grade should be reported separately for both tumor components. The staging of MiNEN is based on the current scheme of the UICC TNM classification of carcinomas of the exocrine pancreas [1]. In the differential diagnosis of MiNEN, acinar cell carcinoma of the pancreas must be distinguished, using a panel of acinar and neuroendocrine immunohistochemical markers (as mentioned in the differential diagnosis of NEC and acinar cell carcinoma) [7, 33].
The molecular features of MiNEN (at least of those with adenocarcinoma components) appear to be more closely related to those of non-neuroendocrine adenocarcinomas than to those of NECs, as BRAF, KRAS and APC mutations are common while RB1 mutations are sparse and TP53 mutations occur in lower frequency compared to NECs [35]. Recent publications have also described microsatellite instability and ATRX mutations in MiNEN [41,42,43]. However, the genetic landscape of MiNEN is heterogenous and complex and remains to be elucidated. Biopsies of these heterogeneous tumors might not include both components, posing an additional difficulty to both diagnostics and analysis of genetic alterations for research [44].
Prognosis
The prognosis of neuroendocrine neoplasms depends on various factors, including primary tumor location, histological type, tumor grade, tumor stage at initial diagnosis (tumor size and metastases), and the presence of vascular invasion. NET G1 and G2 show slow growth with good prognosis. Patients with NET G3 have a better prognosis compared to those with NEC but overall survival is worse than for NET G1 and G2 [2, 7, 45, 46].
Within NEC, two prognostically distinct groups can be defined by using a Ki-67 cut-off of 55%. NECs > 55% are associated with an increased rate of mutations in TP53, KRAS and BRAF and poor overall survival [47,48,49]. There is no significant difference in the survival of patients with LCNEC compared to SCNEC [32].
MiNEN typically behave in an aggressive way and have an unfavorable prognosis compared to well-differentiated NETs. It is unclear whether the prognosis is better or worse than that of NECs [44]. The crucial prognostic factors for GEP-MiNEN are TNM stage and tumor composition, especially the proliferation rate of the neuroendocrine component [49, 50].
Conclusion
GEP-NENs are a rare, heterogeneous group of tumors that, in difficult cases, represent a diagnostic challenge for pathologists. The subdivision of NENs into distinct groups is crucial for the treatment of these tumors. However, intratumoral heterogeneity limits the accuracy of the grading system in the biopsy material. The multidisciplinary care of patients with GEP-NENs by an experienced team and presentation in a multidisciplinary tumor board is crucial for optimized individual and successful therapy.
Take-home message
The subdivision of gastroenteropancreatic neuroendocrine neoplasms (NENs) into distinct groups, namely well-differentiated neuroendocrine tumors (NET) G1–G3 and poorly differentiated neuroendocrine carcinomas (NEC), is crucial for the treatment of these tumors. They can be differentiated by morphology, immunohistochemical expression and molecular alterations.
References
WHO Classification of Tumours: Digestive system tumours. 5th ed. ition ed: IARC Press; 2019.
Basturk O, Yang Z, Tang LH, Hruban RH, Adsay V, McCall CM, et al The high-grade (WHO G3) pancreatic neuroendocrine tumor category is morphologically and biologically heterogenous and includes both well differentiated and poorly differentiated neoplasms. Am J Surg Pathol. 2015;39(5):683–90.
McCall CM, Shi C, Cornish TC, Klimstra DS, Tang LH, Basturk O, et al Grading of well-differentiated pancreatic neuroendocrine tumors is improved by the inclusion of both Ki67 proliferative index and mitotic rate. Am J Surg Pathol. 2013;37(11):1671–7.
Rindi G, Klimstra DS, Abedi-Ardekani B, Asa SL, Bosman FT, Brambilla E, et al A common classification framework for neuroendocrine neoplasms: an International Agency for Research on Cancer (IARC) and World Health Organization (WHO) expert consensus proposal. Mod Pathol. 2018;31(12):1770–86.
Fazio N, Milione M. Heterogeneity of grade 3 gastroenteropancreatic neuroendocrine carcinomas: New insights and treatment implications. Cancer Treat Rev. 2016;50:61–7.
Falconi M, Eriksson B, Kaltsas G, Bartsch DK, Capdevila J, Caplin M, et al ENETS Consensus Guidelines Update for the Management of Patients with Functional Pancreatic Neuroendocrine Tumors and Non-Functional Pancreatic Neuroendocrine Tumors. Neuroendocrinology. 2016;103(2):153–71.
Coriat R, Walter T, Terris B, Couvelard A, Ruszniewski P. Gastroenteropancreatic Well-Differentiated Grade 3 Neuroendocrine Tumors: Review and Position Statement. Oncologist. 2016;21(10):1191–9.
TNM Classification of Malignant Tumours. 8th ed. ed: Wiley; 2017.
Heetfeld M, Chougnet CN, Olsen IH, Rinke A, Borbath I, Crespo G, et al Characteristics and treatment of patients with G3 gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer. 2015;22(4):657–64.
Elvebakken H, Perren A, Scoazec JY, Tang LH, Federspiel B, Klimstra DS, et al A Consensus-Developed Morphological Re-Evaluation of 196 High-Grade Gastroenteropancreatic Neuroendocrine Neoplasms and Its Clinical Correlations. Neuroendocrinology. 2021;111(9):883–94.
Konukiewitz B, Schlitter AM, Jesinghaus M, Pfister D, Steiger K, Segler A, et al Somatostatin receptor expression related to TP53 and RB1 alterations in pancreatic and extrapancreatic neuroendocrine neoplasms with a Ki67-index above 20. Mod Pathol. 2017;30(4):587–98.
Yachida S, Vakiani E, White CM, Zhong Y, Saunders T, Morgan R, et al Small cell and large cell neuroendocrine carcinomas of the pancreas are genetically similar and distinct from well-differentiated pancreatic neuroendocrine tumors. Am J Surg Pathol. 2012;36(2):173–84.
Zhang Q, Huang J, He Y, Cao R, Shu J. Insulinoma-associated protein 1(INSM1) is a superior marker for the diagnosis of gastroenteropancreatic neuroendoerine neoplasms: a meta-analysis. Endocrine. 2021;74(1):61–71.
Gonzalez I, Lu HC, Sninsky J, Yang C, Bishnupuri K, Dieckgraefe B, et al Insulinoma-associated protein 1 expression in primary and metastatic neuroendocrine neoplasms of the gastrointestinal and pancreaticobiliary tracts. Histopathology. 2019;75(4):568–77.
McHugh KE, Mukhopadhyay S, Doxtader EE, Lanigan C, Allende DS. INSM1 Is a Highly Specific Marker of Neuroendocrine Differentiation in Primary Neoplasms of the Gastrointestinal Tract, Appendix, and Pancreas. Am J Clin Pathol. 2020;153(6):811–20.
Aldera AP, Govender D, Locketz ML, Mukhopadhyay S, McHugh K, Allende D. Combined Use of INSM1 and Synaptophysin Is the Most Sensitive and Specific Panel to Detect Neuroendocrine Neoplasms in the Digestive Tract. Am J Clin Pathol. 2020;154(6):870–1.
Tanigawa M, Nakayama M, Taira T, Hattori S, Mihara Y, Kondo R, et al Insulinoma-associated protein 1 (INSM1) is a useful marker for pancreatic neuroendocrine tumor. Med Mol Morphol. 2018;51(1):32–40.
Francis JM, Kiezun A, Ramos AH, Serra S, Pedamallu CS, Qian ZR, et al Somatic mutation of CDKN1B in small intestine neuroendocrine tumors. Nat Genet. 2013;45(12):1483–6.
Wang GG, Yao JC, Worah S, White JA, Luna R, Wu TT, et al Comparison of genetic alterations in neuroendocrine tumors: frequent loss of chromosome 18 in ileal carcinoid tumors. Mod Pathol. 2005;18(8):1079–87.
Kytola S, Hoog A, Nord B, Cedermark B, Frisk T, Larsson C, et al Comparative genomic hybridization identifies loss of 18q22-qter as an early and specific event in tumorigenesis of midgut carcinoids. Am J Pathol. 2001;158(5):1803–8.
Andersson E, Sward C, Stenman G, Ahlman H, Nilsson O. High-resolution genomic profiling reveals gain of chromosome 14 as a predictor of poor outcome in ileal carcinoids. Endocr Relat Cancer. 2009;16(3):953–66.
Park JK, Paik WH, Lee K, Ryu JK, Lee SH, Kim YT. DAXX/ATRX and MEN1 genes are strong prognostic markers in pancreatic neuroendocrine tumors. Oncotarget. 2017;8(30):49796–806.
Kim JY, Brosnan-Cashman JA, An S, Kim SJ, Song KB, Kim MS, et al Alternative Lengthening of Telomeres in Primary Pancreatic Neuroendocrine Tumors Is Associated with Aggressive Clinical Behavior and Poor Survival. Clin Cancer Res. 2017;23(6):1598–606.
Singhi AD, Liu TC, Roncaioli JL, Cao D, Zeh HJ, Zureikat AH, et al Alternative Lengthening of Telomeres and Loss of DAXX/ATRX Expression Predicts Metastatic Disease and Poor Survival in Patients with Pancreatic Neuroendocrine Tumors. Clin Cancer Res. 2017;23(2):600–9.
Jiao Y, Shi C, Edil BH, de Wilde RF, Klimstra DS, Maitra A. et al DAXX/ATRX, MEN1, and mTOR pathway genes are frequently altered in pancreatic neuroendocrine tumors. Science. 2011;331(6021):1199–203.
Noe M, Pea A, Luchini C, Felsenstein M, Barbi S, Bhaijee F, et al Whole-exome sequencing of duodenal neuroendocrine tumors in patients with neurofibromatosis type 1. Mod Pathol. 2018;31(10):1532–8.
Scarpa A, Chang DK, Nones K, Corbo V, Patch AM, Bailey P. et al Whole-genome landscape of pancreatic neuroendocrine tumours. Nature. 2017;543(7643):65–71.
Pelosi G, Bianchi F, Dama E, Metovic J, Barella M, Sonzogni A, et al A Subset of Large Cell Neuroendocrine Carcinomas in the Gastroenteropancreatic Tract May Evolve from Pre-existing Well-Differentiated Neuroendocrine Tumors. Endocr Pathol. 2021;32(3):396–407.
Pelosi G, Bianchi F, Dama E, Simbolo M, Mafficini A, Sonzogni A, et al Most high-grade neuroendocrine tumours of the lung are likely to secondarily develop from pre-existing carcinoids: innovative findings skipping the current pathogenesis paradigm. Virchows Arch. 2018;472(4):567–77.
Kasajima A, Konukiewitz B, Schlitter AM, Weichert W, Kloppel G. An analysis of 130 neuroendocrine tumors G3 regarding prevalence, origin, metastasis, and diagnostic features. Virchows Arch. 2022;480(2):359–68.
Kloppel G, Neoplasms N. Dichotomy, Origin and Classifications. Visc Med. 2017;33(5):324–30.
Basturk O, Tang L, Hruban RH, Adsay V, Yang Z, Krasinskas AM, et al Poorly differentiated neuroendocrine carcinomas of the pancreas: a clinicopathologic analysis of 44 cases. Am J Surg Pathol. 2014;38(4):437–47.
Konukiewitz B, Jesinghaus M, Kasajima A, Kloppel G. Neuroendocrine neoplasms of the pancreas: diagnosis and pitfalls. Virchows Arch. 2022;480(2):247–57.
Garcia-Carbonero R, Sorbye H, Baudin E, Raymond E, Wiedenmann B, Niederle B, et al ENETS Consensus Guidelines for High-Grade Gastroenteropancreatic Neuroendocrine Tumors and Neuroendocrine Carcinomas. Neuroendocrinology. 2016;103(2):186–94.
Jesinghaus M, Konukiewitz B, Keller G, Kloor M, Steiger K, Reiche M, et al Colorectal mixed adenoneuroendocrine carcinomas and neuroendocrine carcinomas are genetically closely related to colorectal adenocarcinomas. Mod Pathol. 2017;30(4):610–9.
Takizawa N, Ohishi Y, Hirahashi M, Takahashi S, Nakamura K, Tanaka M, et al Molecular characteristics of colorectal neuroendocrine carcinoma; similarities with adenocarcinoma rather than neuroendocrine tumor. Hum Pathol. 2015;46(12):1890–900.
Karkouche R, Bachet JB, Sandrini J, Mitry E, Penna C, Cote JF, et al Colorectal neuroendocrine carcinomas and adenocarcinomas share oncogenic pathways. A clinico-pathologic study of 12 cases. Eur J Gastroenterol Hepatol. 2012;24(12):1430–7.
Woischke C, Schaaf CW, Yang HM, Vieth M, Veits L, Geddert H, et al In-depth mutational analyses of colorectal neuroendocrine carcinomas with adenoma or adenocarcinoma components. Mod Pathol. 2017;30(1):95–103.
Olevian DC, Nikiforova MN, Chiosea S, Sun W, Bahary N, Kuan SF. et al Colorectal poorly differentiated neuroendocrine carcinomas frequently exhibit BRAF mutations and are associated with poor overall survival. Hum Pathol. 2016;49:124–34.
Kimura T, Miyamoto H, Fukuya A, Kitamura S, Okamoto K, Kimura M, et al Neuroendocrine carcinoma of the pancreas with similar genetic alterations to invasive ductal adenocarcinoma. Clin J Gastroenterol. 2016;9(4):261–5.
Lou L, Lv F, Wu X, Li Y, Zhang X. Clinical implications of mismatch repair deficiency screening in patients with mixed neuroendocrine non-neuroendocrine neoplasms (MiNEN). Eur J Surg Oncol. 2021;47(2):323–30.
Yeo MK, Yoon N, Bae GE. Clinicopathologic and Molecular Characteristics of Gastrointestinal MiNENs. Front Oncol. 2021;11:709097.
Sciammarella C, Bencivenga M, Mafficini A, Piredda ML, Tsvetkova V, Paolino G, et al Molecular Analysis of an Intestinal Neuroendocrine/Non-neuroendocrine Neoplasm (MiNEN) Reveals MLH1 Methylation-driven Microsatellite Instability and a Monoclonal Origin: Diagnostic and Clinical Implications. Appl Immunohistochem Mol Morphol. 2022;30(2):145–52.
Frizziero M, Chakrabarty B, Nagy B, Lamarca A, Hubner RA, Valle JW. et al Mixed Neuroendocrine Non-Neuroendocrine Neoplasms: A Systematic Review of a Controversial and Underestimated Diagnosis. J Clin Med. 2020;9:1.
Velayoudom-Cephise FL, Duvillard P, Foucan L, Hadoux J, Chougnet CN, Leboulleux S, et al Are G3 ENETS neuroendocrine neoplasms heterogeneous? Endocr Relat Cancer. 2013;20(5):649–57.
Tang LH, Untch BR, Reidy DL, O’Reilly E, Dhall D, Jih L, et al Well-Differentiated Neuroendocrine Tumors with a Morphologically Apparent High-Grade Component: A Pathway Distinct from Poorly Differentiated Neuroendocrine Carcinomas. Clin Cancer Res. 2016;22(4):1011–7.
Busico A, Maisonneuve P, Prinzi N, Pusceddu S, Centonze G, Garzone G, et al Gastroenteropancreatic High-Grade Neuroendocrine Neoplasms: Histology and Molecular Analysis, Two Sides of the Same Coin. Neuroendocrinology. 2020;110(7–8):616–29.
Milione M, Maisonneuve P, Spada F, Pellegrinelli A, Spaggiari P, Albarello L, et al The Clinicopathologic Heterogeneity of Grade 3 Gastroenteropancreatic Neuroendocrine Neoplasms: Morphological Differentiation and Proliferation Identify Different Prognostic Categories. Neuroendocrinology. 2017;104(1):85–93.
Milione M, Maisonneuve P, Pellegrinelli A, Grillo F, Albarello L, Spaggiari P, et al Ki67 proliferative index of the neuroendocrine component drives MANEC prognosis. Endocr Relat Cancer. 2018;25(5):583–93.
Huang YC, Yang NN, Chen HC, Huang YL, Yan WT, Yang RX, et al Clinicopathological features and prognostic factors associated with gastroenteropancreatic mixed neuroendocrine non-neuroendocrine neoplasms in Chinese patients. World J Gastroenterol. 2021;27(7):624–40.
Funding
Open access funding provided by Medical University of Graz.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H. Henzinger and I. Brcic declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Henzinger, H., Brcic, I. From morphology to molecular targets—the pathologist’s view in diagnosing gastroenteropancreatic neuroendocrine neoplasms. memo 15, 287–293 (2022). https://doi.org/10.1007/s12254-022-00850-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12254-022-00850-5