Abstract
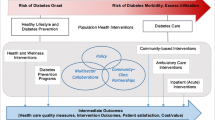
The current diabetes epidemic threatens to overwhelm the healthcare system unless we redesign how diabetes care is delivered. The number of endocrinologists is grossly inadequate to provide care for all individuals with diabetes, but with the appropriate utilization of the primary care workforce and alternative healthcare providers working together in teams, effective diabetes care can be provided to all. We propose a patient-centered, goal-based approach with resources devoted to care coordination, measurement of outcomes, appropriate use of technology, and measurement of patient satisfaction. Financial incentives to healthcare systems and providers need to be based on defined outcome measures and reducing long-term total medical expenditures, rather than reimbursement based on number of visits and lengthy documentation. Endocrinologists have a responsibility in setting up effective diabetes care delivery systems within their organizations, in addition to delivering diabetes care and serving as a resource for the educational needs for other medical professionals in the community. There are major challenges to implementing such systems, both at the financial and organizational levels. We suggest a stepwise implementation of discrete components based on the local priorities and resources and provide some examples of steps we have taken at our institution.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
CDC. Diabetes report card 2014. www.cdc.gov/diabetes/library/reports/congress.html Accessed on 16 Feb 2016. 2014.
Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med. 2014;370(16):1514–23. doi:10.1056/NEJMoa1310799.
CDC. Annual number (in thousands) of new cases of diagnosed diabetes among adults aged 18–79 years, United States, 1980–2014. 2015. http://www.cdc.gov/diabetes/statistics/incidence/fig1.htm Accessed 16 Feb 2016.
Dall TM, Yang W, Halder P, Pang B, Massoudi M, Wintfeld N, et al. The economic burden of elevated blood glucose levels in 2012: diagnosed and undiagnosed diabetes, gestational diabetes mellitus, and prediabetes. Diabetes Care. 2014;37(12):3172–9. doi:10.2337/dc14-1036.
Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999–2010. N Engl J Med. 2013;368(17):1613–24. doi:10.1056/NEJMsa1213829.
Lu H, Holt JB, Cheng YJ, Zhang X, Onufrak S, Croft JB. Population-based geographic access to endocrinologists in the United States, 2012. BMC Health Serv Res. 2015;15(1):541. doi:10.1186/s12913-015-1185-5.
Vigersky RA, Fish L, Hogan P, Stewart A, Kutler S, Ladenson PW, et al. The clinical endocrinology workforce: current status and future projections of supply and demand. J Clin Endocrinol Metab. 2014;99(9):3112–21. doi:10.1210/jc.2014-2257.
Primary Care Workforce Facts and Stats Number 1. Agency for Healthcare Research and Quality 2010 http://www.ahrq.gov/research/findings/factsheets/primary/pcwork1/index.html Accessed 1 May 2016.
Primary Care Physicians by Field. The Henry J Kaiser Family Foundation 2016. http://kff.org/other/state-indicator/primary-care-physicians-by-field/ Accessed 4 May 2016.
Whitcomb ME. A cross-national comparison of generalist physician workforce data. Evidence for US supply adequacy. JAMA. 1995;274(9):692–5.
Salsberg ES. Is the physician shortage real? Implications for the recommendations of the institute of medicine committee on the governance and financing of graduate medical education. Acad Med. 2015;90(9):1210–4. doi:10.1097/ACM.0000000000000837.
Weeks DL, Polello JM, Hansen DT, Keeney BJ, Conrad DA. Measuring primary care organizational capacity for diabetes care coordination: the Diabetes Care Coordination Readiness Assessment. J Gen Intern Med. 2014;29(1):98–103. doi:10.1007/s11606-013-2566-2. This report describes the development and validation of an instrument which assesses the capabilities of primary care practices to deliver patient-centered diabetes care.
Chen PG, Mehrotra A, Auerbach DI. Do we really need more physicians? Responses to predicted primary care physician shortages. Med Care. 2014;52(2):95–6. doi:10.1097/MLR.0000000000000046.
Powers BW, Chaguturu SK. ACOs and high-cost patients. N Engl J Med. 2016;374(3):203–5. doi:10.1056/NEJMp1511131.
McCluskey P. Partners’ $1.2b patient data system seen as key to future—aims for one file per person, fewer errors. The Boston Globe. June 1, 2015. http://www.bostonglobe.com/business/2015/05/31/partners-launches-billion-electronic-health-records-system/oo4nJJW2rQyfWUWQlvydkK/story.html. Accessed 1 May 2016
McCluskey P. UMass Memorial Health Care plans big patient record upgrade. The Boston Globe. July 27, 2015. http://www.bostonglobe.com/business/2015/07/27/umass-memorial-health-care-spend-million-patient-record-upgrade/0SCwlTr7UUindy7DF21tSK/story.html. Accessed 1 May 2016
Hsu WC, Lau KH, Huang R, Ghiloni S, Le H, Gilroy S, et al. Utilization of a cloud-based diabetes management program for insulin initiation and titration enables collaborative decision making between healthcare providers and patients. Diabetes Technol Ther. 2016;18(2):59–67. doi:10.1089/dia.2015.0160.
Grady M, Cameron H, Levy BL, Katz LB. Remote health consultations supported by a diabetes management web application with a new glucose meter demonstrates improved glycemic control. J Diabetes Sci Technol. 2015. doi:10.1177/1932296815622646.
Zhai YK, Zhu WJ, Cai YL, Sun DX, Zhao J. Clinical- and cost-effectiveness of telemedicine in type 2 diabetes mellitus: a systematic review and meta-analysis. Medicine. 2014;93(28), e312. doi:10.1097/MD.0000000000000312.
Carallo C, Scavelli FB, Cipolla M, Merante V, Medaglia V, Irace C, et al. Management of Type 2 diabetes mellitus through telemedicine. PLoS One. 2015;10(5), e0126858. doi:10.1371/journal.pone.0126858.
Watts SA, Roush L, Julius M, Sood A. Improved glycemic control in veterans with poorly controlled diabetes mellitus using a Specialty Care Access Network-Extension for Community Healthcare Outcomes model at primary care clinics. J Telemed Telecare. 2015. doi:10.1177/1357633X15598052.
Ackroyd SA, Wexler DJ. Effectiveness of diabetes interventions in the patient-centered medical home. Curr Diabetes Rep. 2014;14(3):471. doi:10.1007/s11892-013-0471-z. This article examines the various aspects of diabetes care delivery using the patient-centered medical home concept, including the financial implications and challenges.
Tricco AC, Ivers NM, Grimshaw JM, Moher D, Turner L, Galipeau J, et al. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet. 2012;379(9833):2252–61. doi:10.1016/S0140-6736(12)60480-2.
Shi L, Khurshid A. Capsule commentary on Weeks et al., measuring primary care organizational capacity for diabetes care coordination: the diabetes care coordination readiness assessment. J Gen Intern Med. 2014;29(1):178. doi:10.1007/s11606-013-2614-y.
Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. Ann Fam Med. 2009;7(3):254–60. doi:10.1370/afm.1002.
Bojadzievski T, Gabbay RA. Patient-centered medical home and diabetes. Diabetes Care. 2011;34(4):1047–53. doi:10.2337/dc10-1671.
American Diabetes A. 1. Strategies for improving care. Diabetes Care. 2016;39 Suppl 1:S6–12. doi:10.2337/dc16-S004. Evidence-based recommendations for improving diabetes care, touching on a variety of aspects including chronic care model, team approach, self-management education, and vulnerable populations.
Association of American Medical Colleges. The complexities of physician supply and demand: projections from 2013 to 2025. 2015 https://www.aamc.org/download/426242/data/ihsreportdownload.pdf. Accessed 16 Feb 2016.
Jackson GL, Lee SY, Edelman D, Weinberger M, Yano EM. Employment of mid-level providers in primary care and control of diabetes. Prim Care Diabetes. 2011;5(1):25–31. doi:10.1016/j.pcd.2010.09.005.
Ohman-Strickland PA, Orzano AJ, Hudson SV, Solberg LI, DiCiccio-Bloom B, O’Malley D, et al. Quality of diabetes care in family medicine practices: influence of nurse-practitioners and physician’s assistants. Ann Fam Med. 2008;6(1):14–22. doi:10.1370/afm.758.
Kuo YF, Goodwin JS, Chen NW, Lwin KK, Baillargeon J, Raji MA. Diabetes mellitus care provided by nurse practitioners vs primary care physicians. J Am Geriatr Soc. 2015;63(10):1980–8. doi:10.1111/jgs.13662.
Lenz ER, Mundinger MO, Hopkins SC, Lin SX, Smolowitz JL. Diabetes care processes and outcomes in patients treated by nurse practitioners or physicians. Diabetes Educ. 2002;28(4):590–8.
Siminerio L, Ruppert KM, Gabbay RA. Who can provide diabetes self-management support in primary care? Findings from a randomized controlled trial. Diabetes Educ. 2013;39(5):705–13. doi:10.1177/0145721713492570.
Martin AL. Changes and consistencies in diabetes education over 5 years: results of the 2010 National Diabetes Education Practice Survey. Diabetes Educ. 2012;38(1):35–46. doi:10.1177/0145721711427611.
Brown NN, Carrara BE, Watts SA, Lucatorto MA. RN diabetes virtual case management: a new model for providing chronic care management. Nurs Adm Q. 2016;40(1):60–7. doi:10.1097/NAQ.0000000000000147.
Boren SA, Fitzner KA, Panhalkar PS, Specker JE. Costs and benefits associated with diabetes education: a review of the literature. Diabetes Educ. 2009;35(1):72–96. doi:10.1177/0145721708326774.
Duncan I, Birkmeyer C, Coughlin S, Li QE, Sherr D, Boren S. Assessing the value of diabetes education. Diabetes Educ. 2009;35(5):752–60. doi:10.1177/0145721709343609.
Forbes A, While A. The nursing contribution to chronic disease management: a discussion paper. Int J Nurs Stud. 2009;46(1):119–30. doi:10.1016/j.ijnurstu.2008.06.010.
Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, Diez Roux AV, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299(23):2751–9. doi:10.1001/jama.299.23.2751.
Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. 2012;142(Suppl):S8–21. doi:10.1016/S0165-0327(12)70004-6.
Katon W, Russo J, Lin EH, Heckbert SR, Karter AJ, Williams LH, et al. Diabetes and poor disease control: is comorbid depression associated with poor medication adherence or lack of treatment intensification? Psychosom Med. 2009;71(9):965–72. doi:10.1097/PSY.0b013e3181bd8f55.
Lin EH, Rutter CM, Katon W, Heckbert SR, Ciechanowski P, Oliver MM, et al. Depression and advanced complications of diabetes: a prospective cohort study. Diabetes Care. 2010;33(2):264–9. doi:10.2337/dc09-1068.
Park M, Katon WJ, Wolf FM. Depression and risk of mortality in individuals with diabetes: a meta-analysis and systematic review. Gen Hosp Psychiatry. 2013;35(3):217–25. doi:10.1016/j.genhosppsych.2013.01.006.
Pillay J, Armstrong MJ, Butalia S, Donovan LE, Sigal RJ, Chordiya P, et al. Behavioral programs for type 1 diabetes mellitus: a systematic review and meta-analysis. Ann Intern Med. 2015;163(11):836–47. doi:10.7326/M15-1399.
Hermanns N, Schmitt A, Gahr A, Herder C, Nowotny B, Roden M, et al. The effect of a Diabetes-Specific Cognitive Behavioral Treatment Program (DIAMOS) for patients with diabetes and subclinical depression: results of a randomized controlled trial. Diabetes Care. 2015;38(4):551–60. doi:10.2337/dc14-1416.
Garrett C, Doherty A. Diabetes and mental health. Clin Med. 2014;14(6):669–72. doi:10.7861/clinmedicine.14-6-669.
Theising KM, Fritschle TL, Scholfield AM, Hicks EL, Schymik ML. Implementation and clinical outcomes of an employer-sponsored, pharmacist-provided medication therapy management program. Pharmacotherapy. 2015;35(11):e159–63. doi:10.1002/phar.1650.
Kraemer DF, Kradjan WA, Bianco TM, Low JA. A randomized study to assess the impact of pharmacist counseling of employer-based health plan beneficiaries with diabetes: the EMPOWER study. J Pharm Pract. 2012;25(2):169–79. doi:10.1177/0897190011418513.
Shawn McFarland M, Wallace JP, Parra J, Baker J. Evaluation of patient satisfaction with diabetes management provided by clinical pharmacists in the patient-centered medical home. Patient. 2014;7(1):115–21. doi:10.1007/s40271-013-0039-7.
Wang Y, Yeo QQ, Ko Y. Economic evaluations of pharmacist-managed services in people with diabetes mellitus: a systematic review. Diabet Med. 2015. doi:10.1111/dme.12976.
Bolen SD, Sage P, Perzynski AT, Stange KC. No moment wasted: the primary-care visit for adults with diabetes and low socio-economic status. Prim Health Care Res Dev. 2016;17(1):18–32. doi:10.1017/S1463423615000134.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Samir Malkani, Sheri A. Keitz, and David M. Harlan declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Health Care Delivery Systems and Implementation in Diabetes
Rights and permissions
About this article
Cite this article
Malkani, S., Keitz, S.A. & Harlan, D.M. Redesigning Diabetes Care: Defining the Role of Endocrinologists Among Alternative Providers. Curr Diab Rep 16, 121 (2016). https://doi.org/10.1007/s11892-016-0818-3
Published:
DOI: https://doi.org/10.1007/s11892-016-0818-3