Abstract
Intravenous immunoglobulin (IVIG) has been suggested for the treatment of many ailments due to its ability to modulate the immune system and to provide passive immunity to commonly circulating pathogens. Its use as primary and adjunctive therapy for the treatment of conditions affecting critically ill patients is an attractive option, especially when alternative therapy does not exist. The body of literature on the use of IVIG for the treatment of several serious conditions, including sepsis, toxic shock syndrome, acute myocarditis, Stevens-Johnson syndrome, toxic epidermal necrolysis, and H1N1 influenza, were reviewed. Despite advances in treatment of these conditions since they were first described, there remains a paucity of well-designed studies on the use of IVIG for their treatment. Therefore, the use of IVIG for treatment of these conditions remains controversial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intravenous immunoglobulin consists of highly concentrated immunoglobulins that are derived from the pooled plasma of many healthy human donors. Intravenous immunoglobulin preparations contain not only mostly IgG but also traces of IgA and IgM. The Food and Drug Administration (FDA) requires that intravenous immunoglobulin (IVIG) contain at least a specified concentration of immunoglobulins to measles virus, Corynebacterium diphtheriae, poliovirus, and hepatitis B virus [1]. However, the concentration of immunoglobulins to other pathogens can be highly variable. Intravenous immunoglobulin has been used for many years for the treatment of humoral immunodeficiencies. Owing to its anti-inflammatory properties and immunomodulatory effects, IVIG has been used for various other conditions. Intravenous immunoglobulin derives its potent anti-inflammatory effects via several mechanisms. Intravenous immunoglobulin decreases proliferation of T cells and T cell subsets [2–5]. The production of pro-inflammatory cytokines TNF-alpha, IL-1, and IL-2 are reduced by IVIG [6–8]. Intravenous immunoglobulin is also thought to exert effects via competitive binding to Fc receptors on macrophages, thereby deactivating phagocytosis [9, 10]. The data supporting the use of IVIG in life-threatening conditions are varied with some supported by strong evidence, while others are merely anecdotal. This manuscript will review and summarize the supporting data for the use of IVIG in critically ill patients.
The mechanism of action of IVIG has not been clearly defined. Several proposed mechanisms have been suggested, with most evidence being limited to in vitro and animal studies. Anti-inflammatory effects of IVIG may arise from the presence of antibodies against pro-inflammatory cytokines (TNF-α, IL-1α, and IL-6) [11, 12]. Administration of IVIG also leads to increases in anti-inflammatory cytokines and potentially to downregulation of adhesion molecule, chemokine, and chemokine-receptor expression [13]. In individuals being treated for autoimmune and inflammatory conditions, excessive pro-inflammatory cytokines can lead to a state of decreased responsiveness to glucocorticoids [14]. Intravenous immunoglobulin has been shown to improve clinical responses and T cell affinity in glucocorticoid-resistant asthma, possibly via suppression of pro-inflammatory cytokine production [15, 16]. Immunomodulatory effects may be derived from interactions with IgG antigen-binding fragment (Fab) or Fc. The Fab portion of antibodies contained in IVIG binds to inflammatory proteins and receptors, such as cytokines, cytokine receptors, Fas, and CD5 [17, 18•]. An additional proposed mechanism of action is binding of IgG to complement fragments thereby blocking deposition on target tissues [19]. Neonatal Fc receptor (FcRn) prevents degradation of autoantibodies. Theoretically, IgG-saturated FcRn should result in increased autoantibody degradation. However, no studies have ever substantiated this theory. Intravenous immunoglobulin may upregulate expression of an inhibitory receptor, FcγRIIB, on macrophages and reduce pro-inflammatory response [20]. Additional evidence suggests that there may be a receptor on regulatory macrophages that recognizes sialylated Fc fragments of IgG contained in IVIG and promotes anti-inflammatory effects [18•].
Sepsis
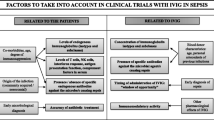
Sepsis and septic shock are clinical syndromes characterized by a severe systemic inflammatory response to infection. The incidence of sepsis continues to increase. From 1997 to 2000, the incidence of sepsis increased from 82.7 to 240.4 per 100,000 population [21]. Fortunately, the mortality rate related to sepsis decreased during the same time period from 27.8 to 17.9 % [21]. The decreased sepsis mortality rate is likely related to advances in early recognition and attempts at early reversal of the condition. Despite decreasing mortality in sepsis, the disease burden and mortality rate remain unacceptably high. The backbone of sepsis therapy includes maintenance of appropriate hemodynamic status and prompt administration of antibiotics. Additional adjunctive therapies have been suggested for the treatment of sepsis, including IVIG. Intravenous immunoglobulin has been proposed for treatment of sepsis due to its ability to modulate inflammation and its ability to bind to endotoxin.
To date, trials have demonstrated conflicting results regarding the efficacy of IVIG in the treatment of sepsis. No conclusive evidence exists for the routine use of IVIG in the treatment of adult or pediatric sepsis. A randomized trial of 653 patients from 23 centers concluded that the use of IVIG for the treatment of sepsis did not decrease mortality rate or improve pulmonary function when compared to that of placebo. The 28-day mortality rate was 37.3 % in the placebo group versus 39.3 % in the IVIG group (p = 0.67) [22]. Several meta-analyses, on the other hand, have demonstrated a reduction in 28-day mortality rate with the use of IVIG when compared to either placebo or no IVIG. However, all of these meta-analyses were limited by study heterogeneity. When the meta-analyses focused on only well-designed studies with low risk of bias, the mortality rate reduction disappeared [23–25]. One meta-analysis showed an overall reduction in mortality rate with the use of IVIG versus placebo (RR = 0.79, 95 % CI 0.69, 0.9). This same study revealed a greater benefit of IgA- and IgM-enriched IVIG versus immunoglobulin preparation containing only IgG (RR = 0.66, 95 % CI 0.51, 0.84) [26]. No large randomized controlled trials have compared IgA- and IgM-enriched IVIG versus placebo for the treatment of sepsis.
Likewise, data in children are conflicting. A randomized controlled trial of 100 children in Egypt with sepsis resulted in a decreased mortality rate and length of hospital stay in the group treated with IVIG [27]. In a meta-analysis, 640 neonates with suspected or proven sepsis reported a reduction in mortality rate with the use of IVIG versus no treatment or placebo. In this study, there was reduced mortality in both infants with suspected sepsis (RR = 0.58, 95 % CI 0.38, 0.89) and in infants with proven sepsis (RR = 0.55, 95 % CI 0.38, 0.98) [28]. This conclusion was encouraging for the potential utility of IVIG and provoked further investigation. Subsequently, a large and robust randomized controlled trial conducted by the International Neonatal Immunotherapy study (INIS) group of 3493 neonates being treated for suspected or proven sepsis found no benefit in the rates of mortality or major disability at 2 years of age with the use of IVIG versus placebo (RR = 1.00, 95 % CI 0.92, 1.08) [29•].
Data on the use of IVIG for the treatment of adult and pediatric sepsis is not conclusive, yet most well-designed studies reveal no benefit. One adult meta-analysis demonstrated possible benefit with the use of IgA- and IgM-enriched IVIG. Large randomized controlled trials are needed to define the clinical utility of IVIG in sepsis treatment. Neonates are the only age group that have undergone a large randomized controlled trial; this demonstrated that there is no benefit for the use of IVIG in the treatment of sepsis in this age group. In this study, confounding was controlled for by randomizing neonates into treatment and placebo groups based on characteristics. In addition, the patients received a standard weight-based dose of IVIG. The main eligibility criterion for treatment was for infants to be receiving antibiotics for suspected or proven serious infection. The subjectivity of this inclusion criterion should be noted as a potential limitation of this study. Additionally, patients were not randomized according to the causative organism. Therefore, further studies analyzing the benefit of IVIG for the treatment of specific pathogens would be useful.
Toxic Shock Syndrome
Toxic shock syndrome, caused by Staphylococcus aureus or Streptococcus pyogenes, results from the release of bacterial exotoxins, such as toxic shock syndrome toxin-1 (TSST-1) and streptococcal pyrogenic exotoxin A. These toxins, so-called superantigens, bypass the normal interaction of the antigen presenting cells and T-lymphocytes. The result is activation of large numbers of T cells and massive cytokine release [30]. Cytokine production accounts for the symptoms of toxic shock syndrome, including fever, hypotension, and skin manifestations. Normally, about 30 % of children demonstrate elevated titers of anti-TSST-1 antibody by the time they are 2 years old and greater than 90 % of people demonstrate elevated titers by the time they are 25 years old [31]. Conversely, patients presenting with toxic shock syndrome have a paucity of these antibodies [32]. Intravenous immunoglobulin has been shown in vitro to neutralize TSST-1 and streptococcal superantigens [33–35]. It has therefore been theorized that IVIG is helpful in the treatment of toxic shock syndrome due to its ability to neutralize superantigens, replace deficient antibodies, and via its general anti-inflammatory effects. In vitro neutralization of superantigens may depend on the specific IVIG preparation used [36].
Case reports suggest a potential role of IVIG for the treatment of streptococcal toxic shock syndrome [37, 38]. Furthermore, a retrospective observational study of 53 patients resulted in a reduction in 30-day mortality rate in the group treated with IVIG versus the group treated with placebo (67 versus 34 %, p = 0.02) [39]. The only randomized controlled trial, consisting of 21 patients, was terminated early due to an inability to recruit an adequate number of patients. This study, however, did demonstrate a trend toward reduced 28-day mortality rate for patients with streptococcal toxic shock syndrome treated with IVIG (3.6-fold reduction). The trial did not achieve statistical significance (p = 0.3) [40]. The effectiveness of IVIG for the treatment of streptococcal toxic shock syndrome in adults and children was challenged by a retrospective cohort of 192 pediatric patients. The use of IVIG versus placebo did not result in any difference in mortality rate (4.5 versus 4.5 %, p = 1.0). Moreover, IVIG was associated with increased length of hospital stay (25 versus 12 days, p = 0.003) [41]. The use of IVIG in the treatment of staphylococcal toxic shock syndrome is less well studied; however, an in vitro study suggests that S. aureus superantigen may be less effectively inhibited than that of S. pyogenes [42].
The treatment of streptococcal toxic shock syndrome is supported by several case reports and retrospective studies. At the same time, a pediatric retrospective cohort study demonstrated no benefit. Data on use of IVIG for the treatment of staphylococcal toxic shock syndrome is extremely lacking. While a large randomized controlled trial is needed to define the role of IVIG for the treatment of toxic shock syndromes, this would be challenging due to the rarity of the condition. With the given evidence, IVIG may be useful as adjunctive therapy for the treatment of streptococcal toxic shock syndrome.
Acute Myocarditis
Acute myocarditis is a clinical condition resulting from inflammation of cardiac muscle, which is often caused by viral illness. Both the antiviral and immunomodulatory effects of IVIG suggest that it may play a role in the treatment of acute myocarditis. In animal models using mice inoculated with coxsackievirus B3 or murine encephalomyocarditis virus, IVIG led to decreased myocardial damage, decreased production of the pro-inflammatory cytokines TNF-alpha, IFN-gamma, and IL-6, and better survival when compared to that of placebo (21/21 versus 10/21, p < 0.01) [43, 44]. Multiple case reports and case series have documented the successful treatment of acute myocarditis with IVIG [45–48]. As none of these trials had a control arm, it is difficult to determine if patients improved as a result of the IVIG or as a result of the natural course of illness. The only randomized, controlled trial using 62 patients with acute dilated cardiomyopathy concluded no benefit of treatment with IVIG over placebo. Both groups demonstrated significant improvement in left ventricular ejection fraction over time; however, there was no significant difference between groups [49].
Viruses cause the majority of acute myocarditis in children. Intravenous immunoglobulin may be especially helpful in this group because the preparations contain pooled immunoglobulins against many viruses that circulate in the community. Still, the use of IVIG for the treatment of acute myocarditis remains controversial in children. No randomized controlled trials of IVIG for the treatment of myocarditis in children exist. A retrospective review compared 21 children treated with IVIG with a historical cohort of 25 children treated without IVIG. All had a diagnosis of acute myocarditis. Those treated with high-dose IVIG (2 g/kg) for presumed myocarditis had improved cardiac function at the time of treatment and up to 1 year after. There was also a trend toward improved survival 1 year later in the group treated with IVIG (84 versus 60 %, p = 0.069) [50]. The results of this study may be confounded by the fact that the treatment group was observed from a later date, when other adjunctive therapy had improved, than that of the historical control group. The treatment group received cardiac medications (e.g., ACE inhibitors and inotropes) in addition to IVIG, whereas the historical control group did not. It is therefore difficult to differentiate whether the improvement in cardiac function was due to the IVIG versus other cardiac medications.
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are considered variants of the same pathologic process [51]. They are characterized by widespread blisters and purpuric lesions. Both are severe, life-threatening reactions, most commonly in response to medications (or infection in children). Both conditions are caused by an overexpression of Fas ligand-induced keratinocyte apoptosis, which then leads to necrosis and sloughing of the epidermis. The most important component of therapy for SJS/TEN is supportive care with a focus on maintenance of fluid and electrolyte status and prevention of infection. Intravenous immunoglobulin is a suggested treatment adjunct as it blocks the Fas-Fas ligand-mediated keratinocyte apoptosis [52].
Several case reports and case series have reported the successful treatment of both SJS and TEN with IVIG [53–57]. A handful of retrospective cohort studies have failed to show a significant reduction in mortality rate, despite a trend toward reduced mortality rate [58–61]. All studies were small, owing to the rarity of SJS and TEN. One Chinese retrospective cohort of 82 patients did demonstrate a reduced hospital length of stay with the use of IVIG plus corticosteroids versus corticosteroids alone (26.4 ± 9.5 versus 18.1 ± 5.3 days, p < 0.05) [58]. Therefore, IVIG may have some utility in the treatment of SJS and TEN, but the evidence is not sufficient to say this with certainty.
H1N1 Influenza
Pandemic 2009 H1N1, sometimes called “swine flu,” is a novel strain of influenza that was first described in April 2009. Compared to seasonal influenza in previous years, 2009 H1N1 disproportionately affects healthy people under the age of 65 [62]. A study by the CDC reported low levels of IgG against 2009 H1N1 in people younger than 65. Immunoglobulin G against pandemic influenza was found in the serum of no children, in 6–9 % of serum of 18- to 64-year olds, and in 33 % of serum of those greater than 65 years old [63]. Additional therapeutic options are needed for cases of severe influenza and for cases caused by oseltamivir-resistant strains.
Convalescent serum was historically used for treatment of many illnesses prior to the availability of antibiotics. A meta-analysis reported decreased crude mortality rate in patients infected with Spanish flu when treated with convalescent human serum from survivors [64]. More recently, case reports have demonstrated successful treatment of influenza-associated acute respiratory distress syndrome with either convalescent serum or IVIG [65, 66]. Intravenous immunoglobulin preparations from plasma obtained even prior to the 2009 pandemic influenza outbreak contain neutralizing antibody against 2009 H1N1 influenza [67, 68]. Treatment of 2009 H1N1 influenza virus-infected mice with IVIG resulted in improved survival when compared with that of placebo (88 versus 30 %) [69]. Hyperimmune IVIG (H-IVIG), prepared from convalescent plasma from patients who recovered from 2009 H1N1 influenza, may be a promising treatment for patients with severe influenza. A double-blind randomized controlled trial of 35 patients reported a significantly lower day 5 and day 7 post treatment influenza viral load (3.3 versus 4.67 log10 copies, p = 0.04 and undetectable versus 4.53 log10 copies, p = 0.02, respectively) and reduced mortality (OR 0.14, 95 % CI 0.02, 0.92) when compared with that of the control group [70]. Patients with IgG2 subclass deficiency can have especially severe disease secondary to 2009 H1N1 influenza [71, 72]. A case series documenting treatment of this group of patients with H-IVIG resulted in clinical improvement [73]. Treatment with H-IVIG may be limited by practical aspects of convalescent plasma collection [74].
While no randomized controlled trials have assessed the utility of IVIG for the treatment of 2009 H1N1 influenza, prior success when using convalescent serum from influenza survivors suggest that immunoglobulins may serve as treatment adjuncts. Certain patient subgroups, including those with severe illness and those with IgG subclass deficiencies may derive greater benefit.
Adverse Events Associated with IVIG
A large percentage of patients receiving IVIG experience adverse effects [75]. These include mild reactions such as fever, chills, abdominal pain, myalgias, or headaches [76]. More serious reactions have been reported and include anaphylaxis, hypotension, thrombotic events, aseptic meningitis, Stevens-Johnson syndrome, and renal failure [76]. Potential risks and benefits must be fully considered when prescribing IVIG for critically ill patients.
Another consideration with the use of IVIG is the potential for transmission of infectious agents. Prior to 1985 and the advent of HIV antibody testing in blood products, an estimated 12,000 to 25,000 individuals were infected through receipt of red blood cells, platelets, or plasma [77]. Likewise, hepatitis C was once commonly spread through transfusion prior to 1992 when routine screening of blood products began in the USA [78]. Although the blood supply undergoes rigorous screening for known viruses and the risk of transmission is low, there is a very real risk of transmission of yet to be discovered infectious agents. This is evidenced through the history of HIV and hepatitis C transmission. Variant Creutzfeldt-Jakob disease (vCJD), which many people may have been exposed to during travels or residence in the UK and other European countries, can also be transmitted through the blood supply. Based on models, the risk of transmission through red blood cell transfusion is estimated to be between 1 in 480,000 to 1 in 134 million [79]. While prion filtration and donor deferral appear to be effective approaches to reduce the risk of transmission, they are not currently employed [80, 81].
Summary
Intravenous immunoglobulin exerts its effects through immunoglobulin replacement, anti-inflammatory effects, and immunomodulatory effects. Based on these properties, IVIG has been proposed as an adjunct therapy for critically ill patients. However, conclusive data to support the use of IVIG in sepsis, toxic shock syndrome, acute myocarditis, SJS/TEN and severe H1N1 is lacking (Table 1). The INIS trial provided definitive evidence of no utility of IVIG for treatment of sepsis in neonates. While most adult studies suggest no role of IVIG for the routine treatment of sepsis, there is some evidence to suggest that IgA- and IgM-enriched immunoglobulin preparations may play a role as treatment adjuncts. Additionally, sporadic, anecdotal case reports do show some benefit in individual patients. Despite this, to decide upon whether routine use of IVIG should be a standard of care in certain conditions, rigorous trials to support the use of IVIG in the treatment of pediatric and adult sepsis are still needed. Well-designed studies documenting the clinical utility of IVIG for treatment of streptococcal toxic shock syndrome are also lacking. However, in vitro and several smaller in vivo studies suggest that IVIG may play a beneficial role in streptococcal toxic shock syndrome. The evidence for use of IVIG for the treatment of staphylococcal toxic shock syndrome is virtually nonexistent. Data for the use of IVIG for the treatment of acute myocarditis is conflicting but may provide some benefit in the pediatric population where viral etiologies tend to predominate. Likewise, smaller studies resulted in inconsistent outcomes for the use of IVIG in the treatment of SJS and TEN. Influenza virus has been successfully treated in the past with convalescent serum of survivors, suggesting a current role of IVIG for the treatment of pandemic 2009 H1N1 influenza virus. A small randomized controlled trial reported improved survival. Intravenous immunoglobulin may be especially beneficial in patients with severe illness secondary to influenza virus and those with IgG2 deficiency. Larger, more rigorous studies are required for definitive evidence to support the use of IVIG in critically ill patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
American Academy of Pediatrics. Red Book: 2012 Report of the Committee on Infectious Diseases. Pickering LK, ed. 29th ed. Elk Grove Village, IL; 2012:56-62.
Kawada K, Terasaki PI. Evidence for immunosuppression by high dose gammaglobulin. Exp Hematol. 1987;15:133–6.
Tsubakio T, Kurata Y, Katagiri S, et al. Alteration of T cell subsets and immunoglobulin synthesis in vitro during high dose gamma-globulin therapy in patients with idiopathic thrombocytopenic purpura. Clin Exp Immunol. 1983;53:697.
Delfraissy JF, Tchernia G, Laurian Y, et al. Suppressor cell function after intravenous gammaglobulin treatment in adult chronic idiopathic thrombocytopenic purpura. Br J Haematol. 1985;60:315.
Koffman BM, Dalakas MC. Effect of high-dose intravenous immunoglobulin on serum chemistry, hematology, and lymphocyte subpopulations: assessments based on controlled treatment trials in patients with neurological diseases. Muscle Nerve. 1997;20:1102.
Anderson J, Skansen-Saphir U, Sparrelid E, et al. Intravenous immune globulin affects cytokine production in T lymphocytes and monocytes/macrophages. Clin Exp Immunol. 1996;104 Suppl 1:10–20.
Menezes MCS, Benard G, Sato MN, et al. In vitro inhibitory activity of tumor necrosis factor alpha and interleukin-2 of human immunoglobulin preparations. Int Arch Allergy Immunol. 1997;114:323–8.
Shimozato T, Iwata M, Tamura N. Suppression of tumor necrosis factor alpha production by a human immunoglobulin preparation for intravenous use. Infect Immun. 1990;58:1384.
Samuelsson A, Towers TL, Ravetch JV. Anti-inflammatory activity of IVIG mediated through the inhibitory Fc receptor. Science. 2001;291:484.
Anthony RM, Kobayashi T, Wermeling F, Ravetch JV. Intravenous gammaglobulin suppresses inflammation through a novel T(H)2 pathway. Nature. 2011;475:110.
Gupta M, Noel GJ, Schaefer M, et al. Cytokine modulation with immune γ-globulin in peripheral blood of normal children and its implications in Kawasaki disease treatment. J Clin Immunol. 2001;21:193–9.
Takei S, Arora YK, Walker SM. Intravenous immunoglobulin contains specific antibodies inhibitory to activation of T cells by staphylococcal toxin superantigens. J Clin Invest. 1993;91:602–7.
Aukrust P, Froland SS, Liabakk NB, et al. Release of cytokines, soluble cytokine receptors, and interleukin-1 receptor antagonist after intravenous immunoglobulin administration in vivo. Blood. 1994;84:2136–43.
Kam JC, Szefler SJ, Surs W, et al. Combination IL-2 and IL-4 reduces glucocorticoid receptor-binding affinity and T cell response to glucocorticoids. J Immunol. 1993;151:3460–6.
Spahn JD, Leung DYM, Chan MTS, et al. Mechanisms of glucocorticoid reduction in asthmatics treated with intravenous immunoglobulin. J Allergy Clin Immunol. 1999;103:421–6.
Modiano JF, Amran D, Lack G, et al. Posttranscriptional regulation of T cell IL-2 production by human pooled immunoglobulin. Clin Immunol Immunopathol. 1997;83:77–85.
Vassilev T, Gelin C, Kaveri SV. Antibodies to the CD5 molecule in normal human immunoglobulins for therapeutic use (intravenous immunoglobulins, IVIG). Clin Exp Immunol. 1993;92:369–72.
Gelfand EW. Intravenous immune globulin in autoimmune and inflammatory diseases. N Engl J Med. 2012;367:2015–25. This paper provides a thorough review of currently proposed mechanisms of action of IVIG.
Sylvestre D, Clynes R, Ma M. Immunoglobulin G-mediated inflammatory responses develop normally in complement-deficient mice. J Exp Med. 1996;184:2385–92.
Tackenberg B, Jelcic I, Baerenwaldt A, et al. Impaired inhibitory Fcγ receptor IIB expression on B cells in chronic inflammatory demyelinating polyneuropathy. Proc Natl Acad Sci U S A. 2009;106:4788–92.
Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–54.
Werdan K, Pilz G, Bujdoso O, et al. Score-based immunoglobulin G therapy of patients with sepsis: the SBITS study. Crit Care Med. 2007;35:2693.
Alejandria MM, Lansang MA, Dans LF, Mantaring 3rd JB. Intravenous immunoglobulin for treating sepsis, severe sepsis and septic shock. Cochrane Database Syst Rev. 2013;9, CD001090.
Pildal J, Gøtzsche PC. Polyclonal immunoglobulin for treatment of bacterial sepsis: a systematic review. Clin Infect Dis. 2004;39:38.
Laupland KB, Kirkpatrick AW, Delaney A. Polyclonal intravenous immunoglobulin for the treatment of severe sepsis and septic shock in critically ill adults: a systematic review and meta-analysis. Crit Care Med. 2007;35:2686.
Kreymann KG, de Heer G, Nierhaus A, Kluge S. Use of polyclonal immunoglobulins as adjunctive therapy for sepsis or septic shock. Crit Care Med. 2007;35:2677.
El-Nawawy A, El-Kinany H, Hamdy El-Sayed M, Boshra N. Intravenous polyclonal immunoglobulin administration to sepsis syndrome patients: a prospective study in a pediatric intensive care unit. J Trop Pediatr. 2005;51:271.
Ohlsson A, Lacy JB. Intravenous immunoglobulin for suspected or subsequently proven infection in neonates. Cochrane Database Syst. Rev. 2010. CD001239
INIS Collaborative Group, Brocklehurst P, Farrell B, et al. Treatment of neonatal sepsis with intravenous immune globulin. N Engl J Med. 2011;365:1201. This large randomized, controlled trial provided definitive evidence for lack of benefit of IVIG for the treatment of neonatal sepsis.
Que YA, Moreillon P. Staphylococcus aureus (including staphylococcal toxic shock). In: Mandell: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, 7th ed. Philadelphia: Churchill Livingstone, An Imprint of Elsevier; 2009: 2543-74
Vergeront JM, Stolz SJ, Crass BA, et al. Prevalence of serum antibody to staphylococcal enterotoxin F among Wisconsin residents: implications for toxic-shock syndrome. J Infect Dis. 1983;148(4):692–8.
Stolz SJ, Davis JP, Vergeront JM, et al. Development of serum antibody to toxic shock toxin among individuals with toxic shock syndrome in Wisconsin. J Infect Dis. 1985;151(5):883–9.
Yanagisawa C, Hanaki H, Natae T, et al. Neutralization of staphylococcal exotoxins in vitro by human-origin intravenous immunoglobulin. J Infect Chemother. 2007;13:368–72.
Norrby-Teglund A, Kaul R, Low DE, et al. Plasma from patients with severe invasive group A streptococcal infections treated with normal polyspecific IgG inhibits streptococcal superantigen-induced T cell proliferation and cytokine production. J Immunol. 1996;156:3057.
Norrby-Teglund A, Kaul R, Low DE, et al. Evidence for the presence of streptococcal-superantigen-neutralizing antibodies in normal polyspecific immunoglobulin G. Infect Immun. 1996;64:5395.
Darenberg J, Söderquist B, Normark BH, Norrby-Teglund A. Differences in potency of intravenous polyspecific immunoglobulin G against streptococcal and staphylococcal superantigens: implications for therapy of toxic shock syndrome. Clin Infect Dis. 2004;38:836.
Barry W, Hudgins L, Donta ST, Pesanti EL. Intravenous immunoglobulin therapy for toxic shock syndrome. JAMA. 1992;267:3315.
Lamothe F, D’Amico P, Ghosn P, et al. Clinical usefulness of intravenous human immunoglobulins in invasive group A streptococcal infections: case report and review. Clin Infect Dis. 1995;21(6):1469–70.
Kaul R, McGeer A, Norrby-Teglund A, et al. Intravenous immunoglobulin therapy for streptococcal toxic shock syndrome—a comparative observational study. The Canadian Streptococcal Study Group. Clin Infect Dis. 1999;28:800–7.
Darenberg J, Ihendyane N, Sjölin J, et al. Intravenous immunoglobulin G therapy in streptococcal toxic shock syndrome: a European randomized, double-blind, placebo-controlled trial. Clin Infect Dis. 2003;37:333.
Shah SS, Hall M, Srivastava R, et al. Intravenous immunoglobulin in children with streptococcal toxic shock syndrome. Clin Infect Dis. 2009;49:1369.
Schrage B, Duan G, Yang LP, et al. Different preparations of intravenous immunoglobulin vary in their efficacy to neutralize streptococcal superantigens: implications for treatment of streptococcal toxic shock syndrome. Clin Infect Dis. 2006;43:743.
Takada H, Kishimoto C, Hiraoka Y. Therapy with immunoglobulin suppresses myocarditis in a murine coxsackievirus B3 model. Antiviral and anti-inflammatory effects. Circulation. 1995;92(6):1604–11.
Kishimoto C, Takada H, Kawamata H, et al. Immunoglobulin treatment prevents congestive heart failure in murine encephalomyocarditis viral myocarditis associated with reduction of inflammatory cytokines. J Pharmacol Exp Ther. 2001;299(2):645–51.
McNamara DM, Rosenblum WD, Janosko KM, et al. Intravenous immune globulin in the therapy of myocarditis and acute cardiomyopathy. Circulation. 1997;95(11):2476–8.
Nigro G, Bastianon V, Colloridi V, et al. Human parvovirus B19 infection in infancy associated with acute and chronic lymphocyte myocarditis and high cytokine levels: report of 3 cases and review. Clin Infect Dis. 2001;31:65–9.
Takeda Y, Yasuda S, Miyazaki S, et al. High-dose immunoglobulin G therapy for fulminant myocarditis. Jpn Circ J. 1998;62:871–2.
Tedeschi A, Giannini S, Ciceri L, Massari FM. High-dose intravenous immunoglobulin in the treatment of acute myocarditis. A case report and review of the literature. J Intern Med. 2002;251:169–73.
McNamara DM, Holubkov R, Starling RC, et al. Controlled trial of intravenous immune globulin in recent-onset dilated cardiomyopathy. Circulation. 2001;103:2254–9.
Drucker NA, Colan SD, Lewis AB, et al. Gamma-globulin treatment of acute myocarditis in the pediatric population. Circulation. 1994;89:252.
Duvic M. Urticaria, drug hypersensitivity rashes, nodules and tumors, and atrophic diseases. In: Goldman: Goldman’s Cecil medicine, 24th ed. Saunders, An Imprint of Elsevier; 2011: 2532-43
Viard I, Wehrli P, Bullani R, et al. Inhibition of toxic epidermal necrolysis by blockade of CD95 with human intravenous immunoglobulin. Science. 1998;282:490–3.
Phan TG, Wong RC, Crotty K, Aldestein S. Toxic epidermal necrolysis in acquired immunodeficiency syndrome treated with intravenous gammaglobulin. Aust J Dermatol. 1999;40(3):153–7.
Magina S, Lisboa C, Goncalves E, et al. A case of toxic epidermal necrolysis treated with intravenous immunoglobulin. Br J Dermatol. 2000;142(1):191–2.
Tristani-Firouzi P, Peterson MJ, Saffle JR. Treatment of toxic epidermal necrolysis with intravenous immunoglobulin in children. J Am Acad Dermatol. 2002;47(4):548–52.
Wolff K, Tappeiner G. Treatment of toxic epidermal necrolysis: the uncertainty persist but the fog is dispersing. Arch Dermatol. 2003;139(1):85–6.
Comparin C, Hans Filho G, Takita LC, et al. Treatment of toxic epidermal necrolysis with intravenous immunoglobulin: a series of three cases. An Bras Dermatol. 2012;87(3):477–81.
Chen J, Wang B, Zeng Y, Xu H. High-dose intravenous immunoglobulins in the treatment of Stevens-Johnson syndrome and toxic epidermal necrolysis in Chinese patients: a retrospective study of 82 cases. Eur J Dermatol. 2010;20(6):743–7. doi:10.1684/ejd.2010.1077.
Schneck J, Fagot JP, Sekula P, et al. Effects of treatments on the mortality of Stevens-Johnson syndrome and toxic epidermal necrolysis: a retrospective study on patients included in the prospective EuroSCAR Study. J Am Acad Dermatol. 2008;58:33–40.
Stella M, Clemente A, Bollero D, et al. Toxic epidermal necrolysis (TEN) and Stevens-Johnson syndrome (SJS): experience with high-dose intravenous immunoglobulins and topical conservative approach. A retrospective analysis. Burns. 2007;33:452–9.
Yang Y, Xu J, Li F, Zhu X. Combination therapy of intravenous immunoglobulin and corticosteroid in the treatment of toxic epidermal necrolysis and Stevens-Johnson syndrome: a retrospective comparative study in China. Int J Dermatol. 2009;48(10):1122–8. doi:10.1111/j.1365-4632.2009.04166.x.
To KK, Wong SS, Li IW, et al. Concurrent comparison of epidemiology, clinical presentation and outcome between adult patients suffering from the pandemic influenza A (H1N1) 2009 virus and the seasonal influenza A virus infection. Postgrad Med J. 2010;86:515–21.
Katz J, Hancock K, Veguilla V, et al. Serum cross-reactive antibody response to a novel influenza A (H1N1) virus after vaccination with seasonal influenza vaccine. Morb Mortal Wkly Rep. 2009;58:521–4.
Luke TC, Kilbane EM, Jackson JL, et al. Meta-analysis: convalescent blood products for Spanish influenza pneumonia: a future H5N1 treatment? Ann Intern Med. 2006;145(8):599–609.
Zhou B, Zhong N, Guan Y. Treatment with convalescent plasma for influenza A (H5N1) infection. N Engl J Med. 2007;357:1451.
Chong JL, Sapari S, Kuan YC. A case of acute respiratory distress syndrome associated with novel H1N1 treated with intravenous immunoglobulin G. J Microbiol Immunol Infect. 2011;44:319–22.
Hong DK, Tremoulet AH, Burns JC, et al. Cross-reactive neutralizing antibody against pandemic 2009 H1N1 influenza A virus in intravenous immunoglobulin preparations. Pediatr Infect Dis J. 2011;30:67–9.
Yunoki M, Kubota-Koketsu R, Urayama T, et al. Significant neutralizing activity of human immunoglobulin preparations against pandemic 2009 H1N1. Br J Haematol. 2010;148:953–55.
Hagiwara K, Kawami S, Kato-Mori Y, et al. Protective role of human intravenous immunoglobulin from influenza A virus infection in mice. Open Hemotol J. 2012;6:8–11.
Hung I, To K, Lee CK, et al. Hyperimmune IV immunoglobulin treatment: a multicenter double-blind randomized controlled trial for patients with severe 2009 influenza A (H1N1) infection. Chest. 2013;144:464–73.
Gordon CL, Johnson PD, Permezel M, et al. Association between severe pandemic 2009 influenza A (H1N1) virus infection and immunoglobulin G(2) subclass deficiency. Clin Infect Dis. 2010;50:672–8.
Gordon CL, Holmes NE, Grayson ML, et al. Comparison of immunoglobulin G subclass concentrations in severe community-acquired pneumonia and severe pandemic 2009 influenza A (H1N1) infection. Clin Vaccine Immunol. 2012;19:446–8.
Gordon CL, Langan K, Charles P, et al. Pooled human immunoglobulin therapy in critically ill patients with pandemic 2009 influenza A (H1N1) pneumonitis and immunoglobulin G2 subclass (IgG2) deficiency. Clin Infect Dis. 2011;52:422–6.
Wong HK, Lee CK, Hung I, et al. Practical limitations of convalescent plasma collection: a case scenario in pandemic preparation for influenza A (H1N1) infection. Transfusion. 2010;50:1967–71.
2002 Immune Deficiency Foundation patient survey. Available at: http://www.primaryimmune.org/pid/survey.htm. Accessed February 12, 2014.
Orange JS, Hossny EM, Weiler CR, et al. Use of intravenous immunoglobulin in human disease: a review of evidence by members of the primary immunodeficiency committee of the American Academy of Allergy, Asthma and Immunology. J Allergy Clin Immunol. 2006;117:S525–553.
Kalbfleisch JD, Lawless JF. Estimating the incubation time distribution and expected number of cases of transfusion-associated acquired immune deficiency syndrome. Transfusion. 1989;29(8):672.
Centers for Disease Control. Hepatitis C FAQs for the Public. Available at: http://www.cdc.gov/hepatitis/c/cfaq.htm#cFAQ31. Accessed May 8, 2014.
Yang H, Gregori L, Asher DM, et al. Risk assessment for transmission of variant Creutzfeldt-Jakob disease by transfusion of red blood cells in the United States. Transfusion. 2014 Apr 1
Teljeur C, Flattery M, Harrington P, et al. Cost-effectiveness of prion filtration of red blood cells to reduce the risk of transfusion-transmitted variant Creutzfeldt-Jakob disease in the Republic of Ireland. Transfusion. 2012;52(11):2285–93.
Correll PK, Law MG, Seed CR, et al. Variant Creutzfeldt-Jakob disease in Australian blood donors: estimation of risk and the impact of deferral strategies. Vox Sang. 2001;81(1):6–11.
Compliance with Ethics Guidelines
Conflict of Interest
Summer Donovan and Gonzalo Bearman have no disclosures relevant to this work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Cardiovascular Infections
Rights and permissions
About this article
Cite this article
Donovan, S., Bearman, G.M.L. Use of Intravenous Immunoglobulin in Critically Ill Patients. Curr Infect Dis Rep 16, 447 (2014). https://doi.org/10.1007/s11908-014-0447-4
Published:
DOI: https://doi.org/10.1007/s11908-014-0447-4